Abstract
Overwhelming postsplenectomy infection (OPSI) syndrome is a rare condition, but is associated with high mortality. However, recognition and clinical management of OPSI is not well established. The prevalence of splenectomy increased recently because it was a clinically effective treatment for hepatitis C virus-associated thrombocytopenia before the introduction of the interferon/ribavirin combination therapy. We reviewed the literature characterizing the clinicopathological features of OPSI and assessed the most effective and feasible administration of the condition. A Medline search was performed using the keywords 'overwhelming', 'postsplenectomy infection', 'postsplenectomy sepsis', 'chronic liver disease', and/or 'splenectomy'. Additional articles were obtained from references within the papers identified by the Medline search. Durations between splenectomy and onset of OPSI ranged from less than 1 wk to more than 20 years. Autopsy showed that many patients with OPSI also had Waterhouse-Friderichsen syndrome. Although the mortality rate from OPSI has been reduced by appropriate vaccination and education, the precise pathogenesis and a suitable therapeutic strategy remain to be elucidated. Protein energy malnutrition (PEM) is commonly observed in cirrhotic patients. Since the immune response in patients with PEM is compromised, a more careful management for OPSI should therefore be applied for cirrhotic patients after splenectomy. In addition, strict long-term follow up of OPSI patients including informed consent will lead to a better prognosis.
Keywords: Overwhelming postsplenectomy infection, Splenectomy, Overwhelming, Postsplenectomy sepsis, Chronic liver disease, Postsplenectomy infection
INTRODUCTION
Splenectomized patients are a significant infection risk, because the spleen is the largest accumulation of lymphoid tissue in the body[1]. Overwhelming postsplenectomy infection (OPSI) is a serious fulminant process that carries a high mortality rate[2–4]. OPSI cases have been well documented, and more recently the syndrome was reviewed in the literature[1,5,6]. The pathogenesis and risk of developing fatal OPSI remain ill-defined, however, especially in the normal adult host.
Anti-hepatitis C virus (HCV) therapy with pegylated interferon has proven effective for virus clearance in recent years[7,8]. Prior to that, treatment of HCV-associated thrombocytopenia was an important and unresolved problem[9,10]. Splenectomy in patients with hepatitis C cirrhosis is now a safer prelude to antiviral treatment[11–14]. However, protein energy malnutrition (PEM) is a common manifestation in patients with liver cirrhosis, with incidences as high as 65%-90%[15–17], putting them at a higher risk of OPSI, because patients with PEM generally have a reduced immune response. This review describes the clinical features of OPSI and discusses management strategies for patients with OPSI, particularly those with chronic liver disease.
Symptoms of OPSI
King and Shumacker first described bacterial sepsis following splenectomy in infants and children in 1952[18]. It emerged subsequently that a comparable syndrome occurs in asplenic adults REF. Fulminant bacterial sepsis in asplenic patients will be termed OPSI in this review in keeping with common usage in the literature.
Aspecific and mild physical symptoms of postsplenectomy appear in the early stages of OPSI. These include fatigue, colored skin, body weight loss, abdominal pain, diarrhea, constipation, nausea, and headache (Table 1)[6,19]. Pneumonia and meningitis are frequent more severe concomitants. The clinical course may rapidly progress to coma and death within 24 to 48 h, due to the high incidence of shock, hypoglycemia, marked acidosis, electrolyte abnormalities, respiratory distress, and disseminated intravascular coagulation[20,21]. The mortality rate is 50%-70% despite aggressive therapy that includes intravenous fluids, antibiotics, vasopressors, steroids, heparin, packed red blood cells, platelets, cryoprecipitates, and fresh frozen plasma[2,19,22–24]. The later clinical course frequently mirrors that of Waterhouse-Friderichsen syndrome (WFS), and bilateral adrenal hemorrhage may be found at autopsy[25,26]. The mechanism that connects splenectomy to WFS is unknown but the possible causes of OPSI include loss of splenic phagocytic function, decreasing serum immunoglobulin levels, suppression of lymphocyte sensitivity, or a change in the opsonin system[27,28].
Table 1.
Clinical features of overwhelming postsplenectomy infection
| Cryptic infection (no obvious focus) |
| Short, nonspecific prodrome |
| Massive bacteremia with encapsulated organism |
| Septic shock with disseminated intravascular coagulation |
| Marked virulence: 50% to 70% mortality |
| Death ensues in 24 to 48 h |
Overwhelming postsplenectomy infection had been defined as septicemia and/or meningitis, usually fulminant but not necessarily fatal, and occurring at any time after removal of the spleen.
Risk factors
Splenectomized patients are at risk of life-threatening sepsis. Major factors for stratifying risk include the age at which splenectomy occurs, the subsequent time interval from splenectomy, the reason for splenectomy, and the overall immune status of the patient REF.
Infants do not acquire specific antibodies against encapsulated organisms until relatively late in the development of antibody responses. Although OPSI can occur at any age, children are therefore at greater risk of developing the condition, especially those under the age of 2 years[29,30]. However, estimates of the incidence and timing of OPSI vary widely in the literature, and some authors report the greatest risk of developing OPSI in the first two years after splenectomy[31]. Recent reports recommended that all asplenic patients should receive optimal advice and protection against OPSI regardless of the underlying etiology, based on evidence that the increased risk of severe sepsis after splenectomy is lifelong[32,33].
Splenectomy performed for a hematological disorder, including thalassemia, hereditary spherocytosis, auto-immune hemolysis, immune thrombocytopenic purpura, or lymphoma, appears to carry a higher risk than splenectomy performed as a result of trauma[34,35]. In addition, patients with hematological and autoimmune disorders, or lymphoma show impaired immunity, and patients undergoing treatment such as chemotherapy often show decreased serum immunoglobulin levels; both groups may therefore have an increased susceptibility for OPSI.
Hyposplenism occurs when splenic functions are reduced by disease or are absent congenitally or after splenectomy. Howell-Jolly bodies are small, round remnants of the original erythrocyte nucleus. Increased numbers of Howell-Jolly bodies in a peripheral blood smear, although not overly sensitive, can identify the degree of hyposplenism that presents a risk for developing OPSI[2,19,36].
Infecting organisms in OPSI
Outside the splenic circulation, polysaccharide antigens are poorly immunogenic in comparison with protein antigens. This contributes to polysaccharide-coated bacteria evading the immune response and subsequent phagocytosis[28]. Host defenses against bacteria are therefore critically dependent on humoral immunity and production of type-specific antibodies. While liver Kupffer cells clear most well-opsonized bacteria, encapsulated organisms resist antibody binding and are primarily removed by the spleen. Sepsis in asplenic patients can occur with any organism, be it bacteria, virus, fungus, or protozoan, however encapsulated organisms are frequently associated with sepsis in splenectomized patients. Encapsulated organisms such as Streptococcus pneumoniae are particularly resistant to phagocytosis, but is quickly overcome in the presence of even a small amount of type-specific antibody[24,37]. Without the spleen, prompt antibody production against a newly encountered antigen is impaired and bacteria proliferate rapidly. Therefore, the risk of invasive pneumococcal disease in patients without a spleen is 12-25 times greater than that in the population at large[38,39]. Invasive disease in the asplenic patient due to such encapsulated organisms as Streptcoccus pneumoniae (50%-90%), Neisseria meningitides, Hemophilus influenzae, and Streptococcus pyogens (25%) leads to uninhibited bacterial overgrowth[24,29,33,37].
Prevention of OPSI
Treatment of OPSI is generally aggressive due to the serious nature of the condition and associated mortality. Comprising intravenous fluids, antibiotics, vasopressors, steroids, heparin, packed red blood cells, platelets, cryoprecipitates, and fresh frozen plasma, it may fail to alter the course of this fulminant septic syndrome[25].Therefore, prevention of OPSI is extremely important for immunocompromised patients who have undergone splenectomy.
Preventive strategies including vaccination and education are also important for splenectomized patients. Functionally or anatomically asplenic patients are at increased risk of infection from encapsulated organisms compared to the general population. Vaccines available for the most common organisms include the 23-valent pneumococcal polysaccharide vaccine, a 7-valent protein-conjugated pneumococcal vaccine, the Hemophilus influenzae type B vaccine, and the meningococcal vaccine[28]. The polysaccharide-based pneumococcal vaccine is recommended for all adults at increased risk of pneumococcal infection, and particularly the asplenic patients[40]. The Centers for Disease Control and Prevention in the US (revaccination every 6 years) and the British Committee for Standards in Haematology (revaccination every 5-10 years) recommended revaccination for the prevention of OPSI, at the same time emphasizing the rather frequent need for shorter intervals between revaccinations to keep antibody concentrations at a level sufficient by probability to confer protection[41,42].Unfortunately, fatal pneumococcal sepsis has been reported in asplenic, vaccinated patients. It remains advisable, nevertheless, to offer splenectomized patients protection due to their increased risk of developing severe disease and because the vaccine itself poses minimal risk. Jockovich[43] reported no OPSI among patients vaccinated before splenectomy; however, 10.4% of patients who did not receive vaccination developed OPSI. In addition, 5% of patients who were given vaccination after splenectomy developed OPSI. For elective splenectomy, the vaccine should be given at least 2 wk before surgery[43,44].
Finally, patient education represents a mandatory strategy for preventing OPSI. Studies have shown that from 11% to 50% of splenectomized patients remain unaware of their increased risk for serious infection or the appropriate health precautions that should be undertaken[45,46]. Patients should understand the potential severity of OPSI and the possibility of rapid progression. Physicians should inform any new healthcare professionals, including dentists, of asplenic status. In particular, the presence of increased Howell-Jolly bodies on a peripheral blood smear should be highlighted on the laboratory report to inform the patients’ physicians of possible hyposplenism[2,19,36], This information and its significance should be in turn relayed to the patient. Moreover, advice for asplenic individuals to be issued with a form of medical alert, such as a card or a bracelet, has two purposes. First, it should provide a constant reminder to the individual of their condition and, second, knowledge of their state might be vital for medical attendants in the event of a medical emergency. This aspect of patient management needs increased attention as only one patient was found to hold such a card. The possibility that OPSI episodes in asplenic patients may have been avoided with improved knowledge cannot be excluded[5].
Future directions
HCV is a major public health problem and a leading cause of chronic liver disease. Various studies have suggested that 3%-20% of chronically infected patients will develop cirrhosis over a 20-year period, and are at significant risk of developing hepatocellular carcinoma[47]. Recent therapeutic trials in well-defined, selected populations revealed that combinations of interferons and ribavirin are more effective than monotherapy for HCV treatment. Moreover, trials of pegylated interferons yielded improved sustained virus response rates with similar toxicity profiles. As with all clinical decisions, selection of patients for HCV treatment requires an accurate assessment of therapeutic risk vs benefit, a determination that is complicated by exclusion from registration trials of persons with conditions that might increase risk and diminish benefit. Application of these principles to individual patients can be challenging, and the relative strength of recommendation of treatment varies accordingly. However, HCV is also a possible cause of chronic thrombocytopenia in these patients, by a mechanism that remains unclear. Moreover, treatment for HCV often leads to anemia, neutropenia, and thrombocytopenia. These conditions prevent safe application of treatment in patients with baseline pancytopenia, due to the cirrhosis-related hypersplenism[14]. The various treatments used, including steroids and intravenous immunoglobulin, have generally produced only transient responses[48,49]. Nevertheless, partial splenic embolization and laparoscopic splenectomy may enable anti-HCV therapy to be given. Recently, Hayashi et al[14] reported that splenectomy for severe thrombocytopenia with the intent to apply interferon therapy can be beneficial. It is therefore feasible that splenectomy prior to anti-HCV treatment for HCV-related chronic thrombocytopenia will occur more frequently in the near future. In addition, physicians should follow the occurrence of OPSI in these patients not only during the treatment for HCV clearance but also for the entire follow-up period.
CONCLUSION
The spleen is crucial to the host response to infection by clearing polysaccharide-encapsulated bacteria. This response involves the clearing of pathogens from the bloodstream as well as the rapid production of specific antigens. Splenectomy results in an increased risk of septic complications associated with a high mortality rate, the most serious being the development of OPSI. Nonspecific symptoms, including nausea, vomiting, fever, and unconsiousness, followed by a rapid progression to coma and shock characterizes OPSI, and it is treated aggressively.
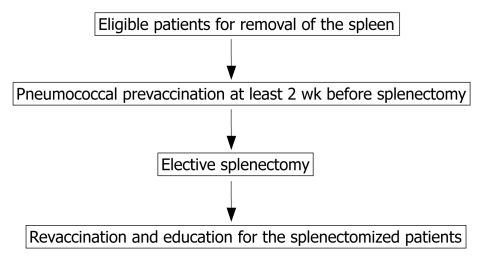
Eradication of HCV with the recently introduced therapy of pegylated interferon and ribavirin would be particularly beneficial in those with advanced liver fibrosis or cirrhosis. Splenectomy might be useful also to raise platelet counts so that pegylated interferon-based therapy can be performed safely in patients with cirrhosis due to HCV. Prevention strategies such as vaccination and education are also potentially important parts of the strategy for splenectomized HCV patients (Figure 1). Finally, reduction of the immune response in patients with chronic liver disease and/or PEM necessitates careful follow up of splenectomized patients with chronic liver disease to monitor the appearance of OPSI.
Figure 1.
A proposed prevention strategy for splenectomized patients in management algorithm.
Footnotes
S- Editor Ma N L- Editor Negro F E- Editor Lu W
References
- 1.Hansen K, Singer DB. Asplenic-hyposplenic overwhelming sepsis: postsplenectomy sepsis revisited. Pediatr Dev Pathol. 2001;4:105–121. doi: 10.1007/s100240010145. [DOI] [PubMed] [Google Scholar]
- 2.Styrt B. Infection associated with asplenia: risks, mechanisms, and prevention. Am J Med. 1990;88(5N):33N–42N. [PubMed] [Google Scholar]
- 3.Lortan JE. Management of asplenic patients. Br J Haematol. 1993;84:566–569. doi: 10.1111/j.1365-2141.1993.tb03128.x. [DOI] [PubMed] [Google Scholar]
- 4.Cullingford GL, Watkins DN, Watts AD, Mallon DF. Severe late postsplenectomy infection. Br J Surg. 1991;78:716–721. doi: 10.1002/bjs.1800780626. [DOI] [PubMed] [Google Scholar]
- 5.Waghorn DJ. Overwhelming infection in asplenic patients: current best practice preventive measures are not being followed. J Clin Pathol. 2001;54:214–218. doi: 10.1136/jcp.54.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brigden ML, Pattullo AL. Prevention and management of overwhelming postsplenectomy infection--an update. Crit Care Med. 1999;27:836–842. doi: 10.1097/00003246-199904000-00050. [DOI] [PubMed] [Google Scholar]
- 7.Strader DB, Wright T, Thomas DL, Seeff LB. Diagnosis, management, and treatment of hepatitis C. Hepatology. 2004;39:1147–1171. doi: 10.1002/hep.20119. [DOI] [PubMed] [Google Scholar]
- 8.Mondelli MU, Silini E. Clinical significance of hepatitis C virus genotypes. J Hepatol. 1999;31 Suppl 1:65–70. doi: 10.1016/s0168-8278(99)80377-8. [DOI] [PubMed] [Google Scholar]
- 9.Pawlotsky JM, Bouvier M, Fromont P, Deforges L, Duval J, Dhumeaux D, Bierling P. Hepatitis C virus infection and autoimmune thrombocytopenic purpura. J Hepatol. 1995;23:635–639. doi: 10.1016/0168-8278(95)80027-1. [DOI] [PubMed] [Google Scholar]
- 10.Bauduer F, Marty F, Larrouy M, Ducout L. Immunologic thrombocytopenic purpura as presenting symptom of hepatitis C infection. Am J Hematol. 1998;57:338–340. doi: 10.1002/(sici)1096-8652(199804)57:4<338::aid-ajh12>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 11.Rios R, Sangro B, Herrero I, Quiroga J, Prieto J. The role of thrombopoietin in the thrombocytopenia of patients with liver cirrhosis. Am J Gastroenterol. 2005;100:1311–1316. doi: 10.1111/j.1572-0241.2005.41543.x. [DOI] [PubMed] [Google Scholar]
- 12.Kercher KW, Carbonell AM, Heniford BT, Matthews BD, Cunningham DM, Reindollar RW. Laparoscopic splenectomy reverses thrombocytopenia in patients with hepatitis C cirrhosis and portal hypertension. J Gastrointest Surg. 2004;8:120–126. doi: 10.1016/j.gassur.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Sangro B, Bilbao I, Herrero I, Corella C, Longo J, Beloqui O, Ruiz J, Zozaya JM, Quiroga J, Prieto J. Partial splenic embolization for the treatment of hypersplenism in cirrhosis. Hepatology. 1993;18:309–314. [PubMed] [Google Scholar]
- 14.Hayashi PH, Mehia C, Joachim Reimers H, Solomon HS, Bacon BR. Splenectomy for thrombocytopenia in patients with hepatitis C cirrhosis. J Clin Gastroenterol. 2006;40:740–744. doi: 10.1097/00004836-200609000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Alberino F, Gatta A, Amodio P, Merkel C, Di Pascoli L, Boffo G, Caregaro L. Nutrition and survival in patients with liver cirrhosis. Nutrition. 2001;17:445–450. doi: 10.1016/s0899-9007(01)00521-4. [DOI] [PubMed] [Google Scholar]
- 16.Tajika M, Kato M, Mohri H, Miwa Y, Kato T, Ohnishi H, Moriwaki H. Prognostic value of energy metabolism in patients with viral liver cirrhosis. Nutrition. 2002;18:229–234. doi: 10.1016/s0899-9007(01)00754-7. [DOI] [PubMed] [Google Scholar]
- 17.Moriwaki H, Miwa Y, Tajika M, Kato M, Fukushima H, Shiraki M. Branched-chain amino acids as a protein- and energy-source in liver cirrhosis. Biochem Biophys Res Commun. 2004;313:405–409. doi: 10.1016/j.bbrc.2003.07.016. [DOI] [PubMed] [Google Scholar]
- 18.King H, Shumacker HB Jr. Splenic studies. I. Susceptibility to infection after splenectomy performed in infancy. Ann Surg. 1952;136:239–242. doi: 10.1097/00000658-195208000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brigden ML. Overwhelming postsplenectomy infection still a problem. West J Med. 1992;157:440–443. [PMC free article] [PubMed] [Google Scholar]
- 20.Chaikof EL, McCabe CJ. Fatal overwhelming postsplenectomy infection. Am J Surg. 1985;149:534–539. doi: 10.1016/s0002-9610(85)80052-0. [DOI] [PubMed] [Google Scholar]
- 21.Leonard AS, Giebink GS, Baesl TJ, Krivit W. The overwhelming postsplenectomy sepsis problem. World J Surg. 1980;4:423–432. doi: 10.1007/BF02393164. [DOI] [PubMed] [Google Scholar]
- 22.Lynch AM, Kapila R. Overwhelming postsplenectomy infection. Infect Dis Clin North Am. 1996;10:693–707. doi: 10.1016/s0891-5520(05)70322-6. [DOI] [PubMed] [Google Scholar]
- 23.Green JB, Shackford SR, Sise MJ, Fridlund P. Late septic complications in adults following splenectomy for trauma: a prospective analysis in 144 patients. J Trauma. 1986;26:999–1004. doi: 10.1097/00005373-198611000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Davidson RN, Wall RA. Prevention and management of infections in patients without a spleen. Clin Microbiol Infect. 2001;7:657–660. doi: 10.1046/j.1198-743x.2001.00355.x. [DOI] [PubMed] [Google Scholar]
- 25.Guidelines for the prevention and treatment of infection in patients with an absent or dysfunctional spleen. Working Party of the British Committee for Standards in Haematology Clinical Haematology Task Force. BMJ. 1996;312:430–434. doi: 10.1136/bmj.312.7028.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bouros D, Nicholson AC, Polychronopoulos V, du Bois RM. Acute interstitial pneumonia. Eur Respir J. 2000;15:412–418. doi: 10.1034/j.1399-3003.2000.15b31.x. [DOI] [PubMed] [Google Scholar]
- 27.Machesky KK, Cushing RD. Overwhelming postsplenectomy infection in a patient with penicillin-resistant Streptococcus pneumoniae. Arch Fam Med. 1998;7:178–180. doi: 10.1001/archfami.7.2.178. [DOI] [PubMed] [Google Scholar]
- 28.Shatz DV. Vaccination considerations in the asplenic patient. Expert Rev Vaccines. 2005;4:27–34. doi: 10.1586/14760584.4.1.27. [DOI] [PubMed] [Google Scholar]
- 29.Singer DB. Postsplenectomy sepsis. Perspect Pediatr Pathol. 1973;1:285–311. [PubMed] [Google Scholar]
- 30.Walker W. Splenectomy in childhood: a review in England and Wales, 1960-1964. Br J Surg. 1976;63:36–43. doi: 10.1002/bjs.1800630109. [DOI] [PubMed] [Google Scholar]
- 31.Di Cataldo A, Puleo S, Li Destri G, Racalbuto A, Trombatore G, Latteri F, Rodolico G. Splenic trauma and overwhelming postsplenectomy infection. Br J Surg. 1987;74:343–345. doi: 10.1002/bjs.1800740504. [DOI] [PubMed] [Google Scholar]
- 32.Stryker RM, Orton DW. Overwhelming postsplenectomy infection. Ann Emerg Med. 1988;17:161–164. doi: 10.1016/s0196-0644(88)80304-4. [DOI] [PubMed] [Google Scholar]
- 33.White BP, Aanning HL. Overwhelming postsplenectomy sepsis twenty-two years after operation risks management and prevention. S D J Med. 1991;44:317–320. [PubMed] [Google Scholar]
- 34.Weintraub LR. Splenectomy: who, when, and why? Hosp Pract (Off Ed) 1994;29:27–34. doi: 10.1080/21548331.1994.11443030. [DOI] [PubMed] [Google Scholar]
- 35.Curti AJ, Lin JH, Szabo K. Overwhelming post-splenectomy infection with Plesiomonas shigelloides in a patient cured of Hodgkin's disease. A case report. Am J Clin Pathol. 1985;83:522–524. doi: 10.1093/ajcp/83.4.522. [DOI] [PubMed] [Google Scholar]
- 36.Doll DC, List AF, Yarbro JW. Functional hyposplenism. South Med J. 1987;80:999–1006. doi: 10.1097/00007611-198708000-00016. [DOI] [PubMed] [Google Scholar]
- 37.Williams DN, Kaur B. Postsplenectomy care. Strategies to decrease the risk of infection. Postgrad Med. 1996;100:195–198, 201, 205. doi: 10.3810/pgm.1996.07.16. [DOI] [PubMed] [Google Scholar]
- 38.Cullingford GL, Watkins DN, Watts AD, Mallon DF. Severe late postsplenectomy infection. Br J Surg. 1991;78:716–721. doi: 10.1002/bjs.1800780626. [DOI] [PubMed] [Google Scholar]
- 39.Aavitsland P, Froholm LO, Hoiby EA, Lystad A. Risk of pneumococcal disease in individuals without a spleen. Lancet. 1994;344:1504. doi: 10.1016/s0140-6736(94)90321-2. [DOI] [PubMed] [Google Scholar]
- 40.Musher DM, Ceasar H, Kojic EM, Musher BL, Gathe JC Jr, Romero-Steiner S, White AC Jr. Administration of protein-conjugate pneumococcal vaccine to patients who have invasive disease after splenectomy despite their having received 23-valent pneumococcal polysaccharide vaccine. J Infect Dis. 2005;191:1063–1067. doi: 10.1086/428135. [DOI] [PubMed] [Google Scholar]
- 41.Whitney CG. Preventing pneumococcal disease. ACIP recommends pneumococcal polysaccharide vaccine for all adults age > or = 65. Geriatrics. 2003;58:20–22, 25. [PubMed] [Google Scholar]
- 42.Davies JM, Barnes R, Milligan D. Update of guidelines for the prevention and treatment of infection in patients with an absent or dysfunctional spleen. Clin Med. 2002;2:440–443. doi: 10.7861/clinmedicine.2-5-440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jockovich M, Mendenhall NP, Sombeck MD, Talbert JL, Copeland EM 3rd, Bland KI. Long-term complications of laparotomy in Hodgkin's disease. Ann Surg. 1994;219:615–621; discussion 621-624. doi: 10.1097/00000658-199406000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Landgren O, Bjorkholm M, Konradsen HB, Soderqvist M, Nilsson B, Gustavsson A, Axdorph U, Kalin M, Grimfors G. A prospective study on antibody response to repeated vaccinations with pneumococcal capsular polysaccharide in splenectomized individuals with special reference to Hodgkin’s lymphoma. J Intern Med. 2004;255:664–673. doi: 10.1111/j.1365-2796.2004.01312.x. [DOI] [PubMed] [Google Scholar]
- 45.White KS, Covington D, Churchill P, Maxwell JG, Norman KS, Clancy TV. Patient awareness of health precautions after splenectomy. Am J Infect Control. 1991;19:36–41. doi: 10.1016/0196-6553(91)90158-9. [DOI] [PubMed] [Google Scholar]
- 46.Kinnersley P, Wilkinson CE, Srinivasan J. Pneumococcal vaccination after splenectomy: survey of hospital and primary care records. BMJ. 1993;307:1398–1399. doi: 10.1136/bmj.307.6916.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McKiernan SM, Hagan R, Curry M, McDonald GS, Kelly A, Nolan N, Walsh A, Hegarty J, Lawlor E, Kelleher D. Distinct MHC class I and II alleles are associated with hepatitis C viral clearance, originating from a single source. Hepatology. 2004;40:108–114. doi: 10.1002/hep.20261. [DOI] [PubMed] [Google Scholar]
- 48.Durand JM, Cretel E, Retornaz F, Lefevre P, Kaplanski G, Soubeyrand J. Alpha interferon therapy in thrombocytopenia associated with hepatitis C virus infection. J Hepatol. 1994;21:277–278. doi: 10.1016/s0168-8278(05)80409-x. [DOI] [PubMed] [Google Scholar]
- 49.Garcia-Suarez J, Burgaleta C, Hernanz N, Albarran F, Tobaruela P, Alvarez-Mon M. HCV-associated thrombocytopenia: clinical characteristics and platelet response after recombinant alpha2b-interferon therapy. Br J Haematol. 2000;110:98–103. doi: 10.1046/j.1365-2141.2000.02132.x. [DOI] [PubMed] [Google Scholar]