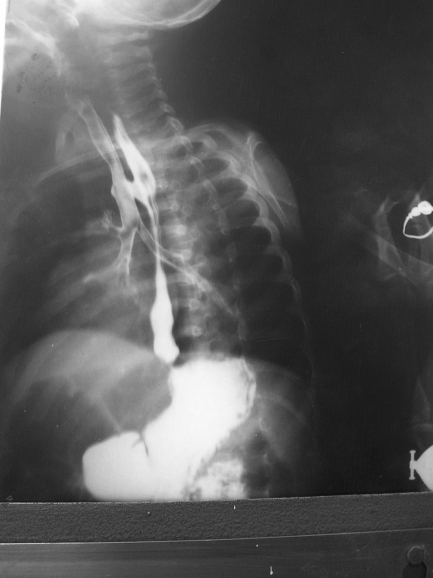
H‐type fistula is a rare, isolated form of tracheo‐oesophageal fistula (TEF). A 9‐month‐old girl presented with paroxysms of persistent cough related to feeds. Repeated hospitalisations, empirical antibiotics, antitubercular treatment and various investigations failed to resolve her symptoms. A barium swallow confirmed an H‐type TEF (fig 1). Thoracoscopic repair was attempted, but cardiorespiratory compromise owing to leakage of tracheal air into the oesophagus through the large defect during anaesthesia prompted us to repair the defect through thoracotomy. Postoperative recovery was uneventful.
Figure 1 Barium oesophagogram showing wide H‐type tracheo‐oesophageal fistula at the T2/T3 level; such a clear fistulous connection is rarely seen.
Congenital isolated TEF (H‐type) is a rare disorder posing diagnostic and management problems.1 N‐type TEF is more frequent than H‐type, owing to the oblique angle of the fistula from the trachea (carina or main bronchi) to the oesophagus, anatomically at the level of the neck root (C7–T1). Pressure changes between both structures can cause entry of air into the oesophagus, or entry of oesophageal content into the trachea. Clinical manifestations—cyanosis, cough and choking with feeding, recurrent chest infections and persistent gastrointestinal distension—are related to the presence of the fistulous connection. Diagnosis is confirmed with oesophagogram or an video‐oesophagogram. In our case, the oesophagogram was so clear that we were prompted to report it. Failure to identify an H‐type TEF, an unsatisfactory radiological method and similar symptoms related to associated anomalies may cause delay in diagnosis and lead to fatality.1,2 If there is a doubt about the radiograph, bronchoscopy and simultaneous administration of methylene blue should be the next diagnostic step.1,3 Any delay in surgery is generally due to delay in diagnosis rather than delay in presentation.
Footnotes
Competing interests: None declared.
References
- 1.Karnak I, Senocak M E, Hicsonmez A.et al The diagnosis and treatment of H‐type tracheoesophageal fistula. J Pediatr Surg 1997321670–1674. [DOI] [PubMed] [Google Scholar]
- 2.Hosono S, Fuyama Y, Ohno T.et al Sudden intractable respiratory failure in extremely low birth weight infants with H‐type tracheoesophageal fistula. J Perinat Med 200230265–268. [DOI] [PubMed] [Google Scholar]
- 3.Pigna A, Gentili A, Landuzzi V.et al Bronchoscopy in newborns with esophageal atresia. Pediatr Med Chir 200224297–301. [PubMed] [Google Scholar]