Abstract
Background
Since 1992, infants with progressive posthaemorrhagic ventricular dilatation (PHVD) have been treated in the Neonatal Intensive Care Unit, Wilhelmina Children's Hospital, Utrecht, The Netherlands, with a ventricular reservoir.
Objective
To retrospectively study the incidence of infection using this invasive procedure.
Methods
Between January 1992 and December 2003, 76 preterm infants were treated with a ventricular reservoir. Infants admitted during two subsequent periods were analysed: group 1 included infants admitted during 1992–7 (n = 26) and group 2 those admitted during 1998–2003 (n = 50). Clinical characteristics and number of reservoir punctures were evaluated. The incidence of complications over time was assessed, with a focus on the occurrence of infection of the reservoir.
Results
The number of punctures did not change during both periods. Infection was significantly less common during the second period (4% (2/50) v 19.2% (5/26), p = 0.029).
Conclusion
The use of a ventricular reservoir is a safe treatment to ensure adequate removal of cerebrospinal fluid in preterm infants with PHVD. In experienced hands, the incidence of infection of the ventricular reservoir or major complications remains within acceptable limits.
Germinal matrix—intraventricular haemorrhages (GMH‐IVHs) in the neonatal period are an important clinical problem. Although the incidence of IVH has decreased over the past decade, it is still a common problem in the very low birthweight infant.1
About 30–50% of infants with an IVH develop post‐haemorrhagic ventricular dilatation (PHVD); the more severe the GMH‐IVH, the higher the risk of developing PHVD.2,3,4 PHVD usually develops within 10–20 days after the onset of GMH‐IVH. Ventricular dilatation, seen using cranial ultrasonography, precedes the development of clinical symptoms by days or even weeks. The clinical signs are a full fontanelle, diastases of the structures and a rapid increase in head circumference. Once it has been recognised that the ventricles are enlarged, frequent assessments by ultrasonography are mandatory. The most widely adopted measurement system is that of Levene and Starte, which measures the ventricular width.5 Another measurement that is increasingly being used is the anterior horn width.6 Repeated lumbar or ventricular punctures have been proved to be ineffective in the treatment of PHVD.7 Others therefore choose to use an external drain or a subcutaneous reservoir.7
The aim of the present study was to retrospectively assess the incidence of infections of ventricular reservoirs in the treatment of PHVD in preterm infants.
Patients and methods
Patients
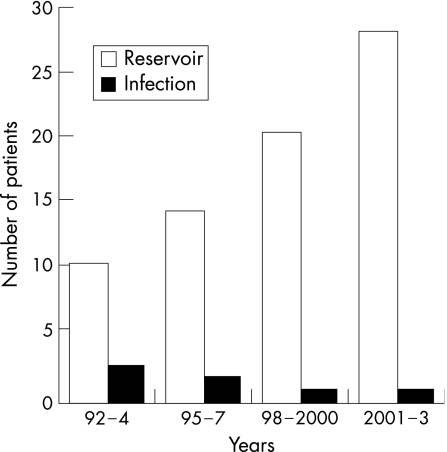
Between January 1992 and December 2003, a total of 76 preterm infants with a ventricular reservoir were studied. We specifically looked at the incidence of infection of the reservoir in these children. We compared two periods: 1992–7 (group 1, n = 26) and 1998–2003 (group 2, n = 50). The period of 12 years was divided into two periods of 6 years to examine whether there were any significant differences over time. We started this treatment policy in 1992 and gained a great deal of experience over the years. Owing to an increased number of referrals for this procedure,which is performed in only 4 of the 10 Dutch neonatal intensive care units, the number of infants in the second period is twice that in the first 6‐year period (fig 1).
Figure 1 Incidence of infection of the reservoir in children between 1992 and 2003.
The notes were reviewed for the clinical characteristics and the number of punctures from the reservoir. Data regarding the total number of punctures were missing for five children, because of incomplete (administrative) data. Clinical characteristics, the number of punctures and the occurrence of infection were compared between the two groups.
Informed parental consent was obtained from the parents before insertion of the reservoir.
PHVD treatment
The policy in the Neonatal Intensive Care Unit, Wilhelmina Children's Hospital, Utrecht, The Netherlands, is to carry out lumbar punctures in those infants who develop PHVD, especially when there is a rapid progression of the ventricular size usually associated with a change in anterior horn width, leading to a change in ventricular shape—the so‐called “ballooning”, both changes suggestive of raised pressure in the ventricular system. If PHVD is not stabilised in the following 5–10 days despite daily lumbar punctures, or when lumbar punctures are not successful, a ventricular reservoir is inserted by the paediatric neurosurgeon8 to enable further control of the intracranial pressure. In our unit, this treatment is often combined with the administration of isosorbide (8 g/kg/day in six doses), an osmotic diuretic that reduces the production of cerebrospinal fluid (CSF).
Ventricular reservoir
During the whole study period, prophylactic intravenous vancomycin was given to all infants for a period of 48 h, and the first dose was given 1 h before placement of the reservoir. A strict sterile procedure was followed during the puncture by the reservoir: sterile gloves, mask and hood, sterile gown and sterile materials. The extent of PHVD was assessed on the basis of a daily ultrasound examination, and it was decided how often and how much CSF needed to be removed. Routinely, we start with withdrawal of 10 ml/kg CSF, divided over two taps. The amount of CSF removed is adjusted every day according to the ultrasound findings. CSF is removed at a rate of 1 ml/min to reduce the risk of rebleeding. The ventricular reservoir is not removed when tapping is no longer required, as the surgical removal of the reservoir is an extra procedure that can give rise to complications such as leakage of CSF.
Furthermore, the reservoir can be used for evaluation of the intracranial pressure in case of delayed symptoms of slowly progressive ventricular dilatation.
Routinely, the CSF was analysed for red cells, white cells, and total protein and glucose, and one CSF culture was undertaken per day. Diagnosis of infection was based on a positive CSF culture. Clinical symptoms of infection were observed.
When a ventricular reservoir infection was diagnosed, treatment with intravenous vancomycin in combination with other antibiotics (amikacine or ceftazidim) was started until the causative microorganism was identified. Thereafter, the antibiotic treatment was based on the resistance pattern of the causative microorganism.
Statistics
Differences between the groups for all variables were tested by Student's t test, Mann–Whitney U test, χ2 test and Cross tabs where appropriate. Data were statistically analysed using SPSS V.11.5 for Windows. Significance was set at p = 0.05.
Results
From 1992 to 2003, 76 preterm infants had an intraventricular reservoir inserted for treatment of their PHVD. The clinical characteristics, gestational age, birth weight, Apgar score and the male:female ratio (table 1) between the two groups were comparable, as was the number of days of inserting the reservoir and the total number of punctures.
Table 1 Clinical characteristics of the study population.
| Group 1(n = 26) | Group 2(n = 50) | |
|---|---|---|
| Male:female | 12:14 | 24:26 |
| Gestational age, weeks | 30.2 (2.8) | 30.2 (2.9) |
| Birth weight, g | 1465 (615) | 1480 (540) |
| Apgar score at 1 min, | 5 (1–9) | 6 (1–10) |
| Apgar score at 5 min, | 8 (4–10) | 8 (5–10) |
| Number of punctures | 23 (6–126) | 22 (5–117) |
| Day of placement of reservoir | 15 (1–49) | 15 (1–86) |
Values are mean (SD) or median (range) as appropriate.
Infection occurred in 5 of the 26 (19.2%) infants from group 1 and in 2 of the 50 (4%) infants from group 2 (fig 1). We found a significant decrease in the number of infants who developed an infection of the reservoir in group 2 compared with that in group 1 (p = 0.029). In five of these seven infants, Staphylococcus epidermidis was cultured from the CSF sampled from the reservoir. The reservoir was not removed. After identification of S epidermidis, vancomycin was given intravenously to all infants for 9–16 days. In two infants, Candida albicans was cultured from the CSF sampled from the reservoir. The reservoir was immediately removed, and both infants were given intravenous fluconazole for 16–24 days.
CSF analysis, carried out at the time of diagnosis of infection, showed pleocytosis in only two infants, 160×106/l and 167×106/l, respectively. None of the seven infants developed clinical symptoms of an infection.
We found no relationship between the number of punctures and the occurrence of an infection (p = 0.093); also, there was a wide range of the number of punctures (5–126).
In addition to infections, the ventricular reservoir had to be removed in 3 of 26 infants from group 1 and in 1 of 50 infants from group 2. Revision of the reservoir was necessary in one patient from group 1 and in four infants from group 2. Placement of a second reservoir, due to lack of communication of the lateral ventricles, was required in one patient from each group. Dehiscence of the wound occurred in one patient from group 1 and in two patients from group 2. We found no significant difference in the occurrence of these problems in both groups (p = 0.504).
In all, 34 of 76 (44.7%) infants required a ventriculoperitoneal drain: 12 of 26 (46%) from group 1 and 22 of 50 (44%) from group 2. We found no significant difference between the groups regarding the number of infants who required a permanent ventriculoperitoneal drain (p = 0.858).
Discussion
In this retrospective study, we looked at the incidence of infections of ventricular reservoirs in preterm infants. The number of infants with an infection of the reservoir decreased considerably over the two 6‐year periods. This marked decrease could be due to several factors. Firstly, we gained a great deal of experience over the years in the removal of CSF using a subcutaneous reservoir. As soon as there was any regrowth of hair, the hair was removed by carefully shaving the area around the reservoir, which was the practice every fortnight. In the second period (1998–2003), we were more careful to prevent the presence of hair in this area. After the operation, a transparent dressing (Tegaderm, 3M Health Care) was put over the wound and the reservoir, which was not removed before the puncture in period 1 as opposed to the procedure in the second period. Secondly, in period 1 children were nursed in an open incubator or cradle, whereas in period 2 they remained in a closed incubator or in a hooded cradle to reduce exposure and excessive handling. Neither the technique of the puncture itself—cleaning the reservoir area before the puncture with iodine (Bethadine, Mandipharma, Basel/Switzerland) leaving it there for at least 1 min, cleaning the reservoir area after the puncture with 70% alcohol, covering the puncture area with a sterile gauze afterwards—nor the use of antibiotics has been changed. Since 1992, prophylactic vancomycin is given intravenously for 48 h.
What is already known on this topic
Limited data are available on the use of ventricular reservoirs.
In two previous studies, the incidence of infection of ventricular reservoirs has been reported to be 8% and 21%.
What this study adds
Ventricular reservoirs are a safe and effective method to ensure controlled removal of cerebrospinal fluid in preterm infants with post‐haemorrhagic ventricular dilatation.
In experienced hands, the incidence of an infection or major complications remains within acceptable limits.
One of the major risks of a ventricular reservoir is the occurrence of an infection. Invasive punctures will be carried out over a prolonged period, usually twice a day, sometimes even three times a day. This should be carried out under conditions of utmost sterility, as in general these patients are vulnerable to infections because of their underdeveloped immune system.5 Monitoring the occurrence of microorganisms in the CSF by undertaking a CSF culture every day is of great importance. The lack of clinical signs of infection in our infants was of interest, and probably a result of early detection of the infection. In this study, it was clearly shown that the risk of infection could be as low as 4% as long as strict precautions were taken.
In treating infants with PHVD, it is important to protect the brain from additional damage secondary to raised intracranial pressure and to minimise the need for a permanent shunt, with the complications of infection and blockage requiring multiple revisions.3,9 Therefore, the policy in our unit is to assess the degree of PHVD on a regular basis using cranial ultrasonography. If PHVD is not stabilised over 5–10 days despite lumbar punctures, a reservoir is placed.
We have no experience in the treatment of PHVD with intraventricular streptokinase. Previous studies10,11 have shown that the use of streptokinase is not recommended. Neither do we use isosorbide as monotherapy; its administration is always in combination with CSF removal, because the use of only diuretics has proved to be ineffective.12 The initial drainage fibrinolytic therapy using two intraventricular catheters to flush the ventricular system had an infection rate of 8%.3 No data are available about the associated risk of infection in the ongoing prospective Drainage Irrigation and Fibrinolytic Trail (DRIFT).3
To the best of our knowledge, data on the incidence of infections of ventricular reservoirs are limited. Hudgins et al2 found an infection rate of 8% and a revision rate of 20%. More recently, Richard et al showed an infection in 21% of the children, which increased during their study period.13 In contrast with their data, our incidence of infection of the ventricular reservoir is decreasing.
Recent data from Persson et al14 show a decrease in the prevalence of infantile hydrocephalus to 6 in 1000 live births at ⩽32 weeks gestation, with a high rate of cerebral palsy (88%) seen among the survivors. Early intervention of PHVD may help to prevent development of infantile hydrocephalus and its cerebral complications. In The Netherlands, a multicentre investigation has started 2006 to study the effect of early versus later insertion of the ventricular reservoir, as recommended in a previous retrospective study.15
Conclusion
Ventricular reservoirs are a safe and effective method to ensure controlled CSF removal in preterm infants with PHVD. In experienced hands, the incidence of an infection or major complications remains within acceptable limits.
Abbreviations
CSF - cerebrospinal fluid
GMH‐IVH - germinal matrix—intraventricular haemorrhages
PHVD - post‐haemorrhagic ventricular dilatation
Footnotes
Competing interests: None declared.
References
- 1.Volpe J J. Intracranial hemorrhage germinal matrix–intraventricular hemorrhage of the premature infant. In: Volpe JJ, ed. Neurology of the newborn, 4th edn. Philadelphia: Saunders, 2001428–493.
- 2.Hudgins R J, Boydston W R, Gilreath C L. Treatment of posthemorrhagic hydrocephalus in the preterm infant with a ventricular access device. Pediatr Neurosurg 199829309–313. [DOI] [PubMed] [Google Scholar]
- 3.Whitelaw A, Cherian S, Thoresen M.et al Posthaemorrhagic ventricular dilatation: new mechanics and new treatment. Acta Paediatr Suppl 200444411–14. [DOI] [PubMed] [Google Scholar]
- 4.Murphy B P, Inder T E, Rooks V.et al Posthaemorrhagic ventricular dilatation in the preterm infant: natural history and predictors of outcome. Arch Dis Child Fetal Neonatal Ed 200287F37–F41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levene M I, Starte D R. A longitudinal study of post‐haemorrhagic ventricular dilatation in the newborn. Arch Dis Child 198156905–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davies M W, Swaminathan M, Chuang S L.et al Reference ranges for the linear dimensions of the intracranial ventricles in preterm neonates. Arch Dis Child Fetal Neonatal Ed 200082F218–F223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whitelaw A. Repeated lumbar or ventricular punctures in newborns with intraventricular haemorrhage. Cochrane Database Syst Rev 20011CD000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Vries L S, Groenendaal F, Gooskens R.et al Unilateral posthaemorrhagic hydrocephalus in the neonatal period or later in infancy. Acta Paediatr 199877–81. [DOI] [PubMed]
- 9.Luciano R, Velardi F, Romagnoli C.et al Failure of fibrinolytic endoventricular treatment to prevent neonatal post‐haemorrhagic hydrocephalus. A case‐control trial. Child Nervous Syst 19971373–76. [DOI] [PubMed] [Google Scholar]
- 10.Whitelaw A. Intraventricular streptokinase after intraventricular haemorrhage in newborn infants. Cochrane Database Syst Rev20011CD001691. [DOI] [PubMed] [Google Scholar]
- 11.Luciano R, Velardi F, Romagnoli C.et al Failure of fibrinolytic endoventricular treatment to prevent neonatal post‐haemorrhagic hydrocephalus. Child Nervous Syst 19971373–76. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy C R, Ayers S, Campbell M J.et al Randomized, controlled trial of acetazolamide and furosemide in posthemorrhagic ventricular dilatation in infancy: follow‐up at 1 year. Pediatrics 2001108597–607. [DOI] [PubMed] [Google Scholar]
- 13.Richard E, Cinalli G, Assis D.et al Treatment of post‐haemorrhage ventricular dilatation with an Ommaya's reservoir: management and outcome of 64 infants. Child Nervous Syst 200117334–340. [DOI] [PubMed] [Google Scholar]
- 14.Persson E K, Hagberg G, Uvebrant P. Hydrocephalus prevalence and outcome in a population‐based cohort of children born in 1989‐1998. Acta Pediatr 200594726–732. [DOI] [PubMed] [Google Scholar]
- 15.de Vries L S, Liem K D, van Dijk K.et al Early versus late treatment of posthaemorrhagic ventricular dilatation: results of a retrospective study from five neonatal intensive care units in The Netherlands. Acta Paediatr 200291212–217. [DOI] [PubMed] [Google Scholar]