Abstract
Background
Sodium acetate gel mattresses provide an active method of warming patients through release of latent heat of crystallisation. They can be used as an adjunct to incubator care or as an exclusive heat source.
Objective
To determine activation temperatures of the Transwarmer mattress needed to achieve plateau temperatures of 38–42°C.
Design and setting
In vitro testing of mattress temperature.
Methods and outcome measures
Transwarmer mattresses were activated at initial temperatures ranging from 5 to 40°C. Mattress temperature was recorded up to 4 h to determine peak and plateau temperatures. Peak and plateau temperatures achieved by the mattress were related to the initial starting temperature.
Results
The starting temperature of the mattress was strongly correlated with peak and plateau temperature (r = 0.99, p<0.001). To achieve the target temperature of 38–42°C, the Transwarmer mattress requires activation between 19.2°C and 28.3°C. A temperature of 37°C could be generated by activation at 17°C.
Conclusions
Safe use of this device is critically dependent on gel temperature at the point of activation. To ensure warming of a hypothermic neonatal patient without running any risk of burns, the mattress should be activated with a gel temperature between 19°C and 28°C.
Interhospital transport places considerable thermal stress on the neonatal patient, with the potential for harmful hypothermia, which is not amenable to simple incubator technologies. Sodium acetate gel mattresses provide an independent, active heat source through the release of latent heat of crystallisation after their activation. These mattresses are made of a sodium acetate gel in a flexible plastic casing and are activated by clicking a metal disc placed in the mattress, initiating crystallisation of the gel.
Commercially available chemical gel mattresses have been advocated as an adjunct to standard neonatal transport incubator care1,2,3 and in warming after paediatric cold immersion.4 These mattresses also form the sole source of heat for some infant and neonatal transport systems.5
In common with several neonatal transport services, our service began to use this device as an adjunct to incubator care of neonates during transfer. A considerable variability in the warming effects of the mattress was noted in clinical practice, possibly in relation to the ambient temperatures at which the mattress had been stored. As the manufacturer's datasheet suggested that the mattress should be activated at room temperature, without specifying an exact temperature range, we wished to examine the performance of the mattress in vitro. Our study aimed to determine the effect of different starting activation temperatures on the final heating temperatures achieved by the Transwarmer mattress.
Methods
The performance of the mattress was assessed through activation at a range of initial gel starting temperatures. All mattress temperatures were measured using a small thermocouple temperature probe placed on the plasticised side of the mattress, which was folded over to prevent cooling by surrounding air. The temperature probe was part of a Fluke 52 K/J thermometer system. This system is accurate between −20°C and 1000°C, to 0.1 of a degree, and was calibrated by an external source (RS Components) to ensure continuing accuracy.
A range of starting mattress temperatures between 5°C and 40°C were used to reflect a range that might be readily encountered in clinical use. The lower temperature could be experienced if a mattress was stored in an ambulance in winter, with the higher temperature achievable if the mattress was kept within a warmed incubator.
Once a stable starting mattress temperature was established, the mattress was activated inside an incubator (Ohmeda Ohio Care Plus (GE Healthcare, Bucks, UK) at 35°C), with mixing of the gel to ensure even activation. It was folded around the temperature probe to ensure even contact with no air pockets. The mattress temperature was then recorded at set intervals over a 4‐h period or until the mattress started to cool.
From the temperature curve at each starting temperature, summary measures of peak and plateau temperatures were determined, with subsequent regression analysis of these variables against mattress starting temperature.
Results
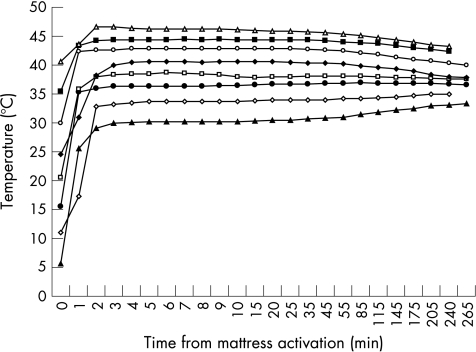
For all starting temperatures, there was a characteristic profile to mattress temperature changes after activation (fig 1). There was rapid heating of the mattress to reach a peak within 3 min and a plateau temperature within 5 min. The plateau temperature was maintained for a median of 68 min, after which the mattress temperature slowly moved towards the ambient incubator temperature. The difference between peak and plateau temperature was never more than 0.5°C and was usually only 0.1–0.2°C.
Figure 1 Temperature profiles of the Transwarmer mattress when activated from different gel starting temperatures, maintained in an incubator at 35°C.
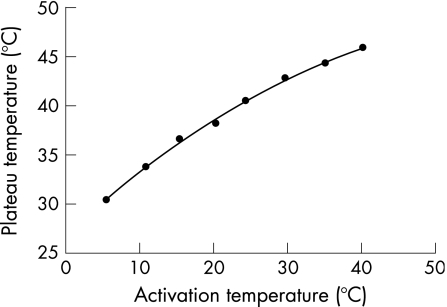
The relationship between starting temperature and peak or plateau temperature was best described by a second‐order regression curve, with no improvement in fit using higher order regression. The effect of starting temperature was both clinically and statistically highly significant (on peak temperature r = 0.99, p<0.01; on plateau temperature r = 0.99, p<0.01). Plateau temperature (PT) was related to activation temperature (AT) by the equation PT = 26.8+(0.689×AT)−(0.0054×AT2).
This regression curve shows that starting temperatures of 19.2–28.3°C would be required to achieve an effective and safe mattress plateau temperature of 38–42°C (fig 2). If a temperature of only 37°C was required, this could be generated by activation at 17°C.
Figure 2 Regression of plateau temperatures against starting activation temperatures of the Transwarmer mattress.
Discussion
The maintenance of normothermia during neonatal transfer is important to sustain normal physiological processes and to minimise oxygen demand. In extremely premature infants, hypothermia is well recognised as an independent factor associated with poor outcome.6 In dealing with this problem, care is needed with direct contact warming, as the thin nature of the premature baby's skin makes it particularly susceptible to burns at relatively low temperatures. Experience using transcutaneous oxygen monitoring7 suggests that burns are possible at temperatures >42°C.
For many patients, adequate temperature control can be achieved using a combination of double‐skinned incubator warming, humidification and plastic occlusive wrapping. Acetate gel mattresses can be a useful adjunct to these methods, but some variability can be noted in the clinical response. Our in vitro studies indicate that this variability may be related to the marked dependence of the activated mattress temperature on the initial starting temperature of the gel.
At the time of this study, the manufacturer of the Transwarmer mattress recommended that it should be stored and activated from room temperature, without defining a precise temperature range. They stated that the mattress would reach a temperature of 40°C if activated at 24°C. However, an incubator system that uses the Transwarmer mattress as its sole heat source5 should not be used at ambient temperatures >23.9°C.
Our data suggest that to warm a cold baby without risking burns, the mattress should be activated from a starting temperature of 19.2–28.3°C to a plateau temperature of 38–42°C. To maintain the temperature of a baby who is already warm, a mattress temperature of 37°C could be achieved by activation above 17°C. During the last year, the manufacturers of the Transwarmer mattress have modified their datasheet to recommend activation temperatures of 18–28°C, and our data support the importance of this recommendation. It should be noted that the mattress may take some time to equilibrate its temperature with its surroundings. The activation temperature is therefore the temperature of the mattress and not that of the surrounding ambient air.
What is known on this topic
Sodium acetate gel mattresses provide an active heat source for patient warming through release of latent heat of crystallisation.
They have been advocated as an adjunct to standard neonatal transport incubator care and in warming after paediatric cold immersion.
What this study adds
To warm a cold baby without risking burns, the Transwarmer mattress should be activated from a starting temperature of 19.2–28.3°C to achieve a plateau mattress temperature of 38–42°C.
To maintain the temperature of a baby who is already warm, a mattress temperature of 37°C could be achieved by activation at >17°C.
Although the usefulness of acetate gel mattresses has been shown in paediatric and neonatal studies, the neonate has particular problems, which mean that these mattresses should be used with care. The challenging characteristics of the neonate include reduced capacity for spontaneous thermogenesis, a higher surface area to body mass ratio, increased evaporative heat losses and increased susceptibility to burns.
With a narrower thermo‐neutral range, the provision of a warm object close to the baby's skin may not ensure the benefits seen in the paediatric population unless that object is controlled within a relatively narrow temperature range. In this context, the mattress might be more useful in neonates if it came supplied with an integrated thermometer strip to guide the user towards safe activation temperatures.
Footnotes
Competing interests: None.
References
- 1.Nielsen H C, Jung A L, Atherton S O. Evaluation of the Porta‐Warm mattress as a source of heat for neonatal transport. Pediatrics 197658500–504. [PubMed] [Google Scholar]
- 2.Herault J, Petroff J, Jeffrey J. The effectiveness of a thermal mattress in stabilizing and maintaining body temperature during the transport of very low birth weight newborns. Appl Nurs Res 200114210–219. [DOI] [PubMed] [Google Scholar]
- 3.Fenton A C, Leslie A, Skeoch C H. Optimising neonatal transfer. Arch Dis Child 200489F215–F219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ryan M, Beattie T F, Husselbee K.et al Use of the infant transwarmer mattress as an external warming modality in resuscitation from hypothermia. Emerg Med J 200320487–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Advanced Healthcare Technology Ltd Baby Pod II operating and maintenance manual. Sudbury, Suffolk: Advanced Healthcare Technology, 2003
- 6.Costeloe K, Hennessy E, Gibson A T.et al The EPICure study: Outcome to discharge from hospital for infants born at the threshold of viability. Pediatrics 2000106659–671. [DOI] [PubMed] [Google Scholar]
- 7.Lofgren O, Jacobson L. The influence of different electrode temperatures on recorded transcutaneous pO2 level. Pediatrics 197964892–897. [PubMed] [Google Scholar]