Abstract
Objectives
(1) To characterise neurodevelopmental outcome of neonates with necrotizing enterocolitis (NEC); (2) to define whether NEC increases risk of neurodevelopmental impairment in very low birth weight neonates; (3) to investigate whether stage of disease or need for surgery increase risk of poor outcome.
Design
A systematic review was performed. Searches identified 182 relevant papers. Ten studies compared extremely low birthweight neonates with NEC to infants of similar age and gestation who did not develop NEC. Data are reported as OR (95% CIs, p values for test for overall effect) and compared by χ2.
Results
7843 children (821 with NEC) were included in the meta‐analysis. Median follow‐up was 20 months (range 12 to 156). Overall, 45% of children who had neonatal NEC were neurodevelopmentally impaired. Infants with NEC were significantly more likely than infants of similar age and gestation who did not develop NEC to be neurodevelopmentally impaired (1.6 (1.3 to 2.0), p = 0.0001) including a higher risk of cerebral palsy (1.5 (1.2 to 2.0), p = 0.001), visual (2.3 (1.0 to 5.1), p = 0.04), cognitive (1.7 (1.4 to 2.2), p<0.0001) and psychomotor impairment (1.7 (1.3 to 2.2), p<0.0001). The odds ratio of neurodevelopmental impairment was also 2.3 times higher in neonates with Bell's stage III disease or requiring surgery ((1.5 to 3.6), p = 0.0001).
Conclusions
NEC is associated with significantly worse neurodevelopmental outcome than prematurity alone. Presence of advanced NEC and need for surgery increase the risk of neurological impairment.
Necrotizing enterocolitis (NEC) occurs in approximately 10% of extremely low birthweight (ELBW, ⩽1000 g) infants1 and surgery is required in 50–70% of these infants.1 Mortality for surgical NEC remains high (up to 40%). There are no specific therapeutic agents for NEC, the therapeutic aim is organ support, together with resection of gangrenous bowel.
Despite advances in neonatal intensive care improving survival of newborn infants, the long‐term outlook for infants with NEC, both those treated conservatively and those requiring surgery, is not well defined. Recent studies have highlighted improved neurodevelopmental outcomes for ELBW infants,2 but note that preterm birth contributes disproportionately to neonatal morbidity and subsequent neurodevelopmental disability.3 Recently, several studies have addressed the aetiology of poor neurodevelopmental outcome of premature or ELBW neonates4,5 and investigated the effects of interventions on neurodevelopmental outcomes.6
A number of studies have assessed neurodevelopmental outcomes of very low birthweight (VLBW, ⩽1500g) or ELBW neonates with NEC,7,8,9 many with small numbers of patients or from single centres.10,11 Some have concluded that surgical NEC is not associated with a greater risk of poor neurodevelopmental outcome than prematurity alone.12 Systematic reviews with or without meta‐analysis allow the reader to judge the potential for generalisation to different populations.
Our aims were, therefore:
(1) to characterise the neurodevelopmental outcome of neonates with NEC;
(2) to investigate whether NEC increases the risk of neurodevelopmental impairment in VLBW neonates;
(3) to investigate whether stage of disease or need for surgery increase the risk of poor neurodevelopmental outcome.
Methods
Literature search strategy
A systematic review of peer‐reviewed literature, including PubMed, ISI Web of Science, Embase and the Cochrane database, was performed. The search strategies used the following keywords and MeSH terms: necrotizing enterocolitis, necrotising enterocolitis, outcome, neurodevelopmental outcome, neurodevelopment, neurodevel* and neurol*. Citation searches were performed in ISI Web of Science and hand searches of reference lists were performed. Studies were included if they met a predefined list of inclusion criteria (table 1) and were selected independently by CR and SE. There were no disagreements concerning eligibility of papers; however, there were several overlapping cohort studies from NIHCHD, so the two reviewers decided between themselves which was the most appropriate paper to include. Data were collected for a predefined list of variables and entered into Cochrane Collaboration Review Manager 4.2 independently by CR and SE.
Table 1 Inclusion criteria for studies.
| Criteria | ||
|---|---|---|
| Publication | Language | Any |
| Date | 1951–2005 | |
| Type | Original research, not reviews | |
| Study | Type | All (retrospective/prospective/RCT/cohort study) |
| Patients included | Date of birth | >1975 |
| Birthweight | ⩽1500 g | |
| Gestation | Any | |
| Follow‐up | At least 1 year | |
| Comparisons | NEC with no NECMedical NEC with surgical NEC | |
RCT, randomised controlled trial; NEC, necrotizing enterocolitis.
Variables and definitions
The variables of interest were defined as follows. Necrotizing enterocolitis was defined as Bell's stage II or above13 diagnosed clinically, radiologically or histologically; medical management included antibiotic usage, withdrawal of feeds and any resuscitative measures; surgery included laparotomy or peritoneal drainage. In one paper,14 infants were classified as stage II or stage III NEC; here, stage III was taken to imply surgical treatment, and stage II medical. Cerebral palsy was defined as a non‐progressive neurological disorder characterised by abnormal limb tone (in one or more limbs) and inability to control movement and posture.9Visual impairment was defined as blindness or visual deficit in at least one eye. Deafness was defined as hearing impairment requiring hearing aids in at least one ear. Mental developmental impairment (MDI) and psychomotor developmental impairment (PDI) were defined as scores of <70 on the relevant Bayley II scale.15 MDI scores assess memory, problem solving, discrimination, classification, language and social skills. PDI scores assess muscle control, walking, running, jumping, use of writing implements and imitation of hand movements. In both scores, the normal range (corrected for age) is 100±15 (mean ±1 SD) so a score of <70 lies >2 SDs below the mean. Infants who are so impaired that testing is impossible are given a score of 49. In studies where Bayley scores were not assessed, patients with impaired mental development (including delayed language development) were grouped with MDI <70 and patients with psychomotor impairment grouped with PDI <70. Neurodevelopmental impairment (NDI) is a composite outcome based on cerebral palsy, bilateral blindness or deafness, PDI score <70, or MDI score <70. This gives an overall estimation of the number of infants with developmental deficit. Papers where Griffiths Developmental scales were used were assigned to the NDI group if the Griffiths GQ score was less than 2SD below the mean corrected for gestational age. In one paper,12 cognitive impairment was marked by requirement for speech therapy and psychomotor development by performance on a self‐developed drawing test. These results were grouped with MDI and PDI respectively.
Very low birth weight (VLBW) infants are those with birthweight ⩽1500 g and a subset of these are extremely low birth weight (ELBW) infants whose birthweight is ⩽1000 g.
Statistical comparisons
Review Manager 4.2 (the Cochrane Collaboration) was used to analyse data. Data are presented as odds ratio (95% confidence intervals) with p values shown for Z test for overall significance and I2 statistic16 for heterogeneity.
Results
Searches performed according to strategy identified 1039 papers; 14 fulfilled inclusion criteria, 13 comparing VLBW or ELBW neonates with NEC to infants of similar age and gestation without NEC,8,9,10,11,12,14,17,18,19,20,21,22,23 and one study24 comparing surgically treated infants with NEC to those treated medically so was included in this analysis only. Three of the 138,9,23 were excluded because of overlap with a more recent study.21 The study characteristics are shown in table 2. All studies were retrospective case control or cohort studies.
Table 2 Characteristics of included studies.
| Authors | Study characteristics | Patient characteristics | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Date published | Study type | Country | Centres | Assessors blinded? | Assessment tool | Dates of birth | Birth weight | Duration of follow‐up (months)* | Follow‐up (%) | Number with NEC (n) | Total number of patients (N) | ||
| Castro17 | 2004 | Cohort | USA | Multi | Yes | BSID II | 1993–1994 | <1000 g | 18–22 | 78 | 72 | 1483 | |
| Chacko18 | 1999 | Case–control | Australia | Single | No | GQ | 1990–1993 | <1000 g | 12–59 | 100 | 40 | 60 | |
| Hintz21 | 2005 | Cohort | USA | Multi | Yes | BSID II | 1995–1998 | 401–1000 g | 18–22 | 79 | 532 | 4933 | |
| Holmsgaard19 | 1996 | Cohort | Denmark | Single | No | Clinical | 1987–1990 | 994 g mean | 42 (mean) | 99 | 4 | 136 | |
| Mayr12 | 1994 | Cohort | Austria | Single | No | Denver | 1978–1991 | <1501 g | 12–156† | 63 | 12 | 18 | |
| Simon24 | 1993 | Cohort | USA | Single | No | BSID I | 1986–1988 | <1500 g | 15† | 100 | 18 | 18 | |
| Sonntag20 | 2000 | Case–control | Germany | Single | No | GQ | 1992–1996 | <1500 g | 20 | 91 | 20 | 60 | |
| Tobiansky10 | 1995 | Case–control | Australia | Single | No | GQ | 1986–1991 | ⩽1500 g | 36–60 | 91 | 49 | 89 | |
| Walsh14 | 1989 | Cohort | USA | Single | No | BSID I | 1975–1983 | <1500 g | 20 | 90 | 36 | 802 | |
| Waugh22 | 1996 | Cohort | Australia | Single | Yes | GQ | 1977–1990 | <1000 g | 24 | 89 | 23 | 199 | |
| Yeh11 | 2004 | Case–control | Taiwan | Single | No | BSID II | 1991–2002 | <1500 g | 18 | 54 | 15 | 45 | |
*All duration of follow‐up times refer to corrected age unless marked with †. Corrected age is gestational age at birth plus chronological age (ie, corrected for prematurity). BSID, Bayley Standardised Infant Development Scale (I and II); GQ, Griffiths Quotient; Denver, Denver developmental screening test.
Altogether, 7843 children were included in the meta‐analysis, of whom 821 had NEC. Median follow‐up was 20 months (range 12 to 156). The median percentage of patients followed up was 90%.
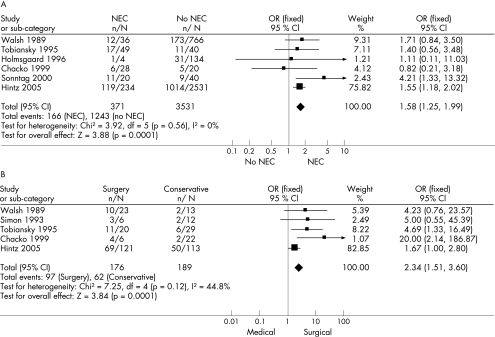
The meta‐analysis results are summarised in table 3. 20% of neonates with NEC developed cerebral palsy, 3% developed visual, 3% hearing, 36% cognitive and 35% psychomotor impairment. All outcomes were worse in neonates with stage III disease or who required surgery (surgical NEC group). There were significant (p<0.05) differences in the odds ratio of cerebral palsy (1.55 (1.19 to 2.03)), visual impairment (2.31, (1.04 to 5.11)), cognitive impairment (1.44 (1.24 to 1.68)) and psychomotor impairment (1.72 (1.35 to 2.19)) between infants with NEC and infants who did not have NEC. Neurodevelopmental impairment occurred in 45% of children who had had neonatal NEC, compared to 35% of children who had been VLBW or ELBW but did not have NEC (χ2 p = 0.0003). Overall, infants with NEC were significantly more likely to have neurodevelopmental impairment (OR 1.58 (1.25 to 1.99), p = 0.0001) (table 3). These data are shown as a Forrest plot in fig 1A. When we analysed the cohort studies separately from the case‐control studies, both analyses yielded similar odds ratios to the combined data, inevitably with wider confidence intervals (case‐control 1.7 (0.92 to 3.21); cohort 1.56 (1.21 to 2.00)).
Table 3 Results of meta‐analyses. NEC vs no NEC.
| Description | NEC | No NEC | Number of studies | I2 (%) | Odds ratio (95% CI) | p Value | References | ||
|---|---|---|---|---|---|---|---|---|---|
| n | N | n | N | ||||||
| Cerebral palsy | 79 | 393 | 590 | 3984 | 5 | 37.4 | 1.55 (1.19 to 2.03) | 0.001 | 10,14,17,19,21 |
| Visual impairment | 10 | 296 | 36 | 2857 | 3 | 0 | 2.31 (1.04 to 5.11) | 0.04 | 10,19,21 |
| Hearing impairment | 9 | 315 | 46 | 2886 | 5 | 0 | 1.50 (0.70 to 3.23) | 0.29 | 10,12,18,19,21 |
| Cognitive impairment | 133 | 369 | 882 | 3680 | 7 | 0.7 | 1.72 (1.35 to 2.19) | <0.0001 | 10,11,12,14,19,21,22 |
| Psychomotor impairment | 115 | 328 | 835 | 3605 | 5 | 0 | 1.71 (1.34 to 2.18) | <0.0001 | 11,12,17,19,21 |
| Neurodevelopmental impairment | 166 | 371 | 1243 | 3531 | 6 | 0 | 1.58 (1.25 to 1.99) | 0.0001 | 10,14,18,19,20,21 |
Figure 1 (A) Forrest plot: Neurodevelopmental Impairment NEC vs. No NEC. (B) Forrest plot: Neurodevelopmental Impairment surgical NEC vs. medical NEC. The Forrest plot is the graphical output of a meta‐analysis. Each study is represented by a dot with 95% confidence intervals represented by horizontal lines. The size of the dot is proportional to the relative size of the study. The diamond represents the combined outcome, its width representing the 95% confidence interval. (n = number affected; N = total number of patients; OR = odds ratio; CI = confidence interval)
When the surgical NEC group was compared with those managed non‐surgically (medical NEC group), they were significantly more likely to have cerebral palsy (OR 2.74 (1.44 to 5.21) p = 0.002) and psychomotor impairment (OR 1.85 (1.07 to 3.21), p = 0.03). There were non‐significant trends towards an increased risk of hearing impairment and cognitive impairment. Overall the surgical NEC group was 2.34 times more likely to have neurodevelopmental impairment than the medical NEC group (95% CI 1.51 to 3.60, p = 0.0001). These data are shown in fig 1B/table 4. There were no significant differences between the medical NEC and No NEC groups for neurodevelopmental impairment (OR 1.02 (0.73 to 1.44), p = 0.89), thus supporting the finding that surgical NEC is specifically associated with a poorer neurodevelopmental outcome than either medically treated NEC or prematurity alone. There were no significant differences for any of the other outcomes between medical NEC and No NEC (results not shown), although there were fewer studies to compare for the other outcome measures.
Table 4 Surgical treatment vs medical treatment.
| Description | Surgical NEC | Medical NEC | Number of studies | I2 (%) | Odds ratio (95% CI) | p Value | References | ||
|---|---|---|---|---|---|---|---|---|---|
| n | N | n | N | ||||||
| Cerebral palsy | 35 | 144 | 15 | 150 | 2 | 53.0 | 2.74 (1.44 to 5.21) | 0.002 | 10,21 |
| Visual impairment | 6 | 142 | 3 | 150 | 2 | 28.9 | 2.40 (0.56 to 10.23) | 0.24 | 10,21 |
| Hearing impairment | 6 | 143 | 1 | 150 | 2 | 0 | 4.93 (0.81 to 29.91) | 0.08 | 10,21 |
| Cognitive impairment | 65 | 161 | 48 | 154 | 3 | 0 | 1.54 (0.96 to 2.48) | 0.07 | 10,14,21 |
| Psychomotor impairment | 47 | 125 | 30 | 123 | 2 | 0 | 1.85 (1.07 to 3.21) | 0.03 | 10,21,24 |
| Neurodevelopmental impairment | 97 | 176 | 62 | 189 | 5 | 44.8 | 2.34 (1.51 to 3.60) | 0.0001 | 10,14,18,21,24 |
The p values shown are the significance of the tests for overall effect for each outcome. n, number affected; N, total number of patients; NEC, necrotizing enterocolitis; I2 = heterogeneity statistic
Discussion
A small number of papers have been published describing the neurodevelopmental outcome of survivors of NEC. Some compare children who had NEC with those born ELBW who did not have NEC, others compare the outcomes of babies treated conservatively with those receiving surgery. Meta‐analyses can be usefully performed on non‐randomised studies,25 in which case caveats must be drawn in the interpretation of the results. Clearly, in comparing ELBW infants who had NEC with those that did not get NEC, we are comparing two populations rather than two groups of individuals randomly allocated from the same population.
Limitations of this type of study include the presence of confounding factors – it is impossible to quantify the effect of factors that are related to both NEC and neurodevelopmental impairment (eg prematurity); this is the most important threat to the validity of results from cohort studies.25 Epidemiological studies are prone to publication bias as only statistically significant findings may be published.26 Other problems which are likely to be greater in meta‐analyses of retrospective, non‐randomised studies include inadequate reporting of methods, variation in study design, variation in inclusion criteria and variation in presentation of results.26 Another potential problem with meta‐analysis of non‐randomised studies is combining data from different types of study design. In this meta‐analysis, we have combined data from cohort and case control studies, although where there were enough studies of each type to undertake two separate analyses, the results were consistent. We chose to combine studies by using odds ratios rather than relative risks as whereas it is appropriate to refer to odds ratios for both cohort and case‐control studies, relative risk cannot be calculated for case‐control studies. Interpretation of odds ratios in the same way as relative risks, however, can overestimate effect sizes where the event is frequent in the index group (as in our study) and the odds ratio is large27 (although most odds ratios we obtained were <2.5). Another potential problem with the approach that we have used is the fact that different papers have used different tools for measurement of neurodevelopmental outcome, although most studies that we included used one of two scores–Bayley scores or Griffiths Quotients.
Despite these limitations, we believe that our results show that neonates who have NEC can expect a significantly worse neurodevelopmental outcome that those VLBW neonates who do not have NEC. Although the risk seems small (OR 1.6), the risk of poor neurodevelopmental outcome is already great in VLBW infants, so any significantly increased risk is important. This results in 45% of NEC survivors having poor neurodevelopmental outcome. If a baby with NEC needs surgery, their neurological outcome becomes even worse (OR 2.34) compared to medically‐treated infants. This finding does not imply that one should not treat a neonate with perforated NEC surgically; it only implies that babies sick enough to require surgery have a worse outcome than those not sick enough to require surgery. In this study, we only included infants that had Bell's stage II or III NEC, as the signs and symptoms for stage I NEC are too non‐specific to make this a meaningful group for comparison. However, even the diagnosis of stage II and stage III NEC can be equivocal and we acknowledge that this is another potential shortcoming of this study.
Factors causing poor neurodevelopmental outcome in premature infants are complex. Neurogenesis, neuronal maturation and synaptogenesis contribute to brain development in the 2nd and 3rd trimester of pregnancy28 so extremely premature infants have a deficit in brain maturation. Postnatal continuation of these processes requires adequate nutrition, and may be adversely affected by many factors associated with prematurity and surgery. Indeed, a specific negative impact of NEC on cerebral growth is suggested by the finding that NEC is a significant predictor of smaller head circumference in ELBW infants.29
Damage to existing cerebral tissue is another likely contributor to poor neurological outcome. This can be caused by infection or inflammation, respiratory insufficiency, hypotension, acidosis, fluctuations in glycaemic control, disseminated intravascular coagulation, anaesthesia and transport. In particular, infection and sepsis, which may result from intestinal perforation and/or gangrene, have been highlighted as independent risk factors.9,30 They cause increased cytokines, which are implicated in the pathogenesis of periventricular leukomalacia, a major determinant of adverse neurological outcome.31 Surgery for NEC also causes a cytokine surge which could be responsible for white matter damage, and it would be interesting to determine if a surgical treatment with a lower degree of tissue trauma (peritoneal drainage) results in a better neurological outcome than laparotomy. Poor outcome may be independently associated with surgery, with or without NEC–28% of surviving ELBW infants who required surgery of any sort have a poor sensorieneural outcome.32 In favour of the severity of disease, rather than surgery per se causing poor neurodevelopmental outcome, Adesanya et al.7 found that neurodevelopmental impairment was worse in infants who had perforated NEC than those with spontaneous bowel perforation.
Most of the studies had good rates of follow up suggesting that the results are representative, although a bias in overestimation of adverse outcomes has been found previously, as children with poor neurodevelopmental outcome are more likely to be retained for follow‐up.7,33,34,35 We analysed cohorts that were born over a wide period of time (1975–2002), which includes babies born before surfactant and high frequency oscillation were introduced. Although the mortality of ELBW neonates has improved, the effects on neurodevelopmental outcome are less well defined.2,5,36
What is already known on this topic
Infants born prematurely have a risk of poor neurodevelopmental outcome.
Previous studies reporting neurodevelopmental outcome of infants who have had necrotizing enterocolitis give conflicting results.
What this study adds
Infants who survive necrotizing enterocolitis have a worse neurodevelopmental outcome than other extremely low birthweight survivors.
Infants who require surgery for necrotizing enterocolitis have an even higher risk of poor outcome than those who receive only medical treatment.
Our findings on the overall rates of poor neurodevelopmental outcome in ELBW infants are comparable to recent population‐based prospective studies which demonstrated that 10% of extremely premature infants had severe motor disability, 2% were blind, 3% were deaf and 49% had some disability37 and that these disabilities persisted into childhood.38 The largest study in our review, that from the National Institute of Child Health,21 was the most complete in terms of available data, therefore in comparisons where only a few studies were included there is a risk that the results of smaller studies are subsumed. However, this paper reported on outcomes from sixteen different centres in the US and many of the other papers are from different countries, so pooling the results makes the results more applicable to patients outside the USA.
If neonates with NEC are at increased risk of adverse neurodevelopmental outcome, two questions arise: can we predict which babies will have an adverse outcome, and can we do anything to prevent it? Logistic regression and neural networks had low sensitivity and specificity for predicting major handicap in ELBW infants39 and although severely abnormal ultrasound has a high predictive value for adverse neurological outcome,23 up to 30% of ELBW survivors with normal neonatal ultrasound are found to have impairment at 18–22 months.40 MRI at school age has recently been suggested to be better predictor of IQ and motor performance than ultrasound,41 but whether neonatal MRI is a better predictor than ultrasound is not known.
Now that we know that infants with NEC are at increased risk of neurodevelopmental impairment we should ensure that neurodevelopmental assessment plays a part in the follow‐up of any new treatment. It is also important that parents and professionals are aware of the increased long term risks in these critically ill neonates.
Abbreviations
ELBW - extremely low birth weight (⩽1000 g)
MDI - mental developmental impairment
NDI - neurodevelopmental impairment
NEC - necrotizing enterocolitis
PDI - psychomotor developmental impairment
VLBW - very low birth weight (⩽1500 g)
Footnotes
Funding: The Stanley Thomas Johnson foundation, Berne, Switzerland.
Competing interests: None.
References
- 1.Pierro A, Hall N. Surgical treatment of infants with necrotizing enterocolitis. Semin Neonatol 20038223–232. [DOI] [PubMed] [Google Scholar]
- 2.Hintz S R, Kendrick D E, Vohr B R.et al Changes in neurodevelopmental outcomes at 18 to 22 months' corrected age among infants of less than 25 weeks' gestational age born in 1993–1999. Pediatrics 20051151645–1651. [DOI] [PubMed] [Google Scholar]
- 3.Fanaroff A A, Hack M, Walsh M C. The NICHD neonatal research network: changes in practice and outcomes during the first 15 years. Semin Perinatol 200327281–287. [DOI] [PubMed] [Google Scholar]
- 4.Wood N S, Costeloe K, Gibson A T.et al The EPICure study: associations and antecedents of neurological and developmental disability at 30 months of age following extremely preterm birth. Arch Dis Child Fetal Neonatal Ed 200590F134–F140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vohr B R, Wright L L, Poole W K.et al Neurodevelopmental outcomes of extremely low birth weight infants <32 weeks' gestation between 1993 and 1998. Pediatrics 2005116635–643. [DOI] [PubMed] [Google Scholar]
- 6.Mestan K K, Marks J D, Hecox K.et al Neurodevelopmental outcomes of premature infants treated with inhaled nitric oxide. N Engl J Med 200535323–32. [DOI] [PubMed] [Google Scholar]
- 7.Adesanya O A, O'Shea T M, Turner C S.et al Intestinal perforation in very low birth weight infants: Growth and Neurodevelopment at 1 Year of Age. J Perinatol 200525583–589. [DOI] [PubMed] [Google Scholar]
- 8.Salhab W A, Perlman J M, Silver L.et al Necrotizing enterocolitis and neurodevelopmental outcome in extremely low birth weight infants <1000 g. J Perinatol 200424534–540. [DOI] [PubMed] [Google Scholar]
- 9.Stoll B J, Hansen N I, Adams‐Chapman I.et al Neurodevelopmental and growth impairment among extremely low‐birth‐weight infants with neonatal infection. JAMA 20042922357–2365. [DOI] [PubMed] [Google Scholar]
- 10.Tobiansky R, Lui K, Roberts S.et al Neurodevelopmental outcome in very‐low‐birth‐weight infants with necrotizing enterocolitis requiring surgery. J Paediatr Child Health 199531233–236. [DOI] [PubMed] [Google Scholar]
- 11.Yeh T C, Chang J H, Kao H A.et al Necrotizing enterocolitis in infants: clinical outcome and influence on growth and neurodevelopment. J Formos Med Assoc 2004103761–766. [PubMed] [Google Scholar]
- 12.Mayr J, Fasching G, Hollwarth M E. Psychosocial and psychomotoric development of very low birthweight infants with necrotizing enterocolitis. Acta Paediatr Suppl 199439696–100. [DOI] [PubMed] [Google Scholar]
- 13.Kliegman R M, Walsh M C. Neonatal necrotizing enterocolitis: pathogenesis, classification, and spectrum of illness. Curr Probl Pediatr 198717213–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walsh M C, Kliegman R M, Hack M. Severity of Necrotizing Enterocolitis ‐ Influence on outcome at 2 years of age. pediatrics 198984808–814. [PubMed] [Google Scholar]
- 15.Bayley N.Bayley scales of infant development II. San Antonio, Texas: Psychological Corporation, 1993
- 16.Higgins J P, Thompson S G. Quantifying heterogeneity in a meta‐analysis. Stat Med 2002211539–1558. [DOI] [PubMed] [Google Scholar]
- 17.Castro L, Yolton K, Haberman B.et al Bias in reported neurodevelopmental outcomes among extremely low birth weight survivors. Pediatrics 2004114404–410. [DOI] [PubMed] [Google Scholar]
- 18.Chacko J, Ford W D A, Haslam R. Growth and neurodevelopmental outcome in extremely‐low‐birth‐ weight infants after laparotomy. Pediatr Surg Int 199915496–499. [DOI] [PubMed] [Google Scholar]
- 19.Holmsgaard K W, Petersen S. Infants with gestational age 28 weeks or less ‐ Impact of neonatal treatment and complications on outcome. Dan Med Bull 19964386–91. [PubMed] [Google Scholar]
- 20.Sonntag J, Grimmer I, Scholz T.et al Growth and neurodevelopmental outcome of very low birthweight infants with necrotizing enterocolitis. Acta Paediatr 200089528–532. [DOI] [PubMed] [Google Scholar]
- 21.Hintz S R, Kendrick D E, Stoll B J.et al Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics 2005115696–703. [DOI] [PubMed] [Google Scholar]
- 22.Waugh J, O'Callaghan M J, Tudehope D I.et al Prevalence and aetiology of neurological impairment in extremely low birthweight infants. J Paediatr Child Health 199632120–124. [DOI] [PubMed] [Google Scholar]
- 23.Hack M, Wilson‐Costello D, Friedman H.et al Neurodevelopment and predictors of outcomes of children with birth weights of less than 1000 g: 1992–1995. Arch Pediatr Adolesc Med 2000154725–731. [DOI] [PubMed] [Google Scholar]
- 24.Simon N P, Brady N R, Stafford R L.et al The effect of abdominal incisions on early motor development of infants with necrotizing enterocolitis. Dev Med Child Neurol 19933549–53. [DOI] [PubMed] [Google Scholar]
- 25.Egger M, Davey Smith G, Schneider M. Systematic reveiws of observational studies. In: Egger M, Davey Smith G, Altman DG, eds. Systematic reviews in health care. London: BMJ Publishing Group, 2001211–227.
- 26.Altman D G.Systematic reviews of evaluations of prognostic variables. In: Egger M, Davey Smith G, Altman DG, eds. Systematic reviews in health care. London: BMJ Publishing Group, 2001228–247.
- 27.Davies H T O, Crombie I K, Tavakoli M. When can odds ratios mislead? BMJ 1998316989–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vohr B R, Allen M. Extreme prematurity‐‐the continuing dilemma. N Engl J Med 200535271–72. [DOI] [PubMed] [Google Scholar]
- 29.Wood N S, Costeloe K, Gibson A T.et al The EPICure study: growth and associated problems in children born at 25 weeks of gestational age or less. Arch Dis Child Fetal Neonatal Ed 200388F492–F500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wheater M, Rennie J M. Perinatal infection is an important risk factor for cerebral palsy in very‐low‐birthweight infants. Dev Med Child Neurol 200042364–367. [DOI] [PubMed] [Google Scholar]
- 31.Ellison V J, Mocatta T J, Winterbourn C C.et al The relationship of CSF and plasma cytokine levels to cerebral white matter injury in the premature newborn. Pediatr Res 200557282–286. [DOI] [PubMed] [Google Scholar]
- 32.Doyle L W, Callanan C, Carse E.et al Surgery and the tiny baby: Sensorineural outcome at 5 years of age. J Paediatr Child Health 199632167–172. [DOI] [PubMed] [Google Scholar]
- 33.Tin W, Fritz S, Wariyar U.et al Outcome of very preterm birth: children reviewed with ease at 2 years differ from those followed up with difficulty. Arch Dis Child Fetal Neonatal Ed 199879F83–F87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Turnbull D. Loss to follow‐up of preterm and very preterm babies. Lancet 19983521875–1876. [DOI] [PubMed] [Google Scholar]
- 35.Doyle L W, Anderson P J. Improved neurosensory outcome at 8 years of age of extremely low birthweight children born in Victoria over three distinct eras. Arch Dis Child Fetal Neonatal Ed 200590F484–F488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wood N S, Marlow N, Costeloe K.et al Neurologic and Developmental Disability after Extremely Preterm Birth. N Engl J Med 2000343378–384. [DOI] [PubMed] [Google Scholar]
- 37.Marlow N, Wolke D, Bracewell M A.et al Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med 20053529–19. [DOI] [PubMed] [Google Scholar]
- 38.Ambalavanan N, Nelson K G, Alexander G.et al Prediction of neurologic morbidity in extremely low birth weight infants. J Perinatol 200020496–503. [DOI] [PubMed] [Google Scholar]
- 39.Laptook A R, O'Shea T M, Shankaran S.et al Adverse neurodevelopmental outcomes among extremely low birth weight infants with a normal head ultrasound: prevalence and antecedents. Pediatrics 2005115673–680. [DOI] [PubMed] [Google Scholar]
- 40.Rademaker K J, Uiterwaal C S, Beek F J.et al Neonatal cranial ultrasound versus MRI and neurodevelopmental outcome at school age in children born preterm. Arch Dis Child Fetal Neonatal Ed 200590F489–F493. [DOI] [PMC free article] [PubMed] [Google Scholar]