Abstract
Objective
To evaluate whether measurement of haemoglobin concentration in neonates using point of care testing agrees with laboratory measurement.
Design
127 paired blood samples taken from babies on a neonatal intensive care unit for full blood count and blood gas analysis by point of care testing were reviewed according to current practice. A comparison was made between the laboratory and blood gas analyser haemoglobin measurements to assess limits of agreement and look for any systematic difference.
Setting
Neonatal Unit, Jessop Wing, Royal Hallamshire Hospital, Sheffield, UK
Patients
Babies staying on the neonatal unit, who currently have contemporaneous blood samples taken for full blood count and blood gas analysis by point of care testing.
Intervention
Results from blood samples were reviewed.
Main outcome measure
Comparison between laboratory and point of care testing haemoglobin concentrations.
Results
The mean laboratory haemoglobin concentration was 155 g/l (range 30–226 g/l); the mean point of care testing haemoglobin concentration was 157 g/l (range 30–228 g/l). The mean (SD) difference between paired samples was 2 (11) g/l; 95% CI −4.0 to 0.1 g/l; and limits of agreement −23 to 19 g/l.
Conclusions
The blood gas analyser on the neonatal unit at Royal Hallamshire Hospital, Sheffield, gives a useful estimation of haemoglobin concentration compared with laboratory measurement, with smaller sample volume. Although this does not replace a full blood count, it is a useful adjunct to neonatal care monitoring.
Keywords: point of care testing (POCT), haemoglobin concentration, neonatal unit, anaemia, blood gas analyser
Point of care testing can be defined as the testing of patient samples at the place where care is delivered.1 Its advantages include the need for small volumes of blood, reducing the risk of iatrogenic anaemia,2 and the timely availability of results, diminishing the interval between receipt of a result and therapeutic intervention.2
Babies requiring neonatal intensive care are susceptible to iatrogenic blood loss from frequent blood sampling,3,4,5,6,7 which can hasten the onset or exacerbate the severity of anaemia.5 Occasionally babies receiving neonatal care may decompensate from occult blood loss—for example, large periventricular or intraventricular haemorrhage—necessitating prompt action on the basis of clinical assessment and timely results. The turnaround time of laboratory tests can be considerable, which may affect clinical decisions.2
Many neonatal units have blood gas analysers located on site, which are used exclusively for neonatal samples. Thus point of care testing is a routine part of neonatal practice. Many modern blood gas analysers can now estimate haemoglobin, glucose and electrolytes on every blood gas sample, without the need for increased sample volume. It has been suggested that the weekly full blood count (requiring 500 μl of blood) carried out for convalescing neonates, solely to identify anaemia, could be replaced by point of care testing (requiring 95 μl of blood).
We therefore evaluated the performance of our blood gas analyser for this potential change in our service delivery. We compared our blood gas analyser's results with the hospital laboratory results for babies who, as part of their routine care, were having contemporaneous blood gas and laboratory haemoglobin measurements for clinical reasons.
Methods
We conducted this service evaluation at the Neonatal Unit, Jessop Wing, Royal Hallamshire Hospital, Sheffield, UK. This hospital is part of the Sheffield Teaching Hospitals NHS Foundation Trust, which has produced a “simple rules toolkit” to ensure that staff do not inadvertently conduct research. We used this tool for assessing the protocol for our service evaluation. It was established as being a service evaluation because we were assessing our current practice (ie there was no change in practice), the output was not applicable to other units, and as such did not require ethical approval to be sought. Other units would have different quality controls, different analysers and different sample handling, and therefore they would need to conduct their own service evaluation prior to adopting any change in their practice.
Our current practice is to take two blood samples from babies staying on the unit, one for full blood count and one for blood gas measurement, which routinely gives a measurement of haemoglobin concentration. The full blood count sample is transported to the hospital laboratory and analysed using a Beckman‐Coulter LH750 analyser (Beckman‐Coulter, High Wycombe, UK); the blood gas specimen is processed using a ABL725 Radiometer blood gas analyser (Radiometer, Copenhagen, Denmark) in the neonatal unit. Both analysers are calibrated regularly and are subject to rigorous quality controls. The laboratory analyser needs a minimum of 500 μl of blood and the blood gas analyser needs only 95 μl per sample.
During the evaluation period, paired results were compared if taken contemporaneously and were of the same type (capillary with capillary, venous with venous, arterial with arterial) either from admission or during the baby's stay on the neonatal unit. Only one result per baby was included to eliminate any bias from individuals.
We analysed the data using the SPSS (version 10.0) and Arcus Biostat (Biostat, Englewood, NJ, USA). Haemoglobin values were compared using paired t test, Pearson's correlation coefficient and the limits of agreement.8
Results
What is already known on this topic
Babies requiring neonatal intensive care are susceptible to iatrogenic blood loss from frequent blood sampling.
Point of care testing, used routinely in neonatal units, can be used to give rapid estimation of haemoglobin on blood gas samples, without increased sample volume.
What this study adds
Haemoglobin measurement by point of care testing does not differ significantly from laboratory measurement across a wide range of values with well‐validated quality control settings.
It may be possible to replace weekly haemoglobin monitoring in convalescing babies with point of care haemoglobin measurement.
A total of 127 paired samples were compared, each from a different baby. The laboratory haemoglobin concentration ranged from 30 g/l to 226 g/l and the blood gas analyser haemoglobin concentration ranged from 30 g/l to 228 g/l. The mean (SD) laboratory haemoglobin concentration was 155 (32) g/l and the mean (SD) point of care testing haemoglobin concentration was 157 (36) g/l. There was a trend to a difference between the means, but this did not reach statistical significance (p = 0.053).
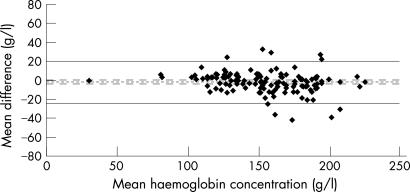
The mean difference between paired samples was 2 g/l (0.7%), SD 11 g/l (7%). There was no systematic difference between the paired measurements, as the 95% CI for the mean difference was −4.0 to 0.1 g/l, crossing zero. The limits of agreement (giving 95% of the differences) were −23 to 19 g/l (−14.2% to 12.6%) (fig 1). Intercentile ranges are given in table 1.
Figure 1 Mean haemoglobin concentration versus the difference between the two measurements in 127 paired samples. The fine dotted line is the mean difference, with 95% CI for the mean shown as the dashed lines. The solid lines show the limits of agreement.
Table 1 Intercentile ranges and confidence levels for haemoglobin estimation.
| Centiles | Values (g/l) | Confidence level | Intercentile range (g/l) | ± value (g/l) |
|---|---|---|---|---|
| 25th to 75th | −7 to 4 | 50% | 11 | 5.5 |
| 12.5th to 87.5th | −12 to 7 | 75% | 19 | 9.5 |
| 5th to 95th | −2 to 13 | 90% | 34 | 17 |
| 2.5th to 97.5th | −24 to 20 | 95% | 42 | 22 |
| 1st to 99th | −38 to 28 | 99% | 67 | 33.5 |
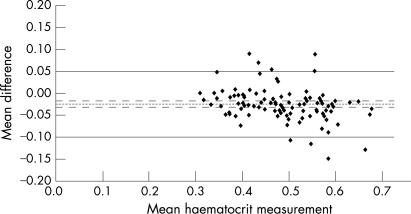
Haematocrit values were available for 104 out of the 127 samples, giving a measured result from the laboratory sample and a calculated value from the point of care testing sample. The mean (SD) laboratory haematocrit was 0.471 (0.083) and the mean (SD) point of care testing haematocrit concentration was 0.496 (0.095). These were significantly different from each other (p<0.001). The mean difference between paired samples was 0.025 (4.8%), SD 0.04 (7.6%). There was a small systematic difference between the paired measurements for haematocrit (95% CI for the mean difference −0.017 to −0.032). The limits of agreement (giving 95% of the differences) were −0.099 to 0.05 (fig 2). Intercentile ranges are given in table 2.
Figure 2 Mean haematocrit measurement versus the difference between the two measurements in 104 paired samples. The dotted line is the mean difference, with 95% CI for the mean shown as the dashed lines. The solid lines are show the limits of agreement.
Table 2 Intercentile ranges and confidence levels for haematocrit estimation.
| Centiles | Values | Confidence level | Intercentile range | ± value |
|---|---|---|---|---|
| 25th to 75th | −0.04 to −0.01 | 50% | −0.04 | −0.02 |
| 12.5th to 87.5th | −0.05 to 0.0 | 75% | −0.06 | −0.03 |
| 5th to 95th | −0.08 to 0.05 | 90% | −0.13 | −0.06 |
| 2.5th to 97.5th | −0.11 to 0.06 | 95% | −0.17 | −0.09 |
| 1st to 99th | −0.13 to 0.09 | 99% | −0.22 | −0.11 |
Discussion
Point of care measurement to estimate haemoglobin concentration has clear theoretical advantages. In this study we have shown that the haemoglobin results of our blood gas analyser do not differ significantly from those from our laboratory. We have also shown that there is no systematic difference between the two measurements across a wide range of haemoglobin values. The data seem to suggest that the spread of the difference in haemoglobin measurements increases at the higher range of values. However, comparing the laboratory haematocrit (an independent variable) with the difference in haemoglobin shows that there is no relationship between the size of the difference or the degree of agreement (r = 0.14, p = 0.14). The haematocrit values seem to agree less well, but this could be because the point of care measurements for haematocrit in our blood gas analyser are derived by using a formula from the measured point of care haemoglobin values.
Practically, we have aided our interpretation of blood gas haemoglobin estimations and can apply different levels of confidence depending on the clinical situation. In pragmatic terms, from table 1, 50% of the results for haemoglobin concentration are within 5 g/l, 75% are within 10 g/l, 90% are within 15 g/l and 95% are within 20 g/l.
Previous studies have validated the use of near‐patient testing of haemoglobin concentration in neonates using a haemoglobinometer (HemoCue, Sheffield, UK).9 However, on our unit, this would mean purchasing other equipment and more training for staff. The integration of the haemoglobin estimation into the results provided by the blood gas machines keeps quality control, maintenance and training all within the established budgets and educational packages. In addition, fewer full blood counts may lead to cost savings and less iatrogenic blood loss, potentially reducing transfusion requirements.10
We believe that in a convalescing baby on our unit it may be possible to replace weekly haemoglobin monitoring with point of care haemoglobin measurement. This would require a valid quality control and ongoing maintenance programme (already in place) and repeated evaluations to ensure that there is no drift in the accuracy of the result. In a critically sick baby on our unit a fall of 10–20 g/l in the haemoglobin measurement should at least prompt reassessment of the baby and may even indicate the need for urgent transfusion, depending on the clinical situation. However, point of care testing cannot replace the full blood count as in critical care platelet and white cell counts are often take into account when altering management.
In conclusion, we believe that we have confirmed the use of point of care haemoglobin estimation on our unit. Although it cannot replace a full blood count, it can be seen as an adjunct to neonatal care monitoring. Other units would need to evaluate their own point of care analysers before making any changes.
Footnotes
Competing interests: None.
References
- 1.Price C. Point of care testing. BMJ 20013221285–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tan K, Booth D, Newell S.et al Point‐of‐care testing of neonatal coagulation. Clin Lab Haematol 200628117–121. [DOI] [PubMed] [Google Scholar]
- 3.Drenck N. Point of care testing in critical care medicine: the clinician's view. Clin Chim Acta 20013073–7. [DOI] [PubMed] [Google Scholar]
- 4.Lin J, Strauss R, Kulhavy J.et al Phlebotomy overdraw in the neonatal intensive care nursery. Pediatrics 200010619–24. [DOI] [PubMed] [Google Scholar]
- 5.Widness J. Pathophysiology, diagnosis, and prevention of neonatal anemia. Neoreviews 20001e61–e68. [Google Scholar]
- 6.Widness J, Kulhavy J, Johnson K.et al Clinical performance of an in‐line point‐of‐care monitor in neonates. Pediatrics 2000106497–504. [DOI] [PubMed] [Google Scholar]
- 7.Widness J, Madan A, Grindeanu L.et al Reduction in red blood cell transfusions among preterm infants: results of a randomized trial with an in‐line blood gas and chemistry monitor. Pediatrics 20051151299–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bland J, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986307–310. [PubMed]
- 9.Rechner I, Twigg A, Davies A.et al Evaluation of the HemoCue compared with the Coulter STKS for measurement of neonatal haemoglobin. Arch Dis Child Fetal Neonatal Ed 200286F188–F189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ray J, Post J, Hamielec C. Use of a rapid arterial blood gas analyzer to estimate blood haemoglobin concentration among critically ill adults. Crit Care 2002672–75. [DOI] [PMC free article] [PubMed] [Google Scholar]