Abstract
The pattern of breathing was studied in 13 premature newborns treated by variable‐flow Nasal Continuous Positive Airway Pressure (NCPAP), conventional NCPAP, and nasal cannulae. Compared to constant‐flow NCPAP and nasal cannulae, the variable‐flow NCPAP increases tidal volume and improves thoraco‐abdominal synchrony, suggesting that variable‐flow NCPAP provides more effective ventilatory support than conventional NCPAP or nasal cannulae.
Nasal Continuous Positive Airway Pressure (NCPAP) is used for ventilation weaning in preterm infants. It improves the synchrony of thoracic and abdominal motions,1,2 increases tidal volume1,2 and the end‐expiratory lung volume,1,3 and changes the pattern of breathing.2
The optimal NCPAP method is presently unknown. Very few studies have compared NCPAP systems and their ability to improve lung functions and breathing patterns.3,4 Conventional NCPAP is usually provided by varying the resistance to exhalation while constant gas flow is delivered by a ventilator through nasal prongs. Efficacy of such systems is limited by the pressure drop across the nasal prongs. In contrast, the variable‐flow NCPAP generator delivers variable high‐velocity jet gas flow toward the upper airway to assist inspiration on demand. CPAP is maintained constant by converting kinetic energy of the gas flow to pressure.
To assess which technique of pressure generation most effectively improves lung function, we compared the breathing patterns recorded during variable‐flow NCPAP, conventional constant‐flow NCPAP, and supplemental O2 delivered via nasal cannulae.
Population and methods
Population
Under investigation were spontaneously breathing preterm infants treated with NCPAP or supplemental O2 via nasal cannulae for weaning from mechanical ventilation. Inclusion criteria were: (1) gestational age from 26 to 32 weeks; (2) mild respiratory failure (FiO2<30%). The study was approved by the Institutional research ethics committee. Written informed consent was obtained from the parents.
Methods
All infants were evaluated on each of the three following devices applied for 30 minutes in random order: (1) a variable‐flow NCPAP generator (Infant‐Flow, EME Tricomed, UK) at a pressure of 5 cm H2O; (2) a conventional constant‐flow NCPAP (Baby‐Flow, Draeger, Germany). The Baby‐flow is a small aluminium chamber with short silicone double prongs for the nasal interface and designed to be used with the ventilator Babylog 8000® (Draeger, Germany) set in CPAP mode (5 cm H2O) at the recommended gas flow of 10 l/min; and 3) nasal cannulae (length = 1 cm, internal diameter = 1.5 mm; Kendal, Germany) connected to an air‐O2 blender‐flowmeter (Sechrist, France) set at 2 l/min.
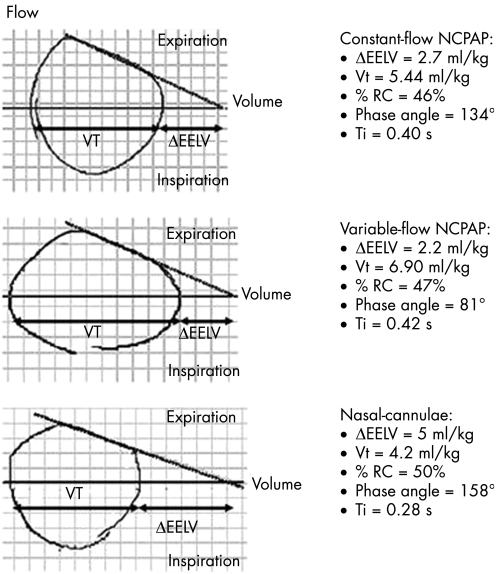
Continuous monitoring of the breathing parameters (Tidal volume (Vt), rib cage contribution to the Vt (%RC), phase angle between abdominal and thoracic motions (θ), respiratory rate (RR), and inspiratory times (Ti)) was obtained from respiratory inductive plethysmography (Respitrace Plus, Sensor Medics, USA) and calibrated by using face mask pneumotachography (Florian, Switzerland). The angle θ is the degree of thoracoabdominal asynchrony—that is, the phase lag between rib cage and abdomen movements during tidal breathing. In the preterm newborn infant, thoracoabdominal asynchrony increases with the respiratory mechanical loading and decreases the ventilatory efficiency of the diaphragmatic work.5 Nasal CPAP was found to improve thoracoabdominal synchrony.1,2,3 Thus, θ may represent a useful marker to compare nasal CPAP devices. The dynamic elevation of end‐expiratory lung volume (ΔEELV) was evaluated from the analysis of the flow‐volume loops. In the preterm infants, to prevent a ventilation/perfusion mismatch, both active contraction of the inspiratory muscles during expiration and expiratory laryngeal narrowing, the EELV was elevated above the static relaxed volume (Vr). ΔEELV represents the difference between EELV level and static relaxed volume. The static relaxed volume was estimated from extrapolation of the linear segment of the flow‐volume curve to zero‐flow, as previously described (see fig 2).2 The regression line was computed by the least‐square method.
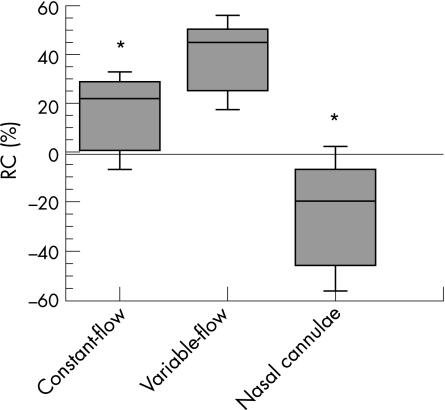
Figure 2 Rib cage contribution to the tidal volume (%RC) measured during constant‐flow Nasal Continuous Positive Airway Pressure (NCPAP), variable‐flow NCPAP, and nasal cannulae. Values are medians (interquartile). *p<0.01, compared with values obtained with variable‐flow NCPAP.
Statistical analysis
The parameters were expressed as means (SD) or medians (interquartile), and compared using repeated measures and factorial analysis of variance (Stat View, California, USA). A p value <0.05 was considered significant.
Results
Nineteen premature infants were enrolled from February to July 2004. Six infants were excluded because of excessive motion artefacts. Thirteen infants were investigated (GA = 29 (1) weeks; BW = 1350±350 g) at a post‐natal age of 3±1 days.
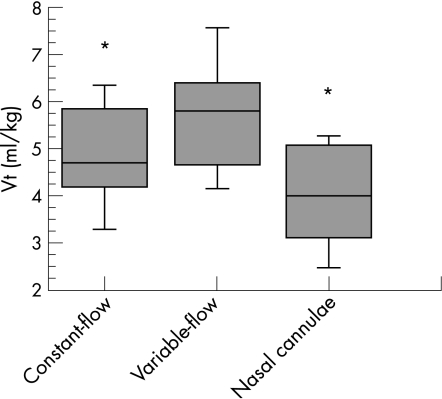
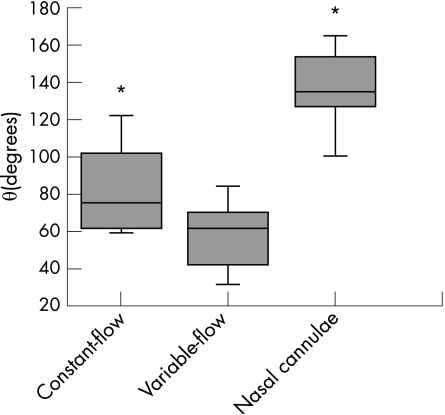
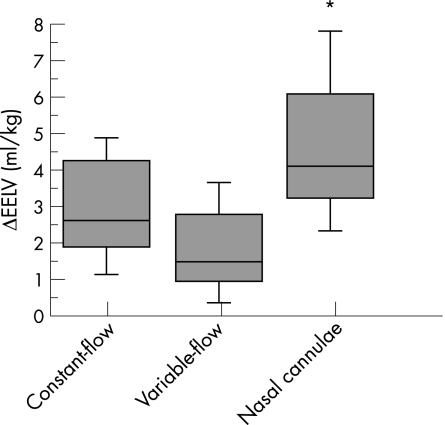
Respiratory rate (RR) and heart rate (HR), systemic blood pressure, FiO2, SpO2, transcutaneous PaCO2, and Ti did not change during the study period (table 1). Mean tidal volume, Vt, and %RC were higher during variable‐flow than during constant‐Flow NCPAP or during nasal cannulae (p<0.05) (fig 1,2). θ was lower with the variable‐flow NCPAP than with the other devices (p<0.05) (fig 3). An individual tracing is presented in fig 4. The mean ΔEELV was lower with the variable‐flow device than with nasal cannulae (p<0.05) (fig 5). However, the mean ΔEELV was similar for the variable‐ and the constant‐flow NCPAP.
Table 1 Changes in respiratory parameters during variable‐flow NCPAP, constant‐flow NCPAP, and nasal cannulae.
| Parameters | Constant‐flow NCPAP | Variable‐flow NCPAP | Nasal cannulae |
|---|---|---|---|
| RR (c/min) | 56 ± 10 | 52 ± 9 | 59 ± 11 |
| HR (b/min) | 145 ± 16 | 143 ± 15 | 139 ± 15 |
| Systemic pressure (mm Hg) | 45 ± 11 | 45 ± 8 | 44 ± 9 |
| SpO2 (%) | 94 ± 3 | 94 ± 2 | 93 ± 2 |
| FiO2 (%) | 26 ± 3 | 25 ± 3 | 26 ± 3 |
| TcPCO2 (mm Hg) | 48 ± 7 | 47 ± 8 | 51 ± 8 |
| Ti (s) | 0.4 ± 0.11 | 0.4 ± 0.09 | 0.4 ± 0.10 |
NCPAP, Nasal Continuous Positive Airway Pressure; RR,
No difference was found for respiratory and heart rate (RR and HR, cycle/min), systemic arterial pressure (systemic pressure, mm Hg), SpO2 (%), FiO2 (%), transcutaneous PaCO2 (TcPCO2, mm Hg), and inspiratory time (Ti, sec) between the different devices. Values are expressed as mean (SD).
Figure 1 Tidal volume (Vt) expressed in ml/kg measured during constant‐flow Nasal Continuous Positive Airway Pressure (NCPAP), variable‐flow NCPAP, and nasal cannulae. Values are medians (interquartile). *p<0.01, compared with values obtained with variable‐flow NCPAP.
Figure 3 Thoraco‐abdominal synchrony expressed as phase angle θ in degrees. Values were measured during constant‐flow Nasal Continuous Positive Airway Pressure (NCPAP), variable‐flow NCPAP, and nasal cannulae. Values are medians (interquartile). *p<0.01, compared with values obtained with variable‐flow NCPAP.
Figure 4 Flow‐volume loops of a representative infant with the constant‐flow Nasal Continuous Positive Airway Pressure (NCPAP), the variable‐flow NCPAP, and with nasal cannulae. Dynamic elevation of end‐expiratory lung volume (ΔEELV) represents the difference between end‐expiratory lung volume level and static relaxation volume. The static relaxation volume can be estimated from extrapolation of the linear segment of the flow‐volume curve to zero‐flow. With variable‐flow NCPAP, the expiratory flow‐volume curve fell linearly to close to the zero‐flow line, consistent with almost complete passive deflation toward the lung volume determined by the passive recoil properties of the respiratory system and by the NCPAP: ΔEELV is low. In contrast, expiratory time was too short to achieve complete lung deflation with nasal cannulae: Such a breathing pattern dynamically elevates EELV. Vt, tidal volume; %RC, rib cage contribution to the tidal volume; θ the phase angle, phase angle between abdominal and thoracic motions; Ti, inspiratory time.
Figure 5 Dynamic elevation of end‐expiratory lung volume (ΔEELV) obtained during variable‐flow NCPAP, constant‐flow Nasal Continuous Positive Airway Pressure (NCPAP), and nasal cannulae. ΔEELV are expressed in ml/kg. Values are medians (interquartile). *p<0.01, compared with values obtained with variable‐flow NCPAP.
Discussion
Previous studies suggested that NCPAP using variable‐flow generator caused greater lung recruitment and lower work of breathing than conventional NCPAP.3,4 Our study clearly shows that the patterns of breathing also differ with the NCPAP system. Increased tidal volume with the variable‐flow NCPAP generator probably results from improved thoraco‐abdominal synchrony and increased contribution of the rib cage to tidal volume. Moreover, low ΔEELV during the variable‐flow NCPAP indicates that the characteristic protective expiratory braking observed in preterm infants is decreased, suggesting effective passive increase in EELV. In contrast, higher ΔEELV with nasal cannulae suggests that the breathing strategy is oriented toward a dynamic elevation of EELV.
Controversies exist on the ability of variable‐flow NCPAP to alter the outcome, despite beneficial effects on the respiratory mechanics and the breathing pattern. In a recent study, no difference in extubation success rate was found between the variable‐flow CPAP and the conventional CPAP groups.6 In our study, O2 need and transcutaneous PaCO2 were similar with the 3 tested NCPAP devices. It is likely that the dynamic volume‐preserving mechanisms may have prevented from lung function impairment, at least for the short study period.
Because of the small sample size, clinical applicability of our data may be limited to a particular population of preterm infants.
Conclusion
Better spontaneous breathing strategy was found with variable‐flow NCPAP compared with constant‐flow NCPAP or with nasal cannulae, as indicated by an increase in the tidal volume, an improved thoraco‐abdominal synchrony, and by a decreased dynamic elevation of end‐expiratory lung volume. These results suggest that variable‐flow NCPAP may provide greater ventilatory support in premature newborns with mild respiratory failure than conventional NCPAP or nasal cannulae.
Acknowledgements
The authors gratefully acknowledge Mr Degas ‐Draeger, France‐ for the technical assistance.
Abbreviations
NCPAP - Nasal Continuous Positive Airway Pressure
ΔEELV - dynamic elevation of end‐expiratory lung volume
EELV - elevation of end‐expiratory lung volume
Footnotes
Competing interests: None.
References
- 1.Elgellab A, Riou Y, Abazine A.et al Effects of nasal continuous positive airway pressure (NCPAP) on breathing pattern in spontaneously breathing premature newborn infants. Intensive Care Med 2001271782–1787. [DOI] [PubMed] [Google Scholar]
- 2.Magnenant E, Rakza T, Riou Y.et al Dynamic behavior of respiratory system during nasal continuous positive airway pressure in spontaneously breathing premature newborn infants. Pediatr Pulmonol 2004371–7. [DOI] [PubMed] [Google Scholar]
- 3.Courtney S E, Pyon K H, Saslow J G.et al Lung recruitment and breathing pattern during variable‐ versus constant‐ flow nasal continuous positive airway pressure in premature infants: an evaluation of 3 devices. Pediatrics 2001107304–308. [DOI] [PubMed] [Google Scholar]
- 4.Pandit P B, Courtney S E, Pyon K H.et al Work of breathing during constant‐and variable‐flow nasal continuous positive airway pressure in preterm neonates. Pediatrics 2001108682–685. [DOI] [PubMed] [Google Scholar]
- 5.Deoras K S, Greenspan J S, Wolfson M R.et al Effects of inspiratory resistive loading on chest wall motion and ventilation: differences between preterm and full‐term infants. Pediatr Res 199232589–594. [DOI] [PubMed] [Google Scholar]
- 6.Stefanescu B M, Murphy W P, Hansell B J.et al A randomized, controlled trial comparing two different continuous positive airway pressure systems for the successful extubation of extremely low birth weight infants. Pediatrics 20031121031–1038. [DOI] [PubMed] [Google Scholar]