Abstract
Purpose
To evaluate whether distance stereoacuity improves following surgery for intermittent exotropia using the Frisby Davis Distance (FD2) and Distance Randot stereotests.
Methods
Eighteen patients (median age 24 years, range 5 to 68 years) with intermittent exotropia were prospectively enrolled. Stereoacuity was measured pre- and 6 weeks post-operatively using the FD2 and Frisby near tests (real depth tests) and Preschool Randot and Distance Randot tests (polaroid vectographs).
Results
Distance stereoacuity measured with the FD2 improved from a median pre-operative value of 80 arc seconds (arcsec) to 40 arcsec post-operatively (P= 0.04) and stereoacuity measured with the Distance Randot improved from a median of nil to 200 arcsec (P= 0.06). In those that had subnormal stereoacuity pre-operatively, there was even more marked improvement in distance stereoacuity (FD2 median nil vs. 40 arcsec, P=0.002; Distance Randot median nil vs. 200 arcsec, P=0.004). Near stereoacuity measured with Frisby and Preschool Randot remained unchanged pre- and post- operatively (median 60 arcsec and 80 arcsec respectively).
Conclusions
There was improvement in distance stereoacuity measured with both the FD2 and Distance Randot stereotests in patients who underwent surgery for intermittent exotropia. The FD2 and Distance Randot may be useful outcomes measures in future clinical trials of interventions for intermittent exotropia.
Introduction
Measurement of distance stereoacuity has previously been used to assess severity of intermittent exotropia and to monitor for deterioration.1-3 Deterioration in stereoacuity has been suggested as a possible indicator of need for surgery in patients with intermittent exotropia and distance stereoacuity has been used as an outcome measure following surgical intervention.3-5
Using older measurement techniques, some authors have reported an improvement in distance stereoacuity following surgery for intermittent exotropia.3-5 Distance stereoacuity, in these studies, was measured using the Baylor Visual Acuity Tester (BVAT) and Binocular Visual System (Mentor, Norwell, MA) equipment is no longer widely available. Two new tests of distance stereoacuity have been recently introduced, the Frisby-Davis Distance (FD2) test6 and the Distance Randot test.7
Using the new FD2 and Distance Randot for measuring distance stereoacuity we have previously reported that stereoacuity is often reduced in patients with intermittent exotropia.2 Based on previous data, we found that stereoacuity was more frequently degraded when measured using the Distance Randot, and we therefore suggested that the Distance Randot appeared to be more sensitive to minimal disruption of binocularity.2 In the present study, we investigated whether distance stereoacuity measured using these two new tests improved following surgery for intermittent exotropia.
Subjects and Methods
Institutional Review Board approval was obtained for this study. All experiments and data collection were conducted in a manner compliant with the Health Insurance Portability and Accountability Act.
Patients
We prospectively enrolled 18 consecutive patients with intermittent exotropia, who were scheduled for surgical intervention. There were 10 males and 8 females ranging in age from 5 to 68 years (median 24 years) with 6 of these patients under 18 years old. Patients with basic type intermittent exotropia (the same deviation at distance and near) or divergence excess exotropia (exotropia greater at distance than near fixation) were included. Patients with convergence insufficiency type exotropia, defined as a near angle ≥ 10 prism diopters greater than the distance angle, and patients with constant exotropia at both distance and near were excluded. Patients were not excluded if they had apparently constant exotropia only at distance (intermittent or phoric at near) or no measurable distance stereoacuity. Five of our 18 patients were initially judged to have constant exotropia in the distance but two of these had measurable FD2 stereo [20 and 80 arc seconds (arcsec)] and one had measurable Distance Randot stereoacuity (60 arcsec), since they could fuse at distance with effort. As we and others have previously reported,2, 3, 8 apparently constant distance exotropia and absent distance stereoacuity are part of the spectrum of intermittent exotropia. Patients were also excluded if they had worse than 20/40 vision in either eye or if they could not comprehend any of the 4 stereoacuity tests. Pre-operative alignment (1 to 23 days before surgery) and post-operative alignment (27 to 66 days after surgery) was measured at near and distance fixation with simultaneous prism and cover test (SPCT) and alternating prism cover test (APCT).
Surgical intervention
Thirteen (72%) of 18 patients underwent unilateral lateral rectus recession and medial rectus resection, 4 patients (22%) underwent three horizontal muscle surgery and 1 patient (5%) had bilateral lateral rectus recessions. Twelve surgeries were performed using adjustable sutures and, when performed this way, the initial distance alignment was set at 2 to 10 pd esotropia post adjustment with the expectation of an exotropic drift.
Stereoacuity
Distance stereoacuity was measured using the FD2 at 3 meters (20 to 200 arcsec) and Distance Randot at 3 meters (60 to 400 arcsec).7, 9, 10 Near stereoacuity was measured at the described test distances for the near Frisby (40 to 400 arcsec) and at 40 centimeters for the Preschool Randot (40 to 800 arcsec).11, 12 Stereoacuity was recorded as “nil” if the largest disparity could not be passed.
Analysis
Stereoacuity thresholds were compared pre- and post-operatively with non-parametric Wilcoxon signed rank tests.
Results
Alignment
Pre-operatively, at distance fixation, the angle of exodeviation ranged from 16 to 60 prism diopters (pd) by APCT (median 32.5 pd). Six weeks post-operatively, the angle of deviation at distance fixation ranged from 12 pd esotropia to 8 pd exophoria by APCT (median 0 pd). Six patients (33%) had a small angle esotropia at distance fixation ranging from 2 to 12 pd (median 3 pd esotropia) measured with SPCT (Table — e-supplement available online at jaapos.org).
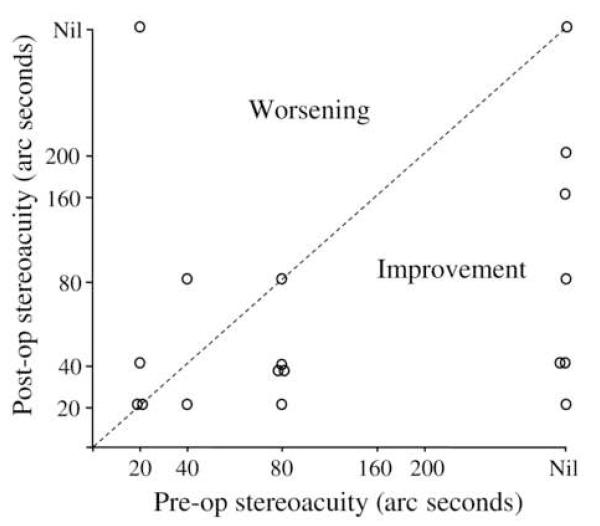
Distance stereoacuity measured using the FD2
Pre-operatively, distance stereoacuity measured using the FD2 ranged from 20 arcsec to nil (median 80 arcsec) with 7 (39%) of 18 patients had no measurable (nil) distance stereoacuity (Figure 1). Post-operatively, distance stereoacuity measured using the FD2 improved in 11 (61%) of 18 patients to an overall median of 40 arcsec (range 20 arcsec to nil, P= 0.04, Figure 1 and Table) and only 2 patients had nil stereoacuity post-operatively. One patient who had nil stereoacuity pre-operatively showed no improvement. One of the patients who developed a post-operative esotropia lost measurable stereoacuity post-operatively. Two other patients appeared to worsen; one from 40 to 80 arcsec and one from 20 to 40 arcsec (Figure 1).
Figure 1.
Pre- and post-operative distance stereoacuity measured using the FD2 stereotest
In order to avoid the potential bias of stereoacuity being unable to improve if the pre-operative stereoacuity was already normal, an additional analysis was performed that included only patients with subnormal stereoacuity. Twelve (67%) of 18 patients had sub-normal distance stereoacuity (i.e., 60 arcsec or worse), pre-operatively, measured using the FD2 and, in this group of patients, FD2 improved from a median of nil pre-operatively, to 40 arcsec post-operatively (P=0.002). Of these 12 patients, 7 (58%) achieved normal stereoacuity post-operatively (Table).
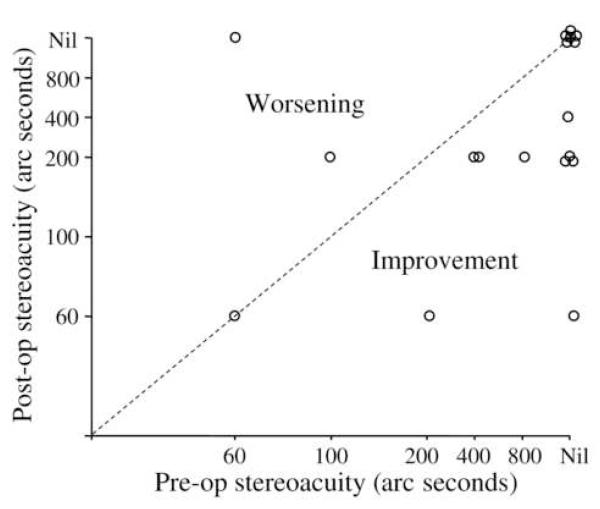
Distance stereoacuity measured using the Distance Randot
Pre-operatively, distance stereoacuity measured using the Distance Randot ranged from 60 arcsec to nil (median nil), with 11 (61%) of 18 patients having no measurable distance stereoacuity (Figure 2). Post-operatively, distance stereoacuity measured using the Distance Randot improved in 9 (50%) of 18 patients to an overall median of 200 arcsec (range 60 arcsec to nil, P= 0.06), with 7 (39%) of 18 patients having no measurable distance stereoacuity post-operatively (Figure 2). Six patients who had no measurable stereoacuity pre-operatively showed no improvement. The one patient who developed a moderate angle esotropia post-operatively and lost stereoacuity measured using the FD2 also lost stereoacuity when measured using the Distance Randot. One other patient appeared to worsen from 100 to 200 arcsec (Figure 2).
Figure 2.
Pre- and post-operative distance stereoacuity measured using the Distance Randot stereotest.
A secondary analysis, analogous to that performed with the FD2, was limited to those patients with sub-normal stereoacuity pre-operatively. In 16 (89%) of 18 patients with sub-normal distance stereoacuity (i.e. 60 arcsec or worse), measured using the Distance Randot, stereoacuity improved from a median of nil to 200 arcsec (P= 0.004), but only 2 (13%) achieved normal stereoacuity (Table).
Near stereoacuity
Pre-operatively, near Frisby was measured in 17 of 18 patients and ranged from 40 arcsec to nil (median 60 arcsec) and only 2 (12%) of 17 patients had no measurable near Frisby stereoacuity pre-operatively. Post-operatively stereoacuity was unchanged (median 60 arcsec) and the 2 patients who had no measurable stereoacuity pre-operatively still had no measurable stereoacuity post-operatively. One patient with the largest post-operative esotropia lost near stereoacuity measured by the near Frisby test (40 arcsec pre-operatively to nil post-operatively).
Pre-operatively, near stereoacuity measured using the Preschool Randot ranged from 40 arcsec to nil (median 80 arcsec) with only 4 (22%) of 18 patients having no measurable near stereoacuity. Post-operatively, median stereoacuity measured using the Preschool Randot was unchanged (median 80 arcsec). Three of the 4 patients who had no measurable stereoacuity pre-operatively still had no measurable stereoacuity post-operatively, although 1 patient acquired 100 arcsec. The one patient mentioned above with the largest post-operative esotropia (12 pd) also had significant reduction in near stereo measured by the Preschool Randot test (60 arc seconds pre-operatively to 400 arc seconds post-operatively).
Discussion
Distance stereoacuity measured using the FD2 and Distance Randot showed overall improvement following surgery for intermittent exotropia. This improvement was particularly evident in those who had subnormal pre-operative distance stereoacuity. Our results using these newly introduced tests of distance stereoacuity are consistent with previous studies3-5 using the older BVAT technology, which is important, because the BVAT hardware is no longer widely available.
Regarding differences between stereoacuity measured using the FD2 and Distance Randot, a greater proportion of patients undergoing surgery for intermittent exotropia achieve normal stereoacuity (60 arcsec or better) post-operatively when measured using the FD2, than the Distance Randot. This finding is consistent with our previous suggestion that the FD2 and Distance Randot seem to measure different aspects of stereoacuity.2, 13 The FD2 is a real world stereotest whereas the Distance Randot test is based on a polaroid vectograph. We have previously suggested that the Distance Randot appears sensitive to mild disruption of the binocular visual system2 possibly related to the dissociation induced by the polarized glasses used for the Distance Randot test. It is also possible that the actual alignment at the moment of testing differs between the FD2 and Distance Randot.
Near stereoacuity was excellent in the majority of patients pre-operatively and this remained essentially unchanged following surgery. Nevertheless, 4 (22%) of 18 patients had no measurable near stereoacuity pre- and post-operatively with either the near Frisby or Preschool Randot. Our findings of near stereoacuity, in intermittent exotropia, are consistent with previous studies where near stereoacuity has been shown to be impaired in a proportion of such patients.5,14 It has been suggested that these patients have continuous central suppression, regardless of exotropic status, which might explain why their stereoacuity did not improve post-operatively.5,14 Central suppression may be illustrated by one of our patients (patient 1 in the Table) who had a micro esotropia at near pre and post-operatively measured using SPCT, which may explain the lack of improvement in stereoacuity. In contrast, pre-operative microtropia does not appear to preclude improvement in distance stereoacuity, for example, patient 14 in the table, who showed a marked improvement in stereoacuity post-operatively.
Regarding surgical overcorrection, 6 patients had an esotropic overcorrection measured at 6 weeks post-operatively (ranging from 2 to 12 pd esotropia by SPCT at distance and 2 to 8 pd esotropia by SPCT at near fixation). A small post-operative esotropia did not preclude excellent stereoacuity; 3 of the 6 patients had normal distance stereoacuity measured using the FD2 and one of the 6 patients had normal distance stereoacuity measured using the Distance Randot. This finding is consistent with previous reports of up to 4 pd esotropia being compatible with fine stereoacuity.15 Nevertheless, patients with larger amounts of post-operative esotropia are at risk of losing their binocular function and in some cases this loss may be permanent.16 One of our patients had a 12 pd post-operative esotropia, with loss of stereoacuity, and was subsequently managed with prism glasses. Correction of the misalignment with prism glasses did not immediately improve stereoacuity. At the latest exam (8 months following surgery) the patient’s esotropia had reduced to 1 pd in the distance and 0 pd at near with recovery of FD2 stereoacuity to 80 arcsec, but Distance Randot stereoacuity remained nil. The risk of losing stereoacuity must be considered when a patient has normal or near-normal stereoacuity pre-operatively. There is much more to gain, and less to lose, in patients with intermittent exotropia who have nil stereoacuity pre-operatively.
There was a group of patients, within our study of intermittent exotropia, who did not show an improvement in distance stereoacuity post-operatively and most of these patients were not esotropic pre- or post-operatively. A potential explanation for the lack of improvement might be central suppression in the absence of a manifest microtropia or other aspects of an underlying abnormal binocular system in intermittent exotropia.
There are a number of limitations to the findings in this study. We had no control group in this study, but it is unlikely that stereoacuity would improve spontaneously to the degree that we found over the duration of the study (immediately pre-operative to 6-weeks post-operative). Nevertheless, the natural history of intermittent exotropia had not been rigorously studied. In our study we found an improvement in distance stereoacuity following surgery for intermittent exotropia but the role of stereoacuity in monitoring intermittent exotropia prior to surgery is still unknown. Further studies are needed to address variability of distance stereoacuity with time, the natural history of intermittent exotropia, and test-retest variability of testing stereoacuity. One weakness of our study is the difference in measurable thresholds between the FD2 and Distance Randot tests, nevertheless, we performed a secondary analysis of the proportion of patients who achieved normal stereoacuity (60 arcsec or better), which confirmed the primary findings of the study. We did not use alternative methods of measuring stereoacuity, such as the Project-O-Chart slides, since our study was focused on two new methods of assessing distance stereoacuity. Finally, our study could have been improved by masking of stereoacuity assessment. Nevertheless, masking of post-operative status would require examiners that were not involved in any aspect of pre-operative care and would require examiners to not look at the patient’s eyes, since redness may still be present at 6 weeks.
Distance stereoacuity measured using the new FD2 and Distance Randot tests improves in most patients following surgery for intermittent exotropia and further studies are required to address the role these tests may play in monitoring intermittent exotropia.
Supplementary Material
Acknowledgments
Supported by: National Institutes of Health Grants EY015799 and EY011751 (JMH), EY005236 (EEB); Research to Prevent Blindness, Inc., New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, MN.
Footnotes
Study was conducted in the Department of Ophthalmology, Mayo Clinic College of Medicine and the Department of Ophthalmology, University of Texas Southwestern Medical Center
Presented in part at the American Association of Pediatric Ophthalmology and Strabismus meeting in Seattle, April 2007
Potential Financial Conflicts: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.von Noorden GK. Binocular Vision and Ocular Motility: Theory and Management of Strabismus. 5th ed Mosby; St Louis, Mo: 1996. pp. 206–96. [Google Scholar]
- 2.Holmes JM, Birch EE, Leske DA, Fu VL, Mohney BG. New tests of distance stereoacuity and their role in evaluating intermittent exotropia. Ophthalmology. 2007;114:1215–20. doi: 10.1016/j.ophtha.2006.06.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stathacopoulos RA, Rosenbaum AL, Zanoni D, Stager DR, McCall LC, Ziffer AJ, et al. Distance stereoacuity. Assessing control in intermittent exotropia. Ophthalmology. 1993;100:495–500. doi: 10.1016/s0161-6420(93)31616-7. [DOI] [PubMed] [Google Scholar]
- 4.O’Neal TD, Rosenbaum AL, Stathacopoulos RA. Distance stereo acuity improvement in intermittent exotropic patients following strabismus surgery. J Pediatr Ophthalmol Strabismus. 1995;32:353–7. doi: 10.3928/0191-3913-19951101-06. [DOI] [PubMed] [Google Scholar]
- 5.Yildirim C, Mutlu FM, Chen Y, Altinsoy HI. Assessment of central and peripheral fusion and near and distance stereoacuity in intermittent exotropic patients before and after strabismus surgery. Am J Ophthalmol. 1999;128:222–30. doi: 10.1016/s0002-9394(99)00079-3. [DOI] [PubMed] [Google Scholar]
- 6.Frisby JP, Davis H, editors. Clinical tests of distance stereopsis: State of the art. Swets & Zeitlinger; Lisse: 2003. pp. 187–90. [Google Scholar]
- 7.Fu VL, Birch EE, Holmes JM. Assessment of a new distance Randot stereoacuity test. J AAPOS. 2006;10:419–23. doi: 10.1016/j.jaapos.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 8.Hatt SR, Haggerty H, Buck D, Adams WE, Strong NP, Clarke MP. Distance Stereoacuity in Intermittent Exotropia. Br J Ophthalmol. 2007;91:219–21. doi: 10.1136/bjo.2006.099465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adams WE, Hrisos S, Richardson S, Davis H, Frisby JP, Clarke MP. Frisby Davis distance stereoacuity values in visually normal children. Br J Ophthalmol. 2005;89:1438–41. doi: 10.1136/bjo.2005.071761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holmes JM, Fawcett SL. Testing distance stereoacuity with the Frisby-Davis 2 (FD2) test. Am J Ophthalmol. 2005;139:193–5. doi: 10.1016/j.ajo.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Frisby JP, Davis H, McMorrow K. An improved training procedure as a precursor to testing young children with the Frisby Stereotest. Eye. 1996;10:286–90. doi: 10.1038/eye.1996.60. [DOI] [PubMed] [Google Scholar]
- 12.Birch E, Williams C, Hunter J, Lapa MC, ALSPAC “Children in Focus” Study Team Random dot stereoacuity of preschool children. J Pediatr Ophthalmol Strabismus. 1997;34:217–22. doi: 10.3928/0191-3913-19970701-08. [DOI] [PubMed] [Google Scholar]
- 13.Leske DA, Birch EE, Holmes JM. Real depth vs randot stereotests. Am J Ophthalmol. 2006;142:699–701. doi: 10.1016/j.ajo.2006.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baker JD, Davies GT. Monofixational intermittent exotropia. Arch Ophthalmol. 1979;97:93–5. doi: 10.1001/archopht.1979.01020010033007. [DOI] [PubMed] [Google Scholar]
- 15.Leske DA, Holmes JM. Maximum angle of horizontal strabismus consistent with true stereopsis. J AAPOS. 2004;8:28–34. doi: 10.1016/j.jaapos.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Pratt-Johnson JA, Barlow JM, Tillson G. Early surgery in intermittent exotropia. Am J Ophthalmol. 1977;84:689–94. doi: 10.1016/0002-9394(77)90385-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.