Hematopoietic cells from patients with acute myeloid leukemia and myelodysplastic syndrome often have defects in DNA repair processes. This study shows that these defects make the cells susceptible to induction of apoptosis by poly ADP-ribose polymerase (PARP) inhibitors.
Keywords: PARP, DNA repair, apoptosis, histone deacetylation inhibition
Abstract
Background
Aberrant or impaired repair of double-strand DNA breaks is a common feature of de novo acute myeloid leukemia and myelodysplastic syndromes. Since poly (ADP-ribose) polymerase (PARP) inhibitors have been recently shown to selectively target cells with defects in double-strand DNA repair, the aim of this study was to explore the possibility of exploiting defects in DNA repair in leukemic cells using PARP inhibitors.
Design and Methods
Leukemic cell lines were exposed to various PARP inhibitors alone and in combination with non-cytotoxic concentrations of DNA methyltransferase inhibitor, 5’ aza-2’-deoxycytidine and/or the histone deacetylase inhibitor, MS275, to test for potentiation of apoptosis with these agents.
Results
PARP inhibitors, KU-0058948 and PJ34, induced cell cycle arrest and apoptosis of primary myeloid leukemic cells and myeloid leukemic cell lines in vitro. Immunofluorescence analysis also revealed that PARP inhibitor sensitivity in these leukemic cells was due to a defect in homologous recombination DNA repair. Addition of 5’ aza-2’-deoxycytidine failed to increase the cytotoxicity of PARP inhibitors. In contrast, MS275 potentiated the cytotoxic effect of KU-0058948 and PJ34 in all PARP inhibitor-sensitive leukemic cells. Immunofluorescence analysis supported the idea that histone deacetylase inhibitors potentiate cytotoxicity by inhibiting DNA repair processes.
Conclusions
On the basis of the data presented here, we suggest that PARP inhibitors can potentially exploit defects in double-strand DNA break repair in leukemic cells, paving the way for testing the therapeutic potential of these agents in myelodysplastic syndromes and acute myeloid leukemia.
Introduction
Despite major advances in the understanding of the biology and pathogenesis of myelodysplastic syndromes (MDS) and acute myeloid leukemias (AML) identification of the most effective and safe form of treatment continues to present a formidable challenge. Standard chemotherapeutic interventions still fail to induce remission in up to 40% of AML patients over the age of 60 years. Furthermore, relapse is common and only 20–30% of mainly young patients enjoy long-term disease-free survival1,2 underscoring the need for novel therapeutic strategies.
Drugs that interfere with epigenetic control of gene transcription, such as DNA methyltransferase inhibitors and histone deacetylase (HDAC) inhibitors, represent new classes of anti-leukemic agents. Clinical trials of the DNA methyltransferase inhibitors, 5’ aza-cytidine and decitabine, using different dose-schedules have confirmed their anti-leukemic activity in both AML and MDS.3 Similarly, HDAC inhibitors have shown promise in phase I/II studies in both myeloid as well as lymphoid malignancies.4 Given the different modes of action of these agents, it is not surprising that a number of clinical trials have reported encouraging results with combinations of both DNA methyltransferase and HDAC inhibitors.4
Aberrant or impaired repair of double-strand DNA breaks is a common feature of congenital genomic instability syndromes, as well as de novo AML and MDS .5,6 We have shown previously that myeloid leukemia cells exhibit pronounced error-prone DNA repair.7 In the present study, we explored the possibility of exploiting defects in DNA repair in leukemic cells using inhibitors of poly ADP-ribose polymerase (PARP). PARP is a single-strand break sensing protein that catalyses the addition of ADP-ribose to surrounding histones and other nuclear proteins.8 PARP inhibitors have been shown to selectively target cells with a defective homologous recombination pathway of double-strand DNA break repair.9 BRCA1, BRCA2, and ATM deficient cells demonstrate extreme sensitivity to PARP inhibitors, resulting in chromosomal instability and death of the responsive cells.10,11 Furthermore, wild-type and BrCA+/− heterozygote clones are resistant to PARP inhibitors, suggesting that these compounds can be used to selectively target cancer cells with abnormal double-strand DNA break repair. We suggest that patients with MDS and AML are prime candidates for PARP inhibitor therapy alone or with DNA methyltransferase and HDAC inhibitors. Combination therapy may further enhance killing of leukemic cells, without an accompanying increase in the cytotoxicity to residual normal hematopoietic cell progenitors, therefore providing yet another novel therapeutic strategy for these difficult to treat hematologic malignancies.
Design and Methods
Drugs
PARP inhibitors PJ34 (IC50: 30 nM) and EB47 (IC50: 45nM) and the HDAC inhibitors, MS275 and apicidin, were purchased from Calbiochem, Nottingham, UK. HDAC inhibitors, trichostatin A, sodium butyrate, and the DNA methyltransferase inhibitor, 5’ aza 2’deoxycytidine (5-aza-2’CdR), were purchased from Sigma Biochemicals, Poole, UK. The PARP inhibitor KU-0058948 (KU) (IC50: 3.4 nM) was donated by Kudos Pharmaceuticals, Cambridge, UK.
Cell culture
The leukemic cell lines HL60, K562, NB4, U937, Kasumi, OC-1, Raji, KG-1 and ME-1 cells were obtained from the American Type Culture Collection. The myelomonocytic/myelodysplastic cell line, P39, was kindly donated by Richard Darley, (University of Wales, Cardiff, UK). Mutz-3 and OCI-AML3 were obtained from the DSMZ, Braunschweig, Germany. Cell lines were cultured at 37° C (5% CO2) in Dutch-modified, RPMI 1640 medium, supplemented with 10% fetal calf serum, 4 mM glutamine and 1% penicillin/streptomycin (all purchased from Sigma-Aldrich Co. Ltd. Poole, UK). Mutz-3 and OCI-AML3 were supplemented with 20% supernatant from the urinary carcinoma cell line, 5637 (DSMZ). Peripheral blood lymphocytes from normal subjects were prepared from heparinized blood using Hypaque-Ficoll (Sigma) gradients and cultured at 1×106/mL in RPMI 1640 supplemented with 10% fetal calf serum, 4 mM glutamine and 1% penicillin/streptomycin. Peripheral blood lymphocytes were stimulated by adding phytohemagglutinin (Sigma) for 48 h, washed several times to remove the phytohemagglutinin, and then cultured in 1 U/mL of interleukin-2 for a maximum of 14 days. For primary cell cultures, bone marrow aspirates and peripheral blood were taken from patients with AML. Mononuclear cells were extracted using Hypaque-Ficoll (Sigma) gradients and cultured at 1×106/mL in RPMI 1640 supplemented with 20% fetal calf serum, 4 mM glutamine, 1% penicillin/streptomycin, 10 ng interleukin-3 and 20 ng stem cell factor for 10 days. All primary AML samples from patients contained between 90–100% AML blasts, as determined by May-Grünwald-Giemsa staining and CD34+ phenotyping. Approval for this research was obtained from King’s College Hospital Local Research Ethics Committee before the study was started. Written informed consent was obtained in accordance with the Declaration of Helsinki prior to blood or bone marrow sample collection. The World Health Organization French American British classification of AML for each patient is listed in Online Supplementary Table S1.
Immunofluorescence
Immunofluorescence studies were performed as described previously.12
Cell cycle analysis
Drugs were added to log phase cells. At the indicated times, aliquots of 2×105 cells were taken and centrifuged at 400xg for 10 min. The supernatant was aspirated and then 70% (v/v) ethanol (at −20°C) was added to the cells and gently vortexed. The cell suspension was again centrifuged at 400xg for 10 min. The supernatant was aspirated and then 1 mL of staining solution (phosphate-buffered saline plus 5 ng fluorescein isothiocyanate, 40 μg propidium iodide, 500 μg RNAase) was added. Samples were analyzed using a FACScan flow cytometer (Becton Dickinson, Franklin Lakes, NJ, USA). An apoptotic index was derived by calculating the percentage sub-G1 events as a fraction of the total sub-G1 + G1 events.
Annexin V staining
Annexin V staining was used as a marker of apoptosis evaluated by FACS analysis. Following exposure to the drugs, cells were incubated with anti-annexin V-fluorescein isothiocyanate and propidium iodide and analyzed by FACS immediately.
Cell survival assays
For cell lines, soft agar, clonogenic assays were performed. Cells were incubated with or without inhibitors in 2.5% bacto-agar (DIFCO) in culture medium. Cells were then seeded to evaluate colony formation. After more than 12 days, viable colonies were fixed in methanol, visualized by staining with MTT solution in phosphate-buffered saline and counted. The plating efficiency of cells exposed to the same concentration of DMSO and untreated controls was determined. For primary cells (AML or peripheral blood lymphocytes) cell survival was determined using trypan blue exclusion analysis. Counts were performed daily for a period of 5 days after addition of the drugs. Non-cytotoxic concentrations of inhibitor were calculated from the dose-response curves constructed from cell survival assays.
Cell staining
Cells were incubated with and without treatment for 7 days. Cells were then cytopspun onto glass slides, fixed in ethanol and stained with May-Grünwald-Giemsa. Images were taken at ×40 magnification
Preparation of nuclear extracts
Nuclear extracts were prepared based on the Sigma protocol (Sigma Biochemicals, Poole, UK). The nuclear extracts were dialysed for 2 X 3 h against E buffer (20 mM Tris-HCl pH 8.0, 0.1 mM KOAc, 20% (v/v) glycerol, 0.5 mM EDTA and 1 mM DTT, Sigma). Finally, nuclear extracts were fast-frozen and stored at −80°C.
Assay of PARP activity
PARP enzyme activity was quantified using the PARP universal colorimetric assay kit (R & D Systems Ltd., Abingdon, UK). This assay measures the incorporation of biotinylated ADP-ribose onto histone proteins bound to a 96-well plate, detected by streptavidin-conjugated horse-radish peroxidase, followed by the addition of a horseradish peroxidase substrate. PARP inhibitors were incubated with the recombinant human PARP enzyme prior to detection. PARP inhibitors were also added to cells prior to nuclear extraction to test for abrogation of cellular PARP activity.
Assay of histone deacetylase activity
HDAC activity was quantified using the HDAC colorimetric assay kit (Biomol, PA, USA). Color de LysTM substrate was incubated with nuclear extract from the P39 leukemic cell line or the Hela nuclear extract, provided with the kit, as a source of HDAC activity. Inhibitors of HDAC activity were incubated with the nuclear extract and substrate prior to the colorimetric assay.
Assay of DNA methyltransferase activity
The activities of DNA methyltransferase 1 and DNA methyltransferase 3b were quantified using a colorimetric assay kit (Epigentek, NY, USA) according to the manufacturer’s instructions. Nuclear extracts of KG-1 and P39 treated with or without 5-aza-2’CdR were prepared.
NAD+/NADH quantification
Total cellular NAD+/NADH levels were assayed using a colorimetric assay kit (Biovision, CA, USA) according to the manufacturer’s instructions.
Bisulfite genomic sequencing
DNA was treated with bisulfite using the Epitect conversion kit (Qiagen, Crawley, UK) and 20 ng were amplified using specific primers for the CDKN2B (p15) promoter. The forward primer sequence, p15F (GGT TTT TTG GTT TAG TTG AAA A) and reverse primer sequence p15R (GGT AGT GGT GAA TAT TTT TAA AAT ATT AGT) would amplify a region of 287 bp, −43 to +243 across the p15 promoter encompassing 30 CpG sites. The polymerase chain reaction conditions were 94° C for 15 min, then (94°C, 30 sec, 55°C, 30 sec, 72°C 30 sec) for 45 cycles plus extension at 72° C for 10 min. The polymerase chain reaction product was cloned into the TOPO TA cloning vector (Invitrogen, Paisley, UK) and, after E. coli transformation, eight colonies were picked from each treatment for sequencing.
Evaluation of the effects of drug combinations
The data from cell survival assays used to construct the dose-response curves were then used to determine the effects of combinations of drugs. Varying concentrations of one drug were used with varying concentrations of the other combination drug at non-cytotoxic or cytotoxic doses. Calcusyn for Windows (Cambridge, UK) software for dose-effect analysis was used to determine whether there were synergistic, additive or antagonistic effects between drugs in combination.
Results
Myeloid leukemia cells are sensitive to PARP inhibitors
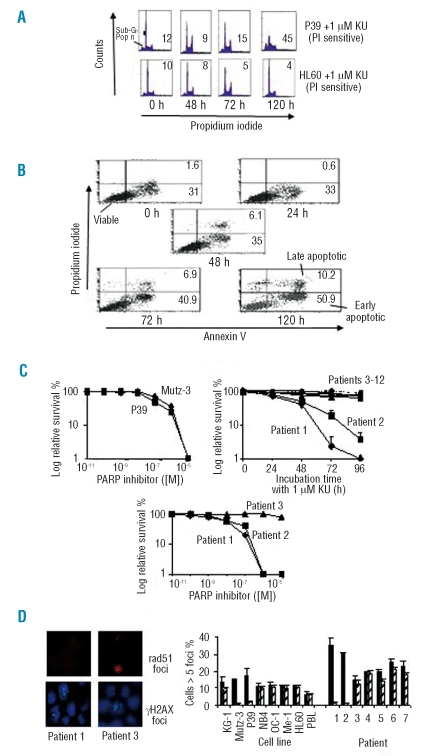
AML and MDS cells are characterized by chromosomal instability that is thought to be associated with defects in DNA repair.5,6,7 We, therefore, investigated the possibility that these cells might be sensitive to PARP inhibitors by exposing a panel of exponentially growing leukemia cell lines to these drugs. When the myelomonocytic/ myelodysplastic cell line, P39, and the acute promyelocytic leukemic-like cell line, HL60, were exposed to KU, we observed an accumulation of cells in S phase and an increase in the G2/M population, features characteristic of stalled DNA replication and DNA damage (Figure 1A, n=3). However, while HL60 recovered by 96 h and then appeared to have a normal cell cycle profile, P39 showed a sizable sub-G1 population (apoptotic index, inset Figure 1A), which suggests continued sensitivity to PARP inhibitors. Apoptotic responses were also recorded using 100 nM KU (Online Supplementary Figure S1A). Furthermore, using an annexin V marker for apoptosis, P39 exhibited significant apoptosis by 48 h which continued to increase for up to 120 h (Figure 1B, n=3, Table 1). The clonogenic survival assay revealed that P39 and the AML cell line, Mutz-3, were very sensitive to KU (Figure 1C, n=3). By contrast, the acute promyelocytic leukemia cell lines, HL60 and NB4, the chronic myeloid leukemia transformed to erythroleukemia cell line, K562, the lymphoma cell line, Raji, the AML lines, ME-1, OCI-AML3, Kasumi-1, U937, OC-1 and normal peripheral blood lymphocytes were insensitive to KU at the same concentrations (Online Supplementary Figure S2A). We next added PARP inhibitors to a panel of primary cells from AML patients. We found that two from a total of 12 cell samples from patients with AML were extremely sensitive to 1 μM KU (Figure 1C) using the trypan blue exclusion assay to determine cell numbers. Furthermore, sensitivity to KU in these two AML patients was at least 2-fold greater than that shown for PARP-sensitive cell lines (Figure 1C).
Figure 1.
The effect of PARP inhibitors on leukemic cells with defective DNA repair. A ( ) 1 μM KU was added to cells for 120 h and the cells were then analyzed by flow cytometry. The frequency of apoptotic cells was determined by estimating the cells in the sub-G1 compartment (lower left quadrant). The apoptotic index (sub-G1 population as a fraction of sub-G1 + G1 populations) is shown in the right inset. (B) 1 μM KU was added to P39 for 120 h before the cells were treated with annexin V-fluorescein isothiocyanate (FL-1, X-axis) and propidium iodide (FL-2, Y-axis). The figures show the percentages of early and late apoptotic cells in the population. (C) The effect of PARP inhibitors on cell survival. Cell survival was assessed by a soft agar clonogenic assay in cell lines and trypan blue exclusion in primary cells. Cells were continuously exposed to PARP inhibitors. KU was added at variable concentrations to human leukemic cell lines, P39, Mutz-3 and cells from AML patients. 1 μM KU was also added to cells from AML patients 1–12 continuously for 5 days and the cells then analyzed by trypan blue exclusion assay. (D) Immunostaining of nuclei from leukemic cells treated with 1 μM KU for 24 h. Cells were probed for γH2AX-P foci (green stain), rad51 foci (red stain) and nuclei were stained with DAPI (blue). The figure shows the frequency of cells displaying γH2AX-P foci(%) (black bars) or rad51 foci(%) (diagonal bars), as detected by immunofluorescence following addition of KU. More than 300 nuclei were counted per experiment, n=3.
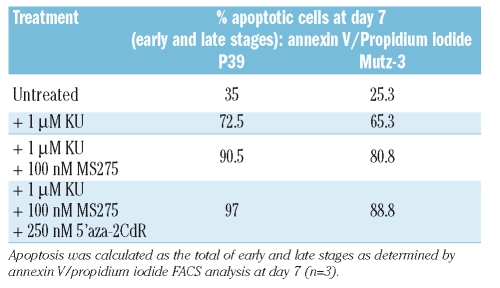
Table 1.
Apoptosis induced in P39 and Mutz-3 cells by 1 μM KU, 100 nM MS275 and 250 nM 5’ aza 2’ CdR, as indicated.
Immunocytochemical analysis was used to determine whether PARP inhibitor sensitivity was attributable to defective DNA repair by homologous recombination. The cell lines that were sensitive to PARP inhibitors, namely P39 and Mutz-3, and the cells from the two PARP inhibitor-sensitive AML patients demonstrated increased γH2AX phosphorylation foci compared to PARP inhibitor-insensitive cells (Figure 1D, Online Supplementary Figure S1B, p<0.01, n=3). Furthermore, P39, Mutz-3 and the two cell samples from patients with AML also demonstrated decreased rad51 foci compared to resistant cell lines and the remaining AML patients’ cells suggesting that the sensitivity to PARP inhibitors was the result of homologous recombination deficiencies in these cells (Figure 1D, Online Supplementary Figure S1B; p<0.01, n=3). In addition, our data also showed that γH2AX phosphorylation was significantly increased in all AML patients’ cells compared to cell lines regardless of their sensitivity to PARP inhibitor (Figure 1D, Online Supplementary Figure S1B p<0.01, n=3).
The cellular response to the combination of PARP inhibitors with either 5’-aza-2’-deoxycytidine or the histone deacetylase inhibitor MS275
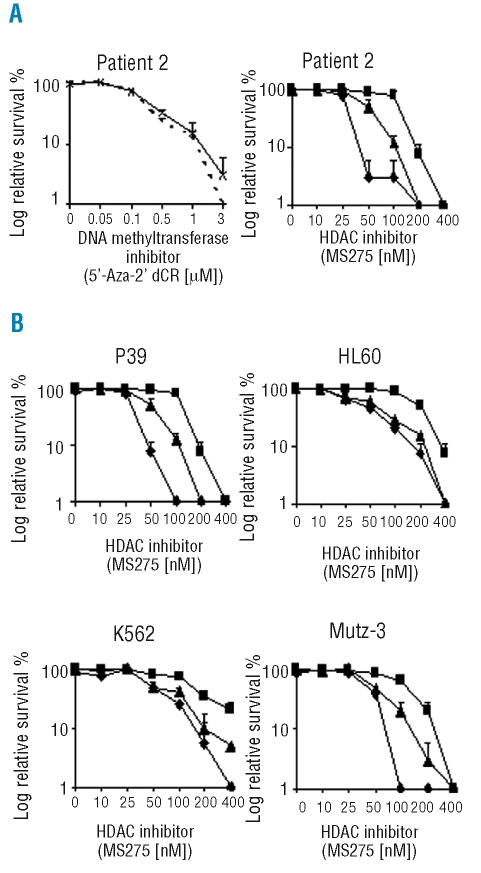
We investigated the possibility that PARP inhibitors might potentiate the cytotoxic responses to DNA methyltransferase or HDAC inhibitors, by adding KU in combination with 5-aza-2’CdR or MS275, respectively. Cells from AML patient n. 2 (PARP inhibitor-sensitive) were subjected to a range of 5-aza-2’CdR concentrations added 48 h prior to a non-cytotoxic concentration of KU (5 nM). Figure 2A shows that addition of KU to 5-aza-2’CdR added 48 h previously resulted in no potentiation of cytotoxicity compared to treatment with 5-aza-2’CdR alone. Addition of a non-cytotoxic concentration of KU (10 nM) to P39, HL60 and Mutz-3 also failed to potentiate the cytotoxicity of 5-aza-2’CdR (Online Supplementary Figure 2B, n=3). Addition of 5-aza-2’CdR 24 h and simultaneously with KU again failed to potentiate cytotoxicity (Online Supplementary figure S1C). Similarly, adding a non-cytotoxic concentration of 5-aza-2’CdR in combination with increasing concentrations of KU failed to have a significant effect on the cytotoxicity produced by KU alone in P39, HL60 and Mutz-3 cell lines (Online Supplementary Figure S2C, n=3). Addition of a non-cytotoxic dose of 5-aza-2’CdR 24 h and simultaneously with KU again failed to potentiate cytotoxicity (Online Supplementary Figure S1D). The combination index (CI) of 5-aza-2’CdR + KU in P39 cells was between 0.8–1.25, which is suggestive of an additive effect of KU on 5-aza-2’CdR cytotoxicity (Table 2, Online Supplementary Figure S3A). Similarly, adding a non-cytotoxic concentration of 5-aza-2’CdR in combination with increasing concentrations of KU failed to have a significant effect on the cytotoxicity produced by KU alone in P39, HL60 and Mutz-3 cells (Table 2).
Figure 2.
The effect of a non-cytotoxic concentration of PARP inhibitor in combination with 5’ aza 2’ dCR and/or MS275. (A) Trypan blue exclusion assays were used to determine cell survival in cells from patient n. 2 with primary AML. The cells were cultured with 5 nM KU and varying concentrations of 5’ aza 2’ dCR and/or MS275 continuously for 5 days. KU + 5’ aza 2’ dCR (dashed line), 5’ aza 2’ dCR alone (crosses and solid line), 5 nM KU + MS275 (triangles), 5’ aza 2’ dCR + KU + MS275 (diamonds), and MS275 alone (squares). (B) Soft agar clonogenic assays were used to determine cell survival in leukemic cell lines in response to non-cytotoxic concentrations of PARP inhibitor alone or in combination with MS275. The cells were exposed continuously for 12–14 days to 10 nM KU and 250 nM 5’ aza 2’ dCR with varying concentrations of MS275. The figure shows cell survival in the presence of KU + MS275 (triangles), 5’ aza 2’ dCR + KU + MS275 (diamonds), and MS275 alone (squares) in P39, HL60, K562 and Mutz-3 cells.
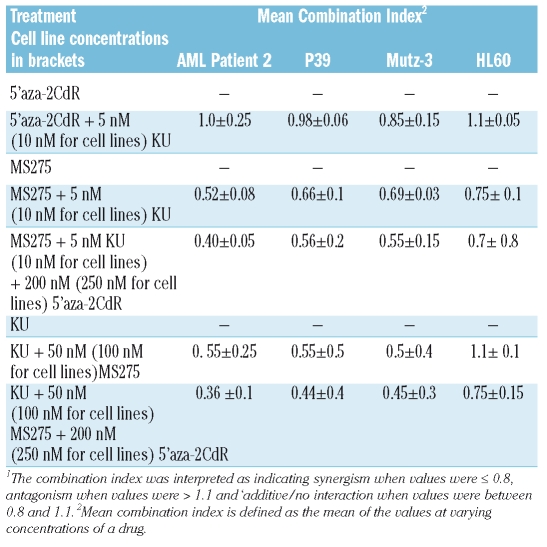
Table 2.
Evaluation of synergy. The relationship between drugs in combination was evaluated using dose-response curves determined through cell survival assays. Calcusyn software was used to determine the combination index1.
Addition of 5 nM KU to increasing concentrations of the HDAC inhibitor, MS275, potentiated the cytotoxic effects of MS-275 by 2-fold (Figure 2A, n=3) in the cells from AML patient n. 2. Non-cytotoxic concentrations of KU (10 nM) also potentiated the cytotoxic effect of MS275 in P39, HL60, K562 and Mutz-3 cells (Figure 2B, n=3). Non-cytotoxic concentrations of KU (10nM) also potentiated the cytotoxic effect of MS275 in P39, HL60, K562 and Mutz-3 cells (Figure 2B, n=3). The CI for MS275 + a non cytotoxic dose of KU was less than 0.5 suggestive of a very strong synergistic relationship between the two compounds (table II, Online Supplementary Figure S3B). Furthermore, addition of a non-cytotoxic concentration (250 nM) of 5-aza-2’CdR added 48 h previously, and KU (10 nM) to MS275 potentiated the cytotoxic response more than the combination of KU and MS275 in all cell lines studied (Figure 2B). The CI for MS275 + a non-cytotoxic dose of KU and 5-aza-2’CdR was less than 0.8, which is suggestive of a synergistic relationship between the three compounds (Table 2, p<0.005, n=3). Similarly, addition of a non-cytotoxic concentration of 50 nM MS275 (100 nM for cell lines) in combination with increasing concentrations of KU, resulted in potentiation of cytotoxicity in myeloid leukemic cells that were only sensitive to PARP inhibitors (those from AML patients n. 1 and n. 2 and the P39, and Mutz-3 cell lines) and not in HL60 cells (PARP inhibitor-insensitive). (Figures 3A,B, Online Supplementary Figure S2D, n=3). The CI for KU + a non-cytotoxic dose of MS275 was less than 0.8, suggesting a synergistic relationship between the two compounds (Table 2, Online Supplementary Figure S3C). Furthermore, a non-cytotoxic concentration (200 nM, 250nM for cell lines) of 5-aza-2’CdR added 48 h prior to a combination of KU and MS275 was able to further potentiate cytotoxicity. The CI for KU + a non-cytotoxic dose of MS275 and 5-aza-2’CdR was less than 0.8, suggesting a synergistic relationship between the three compounds (Table 2, p<0.05, n=3). The sequence of drug addition also appears to be critical as addition of 5-aza-2’CdR at the same time or 24 h prior to KU and MS275 significantly reduced the increase in cytotoxicity (Online Supplementary Figure S1E and S1F).
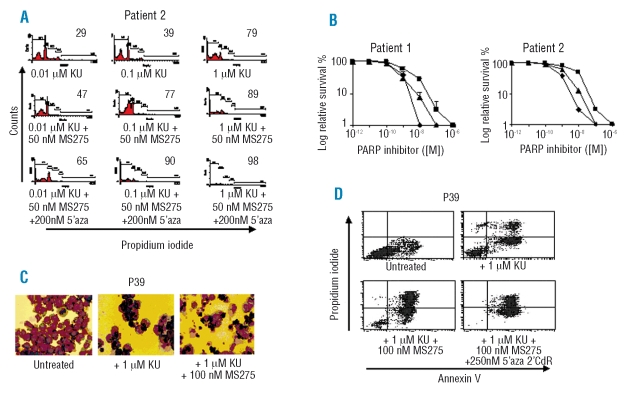
Figure 3.
The effect on leukemic cells of the PARP inhibitor, KU, in combination with non-cytotoxic concentrations of 5’-aza-2’-dCR and/or HDAC inhibitor. (A) The effect of the PARP inhibitor, KU, in combination with the HDAC inhibitor, MS275, and with 5’-aza-2’-dCR on primary AML cells. KU was added at variable concentrations to cells from AML patient # 2 continuously for 5 days with 50 nM MS275 and 200 nM 5’-aza-2’-dCR or KU alone and the cells were then analyzed by flow cytometry. The apoptotic index (sub-G1 population as a fraction of sub-G1 + G1 populations) is shown in the right inset. (B) Trypan blue exclusion assays were used to determine cell sur vival in primary AML cells from patient # 2 exposed to KU, MS275 and 5’-aza-2’-dCR. Cells from AML patients # 1 and # 2 were exposed continuously for 5 days to 50 nM MS275 and 200 nM 5’-aza-2’-dCR with varying concentrations of KU. KU + MS275 (triangles), 5’-aza-2’-dCR + KU + MS275 (diamonds), and KU alone (squares). (C) P39 cells were cultured in 1 μM KU, 1 μM KU + 100 nM MS275 or left untreated for 7 days. At 7 days cells were cytospun onto slides and stained with May-Grünwald stain. Images were taken at X40 magnification. (D) 1 μM KU, 100 nM MS275 and 250 nM 5’-aza-2CdR were added as indicated to P39 cells for 7 days before the cells were treated with annexin V-fluorescein isothiocyanate (FL-1, X-axis) and propidium iodide (FL-2, Y-axis).
Using bisulfite sequencing we confirmed that the non-cytotoxic concentration of 5-aza-2’CdR partially induced promoter demethylation of the p15 gene in KG-1 cells. However, DNA methyltransferase 1 and 3b activities were fully abrogated (data not shown). Giemsa staining of P39 cells after 7 days of incubation with KU and MS275 revealed a substantially decreased number of cells and a significant number of apoptotic cells compared to cells treated with KU alone (Figure 3C). These results were also confirmed by annexin V/propidium iodide FACS analysis (Figure 3D, Table 1) which showed that MS275 significantly potentiated PARP inhibitor cytotoxicity in P39 and Mutz-3 cells (p<0.01, n=3) and addition of a non-cytotoxic dose of 5-aza-2’CdR 48 h previously increased the potentiation still further p<0.05, n=3). Immunocytochemical analysis also revealed that P39 and Mutz-3 cells demonstrated substantially increased γH2AX phosphorylation foci in response to adding a non-cytotoxic concentration of MS275 (100 nM) in combination with 100 μM KU, compared with those produced in response to treatment with 100 μM KU alone (Figure 4A,B, p<0.0001). Significantly, a non-cytotoxic concentration of 5-aza-2’CdR in combination with 100 μM KU did not increase γH2AX phosphorylation foci, compared with those produced by treatment with 100 μM KU alone (Figure 4A,B, n=3).
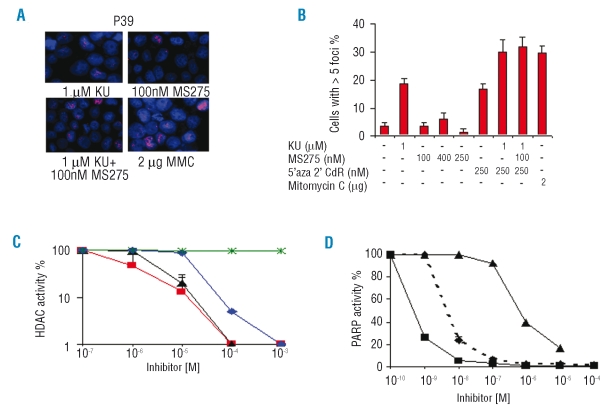
Figure 4.
The effect of PARP and HDAC inhibitors on γH2AX-P foci, as indicators of double-strand DNA break repair. (A) Immunostaining of nuclei (DAPI stained in blue) from P39 cells treated for 24 h with 1 μM KU (top left panel); 100 nM MS275 (top right panel); 1 μM KU + 100 nM MS275 (bottom left panel) and 2 μg mitomycin C (MMC) (bottom right panel). Cells were probed for γH2AX-P foci (red stain). Representative nuclei are shown. (B) Frequency of cells displaying γH2AX-P foci (%), as detected by immunofluorescence, following drug addition. More than 300 nuclei were counted per experiment, n=3. C,D PARP inhibitors do not block HDAC enzyme activity, nor do HDAC inhibitors block PARP enzyme activity. (C) HDAC enzyme activity assays were conducted according to the manufacturer’s instructions with increasing concentrations of MS275 (red line), trichostatin A (black line), apicidin (blue line) and KU (green line). (D) PARP enzyme activity assays were conducted according to the manufacturer’s instructions with recombinant PARP enzyme using increasing concentrations of MS275 (triangles) and KU (squares) or nuclear extracts of patients’ samples (PARP-sensitive and insensitive) as the source of PARP enzyme activity (diamonds, dashed line) and increasing concentrations of KU. PARP activity in the patients’ samples is the mean of the activity in five patients.
PARP inhibitors do not inhibit histone deacetylase activity directly and the histone deacetylase inhibitor MS275 does not inhibit PARP activity directly
It was conceivable that the observed potentiation of MS275 cytotoxicity was due to a direct effect of the PARP inhibitor on HDAC activity. We, therefore, added increasing concentrations of KU or PJ34 to the HDAC assay. We observed that even at millimolar concentrations, there was no inhibition of HDAC activity (Figure 4C, n=3). In contrast, MS275 and standard inhibitors of HDAC activity, such as trichostatin A and apicidin, were able to inhibit HDAC activity at nanomolar concentrations (Figure 4C). Potentiation of cytotoxicity was also not attributable to an inhibition of PARP activity by MS275. This HDAC inhibitor was only able to modify the PARP enzyme activity at ten times the concentration used in the combination experiment (Figure 4D). By contrast, KU was able to abrogate recombinant human PARP activity at nanomolar concentrations used in the combination experiments. Nuclear extracts were also prepared from AML patients’ samples to determine equivalent PARP enzyme activity across samples. Figure 4D shows that the standard error in PARP activity between patients’ samples is very low suggesting there is little difference in PARP enzyme activity between PARP inhibitor-sensitive and insensitive samples from AML patients (Figure 4D, n=3). There was also a 10-fold decrease in sensitivity using PARP derived from patients’ samples compared to recombinant PARP enzyme. Furthermore, total NAD/NADH levels were assayed to determine whether the level of cellular NAD and NADH influenced PARP activity. From nuclear extracts prepared from AML samples we saw that all AML samples demonstrated equivalent levels of total NAD/NADH (data not shown).
Discussion
In this report we show, to our knowledge for the first time, that the PARP inhibitors KU, PJ34 and EB47 exert specific cytotoxic effects in leukemia cells. Cells from two patients with AML, the MDS/AML cell line, P39, and the AML line, Mutz-3, demonstrated abnormal cell cycle profiles, increased double-strand DNA damage and subsequent apoptosis. The HDAC inhibitor, MS275, was also able to potentiate the cytotoxicity of the PARP inhibitors, while addition of 5-aza-2’CdR 48 h prior to MS275 and KU treatment was able to further potentiate cell killing. We suggest that PARP inhibitors alone or in combination with DNA methyltransferase and HDAC inhibitors offer a viable therapeutic option for the treatment of MDS and AML.
Patients with MDS and AML are predominantly over 60 years of age and the rates of both treatment-related mortality and morbidity following intensive chemotherapy are high; as a consequence, treatment options are often limited.1,2 Reduced intensity conditioned allogeneic stem cell transplantation is the only potentially curative treatment, but this is often associated with significant transplant-related mortality and graft-versus-host disease.1,2 The therapeutic effectiveness of DNA methyltransferase and HDAC inhibitors in the treatment of MDS and AML offers hope for patients who are otherwise ineligible for intensive chemotherapy. Potentially, PARP inhibitors, by virtue of their selectivity for malignant cells and lack of toxicity for non-malignant cells, offer attractive options. Cells from two of 12 AML patient and two of 11 leukemia cell lines were sensitive to the PARP inhibitors, suggesting that responsiveness to PARP inhibitor therapy is greater in certain subgroups of myeloid leukemia. The heterogeneity in the degree of cytotoxicity in our cell lines upon exposure to PARP inhibitors testify to this. For example, ‘acute promyelocytic-like’ cell lines, NB4 and HL60, were insensitive to PARP inhibitors, while the most sensitive cell line was P39, a MDS-derived cell line regarded as less transformed and thus more chemosensitive than the AML cell lines. In this respect, we saw that primary cells were significantly more sensitive to PARP inhibitors than cell lines, suggesting that as the leukemic clone progresses, it acquires genomic changes that render the cells less apoptotic and thus more resistant to PARP inhibitors.
AML and MDS are good candidates for PARP inhibitor therapy, exploiting the defects in DNA repair and chromosomal stability in leukemic cells. Chromosomal instability disorders such as Fanconi’s anemia and Bloom’s syndrome also have an increased propensity to transform into MDS and AML.6,13 The aberrant genes in these syndromes are components of the homologous recombination pathway of double-strand DNA break repair. In addition, mutations in other double-strand DNA break repair components, such as NBS1, and DNA ligase IV, have also been detected in leukemia.14,15 We and others have16,17 demonstrated sensitivity to PARP inhibitors in NBS−/−, and Fanconi’s anemia deficient cells, FancA−/− and FancD2−/− cells at equivalent concentrations to those used in our assays and we have also shown previously that leukemic cells display increased and error-prone non-homologous end-joining of double-strand DNA break repair.7 Loss of a non-homologous end-joining factor, DNA-PK, can sensitize cells to inhibitors of PARP.11 In these respects leukemic cells are suitable candidates for PARP inhibitor therapy.
The potentiating effect of KU and the HDAC inhibitor, MS275, has potential clinical importance, especially given that MS275 is currently being tested in clinical trials for the treatment of MDS and AML. HDAC inhibitors have previously been shown to have synergistic effects with DNA methyltransferase inhibitors and to induce apoptosis or differentiation through the re-expression of silent genes.18 Inhibition of methylation must occur before reactivation of gene expression, given that the addition of 5-aza-2’CdR 48 h prior to KU and MS275 significantly enhanced cell death. Potentiation of PARP inhibitor induced cell death through the addition of 5-aza-2’CdR and MS275 could be due to the re-expression of pro-apoptotic genes. Furthermore, both PARP and HDAC inhibitors have previously been shown to potentiate cellular sensitivity to DNA damaging chemotherapeutic agents19 and to irradiation, respectively.20,21 The dramatic increase in γH2AX phosphorylation upon simultaneous exposure to both PARP and HDAC inhibitors also points to an inhibition of DNA repair by HDAC inhibitors. We have previously shown that HDAC inhibitors cause S-phase specific, excessive DNA damage in leukemic cells,12 while other groups have shown that HDAC inhibitors radiosensitize tumor cells by suppressing DNA repair.17 Thus HDAC activity should be considered an essential component of the cellular response to certain types of DNA damage.
The therapeutic approach offered by the use of PARP inhibitors is exciting, exploiting a specific deficiency in leukemic cells. Targeted therapy of this type obviates the side-effects associated with standard chemotherapy. At least five PARP inhibitors have already entered clinical trials for the treatment of solid tumors.22 Initial reports have suggested that there is very little toxicity associated with these drugs alone or in combination with temozolomide.22 Moreover, PARP inhibitors in combination therapy could reduce the nephrotoxocity associated with cisplatin.23 Further insights into PARP sensitivity would also delineate distinct subgroups of leukemia that are responsive to treatment. Thus, understanding the basic cellular and molecular biology of leukemia is vital to the development of methods of treatment based on therapies targeting genetic lesions in MDS and AML. Our data support the feasibility of phase I clinical trials involving PARP inhibitors alone and in with combination HDAC inhibitors in AML and high-risk MDS.
Footnotes
The online version of this article contains a supplementary appendix.
Authorship and Disclosures
All authors contributed equally to this paper.
TG: conception, design, majority of experimental procedures, writing, editing; SS: Conception, design, editing; LMP, NT, NL: experimental procedures; FF: conception, editing; GM: conception, design, editing.
The authors reported no potential conflicts of interest.
Funding: this work was funded by the National Health Service (NHS). Terry Gaymes is employed by the NHS. Lee Macpherson is funded by the Burton group. Natalie Twine is funded by the Elimination of Leukaemia Fund (ELF).
References
- 1.Morgan MA, Reuter CW. Molecularly targeted therapies in myelodysplastic syndromes and acute myeloid leukemias. Ann Hematol. 2006;85:139–63. doi: 10.1007/s00277-005-0051-7. [DOI] [PubMed] [Google Scholar]
- 2.Gingerich J, Bow EJ. Approach to the complications of treatment for acute leukemia in the elderly. Semin Hematol. 2006;43:134–43. doi: 10.1053/j.seminhematol.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 3.Silverman LR, Mufti GJ. Methylation inhibitor therapy in the treatment of myelodysplastic syndrome. Nat Clin Pract Oncol. 2005;1:12–23. doi: 10.1038/ncponc0347. [DOI] [PubMed] [Google Scholar]
- 4.Gore SD. Combination therapy with DNA methyltransferase inhibitors in hematologic malignancies. Nat Clin Pract Oncol. 2005;1:30–5. doi: 10.1038/ncponc0346. [DOI] [PubMed] [Google Scholar]
- 5.Fenaux P, Morel JL. Cytogenetics of myelodysplastic syndromes. Semin Hemat. 1996;33:127–38. [PubMed] [Google Scholar]
- 6.Taniguchi T, D’Andrea AD. Molecular pathogenesis of Fanconi anemia: recent progress. Blood. 2006;107:4223–33. doi: 10.1182/blood-2005-10-4240. [DOI] [PubMed] [Google Scholar]
- 7.Gaymes TJ, Mufti GJ, Rassool FV. The non-homologous end-joining pathway is aberrant in human myeloid leukemias: evidence that KU70/86 is required for the increased frequency of misrepair. Canc Res. 2002;62:2791–7. [PubMed] [Google Scholar]
- 8.Virag S, Szabo C. The therapeutic potential of poly (ADP-ribose) polymerase inhibitors. Pharm Rev. 2002;54:375–429. doi: 10.1124/pr.54.3.375. [DOI] [PubMed] [Google Scholar]
- 9.Bryant HE, Schultz N, Thomas HD, Parker KM, Flower D, Lopez E, et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly (ADP-ribose) polymerase. Nature. 2005;434:913–7. doi: 10.1038/nature03443. [DOI] [PubMed] [Google Scholar]
- 10.Farmer H, McCabe N, Lord CJ, Tutt ANJ, Johnson DA, Richardson TB, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917–21. doi: 10.1038/nature03445. [DOI] [PubMed] [Google Scholar]
- 11.Bryant HE, Helleday T. Inhibition of poly (ADP-ribose) polymerase activates ATM which is required for subsequent homologous recombination repair. Nucl Acid Res. 2006;34:1685–91. doi: 10.1093/nar/gkl108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaymes TJ, Orr S, Mufti GJ, Rassool FV. Histone deacetylase inhibitors (HDI) induce DNA damage and repair: a mechanism for HDI dependent apoptosis in leukaemia cells. Mol Cancer Res. 2006;4:563–73. doi: 10.1158/1541-7786.MCR-06-0111. [DOI] [PubMed] [Google Scholar]
- 13.German J. Bloom’s syndrome. XX. The first 100 cancers. Cancer Genet Cytogenet. 1997;93:100–6. doi: 10.1016/s0165-4608(96)00336-6. [DOI] [PubMed] [Google Scholar]
- 14.Varon R, Reis A, Henze G, von Einsiedel HG, Sperling K, Seeger K. Mutations in the Nijmegen breakage syndrome gene (NBS1) in childhood acute lymphoblastic leukemia (ALL) Canc Res. 2001;61:3570–2. [PubMed] [Google Scholar]
- 15.Riballo E, Critchlow SE, Teo S-H, Doherty AJ, Priestley A, Broughton B, et al. Identification of a defect in DNA ligase IV in a radiosensitive leukaemia patient. Curr Biol. 1999;9:699–704. doi: 10.1016/s0960-9822(99)80311-x. [DOI] [PubMed] [Google Scholar]
- 16.Gaymes TJ, Shall S, Farzaneh F, Mufti GJ. Chromosomal instability syndromes are sensitive to poly ADP ribose polymerase (PARP) inhibitors. Haematologica. 2008;93:1886–9. doi: 10.3324/haematol.13201. [DOI] [PubMed] [Google Scholar]
- 17.McCabe N, Turner NC, Lord CJ, Kluzek K, Bialkowska A, Swift S, et al. Deficiency in the repair of DNA damage by homologous recombination and sensitivity to poly(ADP-ribose) polymerase inhibition. Cancer Res. 2006;66:8109–15. doi: 10.1158/0008-5472.CAN-06-0140. [DOI] [PubMed] [Google Scholar]
- 18.Cameron EE, Bachman KE, Myöhänen S, Herman JG, Baylin SB. Synergy of demethylation and histone deacetylase inhibition in the re-expression of genes silenced in cancer. Nat Genet. 1999;21:103–7. doi: 10.1038/5047. [DOI] [PubMed] [Google Scholar]
- 19.Calabrese CR, Almassy R, Barton S, Batey MA, Calvert AH, Canan-Koch S, et al. Anticancer chemosensitization and radiosensitization by the novel poly (ADP-ribose) polymerase-1 inhibitor AG14361. J Natl Cancer Inst. 2004;96:56–67. doi: 10.1093/jnci/djh005. [DOI] [PubMed] [Google Scholar]
- 20.Kim MS, Blake M, Baek JH, Kohlhagen G, Pommier Y, Carrier F. Inhibition of histone deacetylase increases cytotoxicity to anticancer drugs targeting DNA. Canc Res. 2003;63:7291–300. [PubMed] [Google Scholar]
- 21.Camphausen K, Burgan W, Cerra M, Oswald KA, Trepel JB, Lee MJ, Tofilon PJ. Enhanced radiation-induced cell killing and prolongation of γH2AX foci expression by the histone deacetylase inhibitor MS-275. Canc Res. 2004;641:316–21. doi: 10.1158/0008-5472.can-03-2630. [DOI] [PubMed] [Google Scholar]
- 22.Ratnam K, Low JA. Current development of clinical inhibitors of poly (ADP-ribose) polymerase in oncology. Clin Canc Res. 2007;13:1383–8. doi: 10.1158/1078-0432.CCR-06-2260. [DOI] [PubMed] [Google Scholar]
- 23.Racz I, Tory K, Gallyas F, Jr, Berente Z, Osz E, Jaszlits L, et al. BGP-15 – a novel poly (ADP-ribose) polymerase inhibitor – protects against nephro-toxicity of cisplatin without compromising its antitumor activity. Biochem Pharmacol. 2002;63:1099–111. doi: 10.1016/s0006-2952(01)00935-2. [DOI] [PubMed] [Google Scholar]