Abstract
BACKGROUND
Complete reports of biliary and vascular injuries after laparoscopic cholecystectomy are rare.
STUDY DESIGN
Fifteen patients with complex laparoscopic cholecystectomy injuries underwent corrective operations. The injuries consisted of 14 bile duct injuries and one large laceration of a cirrhotic liver. Five of the bile duct injuries were accompanied by inadvertent occlusion of the right hepatic artery, and one was further complicated by portal vein occlusion. One hepatic artery occlusion and one portal vein occlusion were successfully reconstructed. Two patients with arterial occlusion required right hepatic lobectomy. Corrective biliary operations consisted of common hepaticojejunostomy (seven cases), right and left hepaticojejunostomies (one case), right anterior and left hepaticojejunostomies (two cases), right hepaticojejunostomy (one case), right posterior hepaticojejunostomy (one case), and left hepaticojejunostomy after right lobectomy (two cases).
RESULTS
Except for a patient with a severe laceration of a cirrhotic liver who died as a result of hepatic failure, the remaining 14 patients are alive and well with normal hepatic function tests at six and 37 months after corrective operations.
CONCLUSIONS
A knowledge of anatomy is critical to the prevention of injuries to the hepatobiliary tree and related structures during laparoscopic cholecystectomy. J. Am. Coll. Surg., 1994, 179: 321–325.
Comprehensive reports of successful operative corrections of biliary and vascular injuries caused by laparoscopic cholecystectomy are scarce (1–3). This report was done to summarize our experience in operative corrections of biliary and vascular injuries after laparoscopic cholecystectomy.
MATERIALS AND METHODS
From August 1990 to March 1993, 15 patients were referred to us for operative corrections of laparoscopic cholecystectomy injuries. Six patients were men and nine were women. Their ages ranged from 27 to 80 years, with a mean age of 50 years (Table I).
TABLE I.
CLINICAL PRESENTATION
| Patient No. | Age, y | Sex | Recognition at LC | Conversion to open | Onset of symptoms, d | Symptoms and signs | Operative treatment before referral and days after LC | Referral after LC, d |
|---|---|---|---|---|---|---|---|---|
| 1 | 42 | M | No | No | 3 | Bile peritonitis | None | 10 |
| 2 | 27 | F | No | No | 3 | Bile peritonitis | None | 14 |
| 3 | 61 | M | No | No | 1 | Bile leak through drain | None | 6 |
| 4 | 26 | F | No | No | 14 | Bile peritonitis | Laparotomy, 20 | 24 |
| 5 | 73 | M | No | No | 21 | Recurrent cholangitis | None | 225 |
| 6 | 60 | F | No | No | 10 | Jaundice, fever, bile peritonitis | None | 16 |
| 7 | 73 | F | Yes? | Yes | 1 | GOT 6,798, GPT 4,916 | Hepaticojejunostomy, 0 | 5 |
| 8 | 67 | M | No | No | 2 | Bile leak through drain, jaundice | None | 2 |
| 9 | 37 | F | No | No | 14 | Cholangitis, jaundice | Hepaticojejunostomy, 14 | 17 |
| 10 | 36 | F | Yes? | Yes | 6 | Jaundice, fever, bile peritonitis | Laparotomy, stent, duct-to-duct, 6 | 8 |
| 11 | 46 | M | Yes | Yes | — | — | T-tube, duct-to-duct* right hepatic artery repair, 0 | 0 |
| 12 | 42 | F | No | No | 1 | Bleeding | None | 1 |
| 13 | 33 | F | Yes | Yes | — | — | None | 0 |
| 14 | 80 | M | No | No | 90 | Jaundice | None | 120 |
| 15 | 34 | F | No | No | 14 | Bile peritonitis, fever, subhepatic abscess | None | 27 |
Duct-to-duct, end-to-end choledocho-choledochostomy.
LC, Laparoscopic cholecystectomy; GOT, glutamine-oxaloacetic transaminase; GPT, glutamic-pyruvic transaminase; y, year, and d, day.
Thirteen of the 15 patients underwent elective cholecystectomy for cholecystolithiasis and recent episodes of cholecystitis. The remaining two patients (Nos. 8 and 14) had choledocholithiasis as well as cholecystolithiasis. The latter two patients, and another with known cirrhosis of the liver, had elevated serum bilirubin levels at the time of cholecystectomy.
Laparoscopic cholecystectomy was converted to an open procedure in four of the 15 cases, either because of bleeding (Nos. 7, 10, and 11), or because of severe inflammatory adhesions (No. 13). In these four, biliary duct injury was recognized and reconstruction was attempted at the time of cholecystectomy. However, in two (Nos. 7 and 10) of the four cases, the vascular injuries were not recognized fully even during the open procedure. In the remaining 11 cases, the injuries were not recognized until later (Table I).
The most common clinical manifestation of laparoscopic cholecystectomy injury was severe abdominal pain as a result of bile peritonitis (six cases), followed by fever and jaundice as a result of obstructive cholangitis (four cases). Bile leakage through the drain signaled biliary complications in two cases. Postoperative hypotension was the result of bleeding from hepatic laceration in one case (No. 12) (Table I).
In nine of the 15 cases, the occurrence of serious complication was recognized within a week. However, in the remaining six, clinical manifestation were delayed as long as three months after cholecystectomy. The time of referral ranged from the day of cholecystectomy to more than seven months later. All but two cases were referred to us within a month. Four patients (Nos. 7, 9, 10, and 11) had unsuccessful corrective operations before referral (Table I). In two patients (Nos. 7 and 10), it was not certain whether or not the injuries were recognized at the initial operation.
RESULTS
Biliary duct injury and operation correction
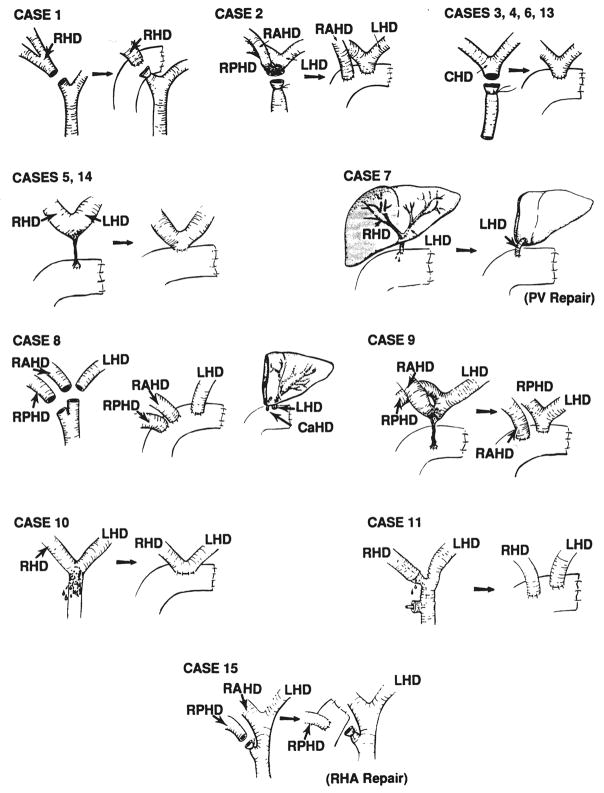
Eleven of the 14 biliary duct injuries occurred at the common hepatic duct (Table I; Fig. 1). Common hepaticojejunostomy with Roux-en-Y reconstruction was successful in seven of the 14 patients (Nos. 3, 4, 5, 6, 10, 13, and 14). In two patients (Nos. 2 and 9), however, the cauterization injury extended above the common hepatic duct. Right anterior and left hepaticojejunostomies were required in these cases because the right posterior duct drained into the left duct. In the remaining two patients (Nos. 7 and 8), left hepaticojejunostomy and right hepatic lobectomy were necessary because the right hepatic artery was also inadvertently ligated.
Fig. 1.
Diagrams of injuries and corrective operations. RHD, Right hepatic duct; RPHD, right posterior hepatic duct; RAHD, right anterior hepatic
Two of the 14 biliary duct injuries (Nos. 1 and 11) occurred at the right hepatic duct, and another (No. 15) at the right posterior hepatic duct. Right hepaticojejunostomy in patient No. 1 and right posterior hepaticojejunostomy in patient No. 15 were successful. In patient No. 11, however, right and left hepaticojejunostomies, were necessary because of necrosis of the common hepatic duct, caused by the right hepatic artery injury (Table II; Fig. 1).
TABLE II.
INJURY, CORRECTIVE OPERATIVE TREATMENT, AND RESULTS
| Patient No. | Injuries | Corrective operative treatment | Results |
|---|---|---|---|
| 1 | Right hepatic duct | Right hepaticojejunostomy | A & W at 37 mo |
| 2 | Common hepatic duct | Right ant. hepaticojejunostomy, right post and left hepaticojejunostomy | A & W at 35 mo |
| 3 | Common hepatic duct | Common hepaticojejunostomy | A & W at 22 mo |
| 4 | Common hepatic duct | Common hepaticojejunostomy | A & W at 19 mo |
| 5 | Common hepatic duct, hepaticoduodenal fistula | Common hepaticojejunostomy | A & W at 18 mo |
| 6 | Common hepatic duct | Common hepaticojejunostomy | A & W at 17 mo |
| 7 | Common hepatic duct, right hepatic artery, portal vein, left hepatic lobe necrosis | Right lobectomy, portal vein reconstruction, left hepaticojejunostomy | A & W at 16 mo |
| 8 | Common hepatic duct, right posterior duct, right hepatic artery, right hepatic lobe ischemia | 1) Right ant. and post. hepaticojejunostomy, 2) Right hepatic lobectomy, left hepaticojejunostomy, caudate hepaticojejunostomy |
A & W at 14 mo |
| 9 | Common hepatic duct | Right ant. hepaticojejunostomy, Right post and left hepaticojejunostomy | A & W at 13 mo |
| 10 | Common hepatic duct, right hepatic artery, right hepatic lobe ischemia, common duct ischemia | Common hepaticojejunostomy | A & W at 13 mo |
| 11 | Right hepatic duct, right hepatic artery, right hepatic lobe ischemia, common duct ischemia | Right hepaticojejunostomy, left hepaticojejunostomy, right hepatic artery reconstruction | A & W at 12 mo |
| 12 | Liver laceration, cirrhosis | Repair laceration | Died day 11 liver failure |
| 13 | Common hepatic duct | Common hepaticojejunostomy | A & W at 10 mo |
| 14 | Common hepatic duct, right hepatic artery | Common hepaticojejunostomy | A & W at 9 mo |
| 15 | Right posterior duct | Right post. hepaticojejunostomy | A & W at 6 mo |
A & W. Alive and well: ant., anterior: post., posterior, and mo, month.
Vascular injury and operative correction
The right hepatic artery was inadvertently ligated in five of 15 cases (Table II; Fig. 1). This arterial injury was associated with the common hepatic duct injury in four patients (Nos. 7, 8, 10, and 14) and with the right hepatic duct injury in one patient (No. 11). The ischemic injury to the right lobe of the liver and the injury to the bile duct were insignificant in two (Nos. 10 and 14) of the five cases, and common hepaticojejunostomy alone was successful. However, in two cases (Nos. 7 and 8), initial biliary reconstruction failed because of ischemic injury, and right hepatic lobectomy with revision of biliary reconstruction was necessary. The portal vein was also inadvertently occluded in patient No. 7 and was reconstructed with an end-to-end anastomosis after thrombectomy. The right hepatic artery injury could be repaired with an arterial allograft in another case (No. 11), but, right and left hepaticojejunostomies, were necessary because of hepatic duct necrosis. Severe laceration of the cirrhotic liver near the round ligament in patient No. 12 might have resulted from the pneumoperitoneum during laparoscopic cholecystectomy.
Complications after operative correction
Initial corrective operation was attempted before referral in four patients. The common hepaticojejunostomy leaked and the right hepatic lobe became necrotic because of inadvertent occlusions of the right hepatic artery and the portal vein in patient No. 7. Right hepatic lobectomy and left hepaticojejunostomy after portal vein reconstruction corrected these serious injuries (Fig. 1). The hepaticojejunostomy became obstructed probably because of cauterization injury or ischemic injury, or both, in patient No. 9. In this case, the right anterior and the left hepaticojejunostomies (the right posterior duct draining into the left duct) were successful (Fig. 1). Primary duct-to-duct anastomosis over an internal stent was disrupted because of bile duct necrosis caused by right hepatic artery occlusion in two patients (Nos. 10 and 11). As the ischemia of the right hepatic lobe was mild, high common hepaticojejunostomy alone was successful in patient No. 10. In another patient with significant ischemia (No. 11), the right posterior hepatic artery could be reconstructed with an arterial allograft, and the right and left hepaticojejunostomies were successful (Fig. I).
There were two cases of biliary leakage after our corrective operation. In one patient (No. 2), there was leakage at the right anterior hepaticojejunostomy, which was successfully revised (Fig. 1). In another case (No. 8) the occlusion of the right hepatic artery was not recognized during the combined right anterior and posterior hepaticojejunostomy and the left hepaticojejunostomy. The leakage from the right duct anastomosis and the ischemic necrosis of the right hepatic lobe were diagnosed three weeks later. The left hepaticojejunostomy and the caudate hepaticojejunostomy after the right hepatic lobectomy corrected the injuries (Fig. 1).
There was a case of biliary obstruction as a result of a retained stone 12 days after hepaticojejunostomy patient No. 5. The stone was removed by a percutaneous procedure.
One patient had fatal hepatic failure after repair of severe laceration of the cirrhotic liver. Transplantation of the liver was planned, but the patient had bronchopneumonia, sepsis, and multiorgan failure before an organ became available. Patient No. 12 died ten days after laparoscopic cholecystectomy.
Follow-up evaluation
Except for the single death, all of the remaining 14 patients were alive and well with normal hepatic function tests six to 37 months after the final corrective operation, as of September 1993 (Table II).
DISCUSSION
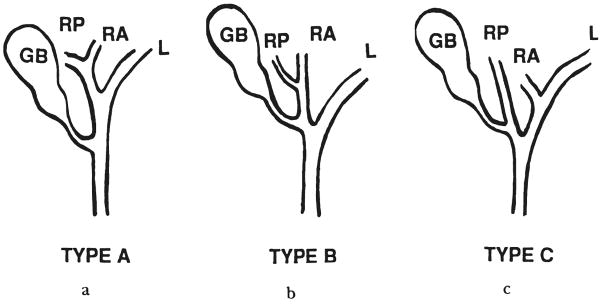
There are basically three types of cystic duct union to the biliary system (Fig. 2). Most commonly, the cystic duct joins the common hepatic duct below the union of the right and left hepatic ducts (Fig. 2a). Occasionally, the cystic duct enters the right hepatic duct above the union of the right and left hepatic ducts and below that of the right anterior and posterior hepatic ducts (Fig. 2b), or it enters the right posterior duct, where the right anterior hepatic duct joins the left hepatic duct (Fig. 2c). Rarely does the right posterior duct drain into the cystic duct (4–9). Eleven of the 14 biliary duct injuries seemed to occur in the most common type A cystic duct union. Two in occurred in patients with type B union, and one in a patient with the type C union. The cystic duct is usually short and away from the center of the hepatic hilum in these variant types of unions, and the right hepatic duct or the right posterior hepatic duct may be easily mistaken as a cystic duct.
Fig. 2.
a, b, and c, Basic patterns of cystic duct union. GB, Gallbladder, RP, right posterior; RA, right anterior, and L, left.
The duct-to-duct anastomosis is not recommended for laparoscopic cholecystectomy injuries because they are generally associated with extensive cauterization injuries. The cauterization injury extended above the common hepatic duct in two patients, and two biliary-enteric anastomoses were required in these patients.
The cystic artery most often arises from the right hepatic artery, its course in relation to the duct is quite variable, and occasionally there are two cystic arteries. The blood supply to the extrahepatic bile duct is usually double, that is, from the hepatic artery, including the right hepatic artery, and from the gastroduodenal artery. These two blood vessels communicate well along the duct (10, 11). The occlusion of one source is usually well tolerated by the duct. However, when the duct is completely or nearly completely transected, the blood supply to a segment of the duct becomes insufficient. Additional cauterization injury during laparoscopic cholecystectomy aggravates the duct ischemia. Therefore, even an isolated common hepatic duct transection should be repaired by the hepaticojejunostomy with Roux-en-Y.
Injury of the right hepatic artery is a well-recognized complication of cholecystectomy. There were five cases of right hepatic artery occlusion in our series. In all of these five cases, significant bleeding was encountered during the laparoscopic cholecystectomy. The operation was converted to an open procedure in three of the five cases. Unfortunately, however, the arterial injury was not recognized in any of the five cases at the time of cholecystectomy, and it was undetected again in two of them, even during the second operation. Inadvertent ligation of the right hepatic artery, when accompanied with the duct injury, can result in the most complex complication, as presented.
Basic anatomic knowledge of the hepatic hilum, as discussed previously, will prevent serious complications of laparoscopic cholecystectomy. Should they occur, it will be of great assistance for the proper corrective operation.
References
- 1.Rossi RL, Schirmer WJ, Braasch JW, et al. Laparoscopic bile duct injuries. Arch Surg. 1992;127:596–602. doi: 10.1001/archsurg.1992.01420050124016. [DOI] [PubMed] [Google Scholar]
- 2.Branum G, Schmitt C, Baillie J, et al. Management of major biliary complications after laparoscopic cholecystectomy. Ann Surg. 1993;217:532–541. doi: 10.1097/00000658-199305010-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ress AM, Sarr MG, Nagorney DM, et al. Spectrum management of major complications of laparoscopic cholecystectomy. Am J Surg. 1993;165:655–669. doi: 10.1016/s0002-9610(05)80783-4. [DOI] [PubMed] [Google Scholar]
- 4.Hjortsjö CH. The topography of the intrahepatic duct systems. Acta Anat. 1951;11:599–615. [PubMed] [Google Scholar]
- 5.Healey JE, Schroy PC. Anatomy of the biliary ducts within the human liver. Analysis of the prevailing pattern of branching and the major variations of the biliary ducts. Arch Surg. 1953;66:599–616. doi: 10.1001/archsurg.1953.01260030616008. [DOI] [PubMed] [Google Scholar]
- 6.Couinaud C. Le Foie Etudes Anatomiques et Chirurgicales. Paris: Masson; 1957. La chirurgie du confluent biliaire superieur; pp. 496–497. [Google Scholar]
- 7.Ohto M, Ono T, Tsuchiya Y, Saisho H. Cholangiography and Pancreatography. Tokyo: Igaku-Shoiu; 1978. Roentgenologic anatomy of the biliary tract; pp. 37–41. [Google Scholar]
- 8.Champetier J, Davin JL, Letoublon C, et al. Aberrant biliary ducts (vasa aberrantia): surgical implications. Anat Clin. 1982;4:137–145. [Google Scholar]
- 9.Smadja C, Blumgart HH. Surgery of the Liver and Biliary Tract. New York: Churchill Livingstone; 1988. The biliary tract and the anatomy of biliary exposure; pp. 11–22. [Google Scholar]
- 10.Northover JMA, Terblanche J. A new look at the arterial supply of the bile duct in man and its surgical implications. Br J Surg. 1979;66:379–384. doi: 10.1002/bjs.1800660603. [DOI] [PubMed] [Google Scholar]
- 11.Terblanche J, Allison HF, Northover JMA. An ischemic basis for biliary strictures. Surgery. 1983;94:52–57. [PubMed] [Google Scholar]