Abstract
The modulation of cellular processes by small molecule inhibitors, gene inactivation, or targeted knockdown strategies combined with phenotypic screens are powerful approaches to delineate complex cellular pathways and to identify key players involved in disease pathogenesis. Using chemical genetic screening, we tested a library of known phosphatase inhibitors and identified several compounds that protected Bacillus anthracis infected macrophages from cell death. The most potent compound was assayed against a panel of sixteen different phosphatases of which CD45 was found to be most sensitive to inhibition. Testing of a known CD45 inhibitor and antisense phosphorodiamidate morpholino oligomers targeting CD45 also protected B. anthracis-infected macrophages from cell death. However, reduced CD45 expression did not protect anthrax lethal toxin (LT) treated macrophages, suggesting that the pathogen and independently added LT may signal through distinct pathways. Subsequent, in vivo studies with both gene-targeted knockdown of CD45 and genetically engineered mice expressing reduced levels of CD45 resulted in protection of mice after infection with the virulent Ames B. anthracis. Intermediate levels of CD45 expression were critical for the protection, as mice expressing normal levels of CD45 or disrupted CD45 phosphatase activity or no CD45 all succumbed to this pathogen. Mechanism-based studies suggest that the protection provided by reduced CD45 levels results from regulated immune cell homeostasis that may diminish the impact of apoptosis during the infection. To date, this is the first report demonstrating that reduced levels of host phosphatase CD45 modulate anthrax pathogenesis.
Interactions between microbes and immune cells play a critical role in microbial pathogenesis. Many pathogenic organisms exploit the host immune machinery and subsequently modulate cell function, signaling, migration, and cytoskeleton rearrangement. Hence, identifying host cellular components with which microbes interact will allow for a more comprehensive understanding of microbial pathogenesis, define common strategies used by multiple pathogens, and elucidate unique tactics evolved by individual species to help establish infections or evade host innate responses. Another interesting aspect of infection is that diverse pathogens seem to target common cellular pathways (1, 2). Thus, identifying host targets exploited by multiple pathogens will be useful in the development of broad-spectrum host-oriented therapeutics and vaccines.
Protein kinases and phosphatases regulate a range of cellular responses to external and internal stimuli, including cell proliferation, metabolism, and apoptosis. Aberrant kinase and/or phosphatase activities underlie many different types of pathological conditions from cancer to infectious diseases. Protein kinases have been extensively investigated as targets for drug discovery. In addition, phosphatases are now being recognized as important regulators of many biological processes. In particular, there is an increasing interest in protein-tyrosine phosphatases (PTPs)3 as drug targets (3–8) because immune cells express a remarkably high proportion of the 107 PTP genes in the human genome (9) and also due to the growing number of human diseases discovered to be associated with PTP abnormalities (9–11). The involvement of cellular and bacterial PTPs during intracellular microbial pathogenesis has been a topic of significant interest (2, 12, 13). The bacterial PTP YopH, secreted by Yersinia pestis, interferes with the host adhesion-regulated signaling pathway via dephosphorylation of selective tyrosine-phosphorylated proteins (14). Activation of host PTPs after infection with bacteria or their virulence factors has been demonstrated for a diverse group of microorganisms such as Mycobacterium tuberculosis and Leishmania donovani (13). Specific mechanistic models of how PTPs contribute to the development of infection and disease progression by highly lethal organisms still remain unclear.
Bacillus anthracis, a Gram-positive spore-forming bacterium, is the etiologic agent of anthrax. The lethal toxin (LT) produced by B. anthracis can cleave host cell mitogen-activated protein kinase kinases (MAPKK), thereby affecting the immune response and the host ability to fight the infection (15, 16). Macrophages are the primary targets of anthrax LT. However, macrophages from only certain strains of mice are susceptible to LT-mediated cell death (17, 18). To date, there is no known direct relation between MAPKK cleavage and LT-induced macrophage cell death, as LT-resistant macrophages exhibit MAPKK cleavage (19–21). This suggests that another cellular target(s) may play a role in anthrax pathogenesis.
Previously, using a chemical genetic approach, we identified a class of Cdc25 inhibitors that protected macrophages from cell death induced by anthrax LT (22). Although Cdc25 was not the cellular target, induction of anti-apoptotic responses by the compounds via either the MAPK-dependent or -independent pathways was responsible for the protective phenotype.
In the present study we investigated if the previously identified phosphatase inhibitors (22) and their analogs produced any phenotypic changes in the B. anthracis infection model. Two compounds that previously protected LT-treated macrophages (22) also protect B. anthracis-infected macrophages. Subsequent in vitro phosphatase profiling studies identified CD45, a previously unknown target of one of the small molecules, as the most sensitive enzyme to the inhibitor. We then investigated the effect of CD45 reduction in anthrax pathogenesis both in cells and in vivo by using antisense phosphorodiamidate morpholino oligomers and mice engineered to express reduced levels of CD45.
EXPERIMENTAL PROCEDURES
Heterozygous and Transgenic Mice—All mice in this study are of the C57BL/6 genetic background. C57BL/6 (CD45100%) wild type mice and exon-9-disrupted CD45 knock-out mice were obtained from The Jackson Laboratory (Bar Harbor, Maine). The heterozygous CD4562% mice have one exon 9 knock-out allele and one wild type allele. Transgenic mice containing a point mutation (C817S) in the membrane proximal phosphatase domain of the CD45 minigene were produced using a CD45 minigene construct containing cDNA for exons 1b-3, the genomic sequence from exon 3 to exon 9, which includes the variably spliced exons and surrounding introns, and cDNA from exon 9 through the polyadenylation signal region in exon 33, as described previously (23, 24). The minigene expresses CD45 in transgenic mice in the same leukocyte-restricted manner and with the same isoform regulation in leukocyte subsets as the endogenous gene (24). The C817S mutation eliminates the catalytic site of the membrane proximal PTP domain and has been shown to abolish CD45 PTP activity in vitro (25), which has been confirmed in ex vivo studies.4 The CSV10 transgenic founder generated using the C817S mutant minigene was bred onto the exon-9-disrupted CD45 knock-out strain for seven generations to place the transgene on the CD45 knock-out and C57BL/6 backgrounds.
The CD45 cell surface expression levels of heterozygous and CSV10+/- mice were determined with flow cytometry by comparison of the mean fluorescence intensities of the lymphocyte populations to those of CD45100% wild type and CD450% knock-out mice (24). The expression level of CSV10 transgenic mice containing one copy of the transgene insertion locus (CSV10+/-) is 62–65%, a level similar to that expressed by CD4562% heterozygous mice.
Chemical Library—A focused library of known phosphatase inhibitors and related napthoquinone- and dione-containing derivatives was used for screening (supplemental Table 1). These compounds were obtained from the NCI Open Chemical Repository, and their structures are available on the following web site, pubchem.ncbi.nlm.nih.gov. The CD45 inhibitor (N-(9,10-dioxo-9,10-dihydro-phenanthren-2-yl)-2,2-dimethyl propionamide) was obtained from Calbiochem, whereas its related analogs (phenanthrene-9,10 dione) and (4-nitrophenanthrene-9,10 dione) were obtained from Sigma.
Phosphorodiamidate Morpholino Oligomer (PMO) Design and Synthesis—The sequence of the CD45 PMO targeting the translational start site is 5′-CCACAAACCCATGGTCATATC-3′. The scrambled PMO (5′-CGGACACACAAAAAGAAAGAAG-3′) was used as a nonbacterial negative control. For efficient delivery of PMOs into cells, an Arg-rich peptide (CH3CONH-(RAhxR)4-Ahx-βAla, designated P007; in which R stands for arginine, Ahx stands for 6-aminohexanoic acid, and βAla stands for β-alanine) was covalently conjugated to the 5′ end of the PMOs through a noncleavable piperazine linker. The methods for the syntheses of PMOs, the conjugation of P007, and the purification and analyses of P007-PMOs have all been described previously (26, 27).
Phosphatase Activity Assay—Protein phosphatases were purchased from Upstate Biotechnology (Lake Placid, NY). A generic substrate, DiFMUP (6,8-difluoro-4-methylumbelliferyl phosphate), was purchased from Invitrogen. All assays were performed in 50 mm HEPES containing 1 mm dithiothreitol and 0.1% bovine serum albumin, pH 7.4, with the following modifications or additions: SHP1, PTPMEG-2, and PTPβ (10 mm MgCl2); PP1α, PP1β, and PP2A (10 mm MnCl2); HePTP, VHR, CD45, TC-PTP, SHP-2, LMPTPA (pH 4.5), and LMPTPB (pH 4.5); PTPMEG-1 (4.8 mm MgCl2 and 3.2 mm MnCl2); PTP-1B (25 mm HEPES, 50 mm NaCl, 5 mm dithiothreitol, and 2.5 mm EDTA). Compound (10 μm) was added to 15 μl of enzyme and incubated for 10 min followed by 10 μl of DiFMUP at a final concentration of 100 μm. The 384-well plate was incubated at room temperature for 60 min and then read in an Analyst (MDC using excitation 360 nm; emission 450 nm). The effect of the compound was compared with control wells containing DMSO (1%). The different phosphatase enzyme characteristics and their concentrations used in this assay have been detailed in supplemental Table 2.
Cdc25B phosphatase activity was measured as described previously (22, 28). Briefly, an assay mixture containing 30 mm Tris, pH 8.0, 75 mm NaCl, 1 mm EDTA, 0.033% bovine serum albumin, I mm dithiothreitol, 40 μm 3-O-methyl fluorescein phosphate, and 0.7 μg/ml His-Cdc25B catalytic domain (a kind gift from Dr. John Lazo, University of Pittsburgh) was incubated with NSC 95397 in DMSO or DMSO (control) for 1 h at room temperature. The reaction was quenched by adding 100 mm NaOH, and the increase in fluorescence was measured at an excitation wavelength of 485 nm and emission wavelength of 530 nm.
To measure CD45 phosphatase activity in protein lysates, equal concentrations of total protein (200 μg) from untreated or PMO-treated macrophages (8 μm, 72 h treatment) were first precleared with protein G-Sepharose beads and then immunoprecipitated overnight with either the nonspecific monoclonal antibody or CD45-specific (clone 30-F11, BD Biosciences) antibody in the presence of protein G beads. After washing, the beads were incubated with 100 μm DiFMUP substrate in 100 μl of assay buffer for 1 h. Supernatant was transferred into 96-well plates, and fluorescence intensity was measured at excitation 358 nm and emission 455 nm. The experiments were repeated independently at least three times. The results are given as averages with S.D.
Flow Cytometry—Antibodies used for fluorescence-activated cell sorter analysis were purchased from BD Pharmingen unless otherwise noted. Antibodies used were directly conjugated to fluorescein isothiocyanate, phycoerythrin (PE), allophycocyanin (APC), peridinin chlorophyll protein (PerCP), or PECy5. Clones used in these studies included CD45 (30-F11), CD3 (17A2), CD4 (RM4–5), CD8 (53-6.7), CD11b (M1/70), CD11c (N418, eBioscience), CD19 (1D3), NK1.1 (PK136, eBioscience), major histocompatibility complex (MHC) I (28-14-8), MHC II (M5/114.15.2), CD44 (IM7), and Ly6G (1A8). Cells (1 × 106) were resuspended in Fc block (anti CD16/CD32 antibody diluted in RPMI medium containing 10% fetal bovine serum), incubated on ice for 30 min, centrifuged, and stained with appropriate combinations of labeled antibodies. After incubation on ice for 60 min, cells were washed and resuspended in 10% formaldehyde. Fluorescence-activated cell sorter analysis was performed using a FACSCalibur flow cytometer (BD Biosciences). Data were analyzed using FlowJo software.
Cell Viability Assay of B. anthracis-infected Macrophages— To test the effects of compounds on cell viability after B. anthracis infection, J774A.1 cells (6 × 105) were pretreated with DMSO (1%) control or compound (10 μm). After 1 h cells were infected with Sterne spores of B. anthracis (5 m.o.i.). After 4 h of incubation at 37 °C, bacterial growth was inhibited by the addition of the antibiotics penicillin (100 IU) and streptomycin (100 μg/ml). To determine cell viability sytox green nucleic acid stain (1 μm, Molecular Probes), which is impermeant to live cells, was added and incubated for 15 min at 37 °C. The cells were centrifuged at 2000 rpm for 2 min and then washed 2 times with complete medium containing antibiotics. The cells were fixed with 1% formaldehyde for 15 min and then analyzed by flow cytometry.
To test the effects of CD45 knock-down on cell viability after B. anthracis infection, J774A.1 cells (6 × 105) were either left untreated or treated with CD45 or SC PMOs. After 72 h cells were harvested and infected with the Sterne spores (5 m.o.i.). After 4 h of incubation at 37 °C, cell viability was measured by the uptake of sytox green dye (as described above).
Immunoblot Analysis—J774A.1 cells (∼1 × 106) seeded in a 6-well plate were either left untreated or incubated with CD45 or scrambled PMO for 72 h. Cells were harvested and lysed in buffer containing 50 mm Tris-HCl, pH 7.4, 150 mm NaCl, 2 mm EDTA, 1% Triton X-100, and protease inhibitor mixture (Sigma). The cell lysates were incubated for 30 min on ice and then centrifuged for 30 min at 14,000 rpm. Cell extracts (30 μg) were electrophoresed on SDS-PAGE and then subjected to Western blotting. A CD45-specific mouse monoclonal antibody (clone 69, BD Pharmingen) was used to detect the immunoreactive proteins that were visualized by Enhanced Chemiluminescence (ECL).
To determine the MEK cleavage pattern, J774A.1 cells were treated with the CD45 or scrambled PMOs (8 μm) for 72 h. Cells were harvested and then treated with anthrax lethal toxin (100 ng/ml Protective antigen (PA83) and 20 ng/ml of lethal factor (LF)) or infected with B. anthracis Sterne spores (5 m.o.i.). After a 4-h incubation time, cells were washed with phosphate-buffered saline (PBS), lysed, and electrophoresed as described above. Western blots were probed with MEK1“NT” antibody (Upstate Biotechnology) or glyceraldehyde-3-phosphate dehydrogenase for uniform protein loading and visualized by ECL.
Animal Studies— 8–10-Week-old mice were used in this study and included both males and females. For in vivo B. anthracis studies, C57BL/6 wild type control (CD45100%), CD4562%, CD4511%, CD4536%, CD450%, and CSV10+/- mice were challenged via an intraperitoneal route with ∼300 colonyforming units (CFU) of Ames strain of B. anthracis. The mice were monitored for 1 month post-challenge.
To test the efficacy of PMOs in vivo, BALB/c mice (6–8 weeks old, n = 6) were pretreated via subcutaneous route with PBS or CD45 PMO or scrambled PMO for 2 days (days -2 and -1). On the third day (day 0), the mice were treated with the PMOs and infected via intraperitoneal route with Ames spores (∼750 CFU). An additional PBS or PMO treatment was given the day after challenge (day 1). Non-tagged PMOs were used for in vivo studies and injected at a dose of 100 mg/kg/day. The mice were monitored for 1 month post-challenge. B. anthracis Ames spores from the same batch were used for all the in vivo mouse studies described in Fig. 4 and 5.
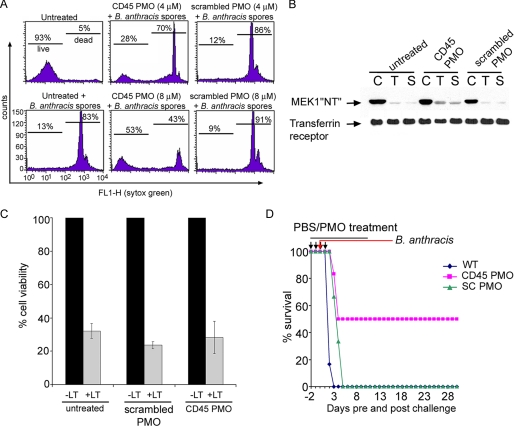
FIGURE 4.
CD45 PMOs affect survival from B. anthracis infection. A, increased cell viability as measured by the uptake of sytox green dye was observed in J774A.1 macrophages incubated for 72 h with CD45 PMO (4 or 8 μm) and then infected for 4 h with Sterne spores. In contrast, cells treated with scrambled PMO were not protected. B, reduced CD45 expression does not prevent MEK cleavage. J774A.1 macrophages were incubated with CD45 PMO (8 μm) or scrambled control PMO (8 μm) for 72 h and subsequently infected with anthrax lethal toxin (100 ng of PA83/20 ng of LF) or Sterne spores for 4 h. Cell lysates were immunoblotted with MEK1“NT” antibody. Lanes C, lysates from uninfected cells; lanes T, lysates from anthrax lethal toxin-treated cells; lanes S, lysates from Sterne-infected cells C, control; T, toxin; S, Sterne spores. As a control for uniform protein loading, the blot was incubated with the anti-transferrin receptor antibody. C, reduced CD45 expression does not protect macrophages from anthrax lethal toxin-induced cell death. J774A.1 macrophages were either not treated or treated with scrambled control (8 μm) or CD45 PMOs (8 μm) for 72 h and then treated with anthrax lethal toxin (100 ng PA83/20 ng LF). After 4 h cell viability was measured using a 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay. The data represent the averages ± S.D. for two independent experiments done in triplicate. D, CD45 PMO treatment protects mice. BALB/c mice were treated subcutaneously with PBS control (wild type (WT), n = 6) or CD45 PMO (n = 6, 100 mg/kg/injection) or SC PMO (n = 6, 100 mg/kg/injection) on days -2, -1, 0, and +1. On day 0 mice were infected intraperitoneally with Ames B. anthracis spores (∼750 CFU). A 50% survival rate was observed in the CD45 PMO-treated mice.
FIGURE 5.
Mice expressing intermediate CD45 levels survive B. anthracis infection. A, mice with intermediate CD45 expression levels (62%) challenged with Ames B. anthracis spores showed a 65% survival rate. In contrast, CD45100%, CD450%, CD4511%, CD4536%, or CSV10+/- (62%) mice with inactive CD45 phosphatase activity showed little to no protection after B. anthracis challenge. B, immunohistochemical staining of spleen with anti-capsule antibody did not show any bacterial load in the CD4562% mice surviving B. anthracis challenge (∼48 h) (right panel) versus moribund CD45100% mice (48 h) (left panel). Scale bar = 100 μm, 20× magnification. RP, red pulp; MZ, marginal zone; PALS, periarteriolar lymphoid sheath.
To determine the humoral responses, CD45100% and CD4562% mice were vaccinated 2 times at 2-week intervals via intraperitoneal injection with 100 μl of anthrax vaccine adsorbed mixed with 10 μg of QS-21 diluted in endotoxin-free PBS. After 35 days, mice were euthanized, blood was collected, and protective antigen (PA)-specific antibodies were measured by enzyme-linked immunosorbent assay.
All research was conducted under an approved protocol and in compliance with the Animal Welfare Act and other federal statutes and regulations related to animals and experiments involving animals and adhered to principles stated in the “Guide for the Care and Use of Laboratory Animals,” National Research Council 1996. The facility where this research was conducted is fully accredited by the Association for Assessment and Accreditation of laboratory Animal Care International.
Phagocytosis and Spore Viability—To enumerate the spores ingested by macrophages, thioglycolate-elicited peritoneal macrophages from CD45 100, 62, and 0% mice were infected with 5 m.o.i. of green fluorescent protein-Sterne spores and plate-centrifuged to synchronize the infection. After 30 min non-permeabilized cells were incubated with a mix of antibodies specific for B. anthracis spore exosporium (to label extracellular spores) and Bacillus polysaccharide (to label extracellular vegetative bacilli) (kindly provided by T. Abshire and J. Ezzel, United States Army Medical Research Institute of Infectious Diseases) followed by a secondary incubation with antibody conjugated to Alexa-594-nm fluorophore. This method labels only those spores adhered to the outside surface of the macrophages. After fixation with formaldehyde, cells were stained with Hoechst dyes, and images from nine sites/well were collected and analyzed using the Discovery-1 high content screening system (Molecular Devices, Downington, PA). Images were analyzed using the cell health module of MataXpress imaging analysis software. Total cell count was based on the number of Hoechst-stained cell nuclei, whereas co-localization of red (anti-spore and anti-bacterial antibody) and green (green fluorescent protein-Sterne spores) fluorescence was scored as spores being on the outside of the cell and with green-only fluorescence being scored as ingested spores.
To measure spore viability, thioglycolate-elicited peritoneal macrophages purified by plastic adherence were infected with Sterne spores at an m.o.i. of 5. After 30 min cell pellets collected by centrifugation were lysed in sterile water and serially diluted, and aliquots were plated onto solid LB agar medium plates, which were then incubated at 37 °C for 16 h. CFU were counted, and data are represented as CFU/ml. Experiments were performed in duplicate and repeated three independent times.
Macrophage Apoptosis—Thioglycolate elicited peritoneal macrophages from 100 or 62% CD45 expressor mice were either left untreated or infected with Sterne B. anthracis spores (10 m.o.i.) or staurosporine (2 μm) as a positive control. After 6 h, macrophage apoptosis was measured using the Apo-One Homogeneous Caspase 3/7 kit (Promega), as per the manufacturer instructions.
Cytotoxicity Assay—J774A.1 macrophages (5 × 104) were either left untreated or treated with scrambled control or CD45 PMO (5 μm). After 72 h cells were treated with 100 ng/ml PA83 and 20 ng/ml LF, a toxin concentration that results in 80–90% killing of macrophages. After 4 h 25 μl of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (1 mg/ml) dye was added, and cells were further incubated for 2 h. The reaction was stopped by adding equal volume of lysis buffer (50% N,N-dimethylformamide and 20% SDS, pH 4.7). Plates were incubated overnight at 37 °C, and cell viability was determined by measuring the absorbance at 570 nm in a multiwell plate reader.
Antibacterial Growth Inhibition Assay—B. anthracis Sterne spores (5 × 105 CFU/ml) diluted in Mueller-Hinton broth were treated with either DMSO control or compounds NSC 95397 (10 μm) or NSC 270012 (10 μm). At time intervals of 2, 5, 7, and 24 h, absorbance at 600 nm was measured. Experiments were done in duplicate and repeated at least two independent times.
Immunohistochemical Staining—To detect the presence of bacilli in infected tissues, the EnVision system (Dako) was used. Briefly, tissue sections were deparaffinized, blocked in methanol/H2O2 solution for 30 min at room temperature, rinsed with water, pretreated with Tris-EDTA, pH 9.0, at 97 °C for 30 min, and then blocked with mouse IgG blocking buffer (Vector Laboratories, 1:20). The tissues were then incubated with mouse anti-capsule antibody (#593) or mouse IgG as negative control serum for 30 min at room temperature. After rinsing 3 times with PBS, peroxidase-labeled polymer conjugated to goat anti-mouse immunoglobulins was added and incubated for 30 min. After rinsing with PBS, substrate-chromogen solution was added and incubated for 5 min. Tissues were then rinsed with PBS, stained with hematoxylin, dehydrated, and mounted with Permount.
RESULTS
Chemical Genetic Screening and Phosphatase Profiling—To assess whether inhibition of host phosphatase function would elicit protection against B. anthracis-induced cell death, a chemical genetic approach was used wherein a focused library of known Cdc25 phosphatase inhibitors (22) and their analogs (supplemental Table 1) were screened in infected macrophages. J774A.1 macrophages pretreated with DMSO control or compounds (10 μm) for 1 h were infected with B. anthracis Sterne spores (5 m.o.i.). After 4 h cell viability was measured by the uptake of sytox green dye using flow cytometry. Two compounds NSC 95397 and NSC 270012 were found to protect B. anthracis-infected macrophages from cell death (Fig. 1A). These two compounds were previously shown to protect macrophages from anthrax LT-mediated cell death (22). To determine whether increased compound concentration would result in greater cell viability, a dose response study using NSC 95397 was performed (supplemental Fig. 1). The results show that the protective efficacy was limited to a narrow dose range of the compound. At concentrations greater than 10 μm, cellular toxicity was observed. Further characterization studies showed that the two most potent compounds, NSC 95397 and NSC 270012 (Fig. 1B), did not inhibit 1) the growth of B. anthracis spores (Fig. 1C), 2) the enzymatic activity of anthrax LF (22), or 3) cellular proteasome activity (22), a host component exploited by anthrax LT to kill susceptible macrophages (29).
FIGURE 1.
Small molecules protect B. anthracis-infected macrophages and inhibit CD45 phosphatase activity in vitro. A, J774A.1 macrophages preincubated for 1 h with NSC 95397 or NSC 270012 (10 μm) were infected with the B. anthracis Sterne spores for 4 h. The cells were stained with sytox green dye and analyzed by flow cytometry. The percentage of living and dead cells is indicated. Data from a representative experiment, which was repeated three times with similar results, are shown. B, chemical structures of the two most potent compounds, NSC 95397 (2,3-bis(2-hydroxyethylsulfanyl)naphthalene-1,4-dione), and NSC 270012 (4-(1,4-dioxonaphthalen-2-yl)sulfanylbutanamide). C, identified compounds did not exhibit anti-microbial activity. B. anthracis Sterne spores were treated with either DMSO (1%), NSC 95397 (10 μm), or NSC 270012 (10 μm), and at various time intervals growth of the bacteria was monitored at an absorbance of 600 nm. D, the compound NSC 95397 (10 μm) demonstrated the most potent in vitro inhibition of CD45 phosphatase activity when screened against a panel of 16 different phosphatases.
Previously, enzymatic assays showed that NSC 95397 inhibited Cdc25, a family of dual specificity phosphatases that functions as important regulators of cell cycle progression (28). Furthermore, NSC 95397 was shown to block G2/M transition in murine and human carcinoma cells (28). However, in J774A.1 macrophages NSC 95397 did not seem to inhibit the cell cycle progression at G2/M phase (supplemental Fig. 2), suggesting that Cdc25 phosphatases may not be the target of this compound and, hence, not involved in protection from B. anthracis infection. To determine the involvement of any other phosphatases, NSC 95397 was screened for inhibitory activity against a panel of sixteen different phosphatases (Fig. 1D and supplemental Table 2), which represents a fraction of the 107 known PTP genes in the human genome. NSC 95397 inhibited several phosphatases to varying extents, implicating these enzymes as potential cellular targets mediating protection against B. anthracis infection. However, maximum inhibition was observed for CD45, and a dose-response study showed that NSC 95397 has an IC50 value of 3.0 μm for this enzyme (supplemental Fig. 3). The majority of the phosphatases tested in this panel belong to the class of protein-tyrosine phosphatases (SHP-1, SHP-2, PTP1B, CD45, TCPTP, LMPTP-A, LMPTP-B, MEG1, MEG2, HePTP, PTPβ), three belong to the class of serine/threonine phosphatases (PP1α, PP1β, and PP2A), and two are dual specificity phosphatases (VHR, Cdc25B).
Small Molecule CD45 Inhibitor and Its Analogs Protect B. anthracis-infected Macrophages—CD45 is abundantly expressed in all nucleated hematopoietic cells and is a well known regulator of T and B cell antigen receptor signaling via the dephosphorylation of the Src-family kinases (30–32). Furthermore, CD45 triggers cytokine production via receptors on Natural Killer (33, 34), mast (35), neutrophil (36), and dendritic cells (37, 38). However, very little is known about the role of CD45 in macrophages during lethal microbial infection. To determine whether the protective effect of NSC 95397 resulted from reduced CD45 function, a known CD45 inhibitor (39) and its analogs (Table 1) were first tested using an in vitro CD45 enzymatic activity assay. The CD45 inhibitor (N-(9,10-dioxo-9,10-dihydro-phenanthren-2-yl)-2,2-dimethyl propionamide) and its analog (phenanthrene-9,10-dione) were both potent inhibitors of CD45 in vitro with IC50 values of 0.4 and 0.3 μm, respectively (Table 1). These compounds were then tested in a cell-based B. anthracis infection assay. As shown in Fig. 2, an increase in cellular protection was observed at a higher concentration (10 μm) of the known CD45 inhibitor (Calbiochem 540215). An intermediate peak observed in the histogram at this high concentration (10 μm) represents a cell population that may have taken up the sytox green dye and, hence, have reduced viability. The compound 156507, a structural analog of the known CD45 inhibitor, is a better inhibitor of CD45 enzymatic activity, but it did not show increased protection of macrophages. This may presumably be due to poor uptake properties.
TABLE 1.
Chemical names, structures, and IC50 values of the compounds tested in the in vitro CD45 phosphatase activity assay
FIGURE 2.
A known CD45 inhibitor protects B. anthracis-infected macrophages. J774A.1 macrophages were preincubated with DMSO control (1%) or compounds (5 or 10 μm). After 1 h cells were infected with B. anthracis Sterne spores (5 m.o.i.) for 4 h. The cells were stained with membrane impermeant sytox green dye and analyzed by flow cytometry. The percentage of living and dead cells is indicated. Data from a representative experiment, which was repeated three times with similar results, are shown.
CD45 Knockdown Using Antisense PMO—To further investigate the effect of reduced CD45 activity in B. anthracis infection, an optimized antisense PMO targeting the translational start site of CD45 mRNA was tested. A time-dependent study showed a maximum knock-down of CD45 expression in macrophages was achieved within 48–72 h of PMO treatment, whereas a scrambled control had no effect on CD45 expression (Fig. 3A). Dose escalation studies showed reduced CD45 expression with increasing PMO concentration (supplemental Fig. 4), and that concentrations up to 9 μm were not toxic to cells. Knock-down of CD45 levels by the targeted PMO was further confirmed by Western blotting (Fig. 3B), and reduction in CD45 phosphatase activity was measured using DiFMUP as substrate in a fluorescent-based assay (Fig. 3C).
FIGURE 3.
Gene-targeted knock-down of CD45 using peptide-conjugated PMO. A, J774A.1 cells were either left untreated or incubated with CD45 or a scrambled (SC) control (8 μm each) PMOs. At 24, 48, 72, and 96 h after treatment cells were stained with either isotype control antibody or fluorescein isothiocyanate-conjugated CD45 antibody and analyzed by flow cytometry. Representative histograms with geometric mean values have been depicted. FITC, fluorescein isothiocyanate. B, protein lysates prepared from cells that were either not treated or treated with CD45 PMO or SC PMO for 72 h and immunoblotted with CD45 antibody. A reduction in CD45 protein levels was observed in cells treated with a higher concentration (8 μm) of CD45 PMO compared with untreated or SC PMO. As a control for uniform protein loading, the bottom half of the blot was probed with glyceraldehyde-3-phosphate dehydrogenase (GAPDH) antibody. C, CD45 was immunoprecipitated from protein lysates prepared from macrophages that were either untreated (Un) or treated with CD45 or scrambled PMOs, and phosphatase activity was measured using DiFMUP substrate. A reduction in CD45 phosphatase activity was observed in cells treated with CD45 PMO but not with the scrambled control. Data from three independent experiments are averaged ± S.D.
CD45 Knock-down in Vitro Protects Macrophages and in Vivo Protects Mice from B. anthracis-induced Death—To determine whether reduced CD45 expression could reduce B. anthracis-induced death, PMO-treated macrophages were infected with B. anthracis spores, and cell viability was determined by measuring the uptake of the membrane impermeant sytox green dye using flow cytometry (Fig. 4A). Cells treated with CD45 PMO showed increased viability at higher PMO concentrations (8 μm) compared with either untreated or scrambled PMO-treated controls. These findings indicated that the induction of macrophage cell death can be reduced substantially by a mechanism that involves a tyrosine phosphorylation-dependent pathway.
The different MEK isoforms have been shown to be the prime targets for anthrax LT proteolytic activity (16, 40). However, the observed protection (Fig. 4A) did not correlate with MEK cleavage patterns, as cells treated with CD45 PMO and then infected with spores or treated externally with LT exhibited MEK cleavage similar to control cells (Fig. 4B). Furthermore, reduced CD45 expression by PMO treatment did not prevent LT-mediated cell death (Fig. 4C). This suggests that the relevant CD45-dependent pathway may not signal through MEK. To date, the direct relationship between MEK cleavage and macrophage susceptibility has not been established, as macrophages that are resistant to LT-induced cytolysis do exhibit MEK cleavage (19).
To investigate the role of CD45 knock-down in an in vivo mouse model, mice (n = 6) were pretreated via a subcutaneous route with either PBS control, scrambled PMO, or CD45 PMO for 2 days. On day 3 the mice were challenged with lethal Ames spores and treated with the PMOs. An additional treatment with the PMOs was administered 1 day after challenge, and survival of the mice was monitored for 30 days. CD45 PMO-treated mice that were challenged with Ames showed an increase in survival rate (50%) compared with scrambled PMO or PBS controls which succumbed to the pathogen (Fig. 4D). A statistically significant increase (p = 0.0026, using the Kaplan Meier survivor analysis log rank test) in the survival curves between the wild type (PBS controls) and each of the treatment groups was observed (supplemental Fig. 5).
Mice Expressing Intermediate CD45 Levels Survive B. anthracis Challenge—To confirm the effect of reduced CD45 activity in anthrax pathogenesis, heterozygous mice expressing intermediate levels of CD45 (CD4562%) and transgenic mice expressing reduced CD45 levels (11 or 36% of the wild type CD45 expression levels) were challenged with the virulent Ames B. anthracis spores, and their survival rates were compared with wild type control (CD45100%), CD45 knock-out mice (CD450%), and transgenic mice with 62% CD45 expression but with the point mutation C817S inactivating the CD45 phosphatase activity (CSV10+/-). The CD45100%, CD450%, and CSV10+/- mice succumbed to the lethal challenge, whereas the CD4511% and CD4536% showed only 10–20% protection. Interestingly, mice with intermediate CD45 expression levels (CD4562%) were protected with a survival rate of 65% (Fig. 5A). A statistically significant difference (p = 0.0050) in the survival curves between the CD45100% and CD4562% was observed using the Kaplan Meier survival analysis log rank test (supplemental Fig. 6). Subsequent studies with transgenic mice expressing intermediate CD45 levels (CD4562%, F+/+) showed a survival rate similar to the heterozygous CD4562% mice after challenge with Ames B. anthracis (supplemental Fig. 7). CD4562% mice that survived 48 h (Fig. 5B, right panel) or 1 month (data not shown) after B. anthracis challenge showed no bacilli in the spleen (Fig. 5B, right panel), lymph nodes, or lungs (data not shown), as observed by immunohistochemical staining with anti-capsule antibody. In contrast, spleen from moribund CD45100% mice showed a heavy bacterial burden in the red pulp (RP) areas with fewer bacilli appearing in cells associated with the marginal zone (MZ) and no visible bacilli in periarteriolar lymphoid sheaths (PALS) (Fig. 5B, left panel). Our in vivo data resulting from these genetically engineered mice suggest that intermediate levels of functionally active CD45 enzyme generate a robust protective immunity that allows the immune cells to respond to B. anthracis infection.
Functional Consequences of Reduced CD45 Expression—To determine whether reduced CD45 expression affected the humoral responses, CD4562% and CD45100% mice with reduced CD45 expression were vaccinated with anthrax vaccine adsorbed, and antibody titers were measured after 35 days. The CD4562% mice generated robust antibody responses similar to the wild type controls, suggesting that reduction in CD45 levels had no effect on humoral responses (Fig. 6A). To investigate if reduced CD45 levels disrupted the biological functions of immune cells, the phagocytic and killing properties of peritoneal macrophages were measured. Macrophages harvested from the CD4562% or CD450% mice possessed the ability to internalize the spores (Fig. 6B) and kill the bacteria (Fig. 6C) as efficiently as those from CD45100% mice.
FIGURE 6.
Intermediate CD45 expression does not affect either the adaptive or the functional properties but reduces apoptosis of the immune cells infected with B. anthracis. A, the CD4562% and CD45100% mice vaccinated with anthrax vaccine adsorbed generated similar levels of anti-PA-specific antibodies. B, thioglycolate-elicited peritoneal macrophages harvested from CD45100%, CD4562%, and CD450% mice were infected with green fluorescent protein-Sterne spores for 30 min. Ingested green fluorescent protein-Sterne spores were distinguished from non-internalized spores by incubating the non-permeabilized cells with a mix of monoclonal antibodies specific for B. anthracis spore exosporium and Bacillus polysaccharide to label all extracellular B. anthracis followed by incubation with secondary antibody conjugate to Alexa-594 fluorophore. The data represent averages from three independent experiments and indicate the percentage of spores internalized/cell. C, thioglycolate-elicited peritoneal macrophages from CD45100%, CD4562%, and CD450% mice were infected with Sterne spores for 30 min, cells were lysed, the entire mix was plated, and CFU/ml were determined. The data represent averages from three independent experiments ± S.D. D, thioglycolate-elicited peritoneal macrophages from CD45100% or CD4562% mice were either left untreated or infected with Sterne spores (10 m.o.i.) or treated with staurosporine (2 μm) for 6 h and then examined for apoptosis using an Apo-One homogenous Caspase-3/7 kit. The -fold change in apoptosis represents the ratio of treated to untreated cells. The data represent averages of three independent experiments ±S.E. E, thioglycolate-elicited peritoneal macrophages harvested from C57BL/6 mice were either not treated or treated with indicated concentrations of the compound NSC 95397 or staurosporine (2 μm) as positive control and then infected with Sterne B. anthracis spores. After 6 h apoptosis was measured using the Apo-One Homogeneous Caspase 3/7 kit.
Prior studies have shown that macrophages from inbred strains of mice vary in their sensitivity to LT-induced cell death (19, 20). Macrophages from C57BL/6 mice are resistant to LT-induced lysis. However, activated macrophages from these mice strains can undergo apoptosis after LT treatment (40, 41). Interestingly, CD4562% macrophages infected with B. anthracis exhibited reduced apoptosis compared with their CD45100% controls as measured by levels of activated caspase 3/7 (Fig. 6D), thus suggesting that reduced CD45 levels regulate apoptosis in these cells. A reduction in apoptosis was also observed in macrophages infected with B. anthracis and treated with compound NSC 95397 (Fig. 6E). Thus, reduction of CD45 PTP activity either by inhibition of the enzyme or by reduction of CD45 protein expression produces a similar functional phenotype (i.e. reduced apoptosis) in B. anthracis-infected macrophages.
To better understand how reduced CD45 activity attenuates B. anthracis infection, a time-course study to monitor functional and cellular changes was conducted as depicted in Fig. 7A. Cell profiling studies of splenocytes indicated a significant increase in the percentages of CD11b+ CD11c- macrophages (24 h) and Ly6G+ granulocytes (42 h) in the CD4562% mice (Fig. 7B). In blood (Fig. 7C) an increased percentage of Ly6G+ granulocytes (6 and 24 h) was also observed in the CD4562% mice compared with CD45100% mice. Both the spleen and blood of CD4562% mice had naturally elevated levels of activated T (CD44high) cells, an observation similar to that reported by McNeill et al. (42) in transgenic mice expressing reduced levels of the single CD45RO isoforms. The time-course study suggests that reduced CD45 levels shift the balance in favor of an effective innate response in the CD4562% mice infected with B. anthracis by enhanced numbers of macrophages and granulocytes, two eminent innate cell subsets which are pivotal in microbial clearance. Hence, innate immune cells in the CD4562% mice may play a central role to confer protection from B. anthracis infection.
FIGURE 7.
Robust immune responses in CD4562% mice challenged with B. anthracis. A, schematic diagram of time line study for CD45100% and CD4562% mice not infected or infected with Ames B. anthracis spores. At each time point (t = 0, 6, 24, 42 h), four mice/group were euthanized, various tissues were harvested, and plasma was collected. B, splenocytes isolated from mice euthanized at time 0, 6, 24, and 42 h post-B. anthracis challenge were stained for cell surface and activation markers and analyzed by flow cytometry. The data represent the averages of four mice/group/time points ±S.E. C, blood cells collected from mice euthanized at time 0, 6, 24, and 42 h post-B. anthracis infection were stained for cell surface and activation markers and analyzed by flow cytometry. The data represent the averages of four mice/group/time point and ±S.E.
DISCUSSION
Several different approaches and experimental mouse models have been developed to investigate anthrax pathogenesis, B. anthracis virulence mechanism, critical cellular players, host immune response to the pathogen, and potential therapeutic targets (43–46). To date, host proteins such as anthrax toxin receptors (ANTXR1 and ANTXR2) (47) and low density lipoprotein receptor-related protein 6 (LRP6) (48) have been considered as potential therapeutic targets against anthrax toxin mediated death. However, the role of LRP6 in anthrax toxin mediated lethality is still not clear (49), and the in vivo protective efficacy of the polyvalent inhibitors developed against the anthrax host receptors has been tested only in the rat lethal toxin model (47). Antibacterial effects of host endoribonuclease RNase-L (50), interferon-inducible host chemokines (51), and caspase-1-mediated interleukin-1β expression (52) have been implicated as important participants in the host defense in mice challenged with Sterne strain of B. anthracis. To date, the role of these critical host targets has not been demonstrated in the highly virulent Ames infection model. In a recent study by Walberg et al. (53), pretreatment of mice with interferon-β resulted in increased survival after challenge with Ames B. anthracis. However, our study is the first to demonstrate that reduced expression of a host protein can provide protection against the highly pathogenic Ames strain infection in vivo.
An important implication of this study is that small molecules identified by in vitro biochemical assays may exhibit off-target effects and hidden phenotypes because of their ability to bind to multiple targets. Such off-target effects may cause cellular toxicity but, more importantly, prove useful for therapeutic intervention or serve as valuable research tools. Furthermore, if the therapeutic class of the compound is known, it could lead to the identification of unrecognized host targets. An unanticipated, hidden phenotype of our known Cdc25 inhibitor (NSC 95397) was its ability to protect macrophages from B. anthracis-induced cell death. Structurally, NSC 95397 contains an electrophilic naphthalene dione scaffold which possesses the potential to engage in Michael type additions and, therefore, may reduce thiol groups of proteins indiscriminately. Despite this potential reactivity, studies by Lazo et al. (28) have shown that this compound is a potent and selective inhibitor of Cdc25B compared with either the dual specificity phosphatase VHR or the protein-tyrosine phosphatase PTP1B. Given these findings, the prospect of developing a highly specific inhibitor analog of NSC 95397 has promise, as modifications to the naphthalene-dione scaffold may result in greater specificity. For example, although the catalytic centers of phosphatases often contain a reactive thiol, the spatial disposition of amino acid side chains around this center may influence the steric accommodation of the ligand during the reduction. This could be the case with NSC 95397. Providing some support for this notion is the relative specificity that NSC 95397 demonstrated previously for Cdc25B (28). Moreover, with respect to this investigation, NSC 95397 has demonstrated a greater inhibitory potency for CD45 relative to Cdc25B, and its lack of inhibitory activity for a number of other phosphatases (shown in Fig. 1D) seems to warrant additional structure-activity relationship studies with CD45 as the target. In light of the potential multi-targeted nature of NSC 95397 and to further investigate whether modulation of CD45 activity is associated with the observed protection to B. anthracis, studies utilizing antisense approaches and mice with reduced CD45 expression were conducted.
Our data suggest that regulated CD45 signaling via reduced CD45 expression levels and, hence, reduced protein-tyrosine phosphatase activity provides protection during virulent Ames B. anthracis infection. The exclusive expression of CD45 by hematopoietic cells coupled with the natural role of these cells in host-pathogen interactions strongly suggest that cells of innate and/or adaptive immunity are responsible for the protective effect. Indeed we find several properties of the immune cells being critically affected. The rapid protective response required for B. anthracis infections, within 2–3 days, predicts that early activation of innate immunity may be critical for survival of mice with reduced CD45 expression. The in vivo time course data suggest that the increased percentages of splenic and peripheral macrophages and granulocytes after B. anthracis infection in CD4562% mice may trigger innate and T cell-mediated responses, resulting in bacterial clearance. Although the role of macrophages or T cells in pathogenesis of anthrax is not well established, recent studies have shown that macrophages (44) and even T cell (54) immune responses are critical in animal survival following B. anthracis infection. The robust protection elicited by intermediate levels of CD45 may possibly be a consequence of differential regulation of the regulatory phosphorylation sites (Tyr(P)-505 and Tyr(P)-394) of p56lck, a Src-family kinase with a key role in T cell signaling (42, 55). Thus, differential CD45 expression levels may control the sensitivity of the signaling pathway. Moreover, the observed protection is not an inherent condition of the genetic reduction of CD45 expression levels, as knockdown of CD45 by PMO in wild type mice resulted in a survival rate similar to the CD4562% mice after infection with B. anthracis. However, the control and clearance of bacterial infections in CD4562% mice is dependent on CD45 phosphatase activity, as CSV10 mice with 62% CD45 expression but with no CD45 phosphatase activity succumbed to the pathogen. The underlying mechanism of how reduced CD45 expression modulates immune cell signaling, which in turn controls the clearance of the pathogen, is not yet fully understood and requires further investigation. The difference in survival of CD45100% and CD4562% mice is not due to Nalp1b allelic differences known to confer sensitivity or resistance of macrophages to anthrax LT in vitro (56), as the C57BL/6 mice strain do not carry the Nalp 1b allele that confers susceptibility yet are sensitive to B. anthracis-induced death. In confirmation, macrophages from the wild type C57BL/6 mice and the CD450% and CD4562% mice used in this study are resistant to LT-induced lysis (supplemental Fig. 8).
It is important to note that B. anthracis spores and independently added LT appear to signal through at least partially divergent pathways, as our results demonstrate that reduced CD45 expression via PMO treatment protects macrophages after B. anthracis infection, but does not protect against direct addition of LT. In contrast, we have previously shown that NSC 95397 prevented MEK1 cleavage and inhibited LT-induced apoptosis of macrophages (22). These observed differences between NSC 95397 and the CD45 PMO studies could be due to the compound inhibiting multiple targets. Furthermore, reduced apoptosis was observed in macrophages derived from CD4562% mice compared with the control CD45100% mice, indicating that differential levels of CD45 may regulate apoptosis in B. anthracis infection.
To date, the functional role of CD45 has been studied in CD45-/- cell lines, CD45 knock-out mice, and mice expressing single CD45 isoforms. Changes that result from only partial reduction in levels of all isoforms of CD45 in cell-based and whole animal models still need to be fully explored. Such changes would mimic conditions resulting from therapeutic administration of the PTP inhibitors or antisense molecules. Our findings suggest that specific PTPs such as CD45 could be targeted for therapeutic intervention of infections by B. anthracis and possibly other infectious diseases. Furthermore, development of host-oriented adjunctive therapeutics would be effective against both the natural and engineered resistant forms of the bacteria.
Supplementary Material
Acknowledgments
We thank Christine Mech, Sean Van Tongeren, Jay Wells, Daniel Reed, and Meagan Cooper for technical support and Drs. Mansour Mohamadzadeh, Javad Aman, and James Burnett for critical review of the manuscript.
This work was supported, in whole or in part, by National Institutes of Health Grant N01-CO-12400, by the Defense Threat Reduction Agency (to S. B. and R. G. P.), the NIAID, National Institutes of Health Grant R43 A1055102 (to W. C. R.), and by the Developmental Therapeutics Program in the Division of Cancer Treatment and Diagnosis of the NCI, National Institutes of Health.
The on-line version of this article (available at http://www.jbc.org) contains supplemental Figs. 1–8 and Tables 1 and 2.
Footnotes
The abbreviations used are: PTP, protein-tyrosine phosphatase; PMO, phosphorodiamidate morpholino oligomers; LF, lethal factor; MAPKK/MEK, mitogen-activated protein kinase kinase; LT, lethal toxin; DiFMUP, 6,8-difluoro-4-methylumbelliferyl phosphate; PA, protective antigen; CFU, colony-forming units; m.o.i., multiplicity of infection; PBS, phosphate-buffered saline.
E. L. Virts, N. Raschke, R. G. Panchal, S. Bavari and W. C. Raschke, manuscript in preparation.
References
- 1.Bhavsar, A. P., Guttman, J. A., and Finlay, B. B. (2007) Nature 449 827-834 [DOI] [PubMed] [Google Scholar]
- 2.Finlay, B. B., and Cossart, P. (1997) Science 276 718-725 [DOI] [PubMed] [Google Scholar]
- 3.Ducruet, A. P., Vogt, A., Wipf, P., and Lazo, J. S. (2005) Annu. Rev. Pharmacol. Toxicol. 45 725-750 [DOI] [PubMed] [Google Scholar]
- 4.Pei, Z., Liu, G., Lubben, T. H., and Szczepankiewicz, B. G. (2004) Curr. Pharm. Des. 10 3481-3504 [DOI] [PubMed] [Google Scholar]
- 5.Bialy, L., and Waldmann, H. (2005) Angew. Chem. Int. Ed. Engl. 44 3814-3839 [DOI] [PubMed] [Google Scholar]
- 6.Umezawa, K., Kawakami, M., and Watanabe, T. (2003) Pharmacol. Ther. 99 15-24 [DOI] [PubMed] [Google Scholar]
- 7.Lazo, J. S., and Wipf, P. (2003) Oncol. Res. 13 347-352 [DOI] [PubMed] [Google Scholar]
- 8.Tautz, L., Pellecchia, M., and Mustelin, T. (2006) Expert Opin. Ther. Targets 10 157-177 [DOI] [PubMed] [Google Scholar]
- 9.Alonso, A., Sasin, J., Bottini, N., Friedberg, I., Friedberg, I., Osterman, A., Godzik, A., Hunter, T., Dixon, J., and Mustelin, T. (2004) Cell 117 699-711 [DOI] [PubMed] [Google Scholar]
- 10.Andersen, J. N., Jansen, P. G., Echwald, S. M., Mortensen, O. H., Fukada, T., Del Vecchio, R., Tonks, N. K., and Moller, N. P. (2004) FASEB J. 18 8-30 [DOI] [PubMed] [Google Scholar]
- 11.Bottini, N., Bottini, E., Gloria-Bottini, F., and Mustelin, T. (2002) Arch. Immunol. Ther. Exp. (Warsz) 50 95-104 [PubMed] [Google Scholar]
- 12.Higashi, H., Tsutsumi, R., Muto, S., Sugiyama, T., Azuma, T., Asaka, M., and Hatakeyama, M. (2002) Science 295 683-686 [DOI] [PubMed] [Google Scholar]
- 13.Nandan, D., Knutson, K. L., Lo, R., and Reiner, N. E. (2000) J. Leukocyte Biol. 67 464-470 [DOI] [PubMed] [Google Scholar]
- 14.Black, D. S., Marie-Cardine, A., Schraven, B., and Bliska, J. B. (2000) Cell. Microbiol. 2 401-414 [DOI] [PubMed] [Google Scholar]
- 15.Agrawal, A., and Pulendran, B. (2004) Cell. Mol. Life Sci. 61 2859-2865 [DOI] [PubMed] [Google Scholar]
- 16.Duesbery, N. S., Webb, C. P., Leppla, S. H., Gordon, V. M., Klimpel, K. R., Copeland, T. D., Ahn, N. G., Oskarsson, M. K., Fukasawa, K., Paull, K. D., and Vande Woude, G. F. (1998) Science 280 734-737 [DOI] [PubMed] [Google Scholar]
- 17.Friedlander, A. M., Bhatnagar, R., Leppla, S. H., Johnson, L., and Singh, Y. (1993) Infect. Immun. 61 245-252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh, Y., Leppla, S. H., Bhatnagar, R., and Friedlander, A. M. (1989) J. Biol. Chem. 264 11099-11102 [PubMed] [Google Scholar]
- 19.Kim, S. O., Jing, Q., Hoebe, K., Beutler, B., Duesbery, N. S., and Han, J. (2003) J. Biol. Chem. 278 7413-7421 [DOI] [PubMed] [Google Scholar]
- 20.Pellizzari, R., Guidi-Rontani, C., Vitale, G., Mock, M., and Montecucco, C. (1999) FEBS Lett. 462 199-204 [DOI] [PubMed] [Google Scholar]
- 21.Ribot, W. J., Panchal, R. G., Brittingham, K. C., Ruthel, G., Kenny, T. A., Lane, D., Curry, B., Hoover, T. A., Friedlander, A. M., and Bavari, S. (2006) Infect. Immun. 74 5029-5034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Panchal, R. G., Ruthel, G., Brittingham, K. C., Lane, D., Kenny, T. A., Gussio, R., Lazo, J. S., and Bavari, S. (2007) Chem. Biol. 14 245-255 [DOI] [PubMed] [Google Scholar]
- 23.Virts, E. L., and Raschke, W. C. (2001) J. Biol. Chem. 276 19913-19920 [DOI] [PubMed] [Google Scholar]
- 24.Virts, E. L., Diago, O., and Raschke, W. C. (2003) Blood 101 849-855 [DOI] [PubMed] [Google Scholar]
- 25.Desai, D. M., Sap, J., Silvennoinen, O., Schlessinger, J., and Weiss, A. (1994) EMBO J. 13 4002-4010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moulton, H. M., Nelson, M. H., Hatlevig, S. A., Reddy, M. T., and Iversen, P. L. (2004) Bioconjugate Chem. 15 290-299 [DOI] [PubMed] [Google Scholar]
- 27.Summerton, J., and Weller, D. (1997) Antisense Nucleic Acid Drug Dev. 7 187-195 [DOI] [PubMed] [Google Scholar]
- 28.Lazo, J. S., Nemoto, K., Pestell, K. E., Cooley, K., Southwick, E. C., Mitchell, D. A., Furey, W., Gussio, R., Zaharevitz, D. W., Joo, B., and Wipf, P. (2002) Mol. Pharmacol. 61 720-728 [DOI] [PubMed] [Google Scholar]
- 29.Tang, G., and Leppla, S. H. (1999) Infect. Immun. 67 3055-3060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alexander, D. R. (2000) Semin. Immunol. 12 349-359 [DOI] [PubMed] [Google Scholar]
- 31.Thomas, M. L., and Brown, E. J. (1999) Immunol. Today 20 406-411 [DOI] [PubMed] [Google Scholar]
- 32.Hermiston, M. L., Xu, Z., and Weiss, A. (2003) Annu. Rev. Immunol. 21 107-137 [DOI] [PubMed] [Google Scholar]
- 33.Shen, F., Xu, X. L., Graf, L. H., and Chong, A. S. (1995) J. Immunol. 154 644-652 [PubMed] [Google Scholar]
- 34.Huntington, N. D., Xu, Y., Nutt, S. L., and Tarlinton, D. M. (2005) J. Exp. Med. 201 1421-1433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berger, S. A., Mak, T. W., and Paige, C. J. (1994) J. Exp. Med. 180 471-476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gao, H., Henderson, A., Flynn, D. C., Landreth, K. S., and Ericson, S. G. (2000) Exp. Hematol. 28 1062-1070 [DOI] [PubMed] [Google Scholar]
- 37.Montoya, M., Dawes, R., Reid, D., Lee, L. N., Piercy, J., Borrow, P., Tchilian, E. Z., and Beverley, P. C. (2006) Eur. J. Immunol. 36 2150-2158 [DOI] [PubMed] [Google Scholar]
- 38.Piercy, J., Petrova, S., Tchilian, E. Z., and Beverley, P. C. (2006) Immunology 118 250-256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Urbanek, R. A., Suchard, S. J., Steelman, G. B., Knappenberger, K. S., Sygowski, L. A., Veale, C. A., and Chapdelaine, M. J. (2001) J. Med. Chem. 44 1777-1793 [DOI] [PubMed] [Google Scholar]
- 40.Park, J. M., Greten, F. R., Li, Z. W., and Karin, M. (2002) Science 297 2048-2051 [DOI] [PubMed] [Google Scholar]
- 41.Muehlbauer, S. M., Evering, T. H., Bonuccelli, G., Squires, R. C., Ashton, A. W., Porcelli, S. A., Lisanti, M. P., and Brojatsch, J. (2007) Cell Cycle 6 758-766 [DOI] [PubMed] [Google Scholar]
- 42.McNeill, L., Salmond, R. J., Cooper, J. C., Carret, C. K., Cassady-Cain, R. L., Roche-Molina, M., Tandon, P., Holmes, N., and Alexander, D. R. (2007) Immunity 27 425-437 [DOI] [PubMed] [Google Scholar]
- 43.Brossier, F., Weber-Levy, M., Mock, M., and Sirard, J. C. (2000) Infect. Immun. 68 1781-1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cote, C. K., Rea, K. M., Norris, S. L., van Rooijen, N., and Welkos, S. L. (2004) Microb. Pathog. 37 169-175 [DOI] [PubMed] [Google Scholar]
- 45.Lyons, C. R., Lovchik, J., Hutt, J., Lipscomb, M. F., Wang, E., Heninger, S., Berliba, L., and Garrison, K. (2004) Infect. Immun. 72 4801-4809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pickering, A. K., Osorio, M., Lee, G. M., Grippe, V. K., Bray, M., and Merkel, T. J. (2004) Infect. Immun. 72 6382-6389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Basha, S., Rai, P., Poon, V., Saraph, A., Gujraty, K., Go, M. Y., Sadacharan, S., Frost, M., Mogridge, J., and Kane, R. S. (2006) Proc. Natl. Acad. Sci. U. S. A. 103 13509-13513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wei, W., Lu, Q., Chaudry, G. J., Leppla, S. H., and Cohen, S. N. (2006) Cell 124 1141-1154 [DOI] [PubMed] [Google Scholar]
- 49.Ryan, P. L., and Young, J. A. (2008) PLoS ONE 3 e1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li, X. L., Ezelle, H. J., Kang, T. J., Zhang, L., Shirey, K. A., Harro, J., Hasday, J. D., Mohapatra, S. K., Crasta, O. R., Vogel, S. N., Cross, A. S., and Hassel, B. A. (2008) Proc. Natl. Acad. Sci. U. S. A. 105 20816-20821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Crawford, M. A., Zhu, Y., Green, C. S., Burdick, M. D., Sanz, P., Alem, F., O'Brien, A. D., Mehrad, B., Strieter, R. M., and Hughes, M. A. (2009) Infect. Immun. 77 1664-1678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kang, T. J., Basu, S., Zhang, L., Thomas, K. E., Vogel, S. N., Baillie, L., and Cross, A. S. (2008) Eur. J. Immunol. 38 1574-1584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walberg, K., Baron, S., Poast, J., Schwartz, B., Izotova, L., Pestka, S., and Peterson, J. W. (2008) J. Interferon Cytokine Res. 28 597-601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Glomski, I. J., Corre, J. P., Mock, M., and Goossens, P. L. (2007) J. Immunol. 178 2646-2650 [DOI] [PubMed] [Google Scholar]
- 55.Zamoyska, R. (2007) Immunity 27 421-423 [DOI] [PubMed] [Google Scholar]
- 56.Boyden, E. D., and Dietrich, W. F. (2006) Nat. Genet. 38 240-244 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.