Abstract
Migraine can be characterized as a chronic disorder with episodic attacks and the potential for progression to chronic migraine. We conducted a PubMed literature search (January 1, 1970 through May 31, 2008) for studies on the impact of migraine, including disability, health-related quality of life (HRQoL), comorbidities, and instruments used by health care professionals to treat patients with migraine. Numerous studies have shown that migraine substantially impairs a person's functions during attacks and diminishes HRQoL during and between attacks. Despite its impact, migraine remains underestimated, underdiagnosed, and undertreated. Several tools are available to help physicians assess the impact of migraine on the daily activities and HRQoL of their patients, such as the 36-Item Short-Form Health Survey and the Headache Impact Test. Improving communication during the office visit through active listening, use of open-ended questions, and use of the “ask-tell-ask” strategy can also help in assessing migraine-related impairment. Together, these tools and communication techniques can lead to a more complete assessment of how migraine affects patients' lives and can aid in the development of the optimal treatment plan for each patient. Both pharmacotherapy (acute and preventive treatment strategies) and nonpharmacological therapies play important roles in the management of migraine.
AMCS = American Migraine Communication Study; HIT = Headache Impact Test; HRQoL = health-related quality of life; MIBS = Migraine Interictal Burden Scale; MIDAS = Migraine Disability Assessment; MPQ = Migraine Prevention Questionnaire; MSQ = Migraine-Specific Quality of Life Questionnaire; PHQ = Patient Health Questionnaire; SF = Short-Form Health Survey
Migraine is recognized as a major cause of disability worldwide. The World Health Report 2001—Mental Health: New Understanding, New Hope cited 135 health conditions, particularly mental and neurologic disorders, that accounted for nearly 40% of all years lived with disability worldwide. Migraine was cited as the 19th leading cause of years lived with disability among both males and females of all ages combined and the 12th leading cause of years lived with disability among females of all ages.1 Females with migraine outnumber males with migraine by nearly 3 to 1.2
Migraine can be characterized as a chronic disorder with episodic attacks, with potential for progression to more frequent and severe patterns.3 Some patients whose migraine attacks are initially episodic experience increasing frequency of headaches over months or years, leading to chronic migraine, in which headaches occur at least 15 days per month.4 Migraine is associated with substantial functional impairment,5 which may include both physical and emotional ramifications. Many aspects of the lives of migraineurs are commonly affected by the condition, including occupational, academic, social, leisure, and family life and responsibilities.5-8 It is well known that migraine headaches cause substantial impairment during attacks (ictal burden). However, mounting evidence suggests that migraines also cause impairment between attacks (interictal burden). In general, migraineurs report poorer subjective well-being and reduced health-related quality of life (HRQoL) during pain-free periods than do age- and sex-matched persons without migraine.8-11
For editorial comment, see page 397
Health care professionals often do not recognize the degree and scope of functional impairment imposed by migraine.7,10,12-14 This contributes to missed opportunities for providing effective acute treatment (medication taken at the time of an attack) and preventive pharmacological (medication taken on a daily basis or other scheduled protocol to avoid attacks) and biobehavioral interventions.7,12,14
We review the total burden of migraine and strategies for managing both the ictal and the interictal burden. A PubMed search of English-language articles published from January 1, 1970 through May 31, 2008 was conducted. The following keywords were used in our search: migraine, headache, migraine prevention, migraine prophylaxis or treatment, migraine disability, headache disability, migraine quality of life or health-related quality of life, migraine functional impairment, migraine assessment tools or scales or questionnaire, and migraine communication. The inclusion of specific studies was based on subjective, comparative evaluation and standard levels of evidence, with instruments that had the strongest psychosomatic data (validity, reliability) given more weight. Likewise, tools relevant to assist health care professionals with treatment of patients were selected.
FUNCTIONAL IMPAIRMENT AND INDIRECT COSTS
Numerous studies have shown that migraine adversely affects daily functioning. In a 5-nation study by Brandes,15 more than half (52.3%) of the 516 adults with migraine interviewed required bed rest to manage their headache attacks. Data from the National Health Interview Survey conducted in 1989 revealed that migraine caused an estimated 10% of US school-aged children to miss, on average, at least 1 day of school during a 2-week period; furthermore, migraine was responsible for restricting activity by an estimated 2.7 million days per year for employed men, 18.8 million days for employed women, and 38.5 million days for housewives (terminology used in original text).16
The indirect cost (ie, excluding direct medical costs) of migraine to employers is enormous. In the study by Stewart et al17 of lost productive time attributable to common pain conditions in the US workforce during a 2-week period, headache was the most common, leading to a mean ± SD loss in productive time of 3.5±0.1 hours per week, followed by back pain and arthritis. Using a large employer database, Hawkins et al18 determined that, for employers, the cost associated with each employee with recognized migraine is approximately $2800 more annually than that for each employee without migraine, primarily because of absenteeism but also because of short-term disability and workers' compensation claims. Projected nationally, the indirect cost of migraine to US employers is approximately $12 billion annually. Migraine also affects the family lives and relationships of migraineurs.19,20
FUNCTIONAL IMPAIRMENT BETWEEN MIGRAINE ATTACKS
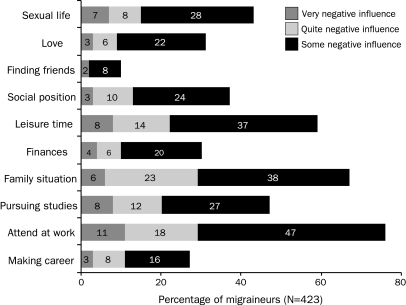
Results of an online poll (N=505) conducted in the United States indicate that migraine imposes a substantial interictal burden (between migraine attacks).11 Of migraineurs surveyed, 76% worried that they would have migraines for the rest of their lives, and 37% worried about migraines between attacks.11 As a patient in another study explained, “I don't travel far by myself, 'cause I never know when it's gonna hit me.”14 Of 423 Swedish adults with migraine surveyed by mail, fewer than half (43%) stated that they recovered completely between attacks. The adverse impact of migraine on key aspects of these respondents' lives is shown in Figure 1.8 In an earlier Swedish study, migraineurs (N=138) reported more subjective symptoms (eg, disturbed vitality, sleep) and a lesser sense of well-being during headache-free periods than did age- and sex-matched controls.9
FIGURE 1.
Impact of migraine on important aspects of life. From Cephalalgia,8 with permission from Blackwell Publishing.
Anxiety in anticipation of the next migraine attack (interictal anxiety) may lead migraineurs to take pain medications before any symptoms of an attack occur, ultimately resulting in overuse of these medications. Phobic avoidance of activities because of fear of migraine or headache (cephalalgiaphobia) is a contributor to the interictal burden of migraine.21 Peres et al21 suggest that cephalalgiaphobia may decrease the threshold for initiating analgesics, leading to acute medication overuse. When episodic migraine is accompanied by acute medication overuse, rebound headaches can occur and may lead to medication overuse headache.22,23 Revised diagnostic criteria for medication overuse headache were published in 2005.24
ASSESSMENT OF ICTAL FUNCTIONAL IMPAIRMENT
Several tools are available for assessing the ictal impact of migraine. The Migraine Disability Assessment (MIDAS) questionnaire25 and Headache Impact Test (HIT)26 can be used in headache assessment in general and in overall headache and migraine management.27 MIDAS is a self-administered questionnaire that consists of 5 questions about days of missed activity or substantially reduced activity in 3 domains: school work or work for pay, household work or chores, and nonwork (family, social, and leisure) activities. Two additional questions pertain to pain frequency and intensity.28 HIT is available in a brief 6-question version known as HIT-6.27,29 This test measures not only lost time in 3 domains but also other areas of impact (eg, pain severity, fatigue, mood).27,29,30 The Headache Disability Inventory31 and Headache Impact Questionnaire32 are helpful research tools but are not ideal for use in clinical practice, partly because they are difficult to score.33 Another useful scale is the International Classification of Functioning, Disability, and Health, which was approved by the World Health Assembly in 2001.34 The International Classification of Functioning, Disability, and Health is not an assessment tool but rather a framework for measuring and comparing the degree of disability caused by migraine and other mental and neurologic disorders and chronic illnesses.5
ASSESSMENT OF INTERICTAL BURDEN
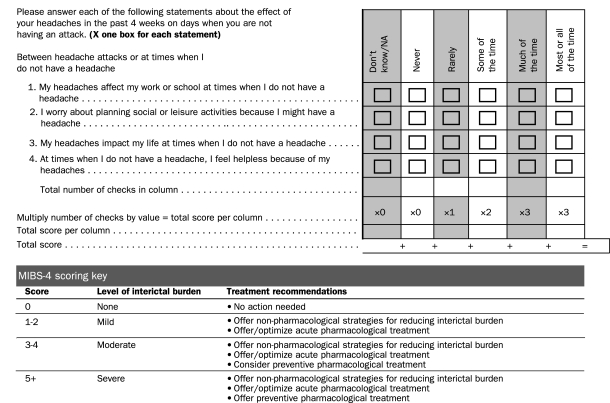
The Migraine Interictal Burden Scale (MIBS) measures interictal migraine-related burden in 4 domains: impairment in work or school, impairment in family and social life, difficulty making plans or commitments, and emotional/affective and cognitive distress.35 MIBS-4 is a 4-item, self-administered questionnaire for clinical use or screening purposes (Figure 2). Because the burden of migraine during attacks only partially predicts the burden between attacks, physicians should routinely ask their patients about the interictal burden of their headaches as a prelude to developing an optimal treatment plan.36
FIGURE 2.
Four-item clinic version of the Migraine Interictal Burden Scale (MIBS-4).
GENERIC AND DISEASE-SPECIFIC MEASURES OF HRQoL
The most widely used generic measures of HRQoL are the 36- and 12-Item Short-Form Health Surveys (SF-36 and SF-12). The SF-36 assesses a range of symptoms associated with common diseases.37 Migraineurs have significantly lower SF-36 scores than persons without migraine, and migraine adversely affects functioning at least as much as depression, diabetes mellitus, and recent myocardial infarction.37 Also, migraineurs have significantly lower HRQoL than those in the general population with no chronic condition.38-40 One of the instruments specifically designed to assess the impact of migraine on HRQoL, the Migraine-Specific Quality of Life Questionnaire (MSQ) version 2.1, consists of 14 items that measure the degree to which migraine affects the patient's daily activities (social life, work) and emotions during a 4-week period.41
SELECTED STUDIES OF ICTAL AND INTERICTAL MIGRAINE-RELATED FUNCTIONAL IMPAIRMENT, REDUCED QUALITY OF LIFE, AND PSYCHIATRIC COMORBIDITIES IN MIGRAINEURS
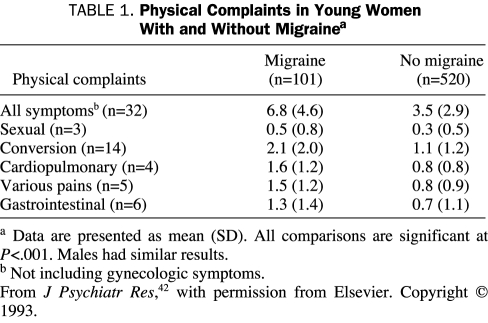
The results of the following studies indicate that migraine is associated with functional impairment, reduced HRQoL, and an increase in comorbid psychiatric conditions. Using personal interviews and follow-up telephone interviews, Breslau and Davis42 studied the association between migraine and psychiatric disorders, physical complaints, indicators of functional impairment, and use of mental health services in 1007 young adults living in southeastern Michigan. Among the key findings were that persons with a history of migraine had significantly more physical symptoms (other than headache) than persons with no history of migraine (Table 1). Migraineurs also had higher lifetime rates of depressive disorders, panic disorder, obsessive-compulsive disorder, generalized anxiety disorder, specific phobias, and suicide attempts than controls and were more likely to have missed work in the preceding month, to assess their general health as “fair” or “poor,” and to use mental health services.42 Increased comorbidity rates between migraine and certain psychiatric disorders were also found in the 2002 Canadian Community Health Survey.43 Mental health data collected in that study indicated that major depressive disorder, bipolar disorder, panic disorder, and social phobia were more than twice as common in migraineurs as in controls. Mental health care use and HRQoL were poorest in those individuals who had both migraine and a psychiatric disorder.
TABLE 1.
Physical Complaints in Young Women With and Without Migrainea
In a population-based, case-control study of residents of greater London, England, Lipton et al44 compared HRQoL between persons with and without migraines and studied the association between HRQoL and work-related disability due to headache. By means of a telephone survey, the investigators randomly selected 200 migraineurs and matched them to 200 controls. The migraineurs scored significantly lower than the controls in 8 of the 9 HRQoL domains of the SF-36, as well as in the 2 summary scores (total physical component summary and total mental component summary). In another analysis, migraineurs were classified as having low, moderate, or high work-related disability according to the number of days during the past year that headache caused them to either miss work or experience reduced work productivity (by half or more). Migraineurs in the high-disability group had substantially lower HRQoL scores than those in the low-disability group for the role-physical (ability to do work or perform other daily activities as a result of physical health), bodily pain, vitality (energy), and social functioning domains of the SF-36. As the degree of disability increased from low to moderate or severe, HRQoL decreased. The investigators concluded that migraine profoundly affects HRQoL and that migraine disability is inversely correlated with HRQoL.44
Dueland et al45 used a telephone survey to study the impact of migraine on work, family, and leisure among 1810 young women living in Israel and 8 European countries. During the prior 6 months, the mean number of missed work or school days due to migraine for the study participants was 1.9, and the mean number of days that they arrived late or left early was 1.5. During the preceding 6 months, 74% of participants reported being unable to function fully at work or school because of migraine, 62% reported 1 or more instances of being unable to spend time with family or friends because of migraine, and 67% reported 1 or more instances of being unable to enjoy recreational or leisure activities because of migraine.45 Lantéri-Minet et al46 analyzed responses to a 2-phase survey designed to explore the influence of anxiety and depression on functional ability and HRQoL in adults with migraine. Compared with individuals who did not have migraine, the 1652 respondents with active migraine had significantly lower mean scores on all 8 scales (P<.01) of the SF-1247 except the physical functioning scale. A significantly higher percentage of individuals with migraine vs those without (P<.01) had anxiety symptoms alone or combined depression and anxiety symptoms.
To examine headache-related interictal burden, Buse et al36 mailed surveys to an independent, stratified population-based sample of 2500 individuals with severe headache. Headache symptoms were used to identify migraine cases based on International Classification of Headache Disorders II criteria.48 Valid returns were obtained from 1734 individuals (69%), and of these, 1391 (80%) met International Classification of Headache Disorders II criteria for migraine. Surveys also included MIBS, MIDAS,33 Patient Health Questionnaire (PHQ) depression module,49 PHQ anxiety and panic disorder modules,50 MSQ version 2.1,41 Migraine Prevention Questionnaire (MPQ), HIT-6 version 1.1,29 Migraine Treatment Optimization Scale,51,52 and Lost Productive Time Work and Health Questionnaire, which includes measures of absenteeism (missed work) and presenteeism (reduced efficiency and productivity during work).53
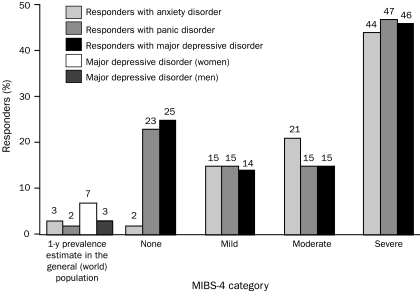
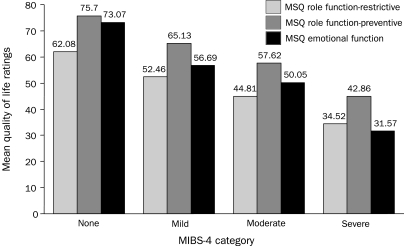
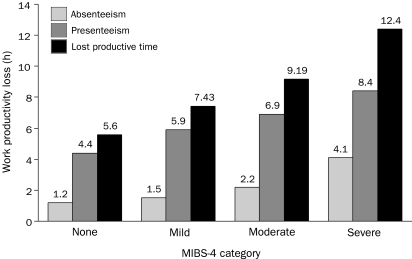
The researchers found moderate positive correlations between MIBS-4 and measures of ictal disability (MIDAS, HIT-6) and several psychological disorders (Figure 3).36,54 As interictal burden increased, so did the prevalence of anxiety disorder, panic disorder, and major depressive disorder. The researchers noted moderate negative correlations between MIBS-4 and HRQoL indicators (as measured by the 3 subscales of MSQ); as interictal burden increased, HRQoL decreased and vice versa (Figure 4).36 In addition, the researchers found moderate positive correlations between MIBS-4 and measures of workplace productivity (lost productive time, absenteeism, presenteeism) (Figure 5).36
FIGURE 3.
Depression, anxiety, and panic disorder in persons with migraine by level of interictal burden as measured by the 4-item Migraine Interictal Burden Scale (MIBS-4).
FIGURE 4.
Mean quality of life ratings (Migraine-Specific Quality of Life Questionnaire [MSQ] subscales) in persons with migraine by level of interictal burden as measured by the 4-item Migraine Interictal Burden Scale (MIBS-4). MSQ role function-restrictive is a measure of the degree to which performance of daily activities is limited by migraines; MSQ role function-preventive is a measure of the degree to which performance of daily activities is interrupted by migraines; MSQ emotional function examines feelings of frustration and helplessness due to migraine.
FIGURE 5.
Absenteeism, presenteeism, and lost productive time in persons with migraine by level of interictal burden as measured by the 4-item Migraine Interictal Burden Scale (MIBS-4).
ROLE OF HEALTH CARE PROFESSIONALS IN ASSESSING MIGRAINE-RELATED FUNCTIONAL IMPAIRMENT, HRQoL, AND COMMON COMORBID CONDITIONS
Effective communication plays a key role in the quality of medical care. Consensus statements from medical professional groups, regulatory agencies, health care professionals, researchers, and patients all recognize its importance.55-58 Although high-quality medical communication contributes to patient satisfaction,59-62 adherence to treatment plans,63 improved medical outcomes,64,65 and decreased risk of malpractice,66 many health care professionals have not had relevant training and lack confidence in their communication skills.13,67-70 Fortunately, research shows that medical communication skills can be successfully taught and acquired,12,14,71,72 leading to improved outcomes.12 Many patients think that their physicians do not understand the impact of headaches on their lives.10 Patients rarely spontaneously mention functional impairment and emotional consequences,27 and physicians do not routinely seek disability information from their patients with migraine.12 However, information about the functional consequences of headache has been shown to positively affect physicians' perceptions and prescribing behavior.12 Eliciting that information helps physicians assess the effect of migraine on their patients' lives and may uncover the need for more aggressive and/or comprehensive treatment plans.
Researchers in the American Migraine Communication Study (AMCS) examined routine communication in headache care (AMCS I)13 and the effectiveness of a brief educational intervention aimed at improving communication in headache care (AMCS II).14 The AMCS I was an observational study in which researchers audiotaped and videotaped actual office visits and conducted separate postvisit interviews with both health care professionals and patients. During these discussions, health care professionals asked an average of 13 questions, of which 91% of those that were migraine specific were closed-ended or short-answer questions focused on frequency (primarily number of attacks per month), severity, headache symptoms, triggers, and other similar features. Questions regarding headache-related impairment and quality of life were rare. Of 20 patients in the study who would be considered appropriate candidates for preventive medication according to a predetermined algorithm, 80% did not receive a preventive treatment strategy, and 50% did not discuss preventive treatment options during the appointment. Interviews with health care professionals and their patients separately after their visits indicated that 55% of health care professional and patient pairs did not report matching information on frequency, and 51% did not agree on impairment. By relying almost exclusively on closed-ended questions, these health care professionals limited their patients' ability to communicate the effect of migraine on their lives. In addition, asking about migraine attacks and not migraine days led professionals to underestimate the number of headache days per month.
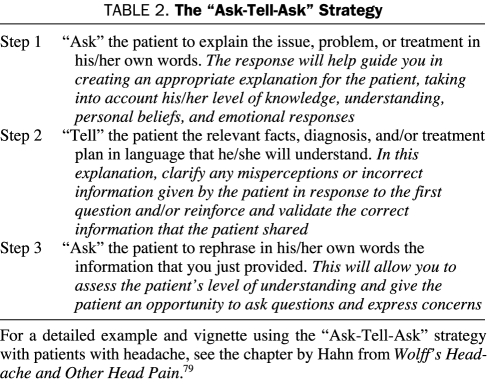
In a subsequent study, researchers developed and tested a brief educational intervention (AMCS II) designed to target deficits observed during AMCS I. In AMCS II, 15 health care professionals who participated in AMCS I participated in an audio interactive, 90-minute, Internet-based training session that reviewed the results of AMCS I and provided 2 communication strategies: the patient-centered “ask-tell-ask” strategy to assess frequency73,74 and use of open-ended questions to assess migraine-related impairment.75 These types of communication techniques are effective76 and are linked to higher levels of both patient and health care professional satisfaction.31,77,78 According to the theory that effective education requires assessing what the patient already knows and believes and then building on (or correcting when necessary) that understanding, the “ask-tell-ask” strategy can be used for any medical communication. In this study, it was used primarily to ensure optimal communication about migraine frequency in headache days. The “ask-tell-ask” strategy is based on 3 simple steps, which can be continued for as long as appropriate (Table 2).79
TABLE 2.
The “Ask-Tell-Ask” Strategy
Use of open-ended questions and the “ask-tell-ask” strategy was found to shorten office visits. In AMCS I (no intervention used), the average visit lasted a median of 11 minutes, whereas in AMCS II (“ask-tell-ask” strategy used), the average visit lasted a median of 9.5 minutes. Furthermore, the median time spent discussing impairment was just more than 1 minute in AMCS I vs less then 30 seconds in AMCS II.14 The recommended techniques led to a more accurate picture of patients' migraine frequency and impairment during and between attacks, more frequent discussion and prescription of preventive and acute treatment, and greater satisfaction with office visits on the part of health care professionals and patients. Open-ended questions about migraine-related impairment and disability yielded information on ictal and interictal burden in 75% of sessions compared with 52% of sessions with closed-ended questions. Using the “ask-tell-ask” strategy increased the frequency of discussion of preventive therapy from 50% of eligible candidates (AMCS I) to 74% (AMCS II).
In addition to gathering data on headache-related functional impairment and HRQoL, health care professionals should inquire about comorbidities, such as mood disorders (eg, depression and anxiety), loss of sleep, low energy level, and poor occupational, social, and family functioning (eg, parenting, marital issues such as conflict, sexual issues). Epidemiological studies show an association between migraine and anxiety, mood, and personality disorders.80,81 Questions about the patient's mood and well-being show concern, contribute to a positive therapeutic alliance, and are associated with higher levels of patient satisfaction,82 reduced emotional distress,68 and symptom resolution.83
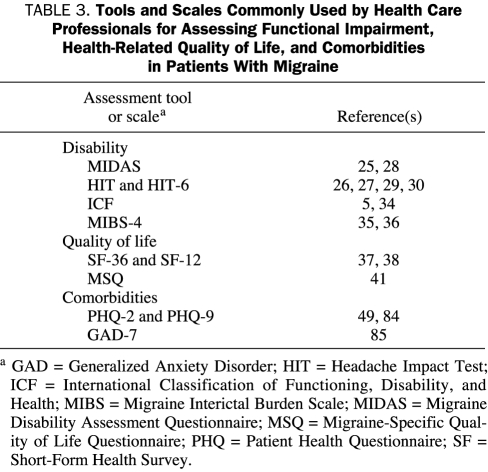
Brief screening instruments can be used to assess depression and anxiety and have been shown to significantly improve the detection of comorbid conditions in clinical practice (Table 3). The PHQ-2 is a 2-item screening instrument that has been empirically shown to detect the presence of depression.84 The PHQ-9 can be used to conduct a more detailed yet still time-efficient evaluation.49 Clinically significant anxiety can be evaluated using the Generalized Anxiety Disorder 7, a 7-item, self-administered questionnaire.85 Once the questionnaires are completed, the health care professional can review them with the patient during the visit; they may facilitate discussion about other areas of concern and further inform treatment decisions. The remaining steps are to educate the patient about migraine, common comorbidities, the taxing effect migraine can have on an individual's life, and treatment options. The patient can then be encouraged to participate in the management of his or her migraines and work with the professional to develop an individualized treatment plan.86 Strategies for building rapport with patients and teaching them how to work with their health care professionals have been reviewed elsewhere and are beyond the scope of this review. (For reviews of effective medical communication strategies, see Hahn79 and Buse and Lipton.87 For reviews of techniques to enhance patient compliance and motivation, see Rains et al88 and Miller and Rollnick.89)
TABLE 3.
Tools and Scales Commonly Used by Health Care Professionals for Assessing Functional Impairment, Health-Related Quality of Life, and Comorbidities in Patients With Migraine
TREATMENT OF MIGRAINE
An array of effective acute and preventive pharmacological and nonpharmacological (ie, biobehavioral) therapies is available to the health care professional for use in treating migraine. The main goals of therapy are to avoid attacks when possible, treat attacks rapidly and consistently with no recurrences, and restore the patient's ability to function and HRQoL.90 Treatment should be individualized for each patient, taking into account variables such as frequency and severity of migraine episodes, trigger factors, comorbidities, patient's lifestyle, and patient preferences.91
Pharmacotherapy
Pharmacotherapy for migraine has been extensively reviewed.90,92-95 The mainstay of acute migraine therapy consists of certain nonspecific agents used for various pain disorders, including headache (eg, aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs), and migraine-specific agents (eg, ergotamine, dihydroergotamine, and the triptans).93 In the stepped-care approach to acute care, treatment is escalated across or within attacks, beginning with simple analgesics. If these agents provide inadequate relief, an analgesic plus an antiemetic or some other combination of medications may be tried. Migraine-specific agents are reserved for use when simpler, inexpensive treatments have failed.96 The US Headache Consortium guidelines recommend a stratified-care approach in which the choice of agent is guided by frequency and severity of the migraine attack, degree of disability, associated nonheadache symptoms such as nausea, previous response to medications, and presence of any comorbid disorders.90
Medications with the highest quality of evidence of efficacy are aspirin, ibuprofen, butorphanol nasal spray, oral opiate combinations, dihydroergotamine nasal spray, and triptans (injectable, oral, and nasal spray). Migraine-specific agents such as the triptans are recommended for patients with moderate to severe migraines or milder headaches that do not respond adequately to nonsteroidal anti-inflammatory drugs or a combination of medications, such as aspirin, acetaminophen, and caffeine.90,92,93 Health care professionals must be sure that patients know how to use acute medications for migraine correctly and understand that overuse can increase the frequency and severity of headaches and reduce treatment efficacy. Medication overuse can be detected by routinely asking questions. (1) Do you ever take a pill before social events or work meetings or because you are anxious before migraine symptoms start? (2) Do you ever take a pill just in case? (3) Do you use acute treatment 3 or more days a week? (4) In addition to your prescription medications, about how often do you take over-the-counter pain medications?97 Health care professionals should discourage patients from anticipatory use of symptomatic medications and set limits on their use to prevent the development of medication overuse headache. Although the majority of migraineurs take acute medication, almost 40% meet the criteria for preventive treatment. Preventive therapy is intended to reduce the frequency of attacks or eliminate them, to reduce the cumulative impact of repeated attacks on the patient's HRQoL and level of disability, to improve the efficacy of acute treatment, and, in some patients, to prevent transformation of episodic migraine to chronic migraine.98,99 Preventive therapies are commonly underused in patients who may be appropriate candidates and who may benefit from treatment. In the American Migraine Prevalence and Prevention survey, 43.3% of migraineurs had never used a migraine preventive agent, although among them 32.4% met expert guideline criteria for considering it (13.1%) or being offered it (19.3%).100 One reason for undertreatment of migraine may be health care professionals' lack of awareness of the positive effects of preventive medications on the HRQoL of migraineurs.99 Using the interviewing techniques of AMCS II to determine the number of migraine days and degree of impairment will help physicians decide whether to consider or offer preventive therapy.
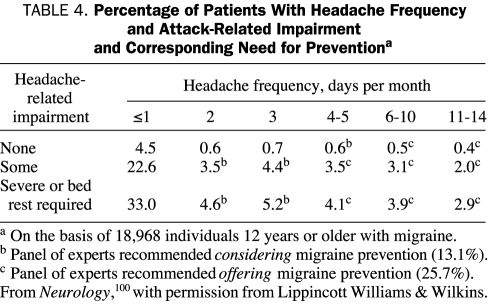
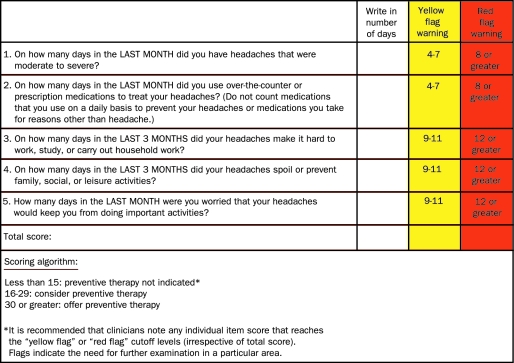
Guidelines for determining the need for preventive therapy based on headache frequency and degree of impairment are presented in Table 4.100 To facilitate clinical implementation of these guidelines in practice, researchers developed the MPQ-5 (Figure 6); psychometric testing demonstrated good reliability and validity.101 The MPQ-5 assesses headache frequency, use of acute treatment, headache-related impairment in several domains, and worry and anxiety related to headache. Responses are summed for a total score, which falls into 1 of 3 categories: preventive treatment not indicated, consider preventive treatment, and offer preventive treatment. In addition, each of the 5 questions has individual cutoff scores, which may raise a “yellow flag” or “red flag.” This information should be used as an indicator that the health care professional should gather additional information and consider appropriate treatments. The β-blockers propranolol and timolol and the neuromodulators divalproex sodium and topiramate are approved for migraine prevention in adults.102-105
TABLE 4.
Percentage of Patients With Headache Frequency and Attack-Related Impairment and Corresponding Need for Preventiona
FIGURE 6.
Migraine Prevention Questionnaire 5 (MPQ-5).
Other agents used for migraine prevention include anti-depressants98,106 and calcium channel blockers; natural products, such as vitamin B2, botulinum toxin, Petasites, and coenzyme Q-10, are useful in some patients.99,107 Our focus is on studies of daily activities and HRQoL with medications that have achieved regulatory approval for use in migraine prophylaxis. With the exception of divalproex sodium, for which improvements in HRQoL measures have been reported in adolescents with migraine,108 most studies have been conducted with topiramate. Garcia-Monco et al109 recently compared the effects of preventive therapy with topiramate and nadolol (which is used off-label for migraine prophylaxis) on HRQoL in patients with migraine. Both drugs significantly improved the SF-36 role-physical domain, but the improvement associated with topiramate treatment was greater than that associated with nadolol treatment.
Several placebo-controlled studies have shown topiramate to be effective for migraine prevention in individuals with episodic migraine or chronic migraine.110-114 The adverse events that occurred in at least 5% of patients receiving topiramate (50-200 mg/d) were largely mild or moderate and included paresthesia, fatigue, memory and concentration difficulties, mood problems, infection, and taste perversion.110-114 Topiramate is effective not only in preventing migraine attacks but also in reducing their freqency; such a reduction may be associated with improvements in the daily work, home, and social activities of migraineurs, as determined by an analysis of MSQ, SF-36, and productivity data from placebo-controlled trials.115-118 Diamond et al115 analyzed data from the 3 pivotal topiramate trials. Results of the pooled analysis indicated that topiramate (100 mg/d) was associated with significant improvement compared with placebo in all MSQ domains (role-restrictive, role-preventive, and emotional function).
A prospective analysis of data from the trial by Silberstein et al112 demonstrated that patients treated with topiramate had statistically significant improvements in MSQ role-restrictive domain scores compared with the placebo group (P=.035 for topiramate, 50 mg/d, and P≤.001 for topiramate, 100 and 200 mg/d). Topiramate-treated patients (100 mg/d) also had significantly improved role-preventive domain scores compared with the placebo group (P=.045). Greater improvements were also observed for the SF-36 role-physical and vitality domain scores in patients receiving topiramate compared with the placebo group, but the difference between the 2 groups was not statistically significant.116 In a similar analysis of data from the trial by Brandes et al,110 patients treated with topiramate (50-200 mg/d) had significantly greater improvement in MSQ role-restrictive (P=.02 for topiramate, 50 mg/d, and P<.001 for topiramate, 100 and 200 mg/d) and role-preventive (P=.007 for topiramate, 50 mg/d; P=.001 for topiramate, 100 mg/d; and P=.002 for topiramate, 200 mg/d) domain scores compared with individuals receiving placebo. Statistically greater improvement was also observed in SF-36 role-physical domain scores in the topiramate, 100 and 200 mg/d, groups (P=.02 vs placebo). The differences in the SF-36 vitality domain scores were not statistically significant between the topiramate-treated and placebo-treated groups, although greater improvements were observed in patients receiving topiramate.117
Dahlöf et al119 assessed the longitudinal effect of topiramate on daily activities and function in the 3 pivotal topiramate trials analyzed by Diamond et al.115 The investigators examined patients' MSQ and SF-36 scores at weeks 8, 16, and 26 of the double-blind phase of each trial, the time points at which the MSQ and SF-36 were given. Compared with the placebo group, patients treated with topiramate (100 mg/d) had significantly improved mean scores for all 3 domains of the MSQ and at all 3 time points (P<.001 for all except role-preventive [P=.024 at week 8]). In addition, topiramate-treated patients (100 mg/d) had significant improvements in 7 of the 8 subscores (not role-emotional) of the SF-36 at week 26 compared with patients receiving placebo. Specifically, topiramate treatment was associated with significant improvements in the physical component summary scores throughout the double-blind phase of the trial (P<.001) and in the mental component summary scores at week 26 (P=.043).
A multicenter, randomized, double-blind, placebo-controlled trial by Dodick et al120 studied the effect of topiramate, 100 mg/d, on migraine-related disability, emotional distress, daily activities, and global impression of change in individuals with chronic migraine. The percentage of patients whose MIDAS scores reflected a greater than 50% improvement in migraine-related disability from baseline was higher in the topiramate group than in the placebo group, but these differences were not statistically significant (P=.074). The MSQ scores (last item carried forward) were significantly improved in patients receiving 100 mg/d of topiramate compared with the placebo group at week 4 in all 3 domains (role-restrictive, role-preventive, and emotional function) and at weeks 8 and 16 in role-restrictive and emotional function (P<.05). The percentage of patients who reported improvement in the Subject's Global Impression of Change scale score was significantly higher in the topiramate treatment group than in the placebo treatment group (75% vs 61%, respectively; P=.025). Findings were similar for the Physician's Global Impression of Change scale scores (72% for topiramate vs 59% for placebo; P=.037).
Workplace productivity has been evaluated in a post hoc analysis of pooled data from 2 randomized, double-blind, placebo-controlled topiramate trials. Lofland et al118 found that the number of hours worked with migraine, the decreased effectiveness caused by migraine (presenteeism), and total lost productivity (absenteeism and presenteeism) were significantly reduced in the group of patients treated with topiramate (100 mg/d) compared with the placebo-treated group.
Nonpharmacological Interventions
Several nonpharmacological interventions have demonstrated empirical efficacy for headache management. As a result, they have become standard components of specialty headache centers and multidisciplinary pain management programs and are endorsed by the US Headache Consortium,121 which consists of several professional agencies, including the American Headache Society, the American Academy of Neurology, and the National Headache Foundation.122 Empirically validated effective nonpharmacological interventions may play an important role in both the acute and the preventive phases of the comprehensive headache management plan and may be offered individually or in conjunction with pharmacotherapy. These interventions offer the benefit of being cost-effective without the potential for drug interactions or adverse effects. Nonpharmacological treatments are useful for patients who need to avoid medication, such as women who are pregnant or trying to become pregnant.123 Also, non-pharmacological therapy may augment the effectiveness of other treatments or minimize the need for their use.124 Several factors, including obesity, depression, anxiety, and stressful life events, have been established as common comorbidities of migraine with bidirectional influences.125,126 Therefore, treating any of the conditions listed previously may also benefit migraine and vice versa.
Headache is a multifaceted disorder that can affect all aspects of patients' lives. Multidisciplinary treatment approaches are often the most effective for the management of headache.127-129 Multidisciplinary headache and pain programs typically involve a range of pain specialists, which may include physicians, nurses, psychiatrists, psychologists, physical therapists, occupational therapists, and social workers, among other health care professionals. For health care professionals who have no multidisciplinary staff, appropriate referrals may be necessary. For more information about finding specialists and making referrals, see the study by Buse and Andrasik.130
Nonpharmacological treatments of migraine include cognitive behavioral therapy, biobehavioral training (ie, biofeedback, relaxation training, and stress management), physical therapy, education, and lifestyle modification or healthy lifestyle training.131 Cognitive behavioral therapy is an empirically tested method that helps patients identify behaviors that may increase or maintain headaches (eg, triggers, stressors, unhealthy lifestyle or habits) and maladaptive or dysfunctional thoughts (ie, cognitions) regarding their headaches.132 Cognitive behavioral therapy can aid in headache management by making patients more aware of triggers, including the association between stress and headache, and identifying and challenging counterproductive or self-defeating beliefs and ideas. Cognitive behavioral therapy is also effective in managing depression, anxiety, panic disorder, obsessive-compulsive disorder, eating disorders, sleep disorders, and other common comorbidities in patients with headache. Patients should work with a licensed psychologist, psychiatrist, or social worker with experience in treating patients with headache or chronic medical conditions. More information about cognitive behavioral therapy can be found on the Association for Behavioral and Cognitive Therapies Web site (www.abct.org).
Biofeedback entails learning to increase awareness of involuntary physiologic functions and bring them under voluntary control, especially functions related to sympathetic arousal, including improving circulation (measured by increasing finger temperature) and reducing muscle tension.133,134 Members of the Association for Applied Psychophysiology and Biofeedback (www.aapb.org) are certified to conduct biofeedback training, but many qualified professionals practice biofeedback therapy without being certified or belonging to this organization. A list of practitioners can be found at the Web site of the Biofeedback Certification Institute of America (www.bcia.org/directory/membership.cfm). Alternatively, patients may work with a licensed psychologist, social worker, physical therapist, or occupational therapist with biofeedback expertise. A list of psychologists with their specialties and location may be obtained through the American Psychological Association.
Relaxation techniques are taught to help patients minimize their physiologic response to stress, decrease sympathetic arousal, and engage the parasympathetic nervous system. Relaxation training is typically conducted by psychologists or other mental health or allied pain professionals but can be self-taught by patients through training manuals or audio or visual relaxation aids. Relaxation training may include diaphragmatic breathing, visual imagery, meditation, prayer, yoga, self-hypnosis, guided relaxation CDs or audiocassettes, and other methods of calming the mind and body. These techniques require regular practice to become effective habitual responses.134,135
Patient education is important for effective headache management. Patients should be well informed about the identification and avoidance of triggers and how to make healthy lifestyle choices. In general, the best advice for migraineurs is to maintain a regular and healthy lifestyle, especially during times when they are most vulnerable to an attack. Healthy lifestyle habits include a regular sleep-wake schedule, regular meals, a diet that avoids processed and unhealthy food, regular exercise, avoidance of excessive caffeine or alcohol consumption, and smoking cessation. Regular practice of stress management and relaxation techniques and self-care should be encouraged. Migraine is also a unique condition in that patients make most of the therapeutic decisions on their own. After a physician prescribes the medication, the patient decides which attacks to treat, when to treat them, how to treat them, the level of adherence, whether to make healthy lifestyle changes, and many other decisions that are central to effective management. Trials of educational interventions have demonstrated significant reductions in pain frequency, intensity, and duration; improved functional status and quality of life; reduced depression; and decreased service utilization (in terms of patient visits to both primary care physicians and the emergency department).136
CONCLUSION
Migraine headache remains an underrecognized and undertreated neurologic disorder despite the availability of effective treatment and management options. Care improves when health care professionals and patients communicate effectively about the burden of migraine, as recommended in treatment guidelines. Health care professionals should routinely evaluate the impact of migraine pain and related disability and reduced HRQoL to determine whether patients are receiving effective treatment and whether additional treatment strategies are warranted. Health care professionals can facilitate effective communication by using techniques such as active listening, open-ended questions, and the “ask-tell-ask” strategy. In addition, a variety of assessment tools and techniques are available for determining the burden of migraine, HRQoL, and common comorbidities. MIDAS, HIT-6, and MIBS-4 are useful tools for gathering data and generating discussion about ictal and interictal disability, and PHQ-9 and Generalized Anxiety Disorder 7 can assist in assessing depression and anxiety, 2 common migraine comorbidities. The MPQ-5 can be helpful in identifying appropriate candidates for preventive treatments. A number of effective medications and empirically validated biobehavioral interventions are available for treating acute attacks, preventing future attacks, and improving the HRQoL of patients with migraine. Accurately evaluating individual patients' needs through the use of assessment tools and effective communication techniques will help create the optimal treatment strategy for each.
Acknowledgments
Editorial support was provided by Kakuri Omari, PhD (Phase Five Communications Inc, New York, NY), with funding from Ortho-McNeil Neurologics.
Footnotes
Dr Buse has received research grants and has been a consultant for Ortho-McNeil Neurologics, Endo Pharmaceuticals, Allergan, and Merck & Co. Dr Lipton has been an adviser, has been a member of the speaker's bureau, and has received research or education grants from Advanced Bionics, Allergan, AstraZeneca, Boehringer-Ingelheim, Bristol-Myers Squibb, Cierra, Endo Pharmaceuticals, GlaxoSmithKline, Minster Machine Co, Merck & Co, Neuralieve, Novartis, Ortho-McNeil Neurologics, Pfizer, Pozen, ProEthics, and St. Jude Medical. Dr Rupnow was an employee of Ortho-McNeil Janssen Scientific Affairs, LLC, a Johnson & Johnson company, at the time of manuscript development.
REFERENCES
- 1.World Health Organization http://www.who.int/whr/2001/en/index.html. The World Health Report 2001: Mental Health: New Understanding, New Hope. Accessed January 12, 2009.
- 2.Lipton RB. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 2001;41(7):646-657 [DOI] [PubMed] [Google Scholar]
- 3.Haut SR. Chronic disorders with episodic manifestations: focus on epilepsy and migraine. Lancet Neurol. 2006;5(2):148-157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bigal ME. When migraine progresses: transformed or chronic migraine. Expert Rev Neurother 2006;6(3):297-306 [DOI] [PubMed] [Google Scholar]
- 5.Leonardi M. The global burden of migraine: measuring disability in headache disorders with WHO's Classification of Functioning, Disability and Health (ICF). J Headache Pain 2005December;6(6):429-440 Epub 2005 Dec 15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clarke CE. Economic and social impact of migraine. QJM 1996;89(1):77-84 [DOI] [PubMed] [Google Scholar]
- 7.Dowson A. The UK Migraine Patient Survey: quality of life and treatment. Curr Med Res Opin 1999;15(4):241-253 [DOI] [PubMed] [Google Scholar]
- 8.Linde M. Attitudes and burden of disease among self-considered migraineurs: a nation-wide population-based survey in Sweden. Cephalalgia 2004;24(6):455-465 [DOI] [PubMed] [Google Scholar]
- 9.Dahlöf CG. Migraine patients experience poorer subjective well-being/quality of life even between attacks. Cephalalgia 1995;15(1):31-36 [DOI] [PubMed] [Google Scholar]
- 10.Dueland AN. The impact of migraine on psychological well-being of young women and their communication with physicians about migraine: a multinational study. Curr Med Res Opin 2005;21(8):1297-1305 [DOI] [PubMed] [Google Scholar]
- 11.New survey reveals worrying between attacks can extend suffering for migraineurs [press release] Titusville, NJ: Ortho-McNeil; June8, 2006. [Google Scholar]
- 12.Holmes WF. Information about migraine disability influences physicians' perceptions of illness severity and treatment needs. Headache 2001;41(4):343-350 [DOI] [PubMed] [Google Scholar]
- 13.Lipton RB, et al. In-office discussions of migraine: results from the American Migraine Communication Study. J Gen Intern Med. 2008August;23(8):1145-1151 Epub 2008 May 6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hahn SR. Healthcare provider-patient communication and migraine assessment: results of the American Migraine Communication Study (AMCS) Phase II. Curr Med Res Opin 2008June;24(6):1711-1718 Epub 2008 May 7 [DOI] [PubMed] [Google Scholar]
- 15.Brandes JL. Global trends in migraine care: results from the MAZE survey. CNS Drugs 2002;16(suppl 1):13-18 [DOI] [PubMed] [Google Scholar]
- 16.Stang PE. Impact of migraine in the United States: data from the National Health Interview Survey. Headache 1993;33(1):29-35 [DOI] [PubMed] [Google Scholar]
- 17.Stewart WF. Lost productive time and cost due to common pain conditions in the US workforce. JAMA 2003;290(18):2443-2454 [DOI] [PubMed] [Google Scholar]
- 18.Hawkins K. Indirect cost burden of migraine in the United States. J Occup Environ Med. 2007;49(4):368-374 [DOI] [PubMed] [Google Scholar]
- 19.Lipton RB. The family impact of migraine: population-based studies in the USA and UK. Cephalalgia 2003;23(6):429-440 [DOI] [PubMed] [Google Scholar]
- 20.Peters M. The patients' perceptions of migraine and chronic daily headache: a qualitative study. J Headache Pain 2005February;6(1):40-47 Epub 2005 Jan 25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peres MF, et al. Cephalalgiaphobia: a possible specific phobia of illness. J Headache Pain 2007February;8(1):56-59 Epub 2007 Feb 19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cupini LM. Medication-overuse headache: pathophysiological insights. J Headache Pain 2005;6(4):199-202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diener HC. Medication-overuse headache: a worldwide problem. Lancet Neurol. 2004;3(8):475-483 [DOI] [PubMed] [Google Scholar]
- 24.Silberstein SD, et al. International Headache Society The International Classification of Headache Disorders, 2nd Edition (ICHD-II): revision of criteria for 8.2 medication-overuse headache [published correction appears in Cephalalgia. 2006;26(3):360] Cephalalgia 2005;25(6):460-465 [DOI] [PubMed] [Google Scholar]
- 25.Stewart WF. Reliability of the migraine disability assessment score in a population-based sample of headache sufferers. Cephalalgia 1999;19(2):107-114 [DOI] [PubMed] [Google Scholar]
- 26.Ware JE., Jr Practical implications of item response theory and computerized adaptive testing: a brief summary of ongoing studies of widely used headache impact scales. Med Care 2000;38(9) (suppl):II73-II82 [PubMed] [Google Scholar]
- 27.Dowson AJ. Assessing the impact of migraine. Curr Med Res Opin 2001;17(4):298-309 [PubMed] [Google Scholar]
- 28.Lipton RB. Clinical trials of acute treatments for migraine including multiple attack studies of pain, disability, and health-related quality of life. Neurology 2005;65(12)(suppl 4):S50-S58 [DOI] [PubMed] [Google Scholar]
- 29. http://www.headachetest.com/HIT6/PDFS/English.pdf. Headache Impact Test-6 Web site. Accessed January 13, 2009.
- 30.Pryse-Phillips W. Evaluating migraine disability: the headache impact test instrument in context. Can J Neurol Sci. 2002;29(suppl 2):S11-S15 [DOI] [PubMed] [Google Scholar]
- 31.Jacobson GP. The Henry Ford Hospital Headache Disability Inventory (HDI). Neurology 1994;44(5):837-842 [DOI] [PubMed] [Google Scholar]
- 32.Stewart WF. Reliability of an illness severity measure for headache in a population sample of migraine sufferers. Cephalalgia 1998;18(1):44-51 [DOI] [PubMed] [Google Scholar]
- 33.Lipton RB. Clinical utility of an instrument assessing migraine disability: the Migraine Disability Assessment (MIDAS) questionnaire. Headache 2001;41(9):854-861 [PubMed] [Google Scholar]
- 34.World Health Organization International Classification of Functioning, Disability and Health. Agenda item 13.9, 54th World Health Assembly, 9th plenary meeting, May 22, 2001 http://www.who.int/classification/icf/site/whares/wha-en.pdf Accessed November 2007
- 35.Buse DC. Development and validation of the Migraine Interictal Burden Scale (MIBS): a self-administered instrument for measuring the burden of migraine between attacks [abstract S05.003]. Neurology 2007;68(suppl 1):A89 [Google Scholar]
- 36.Buse D, et al. The Migraine Interictal Burden Scale (MIBS): results of a population-based validation study [abstract F64]. Headache 2007;47(5):778 [Google Scholar]
- 37.Solomon GD. Quality of life and well-being of headache patients: measurement by the Medical Outcomes Study instrument. Headache 1993;33(7):351-358 [DOI] [PubMed] [Google Scholar]
- 38.Ware JE., Jr The MOS 36-Item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care 1992;30(6):473-483 [PubMed] [Google Scholar]
- 39.Osterhaus JT. Measuring the functional status and well-being of patients with migraine headache. Headache 1994;34(6):337-343 [DOI] [PubMed] [Google Scholar]
- 40.Bussone G. Disability and quality of life in different primary headaches: results from Italian studies. Neurol Sci. 2004;25(suppl 3):S105-S107 [DOI] [PubMed] [Google Scholar]
- 41.Martin BC, et al. Validity and reliability of the Migraine-Specific Quality of Life Questionnaire (MSQ Version 2.1). Headache 2000;40(3):204-215 [DOI] [PubMed] [Google Scholar]
- 42.Breslau N. Migraine, physical health and psychiatric disorder: a prospective epidemiologic study in young adults. J Psychiatr Res. 1993;27(2):211-221 [DOI] [PubMed] [Google Scholar]
- 43.Jette N. Comorbidity of migraine and psychiatric disorders: a national population-based study. Headache 2008April;48(4):501-516 Epub 2007 Dec 7 [DOI] [PubMed] [Google Scholar]
- 44.Lipton RB. Migraine headache disability and health-related quality-of-life: a population-based case-control study from England. Cephalalgia 2003;23(6):441-450 [DOI] [PubMed] [Google Scholar]
- 45.Dueland AN. The impact of migraine on work, family, and leisure among young women: a multinational study. Curr Med Res Opin 2004;20(10):1595-1604 [DOI] [PubMed] [Google Scholar]
- 46.Lantéri-Minet M. Anxiety and depression associated with migraine: influence on migraine subjects' disability and quality of life, and acute migraine management. Pain 2005December;118(3):319-326 Epub 2005 Nov 14 [DOI] [PubMed] [Google Scholar]
- 47.Ware J., Jr A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34(3):220-233 [DOI] [PubMed] [Google Scholar]
- 48.Headache Classification Subcommittee of the International Headache Society The International Classification of Headache Disorders, 2nd ed.Cephalagia 2004;24(suppl 1):1-160 [DOI] [PubMed] [Google Scholar]
- 49.Kroenke K. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Spitzer RL, Patient Health Questionnaire Primary Care Study Group Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA 1999;282(18):1737-1744 [DOI] [PubMed] [Google Scholar]
- 51.Lipton RB, et al. Validity and reliability of the Migraine Treatment Optimization Questionnaire (M-TOQ) in the treatment of migraine [abstract P06.033]. Neurology 2007;68(suppl 1):A263 [Google Scholar]
- 52.Lipton R, et al. Validity and reliability of the Migraine-Treatment Optimization Questionnaire. Cephalalgia 2009February23[Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 53.Stewart WF. Validation of the work and health interview. Pharmacoeconomics 2004;22(17):1127-1140 [DOI] [PubMed] [Google Scholar]
- 54.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders 4th ed. Text Rev. Washington, DC: American Psychiatric Press; 2000. [Google Scholar]
- 55.Simpson M, et al. Doctor-patient communication: the Toronto consensus statement. BMJ 1991;303(6814):1385-1387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lansky D. Measuring what matters to the public. Health Aff (Millwood) 1998;17(4):40-41 [DOI] [PubMed] [Google Scholar]
- 57.The Medical School Objectives Writing Group Learning objectives for medical student education: guidelines for medical schools: report I of the Medical School Objectives Project. Acad Med. 1999;74(1):13-18 [DOI] [PubMed] [Google Scholar]
- 58.Makoul G. Essential elements of communication in medical encounters: the Kalamazoo consensus statement. Acad Med. 2001;76(4):390-393 [DOI] [PubMed] [Google Scholar]
- 59.Hulsman RL. Teaching clinically experienced physicians communication skills: a review of evaluation studies. Med Educ. 1999;33(9):655-668 [DOI] [PubMed] [Google Scholar]
- 60.Hall JA. Satisfaction, gender, and communication in medical visits. Med Care 1994;32(12):1216-1231 [DOI] [PubMed] [Google Scholar]
- 61.Frederikson LG. Exploring information-exchange in consultation: the patients' view of performance and outcomes. Patient Educ Couns 1995;25(3):237-246 [DOI] [PubMed] [Google Scholar]
- 62.Hall JA. Meta-analysis of correlates of provider behavior in medical encounters. Med Care 1988;26(7):657-675 [DOI] [PubMed] [Google Scholar]
- 63.Cox K. A systematic review of two-way communication between patients and healthcare professionals about medicines. National Prescribing Centre Web site http://www.npc.co.uk/med_partnership/resource/major-reviews/systematic-review.html Published May 2004. Accessed January 13, 2009
- 64.Stewart M. The influence of older patient-physician communication on health and health-related outcomes. Clin Geriatr Med. 2000;16(1):25-36 [DOI] [PubMed] [Google Scholar]
- 65.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ 1995;152(9):1423-1433 [PMC free article] [PubMed] [Google Scholar]
- 66.Cole SA. Reducing malpractice risk through more effective communication. Am J Manag Care 1997;3(4):649-653 [PubMed] [Google Scholar]
- 67.Bensing JM. Communication patterns of primary care physicians in the United States and the Netherlands. J Gen Intern Med. 2003;18(5):335-342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Roter DL. Improving physicians' interviewing skills and reducing patients' emotional distress: a randomized clinical trial. Arch Intern Med. 1995;155(17):1877-1884 [PubMed] [Google Scholar]
- 69.Mueller PS, et al. Views of new internal medicine faculty of their preparedness and competence in physician-patient communication. BMC Med Educ. 2006;6(May 26):30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Davis D. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or healthcare outcomes? JAMA 1999;282(9):867-874 [DOI] [PubMed] [Google Scholar]
- 71.Fellowes D. Communication skills training for healthcare professionals working with cancer patients, their families and/or carers. Cochrane Database Syst Rev. 2004;2:CD003751 [DOI] [PubMed] [Google Scholar]
- 72.Roter DL, eds. Improving talk through interventions. In: Doctors Talking With Patients/Patients Talking With Doctors: Improving Communication in Medical Visits 2nd ed.Westport, CT: Praeger; 2006:163-181 [Google Scholar]
- 73.Back AL. Approaching difficult communication tasks in oncology. CA Cancer J Clin. 2005;55(3):164-177 [DOI] [PubMed] [Google Scholar]
- 74.Boyle D. Invite, listen, and summarize: a patient-centered communication technique. Acad Med. 2005;80(1):29-32 [DOI] [PubMed] [Google Scholar]
- 75.Martin LR. Physician facilitation of patient involvement in care: correspondence between patient and observer reports. Behav Med. 2003;28(4):159-164 [DOI] [PubMed] [Google Scholar]
- 76.Abdel-Tawab N. The relevance of client-centered communication to family planning settings in developing countries: lessons from the Egyptian experience. Soc Sci Med. 2002;54(9):1357-1368 [DOI] [PubMed] [Google Scholar]
- 77.Ishikawa H. Physician-patient communication and patient satisfaction in Japanese cancer consultations. Soc Sci Med. 2002;55(2):301-311 [DOI] [PubMed] [Google Scholar]
- 78.Roter DL, et al. Use of an innovative video feedback technique to enhance communication skills training [published correction appears in Med Educ. 2005;39(6):645] Med Educ. 2004;38(2):145-157 [DOI] [PubMed] [Google Scholar]
- 79.Hahn SR. Communication in the care of the headache patient. In: Silberstein SD, eds. Wolff's Headache and Other Head Pain 8th ed.New York, NY: Oxford University Press; 2008:805-824 [Google Scholar]
- 80.Lake AE., III Headache and psychiatric comorbidity: historical context, clinical implications, and research relevance. Headache 2005;45(5):493-506 [DOI] [PubMed] [Google Scholar]
- 81.McWilliams LA. Depression and anxiety associated with three pain conditions: results from a nationally representative sample. Pain 2004;111(1-2):77-83 [DOI] [PubMed] [Google Scholar]
- 82.DiMatteo MR. Relationship of physicians' non-verbal communication skill to patient satisfaction, appointment noncompliance, and physician workload. Health Psychol. 1986;5(6):581-594 [DOI] [PubMed] [Google Scholar]
- 83.Buller MK. Physicians' communication style and patient satisfaction. J Health Soc Behav. 1987;28(4):375-388 [PubMed] [Google Scholar]
- 84.Kroenke K. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care 2003;41(11):1284-1292 [DOI] [PubMed] [Google Scholar]
- 85.Spitzer RL. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-1097 [DOI] [PubMed] [Google Scholar]
- 86.Lipton RB. The role of headache-related disability in migraine management: implications for headache treatment guidelines. Neurology 2001;56(6, suppl 1):S35-S42 [DOI] [PubMed] [Google Scholar]
- 87.Buse DC. Facilitating communication with patients for improved migraine outcomes. Curr Pain Headache Rep. 2008;12(3):230-236 [DOI] [PubMed] [Google Scholar]
- 88.Rains JC. Behavioral facilitation of medical treatment for headache, Part II: theoretical models and behavioral strategies for improving adherence. Headache 2006;46(9):1395-1403 [DOI] [PubMed] [Google Scholar]
- 89.Miller WR. Motivational Interviewing: Preparing People for Change 2nd ed.New York, NY: Guilford Press; 2002. [Google Scholar]
- 90.Silberstein SD, US Headache Consortium Practice parameter: evidence-based guidelines for migraine headache (an evidence based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000;55:754-762 http://www.neurology.org/cgi/reprint/55/6/754.pdf Accessed January 13, 2009 [DOI] [PubMed] [Google Scholar]
- 91.Dowson AJ, MIPCA Migraine Guidelines Development Group. Migraine In Primary Care Advisors New guidelines for the management of migraine in primary care. Curr Med Res Opin 2002;18(7):414-439 [DOI] [PubMed] [Google Scholar]
- 92.Goadsby PJ. Migraine: current understanding and treatment. N Engl J Med. 2002;346(4):257-270 [DOI] [PubMed] [Google Scholar]
- 93.Bigal ME. Acute treatment of migraine headache. Curr Treat Options Neurol. 2003;5(6):423-430 [DOI] [PubMed] [Google Scholar]
- 94.Bigal ME. The preventive treatment of migraine. Neurologist 2006;12(4):204-213 [DOI] [PubMed] [Google Scholar]
- 95.Kaniecki R. Neuromodulators for migraine prevention. Headache 2008April;48(4):586-600 Epub 2008 Jan 18 [DOI] [PubMed] [Google Scholar]
- 96.Lipton RB. Disability assessment as a basis for stratified care. Cephalalgia 1998;18(suppl 22):40-43 [DOI] [PubMed] [Google Scholar]
- 97.Lake AE., III Medication overuse headache: biobehavioral issues and solutions. Headache 2006;46(suppl 3):S88-S97 [DOI] [PubMed] [Google Scholar]
- 98.Ramadan NM, US Headache Consortium http://www.aan.com/professionals/practice/pdfs/gl0090.pdf. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management for prevention of migraine. Accessed January 13, 2009.
- 99.Ramadan NM. Migraine headache prophylaxis: current options and advances on the horizon. Curr Neurol Neurosci Rep. 2006;6(2):95-99 [DOI] [PubMed] [Google Scholar]
- 100.Lipton RB, American Migraine Prevalence and Prevention (AMPP) Advisory Group Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 2007;68(5):343-349 [DOI] [PubMed] [Google Scholar]
- 101.Lipton R. The Migraine Prevention Questionnaire (MPQ): development and validation [abstract F48]. Headache 2007;47(5):770-771 [Google Scholar]
- 102.Blocadren (timolol meleate) [package insert] Whitehouse Station, NJ: Merck & Co; 2002. [Google Scholar]
- 103.Depakote ER (divalproex sodium extended-release) [package insert] North Chicago, IL: Abbot Laboratories; 2006. [Google Scholar]
- 104.Topamax (topiramate) [package insert] Raritan, NJ: Ortho-McNeil Pharmaceutical; 2004. [Google Scholar]
- 105.Inderal LA (propranolol hydrocholoride) long-acting Capsules. [package insert] Philadelphia, PA: Wyeth Pharmaceuticals; 2007. [Google Scholar]
- 106.Snow V, American Academy of Family Physicians. American College of Physicians-American Society of Internal Medicine Pharmacologic management of acute attacks of migraine and prevention of migraine headache. Ann Intern Med. 2002;137(10):840-849 [DOI] [PubMed] [Google Scholar]
- 107.Modi S. Medications for migraine prophylaxis [published correction appears in Am Fam Physician. 2006;74(10):1685] Am Fam Physician 2006;73(1):72-78 [PubMed] [Google Scholar]
- 108.Mendizabal JE. Extended-release divalproex sodium improves the quality of life of adolescent migraineurs [letter]. Headache 2002;42(4):327-328 [DOI] [PubMed] [Google Scholar]
- 109.Garcia-Monco JC. Impact of preventive therapy with nadolol and topiramate on the quality of life of migraine patients. Cephalalgia 2007August;27(8):920-928 Epub 2007 Jul 23 [DOI] [PubMed] [Google Scholar]
- 110.Brandes JL, et al. Topiramate for migraine prevention: a randomized controlled trial. JAMA 2004;291(8):965-973 [DOI] [PubMed] [Google Scholar]
- 111.Diener HC, et al. MIGR-003 Study Group Topiramate in migraine prophylaxis: results from a placebo-controlled trial with propranolol as an active control. J Neurol. 2004;251(8):943-950 [DOI] [PubMed] [Google Scholar]
- 112.Silberstein SD, MIGR-001 Study Group Topiramate in migraine prevention: results of a large controlled trial. Arch Neurol. 2004;61(4):490-495 [DOI] [PubMed] [Google Scholar]
- 113.Diener HC, TOPMAT-MIG-201(TOP-CHROME) Study Group Topiramate reduces headache days in chronic migraine: a randomized, double-blind, placebo-controlled study [published correction appears in Cephalalgia. 2007;27(8):962] Cephalalgia 2007. Jul;27(7):814-823 Epub 2007 Apr 18 [DOI] [PubMed] [Google Scholar]
- 114.Silberstein SD, et al. Topiramate Chronic Migraine Study Group Efficacy and safety of topiramate for the treatment of chronic migraine: a randomized, double-blind, placebo-controlled trial. Headache 2007;47(2):170-180 [DOI] [PubMed] [Google Scholar]
- 115.Diamond M. Topiramate improves health-related quality of life when used to prevent migraine. Headache 2005:45(8):1023-1030 [DOI] [PubMed] [Google Scholar]
- 116.Silberstein SD. The impact of migraine on daily activities: effect of topiramate compared with placebo. Curr Med Res Opin 2006;22(6):1021-1029 [DOI] [PubMed] [Google Scholar]
- 117.Brandes JL. Assessing the ability of topiramate to improve the daily activities of patients with migraine. Mayo Clin Proc. 2006;81(10):1311-1319 [DOI] [PubMed] [Google Scholar]
- 118.Lofland JH. Impact of topiramate migraine prophylaxis on workplace productivity: results from two US randomized, double-blind, placebo-controlled, multicenter trials. J Occup Environ Med. 2007:49(3):252-257 [DOI] [PubMed] [Google Scholar]
- 119.Dahlöf C. The impact of migraine prevention on daily activities: a longitudinal and responder analysis from three topiramate placebo-controlled clinical trials. Health Qual Life Outcomes 2007;5(Oct 4):56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Dodick DW, et al. The impact of topiramate on health-related quality of life indicators in chronic migraine. Headache 2007;47(10):1398-1408 [DOI] [PubMed] [Google Scholar]
- 121.Campbell JK, US Headache Consortium Evidence-based guidelines for migraine headache: behavioral and physical treatments. American Academy of Neurology 2000:1-29 http://www.aan.com/professionals/practice/pdfs/gl0089.pdf Accessed January 13, 2009 [Google Scholar]
- 122.Goslin RE, et al. http://www.clinpol.mc.duke.edu. Behavioral and physical treatments for migraine headache. Technical review 2.2 February 1999. Prepared for the Agency for Healthcare Policy and Research under Contract No. 290-94-2025. Accessed November 2007. [PubMed]
- 123.Scharff L. Maintenance of effects in the nonmedical treatment of headaches during pregnancy. Headache 1996;36(5):285-290 [DOI] [PubMed] [Google Scholar]
- 124.Penzien DB. Behavioral management of recurrent headache: three decades of experience and empiricism. Applied Psychophysiol Biofeedback 2002;27(2):163-181 [DOI] [PubMed] [Google Scholar]
- 125.Bigal ME. Modifiable risk factors for migraine progression. Headache 2006;46(9):1334-1343 [DOI] [PubMed] [Google Scholar]
- 126.Scher AI. Risk factors for headache chronification. Headache 2008;48(1):16-25 [DOI] [PubMed] [Google Scholar]
- 127.Lemstra M. Effectiveness of multidisciplinary intervention in the treatment of migraine: a randomized clinical trial. Headache 2002;42:845-854 [DOI] [PubMed] [Google Scholar]
- 128.Harpole LH. Headache management program improves outcome for chronic headache. Headache 2003;43(7):715-724 [DOI] [PubMed] [Google Scholar]
- 129.Blumenfeld A. Center of excellence for headache care: group model at Kaiser Permanente. Headache 2003;43(5):431-440 [DOI] [PubMed] [Google Scholar]
- 130.Buse DC. Behavioral medicine for migraine. Neurol Clin. 2009;27(2):445-465 [DOI] [PubMed] [Google Scholar]
- 131.Rains JC. Behavioral headache treatment: history, review of the empirical literature, and methodological critique. Headache 2005;45(suppl 2):S92-S109 [DOI] [PubMed] [Google Scholar]
- 132.Beck AT, eds. Cognitive techniques: In Cognitive Therapy of Depression New York, NY: Guilford Press; 1979:142-166 [Google Scholar]
- 133.Schwartz MS, eds. Biofeedback: A Practitioner's Guide 3rd ed.New York, NY: Guilford Press; 2003. [Google Scholar]
- 134.Penzien DB. Psychosocial interventions in the management of recurrent headache disorders, II: description of treatment techniques. Behav Med. 1994;20(2):64-73 [DOI] [PubMed] [Google Scholar]
- 135.Hammond DC, ed. Handbook of Hypnotic Suggestions and Metaphors New York, NY: Norton and Company; 1990. [Google Scholar]
- 136.Rothrock JF. The impact of intensive patient education on clinical outcome in a clinic-based migraine population [published correction appears in Headache. 2006;46(7): 1227] Headache 2006;46(5):726-731 [DOI] [PubMed] [Google Scholar]