Abstract
Evidence suggests that migraine is associated with decreased productivity. This article describes the results of a systematic literature review of peer-reviewed publications that measured the impact of migraine on workplace productivity in the United States and provides recommendations for future research. A MEDLINE search was conducted from January 1, 1990 to July 31, 2008. Articles were included if the results were from a prospective or retrospective study that reported work-specific productivity outcomes in adults with migraine in the United States. Twenty-six studies were included. Nine studies found that diagnosed and/or undiagnosed migraine had a negative impact on worker productivity. Although one migraine prophylactic study found a statistically significant improvement in worker productivity for topiramate-treated patients, another found an insignificant difference in lisinopril-treated patients. Fifteen studies compared the impact of triptan therapy with a control group. The control groups in these studies differed with regard to recall periods, time to follow-up, and types of questionnaires used. Almost all studies found that triptan therapy was associated with a statistically significant improvement in loss in worker productivity vs the control group. Health care professionals can reduce the impact of migraine on worker productivity with appropriate therapy. Researchers should collect presenteeism and absenteeism data, report results in units of time, use a validated instrument, carefully consider recall periods, and report worker productivity separately. In addition, patients with undiagnosed migraine should be included in disease burden studies. When evaluating effects of treatment on productivity, researchers should target well-controlled, double-blind studies and conduct productivity research for new treatments.
HPQ = Health and Work Performance Questionnaire; IHS = International Headache Society; MWPLQ = Migraine Work and Productivity Loss Questionnaire; WHQ = Work and Health Questionnaire; WPSI = Work Productivity Short Inventory
Migraine is a chronic condition characterized by episodic attacks of disabling headaches. These attacks often present with any combination of pain, nausea, light and sound sensitivity, or vomiting. In the United States, approximately 18% of women and 6% of men experience at least 1 migraine headache per year.1 The total costs of disability attributable to these migraines were estimated to exceed $13 billion a year in the United States in 1998.2,3 In addition, a more recent study found that the total cost of lost productive time due to any type of headache pain was $19.6 billion (in 2002 US dollars).4
The prevalence of migraine peaks between the ages of 25 and 55 years, the ages when most individuals with migraine are most likely to be employed.5,6 Since the prevalence of migraine is higher in women, the impact of migraine on the labor force will increase during the upcoming years because more women are entering the workforce. In 2007, women comprised 46% of the total US labor force, and this percentage is expected to increase in the future.7
On an individual level, the disabling impact of migraine may affect a migraineur in numerous ways, including educational and employment choices.8 Migraine has serious deleterious effects on patient quality of life even when patients are not experiencing an attack.9 This is often termed interictal burden.
Evidence suggests that, despite the debilitating effects of migraine, the condition is underdiagnosed and undertreated. The American Migraine Study II found that approximately half of migraineurs are undiagnosed.10 The Landmark Study found that a quarter of individuals whose headache diary accounts met International Headache Society (IHS) criteria11 for migraine were not diagnosed as having migraine when they consulted a physician about headaches.12
For editorial comment, see page 397
This article summarizes the results of a systematic review of the literature on the impact of migraine and migraine treatment on productivity in the workplace in the United States. Research in this review included prospective or retrospective studies of experimental and observational design.
METHODS
A search of MEDLINE (January 1, 1990 to July 31, 2008) was conducted to identify articles that assessed the impact of migraine on work productivity in the United States. The following keywords were combined to identify appropriate citations: migraine disorders OR migrain$ AND absenteeism, productivity, presenteeism, task performance and analysis, sick leave, efficiency, workplace, occupational health, employment, efficiency, organizational, disability, work, economics, cost and cost analysis, cost$, or quality of life. The terms migraine disorders, absenteeism, task performance and analysis, sick leave, efficiency, workplace, occupational health, employment, organizational, and cost and cost analysis were searched as both medical subject headings and keywords. In MEDLINE, a $ within a search term includes any set of letters in place of the $. For example, a keyword search for migrain$ would include all articles with the words migraine, migraines, and migraineurs in the title or abstract.
This review focuses on migraineurs' loss in worker productivity in the United States; therefore, studies were excluded if they did not report the results of worker productivity separately from other types of activities, such as school or leisure; if the article had not been published in the English language; if the focus was animal research; if the results were not reported separately for US participants; if the results were calculated from a model; if the population included individuals 18 years or younger; or if the results were not reported separately for patients with migraine vs other types of headache. Both retrospective and prospective studies were included.
RESULTS
More than 1600 titles and abstracts were reviewed. Twenty-six studies published in 24 manuscripts met all inclusion criteria.5,13-35 Studies were grouped by the type of results reported, including burden of migraine, effect of prophylaxis, placebo-controlled studies of the effect of episodic migraine treatment, and pretest and posttest studies of episodic migraine treatment. Pretest and posttest studies were further divided into those with time-based recall periods and those measuring the impact of a single attack.
Burden of Migraine on US Worker Productivity
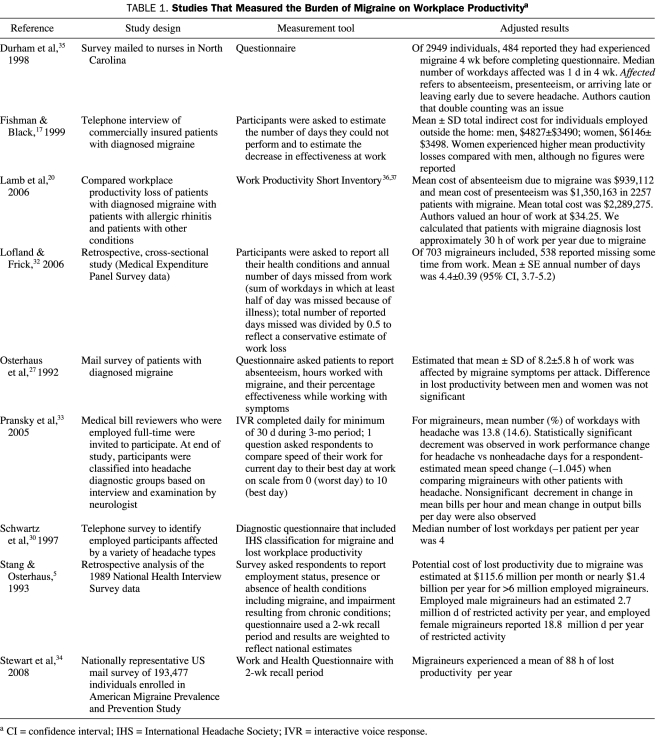
Nine articles estimated the burden of migraine on worker productivity (Table 1).5,17,20,27,30,32-35 In these articles, individuals were asked to estimate the impact of migraine on their work productivity. In 6 of the 9 studies on burden of migraine, all participants had a diagnosis of migraine.5,17,27,32,34,35 Durham et al35 limited migraineurs to those who experienced a migraine within 4 weeks of completing the survey.
TABLE 1.
Studies That Measured the Burden of Migraine on Workplace Productivitya
Three of the 9 studies on burden of migraine included individuals with diagnosed and undiagnosed migraine.20,30,33 In 2 of these 3 studies, individuals with undiagnosed migraine were identified by questions about their headache symptoms, and the responses were compared with IHS diagnostic criteria from 198811 to establish a migraine diagnosis.30,33 Lamb et al20 used the Work Productivity Short Inventory (WPSI),36 a generic productivity questionnaire, to compare the productivity impact of a variety of conditions, including migraine, with the productivity impact of allergic rhinitis. The third study collected data from respondents with headaches, and participants were diagnosed as having migraine or other types of headache by a neurologist when the study was complete.33
Four of the 9 studies on burden of migraine reported the mean cost of lost workplace productivity.5,17,20,35 Stang and Osterhaus5 calculated a national estimate of the cost and number of days of restricted activity due to migraine. Other studies estimated the mean number of hours of work lost per attack (8.2 hours),27 the mean number of hours lost per year (88 hours),34 the mean number of days of work lost per year (4.4 days),32 and the median number of days of work lost per year (4 days).30 Pransky et al33 administered daily surveys with a telephone interactive voice response system and found that 14.6% of workdays for migraineurs were affected by a headache.
Effect of Migraine Prophylaxis on US Worker Productivity
Two studies evaluated the impact of migraine prophylaxis on worker productivity. Lofland et al24 found that the total rate of lost productivity per migraineur was 3.1 hours per month in the topiramate prophylaxis plus episodic treatment group compared with 4.0 hours for placebo plus episodic treatment (P=.002). Schrader et al28 found no statistically significant difference in days of work lost between prophylaxis with lisinopril and placebo (2.30 days per 12 weeks vs 2.09 days per 12 weeks) in a crossover study that enrolled 60 patients. However, lisinopril was associated with a reduction in the number of days with migraine.28
Placebo-Controlled Randomized Studies Evaluating the Effect of Migraine Treatment on US Worker Productivity
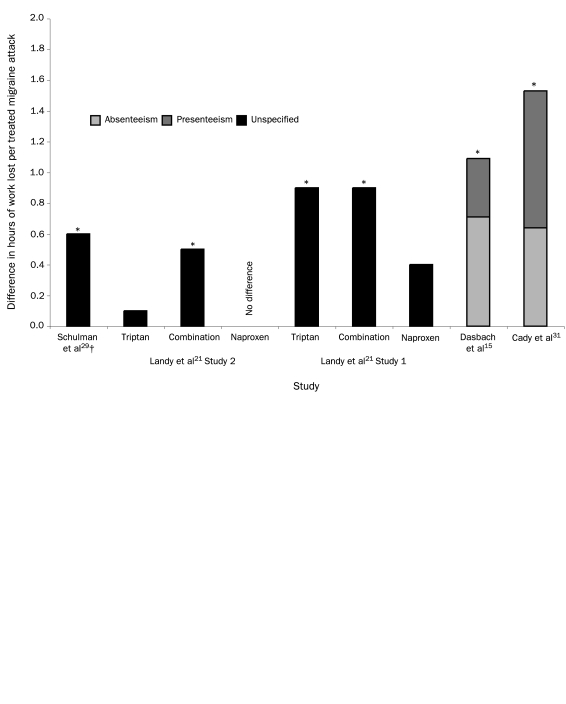
Five studies, reported in 4 publications, compared episodic migraine treatment with placebo in randomized controlled trials and used a recall period that included only 1 work shift.15,21,29,31 The methods used to estimate lost worker productivity appeared to be similar across these 5 studies. The presenteeism and absenteeism results in hours lost per work shift or workday for these studies are summarized in Figure 1. The mean difference in hours of work lost per treated migraineur ranged from no difference to approximately 1.6 hours per migraine attack. For studies that reported mean productivity loss by absenteeism and presenteeism, Figure 1 represents the difference between the sums of the means. Schulman et al29 reported the median productivity loss, whereas the other publications reported the mean productivity loss. The differences between the median productivity losses for the placebo and triptan groups were significantly lower, but the absolute value for the median productivity loss was lower than the absolute value of the mean productivity losses reported by the other studies. This finding suggests that the mean values for productivity loss may be affected by outlier individuals who are reporting high levels of productivity loss.
FIGURE 1.
Mean productivity losses reported in placebo-controlled randomized trials for a single attack or 24-hour period. Asterisk indicates that total productivity loss for treatment is statistically significantly lower than the total productivity loss for placebo (P<.05). Dagger indicates median productivity.
Pretest and Posttest Studies Evaluating the Effect of Treatment on US Worker Productivity
Nine articles reported the results of single-group, pretest and posttest studies.13,14,16,18,19,22,23,25,26 Individuals who initiated triptan therapy were asked to report the impact of migraine on work productivity while treating headaches with usual therapy (pretest) and after initiating triptan therapy (posttest). However, usual therapy was not defined by the study protocol. In each of the studies, usual therapy could include a variety of medications, such as narcotics, barbiturates, nonsteroidal anti-inflammatory drugs, acetaminophen, β-blockers, or any combination thereof. In one example, Adelman et al13 excluded individuals taking monoamine oxidase inhibitors and sumatriptan from their study. In another example, Davies et al16 did not exclude patients taking sumatriptan when defining the usual therapy group for the study that also served as a validation study for the Migraine Work and Productivity Loss Questionnaire (MWPLQ), a migraine-specific productivity questionnaire.
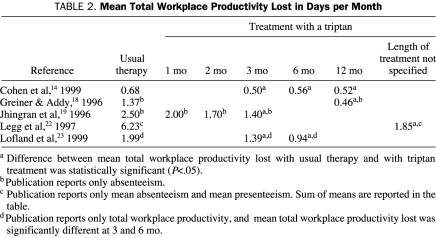
Table 2 summarizes the results from pretest and posttest studies of migraineurs that asked individuals to consider a defined recall period based on time rather than a single migraine attack. A recall period reflects the duration that individuals were instructed to consider when estimating productivity loss. In Table 2 results are reported in days per month of lost work productivity (eg, results reported in days lost per 3 months were divided by 3 by the authors of the current review to reflect days per month). Five of the 8 pretest and posttest studies evaluated migraine with a recall period ranging from 1 month to 12 months.14,18,19,22,23 Workplace productivity data were collected from 1 to 12 months after initiation of triptan therapy. Legg et al22 included all migraineurs who received at least 1 dose of sumatriptan in the treatment results. For all studies that evaluated the effect of a triptan on lost workdays after 3 months or more of therapy, the amount of time lost from work related to migraine headache was less than for usual therapy. However, the recall period for all articles in this set of studies varied. Jhingran et al19 used a 4-week recall. Lofland et al23 and Cohen et al14 used a 3-month recall. Greiner and Addy18 asked patients to report the number of workdays missed “this year before and after sumatriptan.” Some individuals thought the question referred to the calendar year, whereas others thought it referred to the 12-month periods before and after sumatriptan therapy.
TABLE 2.
Mean Total Workplace Productivity Lost in Days per Month
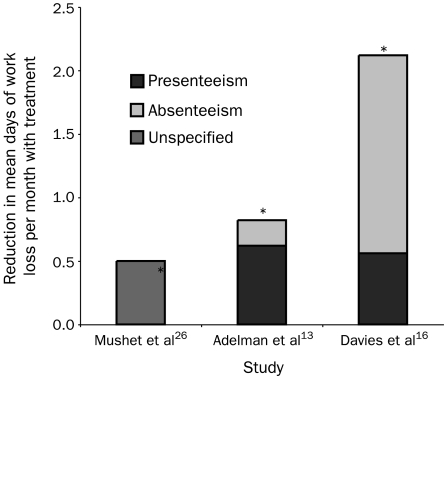
Three pretest and posttest studies reported results for a single migraine attack or 24-hour period (Figure 2). These studies found that triptan therapy was associated with a decreased productivity loss from a half day to more than 2 days per month compared with usual therapy.13,16,26
FIGURE 2.
Mean productivity loss reported by pretest and posttest design studies for a single attack. Asterisk indicates that mean total productivity loss for treatment is statistically significantly lower than the mean total productivity loss for placebo (P<.05).
Miller et al25 used data from 2 different pretest and posttest studies (including the study published by Mushet et al26) and reported the results of a time-series analysis. The authors found that sumatriptan therapy was associated with a 0.5-hour per week improvement in lost productivity due to absenteeism and a 0.3-hour per week improvement in lost productivity due to presenteeism.
Of the 13 publications that described 15 migraine treatment studies (randomized, placebo-controlled, and pretest and posttest) that reported the effect of migraine treatment on work productivity, most studies specifically instructed individuals to treat migraine headaches that were at least moderate to severe in pain level.15,16,18,19,21,25,26,29,31 Four studies allowed patients to treat migraine when pain was at any severity level from mild, moderate, or severe.13,14,22,23 None of the studies that met our inclusion criteria for the current literature review compared productivity loss in migraineurs who were instructed to treat migraine headaches limited to mild pain.
Across all studies, those that included the impact of migraine on presenteeism used the following calculation: Time Missed From Work Because of Symptoms of Migraine + (Time Worked With Symptoms [100 - Percentage of Effectiveness With Migraine Symptoms/100%]). This is sometimes referred to as the human capital method of estimating productivity.27,38,39 The estimates for percentage of effectiveness while working with migraine symptoms were self-reported by study participants. Not all studies reported the results of the mean percentage effectiveness for each treatment group. The estimates for percentage effectiveness while working with migraine symptoms ranged from 42%22 to 80%.13 Participants in the study by Mushet et al26 reported that they were 69% as effective at work with both usual therapy and triptan therapy. However, participants in the study by Legg et al22 reported that they were 42% as effective at work while taking usual therapy and 78% as effective when taking a triptan.
DISCUSSION
Studies have shown that migraineurs experience lower quality of life than the general population40-42 and that attack frequency is inversely related to quality-of-life scores.42 Studies have also shown that effective treatment of migraine has a positive impact on health-related quality of life.13,14,19,23,26 Other studies have described the cost-effectiveness of migraine treatment.43,44 Several of the publications that met the inclusion criteria for this review of workplace productivity also described results from quality-of-life questionnaires.13,14,18,19,21,23,26,28,35 The current study focuses on the impact of migraine and migraine treatment on worker productivity, a topic of interest to employers, health care decision makers, physicians, and patients. Worker productivity is 1 component of the overall impact of migraine.
Our literature review confirms that migraine has a negative impact on worker productivity and that effective therapy can reduce loss in worker productivity. Estimates of the burden of migraine suggest that the average impact of migraine on loss in worker productivity is approximately 4 workdays per year. With 1 exception, all published studies that compared episodic treatment with triptans and placebo or usual therapy found a significant reduction in the hours or days of work lost in patients treated with triptans. We identified 2 studies on prophylactic therapy and worker productivity in migraineurs. Prophylactic therapy with topiramate was shown to improve worker productivity in migraineurs compared with episodic treatment alone. Lisinopril was shown to reduce the number of days with migraine but had no significant impact on days of sick leave.28 In a clinical update of that study published in a different journal, the author suggests that the small sample size (60 patients at enrollment) may have contributed to the insignificant finding for loss in worker productivity.45
The studies designed to evaluate the effect of episodic treatment of migraine headache identified in this literature review used a variety of methods to measure on-the-job productivity loss. Some studies of medication treatment efficacy were randomized, placebo-controlled trials, whereas other studies used a pretest and posttest design. Usual therapy served as a comparator for the treatment groups but was rarely defined in the study methods. For the treatment intervention groups, time undergoing therapy before measuring workplace productivity ranged from duration of a single migraine attack to a recall period of 12 months in which migraine affected on-the-job productivity. Data on the impact of migraine on loss in worker productivity were collected in a variety of ways, including validated questionnaires, diary cards, or telephone interviews. Studies used various recall periods for measuring worker productivity, including hourly measures during each attack to 1-year recall periods. Worker productivity was frequently a secondary end point, and therefore studies probably were not powered to detect statistical significance with regard to the impact of medication therapy on worker productivity. Worker productivity was generally improved in migraineurs treated with medication therapy.
None of the studies that met our inclusion criteria evaluated the effect on productivity of some important new developments in migraine treatment. For example, none of the studies evaluated the impact of occipital nerve stimulation on migraine-related workplace productivity. Occipital nerve stimulation is currently considered an experimental treatment for intractable migraine.46
One of the goals of the current article was to review studies of the effect of migraine medication treatment on US workers. Our search method was designed to identify a subset of publications with a focus on the US workforce with migraine and was not intended to provide a comprehensive view of the impact of headache treatment on productivity.
We excluded studies that reported the impact of migraine on time lost at school and/or lost leisure time if loss in work productivity was not reported separately.47-50 Von Korff et al49 described the results of a population-based, daily diary study that followed up individuals with diagnosed and undiagnosed headaches, including migraine, for 3 months. All study participants were employed for at least 3 days per week and were asked to consider the impact of headaches on work or school when evaluating lost workdays. The authors found that the most severely affected migraineurs experienced the greatest reduction in work productivity. Our search criteria included studies that reported results for patients with a diagnosis of migraine and/or patients whose description of their symptoms met criteria for migraine separately from results of patients with other headache types. Some studies collected data from patients with migraine but reported their results with those from other patients with headache.51,52 Our search was limited to studies that reported the results of US patients separately to limit the impact of inherent differences in health care systems and sick-leave policies. Studies that reported the results of modeling exercises were also excluded because the data used to populate models were likely to be obtained from original research that was included in this review.2,38,43,44,53 For example, Halpern et al44 developed a disease model and used the results of the study by Adelman et al13 to estimate the impact on worker productivity. Similarly, studies that reported reevaluations of previously published data were also excluded. For example, data from Lofland et al23 were reanalyzed by Lofland et al38 in 2001 to compare different mathematical methods for calculating lost productivity. For our review, only the initial study by Lofland et al23 was included. Similarly, Hu et al2 used results of the study by Dasbach et al15 to estimate the overall burden of illness from migraine.
Measuring loss in worker productivity is an increasingly important component of health care research. Recently, the American College of Occupational and Environmental Medicine assembled an expert panel through the Occupational and Environmental Health Foundation to review available instruments for measuring loss in worker productivity in migraineurs. The group identified 4 key characteristics for health-related productivity instruments: (1) supporting scientific evidence, such as reliability and validity; (2) applicability across industries and occupations, disease states, and conditions; (3) ability to support business decision making (ie, calculation of results to monetary unit); and (4) practicality in terms of low cost, self-administration, being easy, and being available in multiple languages.54
The panel suggested that in addition to retrospective assessments of impairment, researchers should use daily employee diaries to supplement their findings. The panel suggested that self-report measures be cross-validated with other workplace assessments. Although this adds a level of complexity to studies, the panel believed that the additional information would be helpful when the goal of the study is to evaluate an intervention.54 The panel concluded that research should focus on basic metrics that can be used as national benchmarks for assessing the quantification of the fiscal impact of health on the corporate bottom line.55
The economic burden of migraine on an employer can be estimated and appropriate interventions offered to employees to address the losses in worker productivity.56 Lipton et al57 recommend that employers take actions to manage migraine in the workplace, including supporting internal health economic research and implementing screening of employees for migraine. Incorporating employee questionnaires for screening, estimating baseline burden of illness, offering appropriate migraine education and conditional management interventions, and measuring program effectiveness are important components of a migraine disease management program for employees.
Because migraine is a chronic and episodic condition, measuring the impact of migraine on worker productivity presents unique opportunities and challenges when compared with other conditions. For example, the impact of allergic rhinitis should be measured during the allergy season.58 However, the impact of depression on work productivity is likely to be more consistent throughout the year.59 In contrast, the impact of migraine on worker productivity should be evaluated for a single episode of migraine or during a period in which migraine headaches are relatively common. The challenge when measuring the impact of migraine by episode is to collect the data at the appropriate time with an appropriate recall period that captures the entire attack. Measuring the impact of migraine over time allows for the inclusion of the interictal burden of migraine, but determination of the appropriate frequency to collect data presents a challenge.
RECOMMENDATIONS FOR RESEARCHERS
The following are 9 recommendations for future research studies with the objective of measuring the burden of migraine and/or the impact of interventions on worker productivity.
First, estimates of the impact of migraine on worker productivity for a population should include a method for identifying individuals with undiagnosed migraine. Studies have estimated that approximately one-quarter of migraineurs have not had their condition diagnosed.1,12 One method for identifying individuals with undiagnosed migraine in a population survey is to include IHS criteria questions for migraines.30 If patients have headaches that meet these criteria, their productivity data could be included in the overall estimate of the impact of migraine on a workforce.
Second, both presenteeism and absenteeism data should be collected and reported separately. Most of the articles identified in this review acknowledge that estimating only absenteeism does not capture the complete burden of migraine on workers or employers. Patients in the studies identified in this review reported a wide range of percentages of effectiveness while working with symptoms. Despite this inconsistency, collecting data on presenteeism is necessary for a complete estimate of the impact of migraine on worker productivity.
Third, studies of worker productivity should report units of time and cost separately. If the cost of productivity loss is reported without a corresponding estimate of time lost from work, future comparisons will need to be adjusted for inflation.
Fourth, researchers should choose well-validated instruments for estimating the productivity loss associated with migraine and other health conditions.54 Properly designed studies will provide additional validation data for the instruments and results that can be compared across studies. Validated instruments used in the studies identified in the current literature review include migraine-specific instruments, such as the MWPLQ, and generic measures of productivity, such as the WPSI, the Work and Health Questionnaire (WHQ), and the Health and Work Performance Questionnaire (HPQ). The developers of the MWPLQ found that the instrument was easy to comprehend, consistently interpreted, and not burdensome for patients.60 The WPSI is a reliable tool for estimating the time and cost impact of medical conditions on worker productivity.36,37 The WHQ is a newer questionnaire that is based on the Work and Health Interview, a telephone-administered questionnaire.61 The WHQ includes 17 questions that measure usual hours of work, missed workdays, days at work but not feeling well, and the impact of reduced performance at work.34 The World Health Organization has supported the HPQ for use across health conditions to inform the Global Burden of Disease project.62,63 The HPQ was developed to address the difficulty associated with measuring presenteeism.63 The HPQ also allows researchers to make adjustments for common challenges, such as when employees make up lost productivity time after hours.62,63 Schultz and Edington64 recently published a review of presenteeism instruments.
Fifth, double-blind studies are preferred over pretest and posttest studies for evaluating the effect of treatment on migraine-related loss in workplace productivity. Pretest and posttest studies may produce spurious results because improvements in worker productivity may represent regression to the mean and be unrelated to the intervention.
Sixth, placebo-controlled or head-to-head active controlled studies are preferred over those comparing treatment to usual therapy. Usual therapy is not standardized, so comparing results across studies is difficult, particularly as new treatments become available. For example, Davies et al16 compared rizatriptan therapy to usual therapy that included sumatriptan, but other studies comparing sumatriptan to usual therapy did not include other triptans in the usual therapy group.
Seventh, researchers should carefully consider the recall period for productivity data collection and evaluate the feasibility of collecting productivity data with both daily employee diaries and retrospective assessments, such as questionnaires. The recall periods used in the studies identified in this review ranged from hourly assessments of productivity31 to an annual recall period.18,24 For studies designed to compare migraine treatments, identifying the most appropriate recall period presents a challenge. The validation study for the MWPLQ was conducted using a 24-hour recall period for a single episode.16 Evidence suggests that a shorter recall period is more likely to provide accurate results65; however, a 24-hour or 1 work shift recall period is likely to underestimate the impact of a migraine that lasts for more than 24 hours. When asked to estimate the mean number of days of work affected by the typical migraine treated with usual therapy, patients in the study by Cohen et al14 reported that 2.05 days of work were affected by each migraine attack. A longer recall period may be needed when the goal is to compare loss in workplace productivity associated with migraine to productivity loss associated with other conditions. When comparing study participant recall with employer payroll records, Kessler et al62 found good concordance with payroll records with 7-day and 28-day (4-week) recall periods. Stewart et al66 recommend a 2-week recall period for measuring lost workplace productivity across a variety of conditions. This recommendation is based on their study of a 7-day recall period and a 4-week recall period. They found that the 4-week recall period led to substantial underreporting of lost productivity time. Evidence suggests that recall periods of 3 months or longer are less likely to provide accurate results.62 One study of cross-conditional absenteeism recommended a recall period of no more than 2 months.67
Eighth, losses in worker productivity should be collected and reported separately from personal time lost. Publications that describe loss in workplace productivity associated with migraine separately from total or leisure activity provide important information for employers, and calculation of economic impact is easier. The burden of migraine clearly affects many aspects of a migraineur's life. Other researchers have appropriately stated the importance of examining the impact of migraine on school and leisure activities.47-50 We acknowledge that reporting the productivity impact of migraine on work underestimates the true impact of migraine. Therefore, we recommend measuring and reporting workplace productivity and other types of productivity separately to provide the most useful information for employers, patients, and other decision makers.
Ninth, studies of new treatments should include measures of worker productivity. Although evidence suggests that effective treatment reduces the impact of migraine on worker productivity, the ability to compare productivity results across treatments will provide important information for patients, prescribers, and payers.
Other issues for consideration by future researchers include the impact that the timing of migraine onset has on worker productivity and the opportunities for real-time data collection. Migraineurs who wake with a headache are often already having moderate to severe pain, therefore missing the opportunity to be treated early. These before-work migraines may affect productivity and lead to additional presenteeism, partial absenteeism, or complete absenteeism. Another issue for consideration is the interictal burden of migraine. Capturing total loss in workplace productivity may be more complex than considering the sum of the impact of individual attacks. Studies have shown that migraineurs are likely to have higher anxiety levels than healthy controls.68,69 This increased anxiety level may affect productivity in the absence of an acute attack. The Migraine Interictal Burden Scale is a validated instrument that was developed to measure the impact of migraine between attacks and was presented recently in a conference abstract.70
New technology allows researchers to use new methods of data capture for collecting work productivity data. Pransky et al33 used an interactive voice response system, and patients called a toll-free number daily to provide their responses using a touch-tone telephone. Other options include data collection via the Internet or handheld computers or smart phones.
Developing comprehensive estimates of the impact of migraine on workplace productivity is a complex undertaking. However, with improved and consistent methods, productivity data can provide important information for patients, physicians, payers, and employers.
CONCLUSION
Migraine has a substantial negative impact on worker productivity. Both health care professionals and employers are stakeholders in providing effective treatment that can reduce that impact in most migraineurs. Employers have an opportunity to reduce the economic impact of migraine on worker productivity by implementing effective disease management programs. Such programs should include patient education on lifestyle changes that may affect the frequency and duration of migraine and, when appropriate, medications for early treatment and/or prophylaxis of migraine. Migraine researchers have an opportunity to improve the quality and comparability of worker productivity data and provide more comprehensive information to decision makers. As more treatment options become available to patients and prescribers, the impact of such therapy on worker productivity will become more important in determining the value of such interventions.
Acknowledgments
We acknowledge Ron C. Kessler, PhD, for his contribution to the design of this study.
Footnotes
GlaxoSmithKline provided funding to Relevant Health Outcomes, Inc, for conduct of the research and development of the submitted manuscript.
Dr Burton has served on an advisory board and received research support from Merck & Co and has received honoraria from GlaxoSmithKline, Merck & Co, Pfizer, and Johnson & Johnson. Dr Landy has served on speakers' bureaus for GlaxoSmithKline, Merck & Co, and Cephalon; has served on advisory boards for GlaxoSmithKline, Merck & Co, Pfizer, Cephalon, and Allergan; and has received research support from GlaxoSmithKline. Ms Downs has received support from GlaxoSmithKline. Dr Runken is an employee of GlaxoSmithKline.
REFERENCES
- 1.Lipton RB, Scher AI, Kolodner K, Liberman J, Steiner TJ, Stewart WF. Migraine in the United States: epidemiology and patterns of health care use. Neurology 2002;58(6):885-894 [DOI] [PubMed] [Google Scholar]
- 2.Hu XH, Markson LE, Lipton RB, Stewart WF, Berger ML. Burden of migraine in the United States: disability and economic costs. Arch Intern Med. 1999;159(8):813-818 [DOI] [PubMed] [Google Scholar]
- 3.Osterhaus JT, Townsend RJ, Gandek B, Ware JE., Jr Measuring the functional status and well-being of patients with migraine headache. Headache 1994;34(6):337-343 [DOI] [PubMed] [Google Scholar]
- 4.Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: results from the American Productivity Audit. J Occup Environ Med. 2003;45(12):1234-1246 [DOI] [PubMed] [Google Scholar]
- 5.Stang PE, Osterhaus JT. Impact of migraine in the United States: data from the National Health Interview Survey. Headache 1993;33(1):29-35 [DOI] [PubMed] [Google Scholar]
- 6.Lipton RB, Stewart WF, von Korff M. Burden of migraine: societal costs and therapeutic opportunities. Neurology 1997;48(3)(suppl 3):S4-S9 [DOI] [PubMed] [Google Scholar]
- 7.US Dept of Labor, Bureau of Labor Statistics http://www.bls.gov/cew/cewbultn07.htm. Quarterly census of employment and wages: employment and wages, annual averages 2007. Accessed February 10, 2009.
- 8.Freitag FG. The cycle of migraine: patients' quality of life during and between migraine attacks. Clin Ther 2007;29(5):939-949 [DOI] [PubMed] [Google Scholar]
- 9.Dahlöf CG, Dimenäs E. Migraine patients experience poorer subjective well-being/quality of life even between attacks. Cephalalgia 1995;15(1):31-36 [DOI] [PubMed] [Google Scholar]
- 10.Lipton RB, Diamond S, Reed M, Diamond ML, Stewart WF. Migraine diagnosis and treatment: results from the American Migraine Study II. Headache 2001;41(7):638-645 [DOI] [PubMed] [Google Scholar]
- 11.Headache Classification Committee of the International Headache Society Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 1988;8(suppl 7):1-96 [PubMed] [Google Scholar]
- 12.Tepper SJ, Dahlöf CG, Dowson A, et al. Prevalence and diagnosis of migraine in patients consulting their physician with a complaint of headache: data from the Landmark Study. Headache 2004;44(9):856-864 [DOI] [PubMed] [Google Scholar]
- 13.Adelman JU, Sharfman M, Johnson R, et al. Impact of oral sumatriptan on workplace productivity, health-related quality of life, healthcare use, and patient satisfaction with medication in nurses with migraine. Am J Manag Care 1996;2(11):1407-1416 [Google Scholar]
- 14.Cohen JA, Beall D, Beck A, et al. Sumatriptan treatment for migraine in a health maintenance organization: economic, humanistic, and clinical outcomes. Clin Ther 1999;21(1):190-204 [DOI] [PubMed] [Google Scholar]
- 15.Dasbach E, Carides G, Gerth W, Santanello N, Pigeon J, Kramer M. Work and productivity loss in the rizatriptan multiple attack study. Cephalalgia 2000;20(9):830-834 [DOI] [PubMed] [Google Scholar]
- 16.Davies GM, Santanello N, Gerth W, Lerner D, Block GA. Validation of a migraine work and productivity loss questionnaire for use in migraine studies. Cephalalgia 1999;19(5):497-502 [DOI] [PubMed] [Google Scholar]
- 17.Fishman P, Black L. Indirect costs of migraine in a managed care population. Cephalalgia 1999;19(1):50-57 [DOI] [PubMed] [Google Scholar]
- 18.Greiner DL, Addy SN. Sumatriptan use in a large group-model health maintenance organization. Am J Health Syst Pharm. 1996;53(6):633-638 [DOI] [PubMed] [Google Scholar]
- 19.Jhingran P, Cady RK, Rubino J, Miller DW, Grice RB, Gutterman DL. Improvements in health-related quality of life with sumatriptan treatment for migraine. J Fam Pract. 1996;42(1):36-42 [PubMed] [Google Scholar]
- 20.Lamb CE, Ratner PH, Johnson CE, et al. Economic impact of workplace productivity losses due to allergic rhinitis compared with select medical conditions in the United States from an employer perspective. Curr Med Res Opin 2006;22(6):1203-1210 [DOI] [PubMed] [Google Scholar]
- 21.Landy S, DeRossett SE, Rapoport A, et al. Two double-blind, multicenter, randomized, placebo-controlled, single-dose studies of sumatriptan/naproxen sodium in the acute treatment of migraine: function, productivity, and satisfaction outcomes. MedGenMed. 2007;9(2):53 [PMC free article] [PubMed] [Google Scholar]
- 22.Legg RF, Sclar DA, Nemec NL, Tarnai J, Mackowiak J. Cost benefit of sumatriptan to an employer. J Occup Environ Med. 1997;39(7):652-657 [DOI] [PubMed] [Google Scholar]
- 23.Lofland JH, Johnson NE, Batenhorst AS, Nash DB. Changes in resource use and outcomes for patients with migraine treated with sumatriptan: a managed care perspective [published correction appears in Arch Intern Med. 1999; 159(18):2228] Arch Intern Med. 1999;159(8):857-863 [DOI] [PubMed] [Google Scholar]
- 24.Lofland JH, Gagne JJ, Pizzi LT, Rupnow M, Silberstein SD. Impact of topiramate migraine prophylaxis on workplace productivity: results from two US randomized, double-blind, placebo-controlled, multicenter trials. J Occup Environ Med. 2007;49(3):252-257 [DOI] [PubMed] [Google Scholar]
- 25.Miller DW, Martin BC, Loo CM. Sumatriptan and lost productivity time: a time series analysis of diary data. Clin Ther 1996;18(6):1263-1275 [DOI] [PubMed] [Google Scholar]
- 26.Mushet GR, Miller DW, Clements B, Pait G, Gutterman DL. Impact of sumatriptan on workplace productivity, nonwork activities, and health-related quality of life among hospital employees with migraine. Headache 1996;36(3):137-143 [DOI] [PubMed] [Google Scholar]
- 27.Osterhaus JT, Gutterman DL, Plachetka JR. Healthcare resource and lost labour costs of migraine headache in the US. Pharmacoeconomics 1992;2(1):67-76 [DOI] [PubMed] [Google Scholar]
- 28.Schrader H, Stovner LJ, Helde G, Sand T, Bovim G. Prophylactic treatment of migraine with angiotensin converting enzyme inhibitor (lisinopril): randomised, placebo controlled, crossover study. BMJ 2001;322(7277):19-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schulman EA, Cady RK, Henry D, et al. Effectiveness of sumatriptan in reducing productivity loss due to migraine: results of a randomized, double-blind, placebo-controlled clinical trial. Mayo Clin Proc. 2000;75(8):782-789 [DOI] [PubMed] [Google Scholar]
- 30.Schwartz BS, Stewart WF, Lipton RB. Lost workdays and decreased work effectiveness associated with headache in the workplace. J Occup Environ Med. 1997;39(4):320-327 [DOI] [PubMed] [Google Scholar]
- 31.Cady RC, Ryan R, Jhingran P, O'Quinn S, Pait DG. Sumatriptan injection reduces productivity loss during a migraine attack: results of a double-blind, placebo-controlled trial. Arch Intern Med. 1998;158(9):1013-1018 [DOI] [PubMed] [Google Scholar]
- 32.Lofland JH, Frick KD. Workplace absenteeism and aspects of access to health care for individuals with migraine headache. Headache 2006;46(1):563-576 [DOI] [PubMed] [Google Scholar]
- 33.Pransky GS, Berndt E, Finkelstein SN, Verma S, Agrawal A. Performance decrements resulting from illness in the workplace: the effect of headaches. J Occup Environ Med. 2005;47(1):34-40 [DOI] [PubMed] [Google Scholar]
- 34.Stewart WF, Wood GC, Razzaghi H, Reed ML, Lipton RB. Work impact of migraine headaches. J Occup Environ Med. 2008;50(7):736-745 [DOI] [PubMed] [Google Scholar]
- 35.Durham CF, Alden KR, Dalton JA, et al. Quality of life and productivity in nurses reporting migraine. Headache 1998;38(6):427-435 [DOI] [PubMed] [Google Scholar]
- 36.Goetzel RZ, Ozminkowski RJ, Long SR. Development and reliability analysis of the Work Productivity Short Inventory (WPSI) instrument measuring employee health and productivity. J Occup Environ Med. 2003;45(7):743-762 [DOI] [PubMed] [Google Scholar]
- 37.Ozminkowski RJ, Goetzel RZ, Long SR. A validity analysis of the Work Productivity Short Inventory (WPSI) instrument measuring employee health and productivity. J Occup Environ Med. 2003;45(11):1183-1195 [DOI] [PubMed] [Google Scholar]
- 38.Lofland JH, Locklear JC, Frick KD. Different approaches to valuing the lost productivity of patients with migraine. Pharmacoeconomics 2001;19(9):917-925 [DOI] [PubMed] [Google Scholar]
- 39.Burton WN, Conti DJ, Chen CY, Schultz AB, Edington DW. The economic burden of lost productivity due to migraine headache: a specific worksite analysis. J Occup Environ Med. 2002;44(6):523-529 [DOI] [PubMed] [Google Scholar]
- 40.Lipton RB, Liberman JN, Kolodner KB, Bigal ME, Dowson A, Stewart WF. Migraine headache disability and health-related quality-of-life: a population-based case-control study from England. Cephalalgia 2003;23(6):441-450 [DOI] [PubMed] [Google Scholar]
- 41.Magnusson JE, Becker WJ. Migraine frequency and intensity: relationship with disability and psychological factors. Headache 2003;43(10):1049-1059 [DOI] [PubMed] [Google Scholar]
- 42.Terwindt GM, Ferrari MD, Tijhuis M, Groenen SM, Picavet HS, Launer LJ. The impact of migraine on quality of life in the general population: the GEM study. Neurology 2000;55(5):624-629 [DOI] [PubMed] [Google Scholar]
- 43.Lofland JH, Kim SS, Batenhorst AS, et al. Cost-effectiveness and cost-benefit of sumatriptan in patients with migraine. Mayo Clin Proc. 2001;76(11):1093-1101 [DOI] [PubMed] [Google Scholar]
- 44.Halpern MT, Lipton RB, Cady RK, Kwong WJ, Marlo KO, Batenhorst AS. Costs and outcomes of early versus delayed migraine treatment with sumatriptan. Headache 2002;42(10):984-999 [DOI] [PubMed] [Google Scholar]
- 45.Chen BH. Lisinopril for migraine. CMAJ 2001;164(9):1337 [Google Scholar]
- 46.Medtronic announces first clinical data on occipital nerve stimulation for chronic migraine to be presented at American Headache Society Meeting: early data show promise for new application of neurostimulation [press release] Minneapolis, MN: Medtronic; June26, 2008. http://wwwp.medtronic.com/Newsroom/NewsReleaseDetails.do?itemId=1214482108297 Accessed February 10, 2009 [Google Scholar]
- 47.Kwong JW, Taylor FR, Adelman JU. The effect of early intervention with sumatriptan tablets on migraine-associated productivity loss. J Occup Environ Med. 2005;47(11):1167-1173 [DOI] [PubMed] [Google Scholar]
- 48.Stewart WF, Lipton RB, Simon D, Von Korff M, Liberman J. Reliability of an illness severity measure for headache in a population sample of migraine sufferers. Cephalalgia 1998;18(1):44-51 [DOI] [PubMed] [Google Scholar]
- 49.Von Korff M, Stewart WF, Simon DJ, Lipton RB. Migraine and reduced work performance: a population-based diary study. Neurology 1998;50(6):1741-1745 [DOI] [PubMed] [Google Scholar]
- 50.Stewart WF, Lipton RB, Simon D. Work-related disability: results from the American Migraine Study. Cephalalgia 1996;16(4):231-238 [DOI] [PubMed] [Google Scholar]
- 51.Weaver MB, Mackowiak JI, Solari PG. Triptan therapy impacts health and productivity. J Occup Environ Med. 2004;46(8):812-817 [DOI] [PubMed] [Google Scholar]
- 52.Collins JJ, Baase CM, Sharda CE, et al. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. J Occup Environ Med. 2005;47(6):547-557 [DOI] [PubMed] [Google Scholar]
- 53.Gerth WC, Sarma S, Hu XH, Silberstein SD. Productivity cost benefit to employers of treating migraine with rizatriptan: a specific worksite analysis and model. J Occup Environ Med. 2004;46(1):48-54 [DOI] [PubMed] [Google Scholar]
- 54.Loeppke R, Hymel PA, Lofland JH, et al. American College of Occupational and Environmental Medicine Health-related workplace productivity measurement: general and migraine-specific recommendations from the ACOEM expert panel [published correction appears in J Occup Environ Med. 2003;45(9):940] J Occup Environ Med. 2003;45(4):349-359 [DOI] [PubMed] [Google Scholar]
- 55.Hymel P, Loeppke R, Baase C, et al. Establishing a research agenda in health and productivity [editorial]. J Occup Environ Med. 2004;46(6):518-520 [DOI] [PubMed] [Google Scholar]
- 56.Warshaw L, Burton W, Schneider W. Role of the workplace in migraine disease management. Dis Manag Health Outcomes 2001;9(2):99-115 [Google Scholar]
- 57.Lipton RB, Silberstein S, Burton W. Relieving an employer's economic headache: ten action steps for managing migraine in the workplace. Am J Integrated Healthcare 1997;1(1):26-31 [Google Scholar]
- 58.Burton WN, Conti DJ, Chen CY, Schultz AB, Edington DW. The impact of allergies and allergy treatment on worker productivity. J Occup Environ Med. 2001;43(1):64-71 [DOI] [PubMed] [Google Scholar]
- 59.Simon GE, Barber C, Birnbaum HG, et al. Depression and work productivity: the comparative costs of treatment versus nontreatment. J Occup Environ Med. 2001;43(1):2-9 [DOI] [PubMed] [Google Scholar]
- 60.Lerner DJ, Amick BC, III, Malspeis S, et al. The migraine work and productivity loss questionnaire: concepts and design. Qual Life Res. 1999;8:699-710 [DOI] [PubMed] [Google Scholar]
- 61.Stewart WF, Ricci A, Leotta C, Chee E. Validation of the work and health interview. Pharmacoeconomics 2004;22(17):1127-1140 [DOI] [PubMed] [Google Scholar]
- 62.Kessler RC, Barber C, Beck A, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occup Environ Med. 2003;45(2):156-174 [DOI] [PubMed] [Google Scholar]
- 63.Kessler RC, Ames M, Hymel PA, et al. Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to evaluate the indirect workplace costs of illness. J Occup Environ Med. 2004;46(6)(suppl):S23-S37 [DOI] [PubMed] [Google Scholar]
- 64.Schultz AB, Edington DW. Employee health and presenteeism: a systematic review. J Occup Rehabil. 2007September;17(3):547-579 Epub 2007 Jul 25 [DOI] [PubMed] [Google Scholar]
- 65.Koopsmanschap M, Burdorf A, Jacob K, Meerding WJ, Brouwer W, Severens H. Measuring productivity changes in economic evaluation: setting the research agenda. Pharmacoeconomics 2005;23(1):47-54 [DOI] [PubMed] [Google Scholar]
- 66.Stewart WF, Ricci JA, Leotta C. Health-related lost productive time (LPT): recall interval and bias in LPT estimates. J Occup Environ Med. 2004;46(6)(suppl):S12-S22 [DOI] [PubMed] [Google Scholar]
- 67.Severens JL, Mulder J, Laheij RJ, Verbeek AL. Precision and accuracy in measuring absence from work as a basis for calculating productivity costs in The Netherlands. Soc Sci Med. 2000;51(2):243-249 [DOI] [PubMed] [Google Scholar]
- 68.Devlen J. Anxiety and depression in migraine. J R Soc Med. 1994;87(6):338-341 [PMC free article] [PubMed] [Google Scholar]
- 69.Andrasik F, Kabela E, Quinn S, Attanasio V, Blanchard EB, Rosenblum EL. Psychological functioning of children who have recurrent migraine. Pain 1988;34(1):43-52 [DOI] [PubMed] [Google Scholar]
- 70.Buse DC, Bigal ME, Rupnow M, Reed M, Serrano D, Lipton RB. Development and validation of the Migraine Interictal Burden Scale (MIBS): a self-administered instrument for measuring the burden of migraine between attacks [abstract S05.003]. Neurology 2007;68(suppl 1):A89 [Google Scholar]