Abstract
Objectives
To characterize the functional trajectories of older persons admitted to a nursing home with disability after an acute hospitalization.
Design, Setting and Participants
Prospective cohort study of 754 community-living residents of greater New Haven, Connecticut, who were 70 years or older and initially nondisabled in four essential activities of daily living. The analytic sample included the 296 participants who were newly admitted to a nursing home with disability after an acute hospitalization.
Measurements
Information on nursing home admissions, hospitalizations, and disability in essential activities of daily living was ascertained during monthly telephone interviews for up to nine years. Disability was defined at the need for personal assistance in bathing, dressing, walking inside one's home, or transferring from a chair.
Results
The median time to the first nursing home admission with disability after an acute hospitalization was 46 (interquartile range, 27.5–75.5) months; and the mean number of disabled activities of daily living upon admission was 3.0 (standard deviation, 1.2). In the month preceding hospitalization, 189 (63.9%) participants had no disability. The most common functional trajectory was discharged home with disability (46.3%), followed by continuous disability in the nursing home (27.4%), discharged home without disability (21.6%), and noncontinuous disability in the nursing home (4.4%). Only 96 (32.4%) participants returned home at their premorbid level of function.
Conclusion
The functional trajectories among older persons admitted to a nursing home with disability following an acute hospitalization are generally poor. Additional research is needed to identify the factors responsible for these poor outcomes.
Keywords: aged, cohort studies, disability evaluation, activities of daily living, nursing homes
Among persons who were 65 years old in 2000, 44% are projected to be admitted to a nursing home during their remaining life, and over half of these are projected to have more than a year of nursing home use (1). According to the 2004 National Nursing Home Survey, approximately 1.5 million persons aged 65 years or older reside in a nursing home (2). The percentage of nursing home residents ranges from about 1.1% of those aged 65 to 74 years to 18.2% of those aged 85 years or older (3). These nursing home residents include a mixture of persons receiving subacute (or postacute) care and those receiving long-term (or custodial) care, many of whom were admitted initially for subacute care after a disabling event (4). The burden of disability among nursing homes residents is high and has been increasing over the past three decades. This increase is thought to be attributable to the aging of the nursing home population and the rise in alternative sites of long-term care (5).
Relatively little is known about the functional trajectories of older persons admitted to a nursing home with disability after an acute hospitalization. Prior studies have focused almost exclusively on long-term care residents; hence, they provide no information on subacute care residents or on transitions in disability after discharge from the nursing home. The absence of data in these areas is problematic given the high rate of transfers between the nursing home and other sites of care, including the community (6), and the importance of functional status to independent living.
In the current study, we set out to characterize the functional trajectories of older persons admitted to a nursing home with disability after an acute hospitalization. We hypothesized that three common and clinically meaningful trajectories would emerge—discharged home without disability, discharged home with disability, and continuous disability in the nursing home. To accomplish our aims, we used data from a unique longitudinal study that includes monthly assessments of disability for up to nine years, along with nearly complete ascertainment of nursing home admissions and hospitalizations, on a large cohort of community-living older persons.
Methods
Study Population
Participants were members of the Precipitating Events Project, a longitudinal study of 754 community-living persons, aged 70 years or older, who were nondisabled (i.e. required no personal assistance) at baseline in four essential activities of daily living—bathing, dressing, walking inside one's home, and transferring from a chair (7). Exclusion criteria included significant cognitive impairment with no available proxy (8), inability to speak English, diagnosis of a terminal illness with a life expectancy less than 12 months, and a plan to move out of the New Haven area during the next 12 months. Significant cognitive impairment was defined either as recall of zero of three items on short-term memory testing or as score less than 20 on the Folstein Mini-Mental State Examination (MMSE) (9) and recall of one or two of three items on the short-term memory test (8).
The cohort was assembled between March 1998 and October 1999; complete details have been provided elsewhere (7,10). Eligibility was determined during a screening telephone interview and was confirmed during an in-home assessment. Persons who were physically frail, as denoted by a timed score of greater than 10 seconds on the rapid gait test (i.e. walk back and forth over a 10-ft [3-m] course as quickly as possible), were oversampled to ensure a sufficient number of participants at increased risk for disability (11,12). Only 4.6% of the 2,753 health plan members who were alive and could be contacted refused to complete the screening telephone interview, and 75.2% of the 1,002 eligible members agreed to participate in the project. Persons who refused to participate did not differ significantly from those who were enrolled in terms of age or sex. The study protocol was approved by the Yale Human Investigation Committee, and all participants provided verbal informed consent.
Data Collection
A comprehensive home-based assessment was completed at baseline, while telephone interviews were completed monthly through December 2007, with a completion rate of 99%. During the comprehensive assessment, data were collected on demographic characteristics, physical frailty as previously described, cognitive status as assessed by the MMSE (9), and nine self-reported, physician-diagnosed chronic conditions: hypertension, myocardial infarction, congestive heart failure, stroke, diabetes mellitus, arthritis, hip fracture, chronic lung disease, and cancer. Participants were considered to be cognitively impaired if they scored less than 24 on the MMSE (9).
Assessment of Disability
Complete details regarding the assessment of disability, including formal tests of reliability and accuracy, are provided elsewhere (8). During the monthly telephone interviews, participants were assessed for disability using standard questions that were identical to those used during the screening telephone interview (8). For each of the four essential activities of daily living, we asked, “At the present time, do you need help from another person to (complete the task)?” Participants who needed help with any of the tasks were considered to be disabled. The reliability of our disability assessment was substantial (kappa=0.75) for reassessments completed within 48 hours and excellent (kappa=1.0) for reassessments performed the same day (8). For participants with significant cognitive impairment, the monthly telephone interviews were completed with a designated proxy. The accuracy of these proxy reports was also found to be excellent, with kappa=1.0 (8). As described in an earlier report (13), we used multiple imputation with 100 random draws per missing observation to address the small amount of missing monthly data on disability.
Ascertainment of Hospitalizations and Nursing Home Admissions
Information on hospitalizations and nursing home admissions was obtained during the monthly telephone interviews. Participants were asked whether they had stayed at least overnight in a hospital since the last interview, i.e. during the past month. The accuracy of these reports was high, with kappa = 0.94 (14). Participants who were hospitalized were asked to provide the primary reason for their admission. These reasons were subsequently grouped into distinct diagnostic categories using a revised version of the protocol described by Ferrucci et al. (15,16). Percent agreement, relative to an independent review of hospital records, was 82%.
Participants were also asked whether they had been admitted to a nursing home during the past month; if yes, the interviewer noted whether the participant was currently in a nursing home. The accuracy of this information was almost perfect, with kappa = 0.96 (17).
Assembly of Analytic Sample
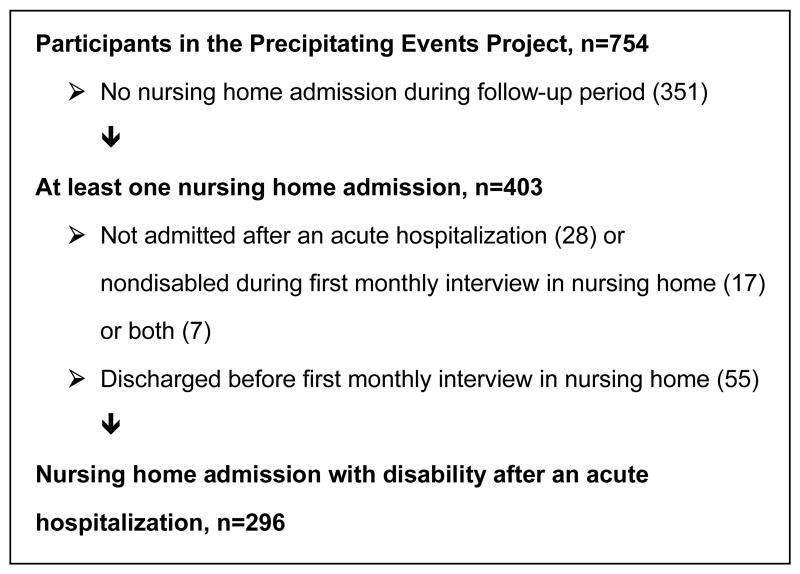
Figure 1 shows the assembly of the analytic sample. To be included, participants had to be admitted to a nursing home with disability after an acute hospitalization, as determined during the first monthly interview that was completed during the nursing home stay. Of the 754 participants, 403 (53.4%) had at least one nursing home admission and 296 (39.3%) had a nursing home admission with disability after an acute hospitalization. Of these, 279 (94.3%) represented the first nursing home admission during the follow-up period, while 14 (4.7%) and 3 (1.0%) represented the second and third admissions, respectively. To enhance clarity, these admissions will subsequently be referred to as the “index” nursing home admissions. Prior work suggests that most of these admissions included Medicare-reimbursed subacute care with rehabilitation services (18). Of the 55 persons who were discharged from the nursing home before completion of a monthly interview, 15 (26.9%) were newly disabled, 14 (25.9%) remained disabled, 19 (34.5%) remained nondisabled, and 7 (12.7%) were no longer disabled during the first monthly interview after their nursing home admission, relative to the monthly interview immediately prior to the acute hospitalization.
Figure 1.
Assembly of the Analytic Sample. Within parentheses are the number of persons excluded for the reasons specified.
Functional Trajectories
Using data from the monthly interviews, we first defined three clinically meaningful trajectories—discharged home without disability, discharged home with disability, and continuous disability in the nursing home. For the first two trajectories, disability status at home was determined during the first monthly interview that was completed after discharge from the nursing home. To meet criteria for the third trajectory, disability must have persisted throughout the nursing home stay, until the end of the follow-up period or death, and the participant must not have been discharged home. Based on review of the data, we subsequently defined a fourth trajectory—noncontinuous disability in the nursing home—which was identical to the third trajectory except that disability did not persist throughout the nursing home stay, meaning that participants had episodes of intermittent recovery.
Statistical Analysis
We compared the baseline characteristics of participants who were and were not included in the analytic sample, using t-tests to evaluate differences in means and chi-square tests to evaluate differences in percentages; and we calculated the frequency distributions of the primary reasons for the acute hospitalizations leading to the index nursing home admissions. Next, we calculated the median time to the index nursing home admission (from entry into the study), the mean number of disabled activities of daily living upon admission to the nursing home, and the duration of the nursing home admissions. Subsequently, we determined the frequency distributions of the functional trajectories after an index nursing home admission; because a large percentage of these admissions were brief, we stratified the results by the duration of the index admission. Among participants having admissions of two months or longer, we calculated the duration of these admissions for each of the functional trajectories; and we compared these values using the Wilcoxon rank sum test for participants who were discharged home with and without disability, respectively, and for those who had continuous and non-continuous disability in the nursing home, respectively.
For each of the functional trajectories, we determined the frequency distributions for the presence of disability prior to the acute hospitalization leading to the index nursing home admission. Disability status was determined during the monthly interview that was completed immediately prior to the hospitalization. Finally, we calculated the percentage of participants who returned home after an index nursing home admission at (or above) their premorbid level of function. This was determined by comparing the number of disabled activities of daily living during the first monthly interview that was completed after discharge from the nursing home with that during the monthly interview that was completed immediately prior to the hospitalization.
Results
Table 1 provides information on the baseline characteristics of participants in the analytic sample. The mean age was about 80 years; nearly two-thirds were female, more than half were physically frail, and about 12% were cognitively impaired. As compared with those who were not included in the analytic sample, participants in the analytic sample were older, had less education but more chronic conditions, and were more likely to live alone and to be physically frail. Table 2 provides information on the primary reasons for hospitalization. The most common diagnostic categories were fall-related injury, infection, arthritis (gout, hip and knee replacement, spinal stenosis, etc.), and cardiac (coronary heart disease, congestive heart failure, arrhythmia, etc.).
Table 1.
Baseline Characteristics of Participants Who Were and Were Not Included in Analytic Sample*
| Included in Analytic Sample | |||
|---|---|---|---|
| Characteristic | Yes N=296 |
No N=458 |
P Value† |
| Age (years), mean ± SD | 79.6 ± 5.4 | 77.7 ± 5.0 | <.001 |
| Female | 189 (63.9) | 298 (65.1) | .73 |
| Non-Hispanic white | 264 (89.2) | 418 (91.3) | .34 |
| Lives alone | 133 (44.9) | 165 (36.0) | .01 |
| Education (years), mean ± SD | 11.7 ± 2.9 | 12.2 ± 2.9 | .02 |
| Chronic conditions‡, mean ± SD | 2.0 ± 1.3 | 1.6 ± 1.1 | <.001 |
| Hypertension | 165 (55.7) | 251 (54.8) | .80 |
| Arthritis | 104 (35.1) | 123 (26.9) | .02 |
| Diabetes mellitus | 66 (22.3) | 71 (15.5) | .02 |
| Chronic lung diseases | 63 (21.3) | 69 (15.1) | .03 |
| Myocardium infarction | 61 (20.6) | 75 (16.4) | .14 |
| Cancer | 49 (16.6) | 75 (16.4) | .95 |
| Stroke | 39 (13.2) | 26 (5.7) | <.001 |
| Congestive heart failure | 20 (6.8) | 29 (6.3) | .82 |
| Hip fracture | 16 (5.4) | 18 (3.9) | .34 |
| Physical frailty§ | 158 (53.4) | 164 (35.8) | <.001 |
| Cognitive impairment‖ | 35 (11.8) | 51 (11.1) | .77 |
Data are presented as No. (%) unless otherwise indicated.
The t-test was used to evaluate differences in means, while the chi-square test was used to evaluate differences in percentages.
Chronic conditions are presented in descending order according to prevalence among participants included in the analytic sample.
Defined as a timed score greater than 10 seconds on the rapid gait test, i.e. walk back and forth over a 10-ft [3-m] course as quickly as possible (11,12).
Defined as a score of less than 24 on the Folstein Mini-Mental State Examination (9).
Table 2.
Primary Reasons for Hospitalization*
| Diagnostic category | No. (%) of all Admissions† |
|---|---|
| Fall-related injury | 52 (17.6) |
| Infection | 49 (16.6) |
| Arthritis | 34 (11.5) |
| Cardiac | 30 (10.1) |
| Stroke | 16 (5.4) |
| Cancer | 14 (4.7) |
| Gastrointestinal bleed | 8 (2.7) |
| Other medical | 73 (24.7) |
| Other surgical | 16 (5.4) |
| Other‡ | 4 (1.4) |
Ascertained by participant report and subsequently grouped into distinct diagnostic categories, as described in the Methods; the first seven categories are presented in order of frequency of occurrence.
The numerator includes the number of admissions during the relevant follow-up period for the specific reason, while the denominator includes the number of admissions for all reasons combined.
Includes responses that could not otherwise be categorized.
For participants in the analytic sample, the median time to the index nursing home admission was 46 (interquartile range [IQR], 27.5–75.5) months. Upon admission to the nursing home, the mean number of disabled activities of daily living was 3.0 (standard deviation [SD], 1.2); disability was present most commonly in bathing (94.9%), followed by dressing (75.3%), walking (68.6%), and transferring (60.5%). More than half (n=159, 53.7%) of the index nursing home admissions had a duration of 2 months or longer; of these, the median duration was 3 (IQR, 2–17) months, while the mean duration was 12.4 (SD, 17.1) months.
Table 3 provides information about the functional trajectories after an index nursing home admission. When the duration of the admission was only one month, the most common trajectory was discharged home with disability, followed by discharged home without disability. Each of the 14 participants classified as continuous disability died after a single month of disability in the nursing home.
Table 3.
Functional Trajectories after an Index Nursing Home Admission*
| Duration of Index Nursing Home Admission | ||||||
|---|---|---|---|---|---|---|
| Functional Trajectory† | 1 month N=137 |
≥ 2 months N=159‡ |
Total N=296 |
|||
| n | % | n | % | n | % | |
| Discharged home without disability | 47 | 34.3 | 17 | 10.7 | 64 | 21.6 |
| Discharged home with disability | 75 | 54.7 | 62 | 39.0 | 137 | 46.3 |
| Continuous disability in nursing home | 14 | 10.2 | 67 | 42.1 | 81 | 27.4 |
| Noncontinuous disability in nursing home | 0 | 0.0 | 13 | 8.2 | 13 | 4.4 |
| Lost to follow-up§ | 1 | 0.7 | 0 | 0.0 | 1 | 0.3 |
The first admission to a nursing home with disability following an acute hospitalization, as determined during the first monthly interview that was completed during the nursing home stay.
As defined in the Methods.
Two participants who remained in a nursing home refused to complete any subsequent interviews after 36 and 66 months and were classified, respectively, as continuous and noncontinuous disability.
This participant was discharged home after only one month in the nursing home but refused to complete any subsequent interviews.
When the duration of the admission was two or more months, the most common trajectories were continuous disability in the nursing home and discharged home with disability, which together comprised more than 80% of all the trajectories. Among the remaining participants having admissions of two or more months, relatively small numbers were discharged home without disability or had noncontinuous disability in the nursing home. Only 3 (23.1%) of the latter participants had three or more consecutive months without disability. The majority of participants with continuous (n=46, 68.7%) and noncontinuous (n=8, 61.5%) disability died in the nursing home, while all of the others were disabled in the nursing home at the end of the follow-up period. With relatively few exceptions, participants who were discharged home had very short stays in the nursing home (median, 2 months; IQR, 2–3 months); the duration of these admissions did not differ significantly between those who were discharged home with disability than without disability (P=.13, Wilcoxon test). Among participants who were not discharged home, there was considerable variability in the duration of nursing home stays (median 17 months, IQR, 5–33 months), although the durations were substantially shorter among those with continuous disability (median 11 months, IQR, 4–29 months) than those with noncontinuous disability (median 30 months, IQR, 18–43 months) (P=.01, Wilcoxon test).
All together, nearly half of the 296 participants with an index nursing home admission were discharged home with disability and more than a quarter had continuous disability in the nursing home, while only about one out of every five was discharged home without disability. The distribution of the functional trajectories did not differ significantly as a function of physical frailty (P=.11, Mantel-Haenszel chi-square). Among the 137 participants without physical frailty, a large minority (46.7%) was discharged home with disability, while similar percentages had continuous disability in the nursing home (25.6%) or were discharged home without disability (24.8%). Differences were observed across the four functional trajectories for age (P<.001, Wilcoxon test), but not sex (P=.16, Mantel-Haenszel chi-square). Participants who had noncontinuous disability in the nursing home were the oldest, with a median age of 85 years, while those who were discharged home without disability were the youngest, with a median age of 77.5 years.
Prior to the index nursing home admission, 189 (63.9%) participants had no disability (Table 4). Of these, less than 30% were ultimately discharged home without disability. Among the 84 initially nondisabled participants who were discharged home with disability, the mean number of disabled activities of daily living declined from 3.0 (SD, 1.2) during the first month in the nursing home to 1.9 (SD, 1.0) during the first month at home (P<.001, paired t-test). The functional trajectories were less favorable for the 107 participants who were disabled prior to the index nursing home admission. Only a small minority was discharged home without disability. Among the 53 initially disabled participants who were discharged home with disability, the mean number of disabled activities of daily living declined from 3.1 (SD 1.1) during the first month in the nursing home to 2.1 (SD 1.0) during the first month at home (P<.001, paired t-test); nearly 40% of these participants (n=21, 39.6%) did not regain their premorbid functional status. All together, of the 296 participants with an index nursing home admission only 96 (32.4%) returned home at (or above) their premorbid level of function.
Table 4.
Functional Trajectories According to Disability Status Prior to the Index Nursing Home Admission*
| Disability Prior to Nursing Home Admission | ||||
|---|---|---|---|---|
| Functional Trajectory† | Not Present N=189 |
Present N=107 |
||
| n | % | n | % | |
| Discharged home without disability | 55 | 29.1 | 9 | 8.4 |
| Discharged home with disability | 84 | 44.4 | 53 | 49.5 |
| Continuous disability in nursing home | 42 | 22.2 | 39 | 36.5 |
| Noncontinuous disability in nursing home | 7 | 3.7 | 6 | 5.6 |
| Lost to follow-up‡ | 1 | 0.5 | 0 | 0 |
Disability status was determined during the monthly interview that was completed immediately prior to the acute hospitalization leading to the index nursing home admission.
As defined in the Methods.
This participant was discharged home after only one month in the nursing home but refused to complete any subsequent interviews.
Discussion
In this prospective cohort study, we found that the functional trajectories among older persons admitted to a nursing home with disability after an acute hospitalization are generally poor, with only about one out of every five participants returning home without disability in essential activities of daily living. These poor outcomes were not preordained since the majority of our participants were nondisabled prior to their acute hospitalization and subsequent nursing home admission. Overall, less than a third of our participants returned home at their premorbid level of function.
We found that being discharged home with disability was the most common functional trajectory among older persons admitted with an index nursing home admission. The duration of these admissions was invariably short, with most being less than one or two months, and did not differ appreciably from that among participants who were discharged home without disability. Among participants who were discharged home with disability, there was a modest reduction in the number of disabled activities of daily living from the first month in the nursing home to the first month at home. Nonetheless, more than 60% of these participants had been nondisabled beforehand, and nearly 40% of the others did not regain their premorbid functional status.
Outcomes were particularly poor among participants who were not discharged home, representing 32% of our study population. All but 14% of these participants had continuous disability, with more than two-thirds subsequently dying in the nursing home. Mortality was also high (more than 60%) among participants with noncontinuous disability in the nursing home, and recovery of independent function was usually short-lived, with less than 25% having three or more consecutive months of no disability at any time during their nursing home stay. Among the nondecedents who were not discharged home, all were disabled at the end of the follow-up period. These poor outcomes cannot be explained solely on the basis of premorbid functional status, since the majority (52%) of participants who were not discharged home had no disability prior to their index nursing home admission.
Although comparisons are difficult because of differences in study design and populations, the outcomes of participants in the current study appear to be worse than those reported in one of the few prior studies that have evaluated patients admitted to a nursing home for subacute care (19). Using data from the Uniform Data System for Medical Rehabilitation, which included over 39,000 patients, with a mean age of 76 years (SD, 12), from a select group of 182 subacute care facilities, Deutsch and collegues demonstrated modest improvements in functional status from the time of admission to discharge. Mortality was remarkably low at only 2.1%, and 78% of patients were discharged to community settings. In contrast to our study, however, data were not available on premorbid functional status, and patients who remained in the nursing home were not followed beyond the initial subacute period, which rarely lasts beyond 2 or 3 months (20). Prior studies that have followed nursing home residents over longer periods of time have generally shown a decline in functional status (21-23).
The current study was not designed to identify the reasons for the poor functional outcomes. One possibility is that subacute care may not be particularly effective in restoring independent function after a disabling event. Although the benefit of rehabilitation after a stroke has been well established, there is relatively little evidence to support the effectiveness of rehabilitation after many other disabling events and essentially no evidence in a subacute care setting (24). Another possibility is that the prognosis after some disabling events is poor. In our study, the most common diagnostic categories for hospitalization leading to the index nursing home admission were fall-related injury, infection, and arthritis, which included joint replacements (among other conditions). Power was not adequate to determine whether the functional trajectories differed according to the primary reason for hospitalization.
Our study did not include data on the actual receipt of rehabilitation. Nonetheless, most new admissions to a nursing home following an acute hospitalization among disabled older persons include Medicare-reimbursed subacute care with rehabilitation services (18). Although rehabilitation can continue after discharge from subacute care, the availability and intensity of home-based rehabilitation declined substantially after passage of the 1997 Balanced Budget Act (18,25,26).
Participants had to be admitted to a nursing home with disability, as determined during the first monthly interview that was completed during the nursing home stay. Although the availability of monthly data on disability is a unique strength of our study, it is possible that some participants were admitted to the nursing home with disability but then recovered independent function by the time of the next monthly interview and that others were admitted without disability but then developed disability. However, only 4.2% of potential participants were excluded because they had no disability during the first monthly interview in the nursing home, and based on clinical experience the likelihood of the second scenario is low. Of note, at least one monthly interview was completed in the nursing home for the vast majority (86.4%) of potential participants. Of those who were excluded because they had been discharged from the nursing home before completion of a monthly interview, the majority (52.8%) were either newly or persistently disabled after their nursing home stay.
The validity of our results is strengthened by the nearly complete ascertainment of nursing home admissions, hospitalizations and disability, by the high reliability and accuracy of these assessments, and by the low rate of attrition. While our participants were members of a single health plan in a small urban area, the generalizability of our results is enhanced by our high participation rate, which was greater than 75%. Moreover, our study population reflects the demographic characteristics of older persons aged 65 years or older in New Haven county, which are comparable to the United States as a whole, with the exception of race (New Haven county has a larger proportion of non-Hispanic whites in this age group than the United States, 91% vs. 84%) (27). Although we oversampled persons who were physically frail, the distribution of the functional trajectories did not differ significantly as a function of physical frailty.
After a disabling event, subacute care in a nursing home is designed to optimize functional status and address ongoing medical conditions. The poor functional outcomes documented in the current study raise potential concerns regarding the effectiveness of the rehabilitative component of subacute care. Additional research is needed to determine the reasons underlying these poor functional outcomes, with the goal of enhancing subacute care and restoring independent function among newly disabled older persons.
Acknowledgments
We thank Denise Shepard, BSN, MBA, Andrea Benjamin, BSN, Paula Clark, RN, Martha Oravetz, RN, Shirley Hannan, RN, Barbara Foster, Alice Van Wie, BSW, Patricia Fugal, BS, Amy Shelton, MPH, and Alice Kossack for assistance with data collection; Wanda Carr and Geraldine Hawthorne for assistance with data entry and management; Peter Charpentier, MPH for development of the participant tracking system; and Joanne McGloin, MDiv, MBA for leadership and advice as the Project Director.
The work for this report was funded by grants from the National Institute on Aging (R37AG17560, R01AG022993). The study was conducted at the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342). Dr. Gill is the recipient of a Midcareer Investigator Award in Patient-Oriented Research (K24AG021507) from the National Institute on Aging.
Footnotes
Author Contributions: Dr. Gill had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Gill.
Acquisition of data: Gill.
Analysis and interpretation of data: Gill, Gahbauer, Han, Allore.
Drafting of the manuscript: Gill, Allore.
Critical revision of the manuscript for important intellectual content: Gill, Gahbauer, Han, Allore.
Statistical analysis: Gahbauer, Han, Allore.
Role of the Sponsors: The organizations funding this study had no role in the design or conduct of the study; in the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
References
- 1.Spillman BC, Lubitz J. New estimates of lifetime nursing home use: have patterns of use changed? Med Care. 2002;40:965–975. doi: 10.1097/00005650-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 2.CDC/NCHS. National Nursing Home Survey, selected years. 2007 http://www.cdc.gov/nchs/data/nnhsd/nursinghomes1973-2004.pdf.
- 3.Jones A. The National Nursing Home Survey: 1999 Summary. National Center for Health Statistics. Vital Health Stat. 2002;152:1–116. [PubMed] [Google Scholar]
- 4.Coleman EA. Challenges of systems of care for frail older persons: the United States of America experience. Aging Clin Exp Res. 2002;14:233–238. doi: 10.1007/BF03324444. [DOI] [PubMed] [Google Scholar]
- 5.Decker FH. Nursing homes, 1977-99: What has changed, what has not? Hyattsville, Maryland: National Center for Health Statistics; 2005. [Google Scholar]
- 6.Murtaugh CM, Litke A. Transitions through postacute and long-term care settings - Patterns of use and outcomes for a national cohort of elders. Med Care. 2002;40:227–236. doi: 10.1097/00005650-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: Incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135:313–321. doi: 10.7326/0003-4819-135-5-200109040-00007. [DOI] [PubMed] [Google Scholar]
- 8.Gill TM, Hardy SE, Williams CS. Underestimation of disability among community-living older persons. J Am Geriatr Soc. 2002;50:1492–1497. doi: 10.1046/j.1532-5415.2002.50403.x. [DOI] [PubMed] [Google Scholar]
- 9.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 10.Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004;291:1596–1602. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- 11.Gill TM, Williams CS, Tinetti ME. Assessing risk for the onset of functional dependence among older adults: The role of physical performance. J Am Geriatr Soc. 1995;43:603–609. doi: 10.1111/j.1532-5415.1995.tb07192.x. [DOI] [PubMed] [Google Scholar]
- 12.Gill TM, Richardson ED, Tinetti ME. Evaluating the risk of dependence in activities of daily living among community-living older adults with mild to moderate cognitive impairment. J Gerontol Med Sci. 1995;50A:M235–M241. doi: 10.1093/gerona/50a.5.m235. [DOI] [PubMed] [Google Scholar]
- 13.Gill TM, Guo Z, Allore HG. Subtypes of disability in older persons over the course of nearly 8 years. J Am Geriatr Soc. 2008;56:436–443. doi: 10.1111/j.1532-5415.2007.01603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gill TM, Allore H, Holford TR, et al. The development of insidious disability in activities of daily living among community-living older persons. Am J Med. 2004;117:484–491. doi: 10.1016/j.amjmed.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 15.Ferrucci L, Guralnik JM, Pahor M, et al. Hospital diagnoses, Medicare charges, and nursing home admissions in the year when older persons become severely disabled. JAMA. 1997;277:728–734. [PubMed] [Google Scholar]
- 16.Gill TM, Allore HG, Holford TR, et al. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292:2115–2124. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]
- 17.Gill TM, Allore HG, Han L. Bathing disability and the risk of long-term admission to a nursing home. J Gerontol A Biol Sci Med Sci. 2006;61:821–825. doi: 10.1093/gerona/61.8.821. [DOI] [PubMed] [Google Scholar]
- 18.Buntin MB. Access to postacute rehabilitation. Arch Phys Med Rehabil. 2007;88:1488–1493. doi: 10.1016/j.apmr.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 19.Deutsch A, Fiedler RC, Iwanenko W, et al. The Uniform Data System for Medical Rehabilitation report: Patients discharged from subacute rehabilitation programs in 1999. Am J Phys Med Rehabil. 2003;82:703–711. doi: 10.1097/01.PHM.0000083665.58045.29. [DOI] [PubMed] [Google Scholar]
- 20.Hoffman ED, Klees BS, Curtis CA. Overview of the Medicare and Medicaid programs. Health Care Finan Rev. 2000;22:175–193. [PubMed] [Google Scholar]
- 21.Richardson J, Bedard M, Weaver B. Changes in physical functioning in institutionalized older adults. Disabil Rehabil. 2001;23:683–689. doi: 10.1080/09638280110055084. [DOI] [PubMed] [Google Scholar]
- 22.McConnell ES, Pieper CF, Sloane RJ, Branch LG. Effects of cognitive performance on change in physical function in long-stay nursing home residents. J Gerontol A Biol Sci Med Sci. 2002;57:M778–M784. doi: 10.1093/gerona/57.12.m778. [DOI] [PubMed] [Google Scholar]
- 23.Gillen P, Spore D, Mor V, et al. Functional and residential status transitions among nursing home residents. J Gerontol A Biol Sci Med Sci. 1996;51:M29–M36. doi: 10.1093/gerona/51a.1.m29. [DOI] [PubMed] [Google Scholar]
- 24.Prvu Bettger JA, Stineman MG. Effectiveness of multidisciplinary rehabilitation services in postacute care: state-of-the-science. A review. Arch Phys Med Rehabil. 2007;88:1526–1534. doi: 10.1016/j.apmr.2007.06.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murkofsky RL, Phillips RS, McCarthy EP, et al. Length of stay in home care before and after the 1997 Balanced Budget Act. JAMA. 2003;289:2841–2848. doi: 10.1001/jama.289.21.2841. [DOI] [PubMed] [Google Scholar]
- 26.Murtaugh CM, McCall N, Moore S, et al. Trends in Medicare home health care use: 1997-2001. Health Aff (Millwood) 2003;22:146–156. doi: 10.1377/hlthaff.22.5.146. [DOI] [PubMed] [Google Scholar]
- 27.American FactFinder. U.S. Census Bureau. [May 29, 2003]; Available at: http://factfinder.census.gov.