Abstract
BACKGROUND:
Ideally, on diagnosis of asthma in a child, parents are counselled to decrease environmental tobacco smoke exposure to their children.
OBJECTIVE:
To determine whether a diagnosis of asthma in children altered parental smoking behaviour toward a reduction in environmental tobacco smoke exposure.
METHODS:
In 2002/2003, a survey was sent to 12,556 households with children born in 1995 in Manitoba. Parents were asked whether their seven-year-old child had asthma, and whether smokers were present in the home in 1995 and/or currently. The likelihood (OR) of a change in parental smoking behaviour was determined according to the presence of asthma in their child, a family history of asthma, the location of residence (rural or urban) and their socioeconomic status.
RESULTS:
A total of 3580 surveys (28.5%) were returned. The overall prevalence of parental smoking in 1995 and 2002/2003 was 32.2% and 23.4%, respectively (31.9%/23.2% and 32.3%/23.6% in rural and urban environments, respectively). In 2002/2003, the prevalence of parental smoking in homes with asthmatic children was 29.8%. Parents were not more likely to quit smoking (OR=1.01, 95% CI 0.66 to 1.54) or smoke outside (OR=1.02, 95% CI 0.56 to 1.83) if their child developed asthma. Parental smoking behaviour (quit smoking or smoked outside) did not change if there was a positive family history of asthma (OR=1.04, 95% CI 0.78 to 1.37), if they lived in a rural or urban location (OR=0.94, 95% CI 0.71 to 1.23), or if they were from a low- or high-income household (OR=1.12, 95% CI 0.85 to 1.47).
CONCLUSIONS:
The likelihood of altering parental smoking behaviour occurred independently of a diagnosis of asthma in their child, a family history of asthma, the location of residence and their socioeconomic status.
Keywords: Asthma, Children, Environmental tobacco smoke, Parents, Smoking cessation
Abstract
HISTORIQUE :
Idéalement, lorsqu’on diagnostique qu’un enfant est asthmatique, on conseille aux parents de limiter l’exposition de leur enfant à la fumée du tabac.
OBJECTIF :
Déterminer si un diagnostic d’asthme chez un enfant modifie le comportement des parents envers le tabagisme afin de réduire l’exposition à la fumée du tabac.
MÉTHODOLOGIE :
En 2002–2003, 12 556 ménages qui avaient eu un enfant en 1995 au Manitoba ont reçu un sondage. On a demandé aux parents si leur enfant de sept ans était asthmatique, s’il y avait eu des fumeurs dans la maison en 1995 et s’il y en avait encore. Les auteurs ont déterminé la probabilité (RC) de modification du comportement des parents envers le tabagisme d’après la présence d’asthme chez leur enfant, les antécédents familiaux d’asthme, le lieu de résidence (rural ou urbain) et le statut socioéconomique.
RÉSULTATS :
Au total, 3 580 sondages (28,5 %) ont été renvoyés. La prévalence globale de tabagisme des parents était de 32,2 % en 1995 et de 23,4 % en 2002–2003 (31,9 %/23,2 % et 32,3 %/23,6 % en milieu rural et urbain, respectivement). En 2002–2003, la prévalence de tabagisme des parents dans les ménages où un enfant était asthmatique était de 29,8 %. Les parents n’étaient pas plus susceptibles d’arrêter de fumer (RC=1,01, 95 % IC 0,66 à 1,54) ou de fumer à l’extérieur (RC=1,02, 95 % IC 0,56 à 1,83) si leur enfant devenait asthmatique. Le comportement des parents envers le tabagisme (arrêter de fumer ou fumer à l’extérieur) ne changeait pas s’il y avait des antécédents familiaux d’asthme (RC=1,04, 95 % IC 0,78 à 1,37), s’ils vivaient en milieu rural ou urbain (RC=0,94, 95 % IC 0,71 à 1,23) ou s’ils provenaient d’un ménage à revenu faible ou élevé (RC=1,12, 95 % IC 0,85 à 1,47).
CONCLUSIONS :
La probabilité de modifier le comportement des parents envers le tabagisme était la même, indépendamment du diagnostic d’asthme chez l’enfant, d’antécédents familiaux d’asthme, du lieu de résidence et du statut socioéconomique.
Exposure to environmental tobacco smoke (ETS) is associated with poor asthma control in children, frequent asthma exacerbations, increased rates of hospital use and reduced rates of recovery after asthma exacerbations. Passive smoke exposure has been shown to increase bronchial hyper-responsiveness in asthmatic children (1–8).
One would expect that parents, on learning that their child is asthmatic and given the knowledge that cigarette smoking exacerbates the illness, would give up smoking or at the very least smoke outside the home (9). Yet, existing research has not addressed this issue. Part of the difficulty is that the prevalence of smoking in the general population has decreased significantly over the past decade, but the reason for this decrease may have little or nothing to do with a specific child’s diagnosis of asthma. Interventions to change parental smoking behaviour have largely been unsuccessful (9–16). In the present study, we asked whether parents would stop smoking once they knew their child had asthma.
METHODS
The present study was approved by the Health Information Policy Committee of Manitoba Health and by the Health Research Ethics Board of the University of Manitoba, Winnipeg, Manitoba.
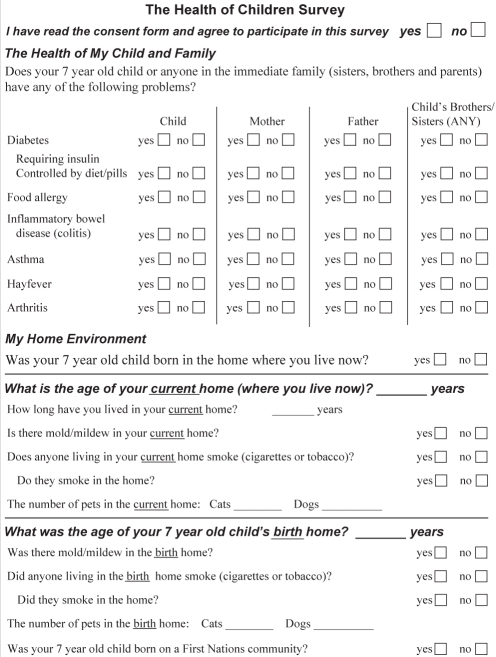
A mail-out survey to the parents of children born in the province of Manitoba in 1995 was sent on our behalf by Manitoba Health in November 2002 and again in January 2003. The survey focused on the health of the child and the child’s family, including atopic (ie, does your child have asthma, hay fever or food allergies?) and nonatopic conditions (ie, does your child have diabetes, inflammatory bowel disease or arthritis?). As well, there were questions (current and retrospective) about the child’s home environment: Does anyone living in this home smoke (cigarettes or tobacco)? Do they smoke inside the home? In 1995, did anyone living in your home smoke (cigarettes or tobacco)? Did they smoke inside the home in 1995?
A sample of the survey is appended to the end of the manuscript.
Methods to increase the response rate of the survey, such as the use of a short, colourful survey and two mail-outs, were used.
No incentives were provided for the return of the surveys.
Returned surveys were stratified by postal code into rural and urban locations. Urban families were stratified by postal code into five income quintiles. Low and high incomes were defined by the bottom and top quintiles, respectively.
Smoking behaviour change was defined as having quit smoking if parents reported indoor or outdoor smoking in 1995 but not in 2002/2003, smoking outdoors if parents reported indoor smoking in 1995 and outdoor smoking in 2002/2003, and any change if parents quit smoking or smoked outdoors in 2002/2003. The likelihood of smoking behaviour change was related to the diagnosis of asthma in the child born in 1995, adjusted for family history of asthma or allergy (hay fever and food allergy), household income and urban or rural location.
Data analysis was performed with SAS software (SAS Institute, USA), and χ2 tests were used to determine significant differences in rates of smoking. Multivariate logistic regression analysis was performed to determine the likelihood of smoking change. Statistical significance was set at P<0.05. Results are reported as OR with 95% CI.
RESULTS
A total of 16,384 children were born in the province of Manitoba in 1995. Of these, 13,980 children lived in the province in 2002. The surveys were sent to all of these families, except for those living in a First Nations community (‘reserves’, which will be studied separately) (n=12,556). The first and second mail-outs resulted in 2114 and 1725 returned surveys, respectively. A total of 3580 surveys (28.5%) were returned.
The demographics of survey participants are shown in Table 1. The urban to rural ratio reflects the population distribution of Manitoba.
TABLE 1.
Demographics of survey participants
| n | % | |
|---|---|---|
| Total returned surveys | 3580 | 100.0 |
| Male/Female children | 1791/1789 | 50.3/49.7 |
| Urban/Rural | 2138/1442 | 59.7/40.3 |
| Has a family history of atopy | 1501 | 41.9 |
| Children born with asthma in 1995 | 439 | 12.3 |
| Has a family history of asthma | 855 | 23.9 |
| Has a father with asthma | 244 | 6.8 |
| Has a mother with asthma | 328 | 9.1 |
| Has siblings with asthma | 484 | 13.5 |
The second mailing of the survey increased the response rate by 12%, but the final response rate was limited by the 17% response rate to the first mailing and the 809 noncurrent mailing addresses. The fact that the survey participants were representative of the asthmatic population was reassuring. The overall prevalence of asthma was 12.3 per 100 children. Asthma was reported in 7.9% of children living in northern rural areas, 10.3% in southern rural areas and 13.9% in urban areas.
A comparison of respondents to nonrespondents is shown in Table 2.
TABLE 2.
Comparison of respondents to nonrespondents
| Category | Percentage of respondents, % | Percentage of nonrespondents, % |
|---|---|---|
| Male | 50.3 | 51.1 |
| Female | 49.7 | 48.9 |
| Current asthma diagnosis | 12.1 | 11.1* |
| Maternal asthma in 1995 | 5.0 | 5.6† |
| Location of residence in 1995 | ||
| Urban | 61.2 | 55.4 |
| Rural south | 34.9 | 32.2 |
| Rural north | 3.9 | 12.3 |
| Location of residence in 2001 | ||
| Urban | 59.0 | 40.2 |
| Rural south | 37.7 | 34.0 |
| Rural north | 3.3 | 12.1 |
Current asthma diagnoses were determined by linking nonrespondent surveys to Manitoba Health Services Insurance Plan database records, and by determining which children had asthma as defined by the International Classification of Diseases ninth revision (ICD-9) code of 493 in-hospital or medical claims, or a prescription of an asthma medication (inhaled corticosteroids, inhaled or oral bronchodilators, cromolyn glycate and leukotriene receptor antagonist) in 2002;
Maternal asthma in 1995 was determined by linking nonrespondent surveys to 1995 Manitoba Health Services Insurance Plan database records, and by determining which mothers had asthma as defined by the ICD-9 code of 493 in-hospital or medical claims, or a prescription of an asthma medication (inhaled corticosteroid, inhaled or oral bronchodilators, cromolyn glycate and leukotriene receptor antagonists) in 1995
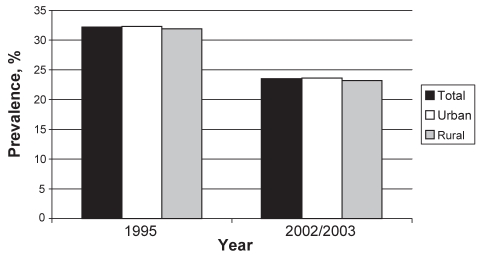
A total of 1151 surveys (32.2%) indicated that a smoker was in the home in 1995 when their child was born. A similar proportion (approximately 33%) of homes that had a smoker present was reported for participants living in both urban (32.3%) and rural (31.9%) locales. In 2002/2003, the prevalence of smoking in the home had decreased from 32.2% (n=1151) to 23.4% (n=839). This decline as shown in Figure 1 was similar for participants residing in both urban and rural locations (23.6% and 23.2%, respectively).
Figure 1).
Smoking prevalence in the province of Manitoba in 1995 and 2002/2003. The black bar represents total smoking prevalence. The white and grey bars represent the smoking prevalence in urban and rural locales, respectively. There were no statistically significant differences between locations
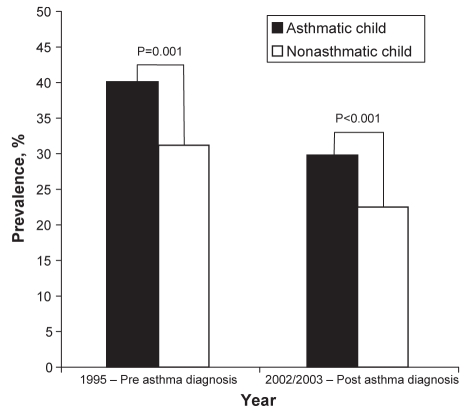
Just over 12% (n=439) of households reported that their child had asthma in 2002/2003. Among this group, 40.0% (n=171) had someone who smoked in 1995. Eight years later, the number of homes with smokers decreased to 29.8%. The prevalence rate was significantly greater than homes without an asthmatic child, where the smoking rates dropped from 31.2% in 1995 to 22.5% in 2002/2003. Homes with an asthmatic child were more likely to have a smoker present in 1995 (P=0.001) and in 2002/03 (P<0.001) (Figure 2).
Figure 2).
Smoking prevalence in homes with and without an asthmatic child. The black bar represents homes with an asthmatic child, and the white bar represents homes with nonasthmatic children. There was a statistically significant difference between the groups in both 1995 (P=0.001) and 2002/2003 (P<0.001)
When compared with homes without an asthmatic child, parents of asthmatic children were not more likely to quit smoking or smoke outside. This was independent of family history of asthma, urban or rural location, and household income (Table 3). As well, parental smoking behaviour (quit smoking or smoke outside) did not change if there was a positive family history of asthma, if they lived in a rural versus an urban location, or if they were from a low- versus high-income household (Table 4).
TABLE 3.
Likelihood of parental smoking behaviour change if their child has asthma
| Factor | Quit smoking* | Smoke outdoors* |
|---|---|---|
| Asthma, OR (95% CI) | 1.01 (0.66–1.54) | 1.02 (0.56–1.83) |
| No asthma, OR | 1.00 | 1.00 |
Adjusted for family history of asthma, rural or urban location, and income
TABLE 4.
Likelihood of parental smoking behaviour change (quit smoking or smoke outside)
| Factor | OR* | 95% CI |
|---|---|---|
| Family history of asthma | 1.04 | 0.78–1.37 |
| No family history of asthma | 1.00 | |
| Rural location | 0.94 | 0.71–1.23 |
| Urban location | 1.00 | |
| Low-income household | 1.12 | 0.85–1.47 |
| High-income household | 1.00 |
Logistic regression
DISCUSSION
Over the past decade, the prevalence of smoking has decreased. In Canada, there has been an 8.8% decrease in smokers aged 15 years or older from 1994/1995 to 2001 (most recent data available) (17). The results from our study indicate a similar downward trend – dropping from 32.2% in 1995 to 23.4% in 2002/2003.
The aim of our study was to determine whether a specific health factor, ie, a diagnosis of asthma in a child, could play a role in changing parental smoking behaviour. Our data suggested that this was not the case; rather, the parents participating in our study with a child diagnosed with asthma were not any more likely to alter their smoking behaviour than counterparts without an asthmatic child.
The present study suggests that ETS exposure is a risk factor for the development and persistence of childhood asthma (Figure 2). It appears that many parents continue to smoke, in spite of having children with asthma. Results from the Childhood Asthma Management Program (CAMP) study (11) revealed that of the children who reported cigarette smoking causing asthma symptoms, 26% had at least one parent who continued to smoke cigarettes. Given a similar proportion of parents who smoked in our study, this suggests, even if smoking causes obvious symptoms in the child, that this relationship does not induce parents to stop. Weiss et al (11) concluded that although environmental modification of asthmatic homes may occur, many children remain exposed to agents involving tobacco smoke that are known to trigger childhood asthma. It appears that the parents’ altruism toward the well-being of their children may not be sufficient to give them the ability to quit smoking.
Many social factors are likely to play a role in the overall decrease in smoking prevalence. Public pressure resulting in changes to governmental health policy appears to have a major impact (ie, increasing taxes for cigarettes and banning smoking in public settings). What, if anything, can be done to help the parents reduce or eliminate exposure of their asthmatic child to tobacco smoke? Most interventions have, to date, been ineffective in changing parental smoking behaviour even when parents are well aware that their asthmatic child’s health may improve (9–16,18). For example, Wakefield et al (10) attempted to provide feedback to low-income parents by using urinary cotinine levels and advice on home smoking restrictions to help decrease exposure. Unfortunately, the intervention proved to be unsuccessful (10).
In fact, some studies (18,19) suggest that counselling parents in smoking cessation may be detrimental. Irvine et al (18) found that a brief intervention to advise smoking parents about the risks of passive smoking to their asthmatic child may have made some parents less inclined to quit smoking. Their conclusion was that if a clinician believes that a child’s health is being affected by parental smoking, the parent’s smoking needs to be addressed as a separate issue from the child’s health. Continuing to ‘badger’ a family to quit smoking may even turn smoking parents away from using preventive health services due to the stigma that parents may feel because they are unable to stop the habit (19).
In one of the few positive studies, Hovell et al (20) showed a significant decrease in second-hand smoke exposure among mothers of preschool asthmatic children after providing seven counselling sessions over a three-month period. The authors concluded that this intensive form of counselling service should be made available to all. However, the cost burden of this intervention can be enormous and likely unacceptable to most publicly funded health care systems. This study demonstrates the positive effect of social support for these mothers. They are likely isolated with their child for long periods of time each day, and social supports may be critical to help alter negative behaviours.
We hypothesized that there would be greater resistance to smoking cessation among parents who participated in the survey from a lower socioeconomic status or from rural locales; however, we found no differences when compared with participants from high-income and urban locales, respectively. What this seems to indicate is that a minority of parents, regardless of social class and geographical location, are highly addicted to cigarette smoking.
For a general health and population survey, our response rate of 28.5% is greater than a recent general population health survey of comparable size, in which a response rate of only 20% was achieved (21). This is often considered a low response rate but only when compared with specific population surveys or problem-specific surveys (22,23). Our survey demographic population reflects the overall population in the province of Manitoba (63% urban and 37% rural, according to Statistics Canada 2001 census) (24), although we had slightly more surveys returned from southern rural regions compared with northern rural regions. The male to female response rate coincided with the sex distribution of children born in the province in 1995, as expected. There was a slight over-representation of returned surveys from those in the higher income quintiles; however, there was good representation from each of the income groups. Finally, we were reassured by how representative our survey was of the asthmatic population. The overall prevalence of asthma was 12.3 per 100 children. Asthma was reported in 7.9% of children living in northern rural areas, 10.3% in southern rural areas and 13.9% in urban areas. This geographic distribution was virtually identical to the prevalence of health care prescriptions for asthma as defined by the Manitoba Health databases for the full 1995 birth cohort (7.9% in northern rural areas, 9.6% in southern rural areas and 13.8% in urban areas) (25). Thus, the survey results were a good reflection of the entire 1995 Manitoba birth cohort.
There may have been an under-reporting of smoking behaviour in our survey because parents may have associated the question of smoking with the question regarding asthma. However, the survey was sent out as a general ‘child health and environment’ questionnaire, and questions regarding the health of their child – ie, does your child have asthma? – were separated from the questions regarding participant’s smoking behaviour. The fact that a greater proportion of surveys indicated that smokers were present in the homes and that their child had asthma compared with homes without children with asthma suggests that participants likely did not associate the two questions. Furthermore, the prevalence of smokers in the survey were similar to Statistics Canada data of trends of smoking across the country (17).
The prevalence of smoking in the province of Manitoba, like elsewhere in Canada, has significantly decreased in the past decade or so. Public pressure and changes to health care policy are likely among the major factors behind this trend. Nevertheless, there is still a substantial minority of Canadian adults who appear to be unable to quit smoking, many of whom are parents with children living at home.
CONCLUSIONS
Smoking is a major preventable cause of illness and death, even for those who are passively exposed. Advising parents that their asthmatic child’s condition is worsened by ETS is not enough to change behaviour. Innovative social policies need to be developed to help addicted individuals overcome their habit and deal with the underlying causes that promote smoking in the first place. Only then can the health burden for parents and their children be reduced if not completely eliminated.
Acknowledgments
A special thanks to the Study of Asthma, Genes and the Environment (SAGE) team, including Rishma Chooniedass, Donna Everette, Brenda Gerwing, Shamima Huq, Marilyn Lilley, Tanya Lilley-Chan, Ingrid Loewen, Diane Stewart and Michelle Tillett.
APPENDIX
Footnotes
FUNDING: This study was funded by the Canadian Institutes of Health Research; the Canadian Allergy, Asthma and Immunology Foundation; the Manitoba Institute of Child Health, Biology of Breathing Theme; and the National Training Program in Allergy and Asthma.
CONFLICT OF INTEREST: There are no conflicts of interest for any of the authors. The funding agencies had no role in the design and conduct of the study; the collection, analysis and review of the data; or the preparation, review, or approval of the manuscript.
REFERENCES
- 1.Abulhosn RS, Morray BH, Llewellyn CE, Redding GJ. Passive smoke exposure impairs recovery after hospitalization for acute asthma. Arch Pediatr Adolesc Med. 1997;151:135–9. doi: 10.1001/archpedi.1997.02170390025005. [DOI] [PubMed] [Google Scholar]
- 2.Cook DG, Strachan DP. Health effects of passive smoking. 3. Parental smoking and prevalence of respiratory symptoms and asthma in school age children. Thorax. 1997;52:1081–94. doi: 10.1136/thx.52.12.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cook DG, Strachan DP. Health effects of passive smoking-10: Summary of effects of parental smoking on the respiratory health of children and implications for research. Thorax. 1999;54:357–66. doi: 10.1136/thx.54.4.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans D, Levison MJ, Feldman CH, et al. The impact of passive smoking on emergency room visits of urban children with asthma. Am Rev Respir Dis. 1987;135:567–72. doi: 10.1164/arrd.1987.135.3.567. [DOI] [PubMed] [Google Scholar]
- 5.Oddoze C, Dubus JC, Badier M, et al. Urinary cotinine and exposure to parental smoking in a population of children with asthma. Clin Chem. 1999;45:505–9. [PubMed] [Google Scholar]
- 6.Wakefield M, Banham D, Martin J, Ruffin R, McCaul K, Badcock N. Restrictions on smoking at home and urinary cotinine levels among children with asthma. Am J Prev Med. 2000;19:188–92. doi: 10.1016/s0749-3797(00)00197-5. [DOI] [PubMed] [Google Scholar]
- 7.Winkelstein ML, Tarzian A, Wood RA. Parental smoking behavior and passive smoke exposure in children with asthma. Ann Allergy Asthma Immunol. 1997;78:419–23. doi: 10.1016/S1081-1206(10)63206-1. [DOI] [PubMed] [Google Scholar]
- 8.Wong GC, Berman BA, Hoang T, Bernaards C, Jones C, Bernert JT. Children’s exposure to environmental tobacco smoke in the home: Comparison of urine cotinine and parental reports. Arch Environ Health. 2002;57:584–90. doi: 10.1080/00039890209602092. [DOI] [PubMed] [Google Scholar]
- 9.Bahceciler NN, Barlan IB, Nuhoglu Y, Basaran MM. Parental smoking behavior and the urinary cotinine levels of asthmatic children. J Asthma. 1999;36:171–5. doi: 10.3109/02770909909056314. [DOI] [PubMed] [Google Scholar]
- 10.Wakefield M, Banham D, McCaul K, et al. Effect of feedback regarding urinary cotinine and brief tailored advice on home smoking restrictions among low-income parents of children with asthma: A controlled trial. Prev Med. 2002;34:58–65. doi: 10.1006/pmed.2001.0953. [DOI] [PubMed] [Google Scholar]
- 11.Weiss ST, Horner A, Shapiro G, Sternberg AL, Childhood Asthma Management Program (CAMP) Research Group The prevalence of environmental exposure to perceived asthma triggers in children with mild-to-moderate asthma: Data from the Childhood Asthma Management Program (CAMP) J Allergy Clin Immunol. 2001;107:634–40. doi: 10.1067/mai.2001.113869. [DOI] [PubMed] [Google Scholar]
- 12.McIntosh NA, Clark NM, Howatt WF. Reducing tobacco smoke in the environment of the child with asthma: A cotinine-assisted, minimal-contact intervention. J Asthma. 1994;31:453–62. doi: 10.3109/02770909409089487. [DOI] [PubMed] [Google Scholar]
- 13.Woodward A, Owen N, Grgurinovich N, Griffith F, Linke H. Trial of an intervention to reduce passive smoking in infancy. Pediatr Pulmonol. 1987;3:173–8. doi: 10.1002/ppul.1950030311. [DOI] [PubMed] [Google Scholar]
- 14.Chilmonczyk BA, Palomaki GE, Knight GJ, Williams J, Haddow JE. An unsuccessful cotinine-assisted intervention strategy to reduce environmental tobacco smoke exposure during infancy. Am J Dis Child. 1992;146:357–60. doi: 10.1001/archpedi.1992.02160150097031. [DOI] [PubMed] [Google Scholar]
- 15.Ashenden R, Silagy C, Weller D. A systematic review of the effectiveness of promoting lifestyle change in general practice. Fam Pract. 1997;14:160–76. doi: 10.1093/fampra/14.2.160. [DOI] [PubMed] [Google Scholar]
- 16.Schönberger HJ, Maas T, Dompeling E, Knottnerus JA, van Weel C, van Schayck CP. Compliance of asthmatic families with a primary prevention programme of asthma and effectiveness of measures to reduce inhalant allergens – a randomized trial. Clin Exp Allergy. 2004;34:1024–31. doi: 10.1111/j.1365-2222.2004.01991.x. [DOI] [PubMed] [Google Scholar]
- 17.Gilmore J.Report on Smoking in Canada 1985 to 2001 Health Statistics Division, Statistics Canada.2002
- 18.Irvine L, Crombie IK, Clark RA, et al. Advising parents of asthmatic children on passive smoking: Randomised controlled trial. BMJ. 1999;318:1456–9. doi: 10.1136/bmj.318.7196.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McBride CM, Lozano P, Curry SJ, Rosner D, Grothaus LC. Use of health services by children of smokers and nonsmokers in a health maintenance organization. Am J Public Health. 1998;88:897–902. doi: 10.2105/ajph.88.6.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hovell MF, Zakarian JM, Matt GE, Hofstetter CR, Bernert JT, Pirkle J. Effect of counselling mothers on their children’s exposure to environmental tobaco smoke: Randomised controlled trial. BMJ. 2000;321:337–42. doi: 10.1136/bmj.321.7257.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Angus VC, Entwistle VA, Emslie MJ, Walker KA, Andrew JE. The requirement for prior consent to participate on survey response rates: A population-based survey in Grampian. BMC Health Serv Res. 2003;3:21. doi: 10.1186/1472-6963-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ronckers C, Land C, Hayes R, Verduijn P, van Leeuwen F. Factors impacting questionnaire response in a Dutch retrospective cohort study. Ann Epidemiol. 2004;14:66–72. doi: 10.1016/s1047-2797(03)00123-6. [DOI] [PubMed] [Google Scholar]
- 23.Eaker S, Bergström R, Bergström A, Adami HO, Nyren O. Response rate to mailed epidemiologic questionnaires: A population-based randomized trial of variations in design and mailing routines. Am J Epidemiol. 1998;147:74–82. doi: 10.1093/oxfordjournals.aje.a009370. [DOI] [PubMed] [Google Scholar]
- 24.Statistics Canada 2001. Census of Canada. <www.statcan.ca> (Version current at August 22, 2007).
- 25.Kozyrskyj AL, Becker AB. Rural-urban differences in asthma prevalence: Possible explanations. J Allergy Clin Immunol. 2004;113(Suppl):S306. [Google Scholar]