Abstract
Tuberculoma of the lung is one of manifestations in tuberculosis and usually presents as a solitary pulmonary nodule (SPN). It is difficult to differentiate tuberculoma from SPN by other benign or malignant diseases. At present, the crucial role of video-assisted thoracoscopic surgery (VATS) in diagnosis and treatment of pulmonary diseases has been well acknowledged. Here, we reported 53 patients undergoing VATS resection for tuberculomas in our series. No postoperative mortality was found and only two patients experienced prolonged air-leakage (>7 d) and two had minor wound infections that were recovered after anti-tuberculosis or antibiotic treatment. Anti-tuberculosis chemotherapy from 6 to 12 months was routinely used postoperatively. We conclude that VATS is a satisfactory tool for the diagnosis and treatment of tuberculoma and can also establish a reliable diagnosis for all patients with SPNs.
Keywords: Tuberculoma, Video-assisted thoracoscopic surgery (VATS), Anti-tuberculosis treatment
INTRODUCTION
Tuberculosis (TB), once the leading cause of death in Taiwan decades ago, has remarkably decreased worldwide in incidence, prevalence, and mortality rate in recent years, due to socioeconomic development and effective chemotherapy (WHO, 2008; Hsueh et al., 2006). However, its incidence and prevalence in Taiwan are still higher than western countries. Tuberculoma, a manifestation of TB, usually presents as a solitary pulmonary nodule (SPN) (van Dyck et al., 2003). Contrary to TB, the incidence of lung cancer has gradually increased and it has become the leading cause of cancer mortality in Taiwan and rest of the world over the last ten years (van Dyck et al., 2003). Therefore, surgical resection has become beneficial to exclude the possibility of malignancy (Ishida et al., 1992; Mitsudomi et al., 1990). Besides, the resection of tuberculoma is valuable for subsequent treatment strategy, because its appearance in adults sometimes stands for a post-primary lesion (Good and Wilson, 1958). Video-assisted thoracoscopic surgery (VATS) has been developed as a minimally invasive and effective tool for diagnosis and treatment of SPNs, including the tuberculomas (Luh and Liu, 2006). Herein we review our experiences in the diagnosis and treatment of tuberculoma by VATS.
PATIENTS AND METHODS
From July 1994 to April 2008, 53 patients with pathologically proved tuberculoma after VATS procedures were included in the present study. Age, sex, history of smoking, and other pulmonary diseases were recorded. Routine physical examination and a series of evaluations including chest X-ray, chest computed tomography (CT) (Fig.1), sputum smear, culture and cytology, and fibro-bronchoscopy were performed. Skin test for purified protein derivative (PPD) was not performed for these patients because TB is still high prevalent in our population. Surgical resection was indicated for the diagnosis of unknown pulmonary nodular lesion as well as improving the treatment effects for subsequent anti-TB chemotherapies. VATS procedures with or without the use of utility minithoracotomy incisions were performed, which we use routinely for limited resections for pulmonary lesions except for ones with dense pleural adhesions. Open posterolateral thoracotomy, which was excluded from this study, was only reserved for some patients requiring lobectomy or dissection of dense pleural adhesions.
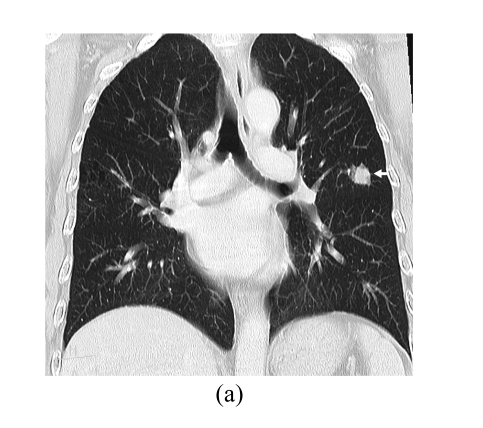
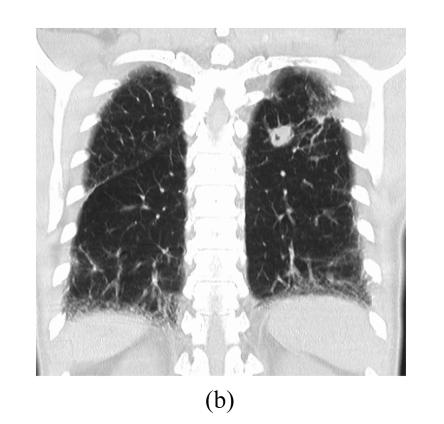
Fig. 1.
CT findings of tuberculomas. They can manifest (a) as a solitary, well-defined nodule with spiculate margins or (b) as a nodule with satellite lesions
VATS was performed after chest CT reviewing by the operator. Only four patients with small (<1 cm) or deep-seated (more than 0.5 cm from the pleural surface) nodules required preoperative hook wire localization. For all the others the lesions could be successfully localized by CT imaging estimation and hand palpation intraoperatively. General anesthesia was induced, and a double lumen endotracheal tube was placed through the guide of flexible bronchoscopy. The operative lung was insufflated. After prepping and draping, the scope port was inserted and its localization depended on the sites of the lesions. Two working ports or single utility incision was then applied for further work on tumor resections. Excising tumor located in the wedge of lung tissue was accomplished by the use of auto suture stapling device (Endo GIA™, Auto Suture, 30~60 mm in length and 3.5~4.8 mm in thickness, Fig.2). One to two 28~32 Fr chest tubes were introduced into the chest cavity postoperatively, and their removal was determined by the draining fluid amount, character, any air-leakage or retained fluid or air in the chest cavity. Anti-tuberculosis chemotherapy was administered after confirming the diagnosis of TB.
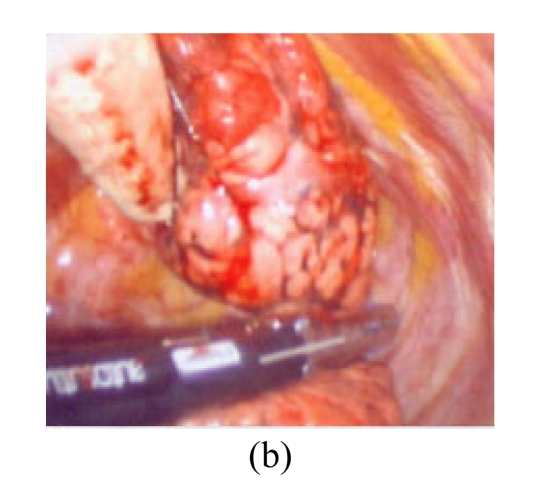
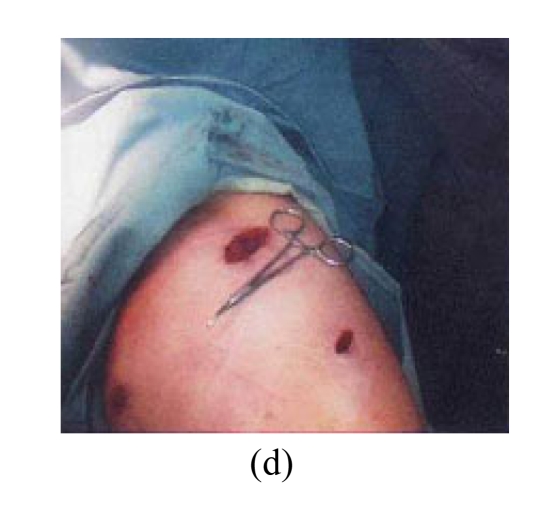
Fig. 2.
VATS for the resection of tuberculoma. (a) Dissecting the pleural adhesion; (b) The Endo GIA™ for the resection of tumor; (c) The cut surface of tumor, revealing caseous necrosis inside the mass; (d) The small wounds of VATS
RESULTS
Clinical features
There were 37 male and 16 female patients, with ages ranging from 18~82 years with mean (42.3±12.5) years. Forty-one (77.3%) of them were asymptomatic and the pulmonary lesion was detected by screening chest X-ray. The remaining 12 patients had respiratory symptoms such as cough, copious, or bloodtinged sputum. Eleven of them had been previously treated for pulmonary tuberculosis. On admission, physical examination was unremarkable and for patients considering surgical treatment, the results of smear, culture, and cytology from sputum, transbronchial or CT/echo-guided needle aspiration or biopsy were negative.
Radiographic findings
According to the chest X-ray and CT pictures, 45 patients had SPNs, and the remaining 8 had satellite nodule(s). The nodular margin was smooth and well-defined in 21, spicular in 23, and notching in 9. Calcification in the nodule was noted in 17 patients, and vascular convergence in 7 (Fig.1).
Preoperative diagnosis
Primary lung cancers were suspected in 36 (67.9%) patients. Metastatic carcinomas were suspected in 2 patients because they had histories of prior colon or breast carcinoma. The remaining 15 patients were diagnosed preoperatively as tuberculoma or other benign pulmonary lesions such as hamartoma or sclerosing hemangioma. Surgical treatment was indicated because these tumors did not decrease in size despite antituberculosis chemotherapy being administered.
Operative and pathological findings
These tumors ranged from 0.7 to 4 cm in diameter, and they were located at the right upper lobe in 19 patients, the right lower lobe in 10, the left upper lobe in 15, and the left lower lobe in 9. Forty-two patients underwent pulmonary wedge resection and the remaining 11 pulmonary segmentectomy. Lobectomy or pneumonectomy was not required for these patients. These procedures were completed through 3 port VATS procedures in 29 patients, using VATS with a utility incision (from 4 to 7 cm in length) in the remaining 24. The operative time ranged from 36 to 185 min (mean (78±26) min). The diagnosis of tuberculoma was confirmed pathologically for all patients. However, the reports of only 22 (41.5%) could be classified as “active” or “inactive.” Active tuberculoma, defined as a central mass of epithelioid cells with Langhan’s type giant cells and varying degrees of caseation (Ishida et al., 1992), was noted in 15 patients, while the remaining 7 were classified as inactive, in which the mass was mostly composed of acellular caseous material and fibrosis, with or without calcification (Ishida et al., 1992). In comparison with their radiological features, the active lesions were mostly presented as nodules with speculated margins and the inactive ones with smooth margins. There was no postoperative mortality and only two patients experienced prolonged air-leakage (>7 d) and two patients had minor wound infections that were recovered after anti-tuberculosis or antibiotic treatment. The median postoperative hospital stay and chest tube insertion period were 6 d (range: 3~29 d) and 5 d (range: 2~28 d), respectively. Anti-tuberculosis chemotherapy from 6 to 12 months was routinely used postoperatively. No recurrence of tuberculous lesions for these patients was noted at adjacent sites during the follow-up period.
DISCUSSION
TB is a major cause of illness and death worldwide, especially in Asia and Africa. Globally, 9.2 million new cases and 1.7 million deaths from TB occurred in 2006, of which 0.7 million cases and 0.2 million deaths were in HIV-positive people (WHO, 2008). TB has been one of the major causes of death in Taiwan for decades, and was ranked third in 1953, sixth in 1975, and 12th from 1995 to 2002 (Hsueh et al., 2006). The mortality rate (cases per 100000 populations) was 295 in 1947 and decreased gradually to 4.3 in 2005. The annual incidence (cases per 100000 populations) of TB was 5150 in 1947 and had declined to 30~40 in the 1970s. However, it rose in the next 20 years, which might partially be attributed to better disease registration system and patient identification. The incidence reached a peak of 74.6 in 2002 and then slowly decreased to 72.5 in 2005.
TB could be classified into primary and post-primary types. Usually a primary disease is characterized by mediastinal and/or hilar adenopathies, and parenchymal opacities typically located in the anterior segments of the lungs. Most patients are symptom-free with only parenchymal scar and calcified lymph nodes left. Post-primary disease is characterized by lung infiltration and formation of cavities mostly situated in the apicoposterior lung segments and superior segments of the lower lobes. It can also be discovered at extrapulmonary sites (Luh et al., 2007). Nonspecific complaints such as cough, anorexia, weight loss, fatigue, fever, hemoptysis or even spontaneous pneumothorax may happen (Chen et al., 2008). In general, the primary TB develops in children while post-primary TB presents in adults due to reactivation of dormant residual foci. However, more and more adult cases were found with primary TB, manifested as newly appearing pulmonary lesions combined with adjacent lymphadenopathies (van Dyck et al., 2003). TB termed as “old” or “inactive,” which is defined as radiographic stability for 6 months and negative sputum cultures, should be replaced by radiographically stable TB, as viable bacilli may persist despite adequate therapy (McAdams et al., 1995).
Tuberculoma usually manifests on the chest X-ray, as a fairly discrete, but sometimes with a spicular margin, nodule, or mass in the lungs. It is one of the most common benign nodules representing up to 25% of all resected pulmonary SPNs (Andreu et al., 2004). Differentiation between the active tuberculomas and malignant tumors is not easy. CT with dynamic imaging can not only more accurately differentiate between the benign and malignant nodules but also assess the activities of tuberculomas (Tateishi et al., 2002). More and more diagnostic tools have been reported to measure the activities of pulmonary tuberculoma, such as double phase acquisition of (18) F fluorodeoxyglucose (FDG) positron emission tomography (PET), CT combined with computer-aided diagnosis (CAD), electrocardiograph (ECG)-gated magnetic resonance imaging (MRI), or 99mTc radioisotope scanning (Kim et al., 2008; Park et al., 2008; Plachcinska et al., 2004; Schaefer et al., 2006). However, there was no statistical difference in the prediction accuracy between the newer imaging techniques or quantitative, computerized measurements and the traditional visual assessments of CT scans by senior radiologists.
The benefits of surgical resection for pulmonary tuberculoma include the accurate diagnosis and differential diagnosis, determining future treatment strategies, and decreasing the dose and duration of anti-TB chemotherapy (Cherkasov et al., 1997). Cancer coexisting with tuberculoma could have occurred in our patients and some other reported cases. However, mechanisms of this phenomenon remain unclear (Ashizawa et al., 2004; Kim et al., 2001). Limited pulmonary resection was required only for patients with tuberculoma or most of other benign SPNs (Didenko, 2007); therefore, this procedure could be performed with the use of VATS, replacing traditional open thoracotomy (Congregado Loscertales et al., 2002; Luh and Liu, 2006; Prytz and Hansen, 1976). VATS can be a good choice for the diagnosis of all SPNs and for the treatment of some benign nodules, including tuberculoma, or solitary metastases (Congregado Loscertales et al., 2002; Luh and Liu, 2006). VATS can be widely applied in the diagnosis or treatment of various TB-related diseases, such as pleural effusion, single or multiple nodules, empyema, or cavitary lesions (Porkhanov et al., 2002). Anti-TB chemotherapy is not necessarily required preoperatively, but usually administered postoperatively (Perel′man and Kravtsova, 1989; Prytz and Hansen, 1976).
In conclusion, pulmonary tuberculoma that usually manifests as an SPN is difficult to differentiate from a malignant tumor, but VATS can provide a reliable diagnosis and part of treatment.
References
- 1.Andreu J, Caceres J, Pallisa E, Martinez-Rodriguez M. Radiological manifestations of pulmonary tuberculosis. Eur J Radiol. 2004;51(2):139–149. doi: 10.1016/j.ejrad.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 2.Ashizawa K, Matsuyama N, Okimoto T, Hayashi H, Takahashi T, Oka T, Nagayasu T, Hayashi K. Coexistence of lung cancer and tuberculoma in the same lesion: demonstration by high resolution and contrast-enhanced dynamic CT. Br J Radiol. 2004;77(923):959–962. doi: 10.1259/bjr/31864795. [DOI] [PubMed] [Google Scholar]
- 3.Chen YJ, Luh SP, Hsu KY, Chen CR, Tsao TC, Chen JY. Video-assisted thoracoscopic surgery (VATS) for bilateral primary spontaneous pneumothorax. J Zhejiang Univ Sci B. 2008;9(4):335–340. doi: 10.1631/jzus.B0720235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cherkasov VA, Stepanov SA, Rudoi EP. Immediate and late outcomes of surgical treatment in patients with tumor-simulating pulmonary tuberculosis. Probl Tuberk. 1997;(3):38–39. (in Russian) [PubMed] [Google Scholar]
- 5.Congregado Loscertales M, Giron Arjona JC, Jimenez Merchan R, Arroyo Tristan A, Arenas Linares C, Ayarra Jarne J, Loscertales J. Usefulness of video-assisted thoracoscopy for the diagnosis of solitary pulmonary nodules. Arch Bronconeumol. 2002;38(9):415–420. doi: 10.1016/s0300-2896(02)75254-x. [DOI] [PubMed] [Google Scholar]
- 6.Didenko GV. Results of surgical treatment in patients with pulmonary tuberculosis. Probl Tuberk Bolezn Legk. 2007;(11):26–28. (in Russian) [PubMed] [Google Scholar]
- 7.Good CA, Wilson TW. The solitary circumscribed pulmonary nodule: study of seven hundred five cases encountered roentgenologically in a period of three and one-half years. J Am Med Assoc. 1958;166(3):210–215. doi: 10.1001/jama.1958.02990030008003. [DOI] [PubMed] [Google Scholar]
- 8.Hsueh PR, Liu YC, So J, Liu CY, Yang PC, Luh KT. Mycobacterium tuberculosis in Taiwan. J Infect. 2006;52(2):77–85. doi: 10.1016/j.jinf.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Ishida T, Yokoyama H, Kaneko S, Sugio K, Sugimachi K, Hara N. Pulmonary tuberculoma and indications for surgery: radiographic and clinicopathological analysis. Respir Med. 1992;86(5):431–436. doi: 10.1016/S0954-6111(06)80011-9. [DOI] [PubMed] [Google Scholar]
- 10.Kim IJ, Lee JS, Kim SJ, Kim YK, Jeong YJ, Jun S, Nam HY, Kim JS. Double-phase 18F-FDG PET-CT for determination of pulmonary tuberculoma activity. Eur J Nucl Med Mol Imaging. 2008;35(4):808–814. doi: 10.1007/s00259-007-0585-0. [DOI] [PubMed] [Google Scholar]
- 11.Kim YI, Goo JM, Kim HY, Song JW, Im JG. Coexisting bronchogenic carcinoma and pulmonary tuberculosis in the same lobe: radiologic findings and clinical significance. Korean J Radiol. 2001;2(3):138–144. doi: 10.3348/kjr.2001.2.3.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Luh SP, Liu HP. Video-assisted thoracic surgery—the past, present status and the future. J Zhejiang Univ Sci B. 2006;7(2):118–128. doi: 10.1631/jzus.2006.B0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luh SP, Hsu JD, Lai YS, Chen SW. Primary tuberculous infection of breast: experiences of surgical resection for aged patients and review of literature. J Zhejiang Univ Sci B. 2007;8(8):580–583. doi: 10.1631/jzus.2007.B0580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McAdams HP, Erasmus J, Winter JA. Radiologic manifestations of pulmonary tuberculosis. Radiol Clin North Am. 1995;33(4):655–678. [PubMed] [Google Scholar]
- 15.Mitsudomi T, Kaneko S, Tateishi M, Yano T, Ishida T, Sugimachi K. Benign tumors and tumor-like lesions of the lung. Int Surg. 1990;75(3):155–158. [PubMed] [Google Scholar]
- 16.Park IN, Ryu JS, Shim TS. Evaluation of therapeutic response of tuberculoma using F-18 FDG positron emission tomography. Clin Nucl Med. 2008;33(1):1–3. doi: 10.1097/RLU.0b013e31815c5128. [DOI] [PubMed] [Google Scholar]
- 17.Perel′man MI, Kravtsova IV. Is preoperative chemotherapy necessary in pulmonary tuberculoma? Probl Tuberk. 1989;(11):19–22. (in Russian) [PubMed] [Google Scholar]
- 18.Plachcinska A, Mikolajczak R, Maecke H, Kozak J, Michalski A, Rzeszutek K, Kusmierek J. Efficacy of 99mTc-EDDA/HYNIC-TOC scintigraphy in differential diagnosis of solitary pulmonary nodules. Cancer Biother Radiopharm. 2004;19(5):613–620. doi: 10.1089/cbr.2004.19.613. [DOI] [PubMed] [Google Scholar]
- 19.Porkhanov VA, Poliakov IS, Kononenko VB, Bodnia VN, Merzeria AD, Kovalenko AD, Mamelov M. Videothoracosopy in diagnosis and surgical treatment of tuberculosis. Khirurgiia (Mosk) 2002;(6):14–16. (in Russian) [PubMed] [Google Scholar]
- 20.Prytz S, Hansen JL. Surgical treatment of “tuberculoma”. A follow-up examination of patients with pulmonary tuberculosis resected on suspicion of tumour. Scand J Thorac Cardiovasc Surg. 1976;10(2):179–182. doi: 10.3109/14017437609167789. [DOI] [PubMed] [Google Scholar]
- 21.Schaefer JF, Vollmar J, Wiskirchen J, Erdtmann B, V Renteln D, Vonthein R, Schick F, Claussen CD, Seemann MD. Differentiation between malignant and benign solitary pulmonary nodules with proton density weighted and ECG-gated magnetic resonance imaging. Eur J Med Res. 2006;11(12):527–533. [PubMed] [Google Scholar]
- 22.Tateishi U, Kusumoto M, Akiyama Y, Kishi F, Nishimura M, Moriyama N. Role of contrast-enhanced dynamic CT in the diagnosis of active tuberculoma. Chest. 2002;122(4):1280–1284. doi: 10.1378/chest.122.4.1280. [DOI] [PubMed] [Google Scholar]
- 23.van Dyck P, Vanhoenacker FM, van den Brande P, de Schepper AM. Imaging of pulmonary tuberculosis. Eur Radiol. 2003;13(8):1771–1785. doi: 10.1007/s00330-002-1612-y. [DOI] [PubMed] [Google Scholar]
- 24.WHO (World Health Organization) Global Tuberculosis Control: Surveillance, Planning, Financing; 2008. (Available from: http://www.who.int/tb/publications/global_report/2008/en/index.html) [Google Scholar]