Abstract
In search of associations between coronary artery disease and symptoms of depression and anxiety, we conducted a prospective cross-sectional study of 314 patients (age range, 19–79 yr) who had presented with chest pain. Coronary angiographic findings were classified into 5 categories (0–4), in which higher numbers indicated more severe disease. Symptoms of depression and anxiety were evaluated by the Beck depression and anxiety inventories, in which higher scores indicated more severe symptoms.
Older age, male sex, diabetes mellitus, hypercholesterolemia, and high income were found in association with coronary artery disease. Woman patients exhibited significantly higher depression and anxiety scores (P < 0.001), even though they had coronary artery disease infrequently (P = 0.003). At first, no significant correlation was found between coronary artery disease levels 0, 1, 2, 3, or 4 and scores of depression or anxiety.
After controlling for sex differences and other confounding variables, however, we found that every 1-point increase in the depression score was associated with an average 5% to 6% increase in abnormal coronary angiographic findings or definitive coronary artery disease, respectively (P = 0.01 and P = 0.002). Although there was no such association between anxiety score and coronary artery disease, the highest anxiety scores were encountered in patients with slow coronary flow.
Key words: Angina pectoris; anxiety disorders; chest pain; confounding factors; coronary angiography; coronary disease/epidemiology/etiology; depression/complications; depressive disorder; interview, psychological; psychiatric status rating scales; sex factors; social environment; somatoform disorders; stress, psychological; Turkey/epidemiology
Epidemiologic studies have shown that depression or anxiety disorder can predict the incidence of coronary artery disease (CAD) in healthy populations.1 Moreover, depression or anxiety disorder can also influence the course and prognosis of known CAD.2–4 Although one study reported similar psychological variables in groups of patients with chest pain who had angiographically normal or abnormal coronary arteries,5 several other studies6–9 reported that patients who had chest pain and normal coronary arteries exhibited more psychiatric illnesses than did patients with definitive CAD.
Because we expected that symptoms of depression and anxiety would be associated with CAD in a consecutive population that had been referred for selective coronary angiography, we compared coronary angiographic findings with depression and anxiety scores that had been estimated in accordance with symptom scales. Our findings are discussed herein.
Patients and Methods
Study Population
This prospective, cross-sectional study comprises 1,064 consecutive patients who were referred to Avrupa Safak Hospital from April through May 2006 for coronary angiography to investigate stable angina pectoris or severe chest pain that probably arose from CAD. Slightly more than 60% of these patients came from our institution, and the rest were referred from 6 other hospitals. Our institutional review board approved the study, and we obtained informed consent from all patients.
From the 1,064 referred patients, we enrolled 314 (152 men and 162 women; mean age, 56.26 ± 11.68 yr [range, 19–79 yr]). The inclusion criteria were age greater than 18 years, a coronary angiogram clear enough to enable evaluation of the cause of stress-induced chest pain, and the patient's consent. The exclusion criteria were current pregnancy, cardiomyopathy, previous myocardial infarction or any revascularization procedures (whether percutaneous transluminal coronary angioplasty or coronary artery bypass grafting), unstable angina pectoris, history of congenital heart disease, chronic renal failure, follow-up visits or medical treatment for chronic psychosis, recent medical treatment for depression, insufficient cooperation, and incomplete study forms.
The study population was chiefly from Gaziosmanpasa, most of whose inhabitants migrated within the last century from elsewhere in Turkey (northern, middle, and eastern Anatolia and the Marmara region), and from various Balkan countries. We believe that our sample is a good representation of the Turkish population.
All patients underwent physical examination, coronary angiography, assessment of atherosclerosis risk factors via questionnaire, New York Heart Association (NYHA) functional classification, and a semi-structured psychiatric interview. Atherosclerosis risk factors, as established by the Turkish Society of Cardiology, include older age (>45 yr in men; >55 yr in women, or earlier in the event of premature menopause), family history of atherosclerosis, current smoking, hypertension (>140/90 mmHg or use of antihypertensive drugs), hypercholesterolemia (total cholesterol >200 mg/dL or low-density lipoprotein [LDL] cholesterol >130 mg/dL), high-density lipoprotein (HDL) cholesterol level <35 mg/dL, and diabetes mellitus. All of these coronary risk factors, except for the HDL level, were analyzed in this study sample.
Evaluation of Socioeconomic Status
Two indicators of socioeconomic status were education and annual household income. Patients' levels of education were defined as “less than high school graduation,” “high school graduation,” or “beyond high school.” Economic status was classified according to the following annual household income levels: less than $8,500 (U.S.), between $8,500 and $42,500, and more than $42,500. These 3 values are in accordance with the regional economic and social status of the residents of Gaziosmanpasa, which is the most populous county of Istanbul. We numbered these education and income indices progressively, as 1, 2, and 3.
Psychological Tests
The authors constructed a semi-structured psychiatric interview that began with the Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI). The BDI is a 21-item scale developed by Beck and colleagues10 that is widely used to measure the severity of depression. Each item was scored from 0 to 3, in increasing order of severity. The scores for each of these 21 items were totaled at the end of the psychological evaluation. Accuracy and reliability studies of the BDI have been conducted by Hisli,11 who accepted a score of 17 or above as indicative of major depression in the Turkish population; we accepted this same value as our indicator of major depression. To distinguish patients with depression, Carney and associates12 used a BDI score equal to or greater than 10, which revealed a moderate sensitivity (78%) and specificity (90%). The BAI is applied in a manner similar to that of the BDI. The validity and reliability of the BAI have been studied in the Turkish population by Ulusoy.13 After completion of the symptom scales and tabulation of the results, we performed a clinical psychiatric interview of every patient. This interview was performed before angiography, so neither the psychiatrist nor the patient was aware of the clinical status or angiographic results.
Coronary Angiography
Before diagnostic coronary angiography, all patients underwent stress electrocardiography, myocardial perfusion scintigraphy, or (for high-risk patients) symptomatic assessment. Selective coronary angiography by means of the conventional Judkins technique and left ventriculography were performed in all patients. Each angiogram was interpreted by 2 cardiologists who were not aware of the psychiatric diagnosis. A significant obstructive atherosclerotic lesion was defined as stenosis equal to or greater than 50% of the luminal diameter in 1 or more coronary arteries. Any differences were resolved by a 3rd cardiologist. The coronary angiographic findings were classified into 5 categories in accordance with their severity (Table I). Groups 0 and 1 (normal coronary arteries and noncritical stenosis, respectively)served as controls when patients were regrouped to facilitate statistical analysis. Groups 2, 3, and 4 were also defined in accordance with the simple and widely used system of coronary angiography risk stratificationestablished for the management of stable angina pectoris.14
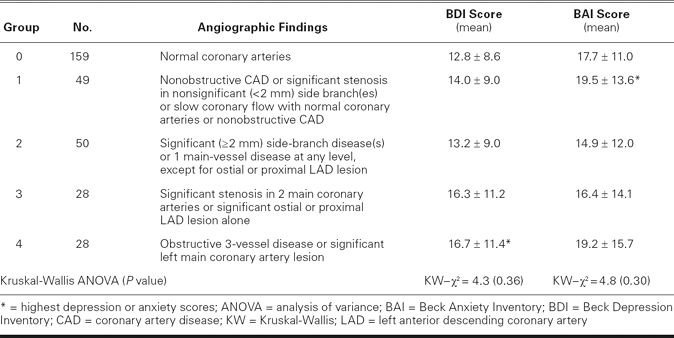
TABLE I. Depression and Anxiety Scores of the Patients
Statistics
Patients' characteristics are summarized as mean ± SD or as percentages; the CAD groups are compared with one another in regard to age by means of Student's t test, in regard to depression and anxiety scores by means of the Mann-Whitney U test or the Kruskal-Wallis test, and in regard to categorical variables by means of the χ2 test. Multivariate logistic regression was processed to control the possible confounding effects of age, sex, varying income and education indices, varying NYHA scores, personal histories of psychiatric visits and treatment for depression or anxiety, and the presence of hypertension, hypercholesterolemia, diabetes mellitus, or smoking. All analyses were performed with SPSS (Statistical Package for the Social Sciences) version 15.0 (SPSS Inc.; Chicago, Ill). Statistical significance was defined as P < 0.05.
Results
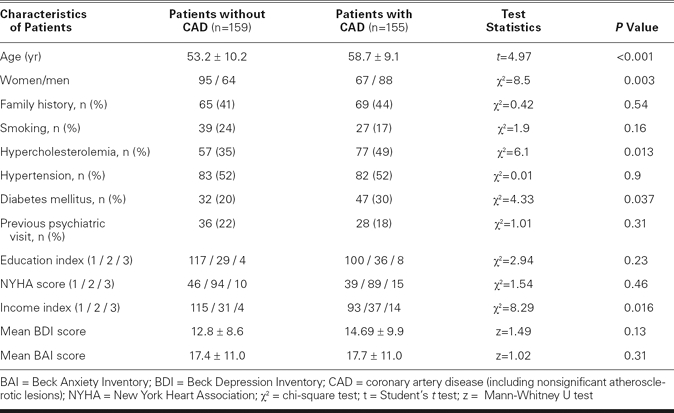
Table II summarizes some of the demographic and clinical characteristics of patients with and without CAD. Our patients with CAD had significantly higher age, higher ratio of male to female, and higher income indices, and an increased prevalence of hypercholesterolemia and diabetes mellitus (P < 0.05). On the other hand, depression and anxiety scores, education indices, NYHA scores, and the prevalence of smoking, hypertension, and family history of atherosclerosis were similar in patients with CAD and without CAD (P > 0.05). Previous psychiatric follow-up for depression or anxiety disorders was documented in 36 patients without CAD and in 28 patients with CAD (P = 0.31).
TABLE II. Patient Characteristics and Clinical Data by Univariate Testing
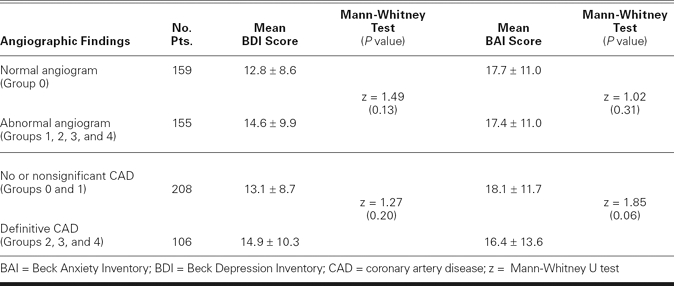
Depression and anxiety scores were similar in the 5 groups of patients (see summaries, Table I). Depression scores had only insignificant increases from Group 0 to Group 1 and from Group 2 to Group 4 (P = 0.36; Kruskal-Wallis analysis of variance). Furthermore, we could not find significant differences in depression or anxiety scores after patients had been regrouped in various ways (P > 0.05; Table III).
TABLE III. Depression and Anxiety Scores of the Patients When Regrouped
Confounding Variables
We came to realize that sex was the chief confounding factor in these analyses. Both depression (15.5 ± 9.4 vs 11.8 ± 8.8; P < 0.0001) and anxiety scores (21.7 ± 12.8 and 13.1 ± 10.1; P < 0.0001) were found to be significantly higher in female patients. On the other hand, female patients were less frequently found to have CAD than were male patients (P = 0.003). In addition, there were confounding factors other than sex: we discovered significant associations (P < 0.05) between depression and anxiety scores and atherosclerosis risk factors such as diabetes mellitus, hypertension, and hypercholesterolemia.
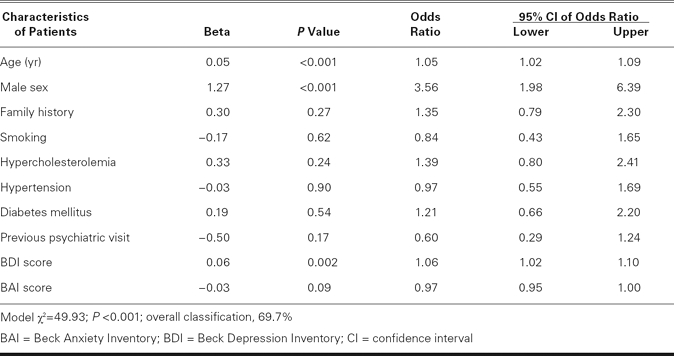
The possible confounding variables discussed above were adjusted during further analyses. After multivariate logistic regression, significant associations were found between depression scores and abnormal coronary angiographic findings or definitive CAD in 2 different analyses (Tables IV and V). A 1-point increase in depression score was associated with an average 5%-to-6% increase in the risk of abnormal coronary angiographic findings or definitive CAD (P = 0.01 and P = 0.002). In contrast, there was no association between anxiety score and coronary angiographic findings. However, the highest BAI score was found in Group 1, which comprised patients with slow coronary flow, nonobstructive CAD, or both (Table I).
TABLE IV. Results of Multivariate Logistic Regression Analysis of Coronary Artery Disease as a Dependent Variable (Group 0 vs Groups 1, 2, 3, and 4)
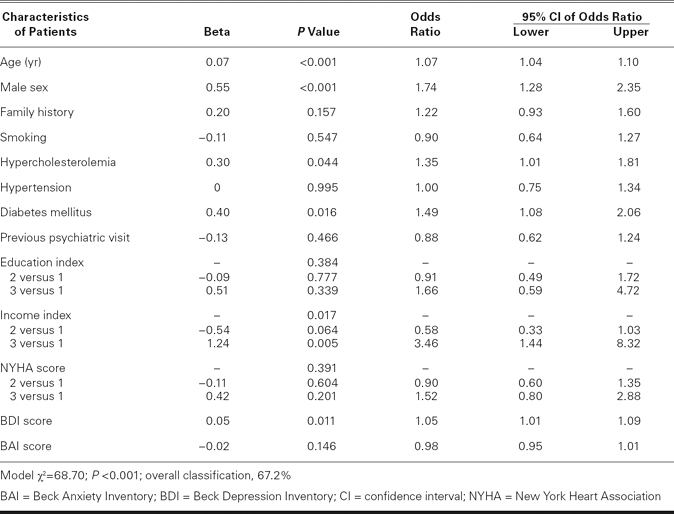
TABLE V. Results of Multivariate Logistic Regression Analysis of Coronary Artery Disease as a Dependent Variable (Groups 0 and 1 vs Groups 2, 3, and 4)
Discussion
Several investigators have considered possible associations between psychological variables and CAD in patients who have undergone coronary angiography, and the results have been conflicting.5–9,15,16 In our study, the depression score in patients who had CAD was at first not significantly different from the depression score in patients who did not have CAD. However, the paradoxical effect of female sex was chiefly responsible for this finding; after controlling for sex and other variables, we found that the depression score was strongly correlated to CAD in our sample. We estimated that every 5-point increase in depression score was associated with a 25%-to-30% increase, on average, in the risk of abnormal coronary angiography findings or definitive CAD.
The associations between CAD and the factors of age, sex, diabetes mellitus or hypercholesterolemia or both, and higher ratio of men to women are not unique to our patients: they can be found elsewhere in the medical literature. The association that we found between CAD and high income level could be coincidental and needs further evaluation. Another interesting finding was the similarity in the NYHA scores of our patients with and without CAD. We speculate that sociocultural factors—agoraphobia, social isolation, and a sedentary life style induced by moderate depression or higher anxiety—could have contributed to the poor physical condition of patients who did not have CAD.
It is known that patients with stable angina pectoris and normal coronary angiography usually have cardiac “syndrome X.” We think it likely that most of our patients in Groups 0 and 1 had syndrome X. In our sample, patients with slow coronary flow (Group 1) had the highest anxiety score. Slow coronary flow has been identified as a definite subset within the wide spectrum of syndrome X and can be used as a marker for myocardial ischemia.17 In another study, Ketterer and coworkers18 showed that syndrome X patients might be more emotionally distressed than healthy controls, indeed as distressed as patients with CAD. In the present study, patients with slow coronary flow also had unexpectedly higher depression symptoms.
We observe that the indications for coronary angiography among our patients arose largely from symptomatic assessment, and that chest pain was chief among these symptoms. Chest pain, we should point out, can also be a symptom of panic disorder, depression, hypochondriasis, somatization disorder, and generalized anxiety disorder.19,20 We should also emphasize the importance of diagnosis, treatment, and follow-up of depression and anxiety disorder in order to prevent unnecessary diagnostic cardiac catheterization, long before these conditions can result in CAD. In fact, 50.6% of our patients had normal coronary angiographic results. On the other hand, we thought that the symptomatic assessment of our patients increased the strength of our study by providing a balanced population. In this manner, we avoided the spectrum bias inherent in a population skewed toward severe or late-stage disease.21
Several hypotheses have been proposed to explain the association between symptoms of depression and anxiety and CAD: increased platelet reactivity, endothelial dysfunction, decreased variability in heart rate, accelerated atherogenesis, and poor adherence to therapies.22,23 Symptoms of depression and anxiety have also been associated with atherosclerosis risk factors.24–27 We have also shown, in a previous study, 28 that diabetes mellitus, hypertension, and hypercholesterolemia, which are known to be causally related to CAD, were associated with depression and anxiety symptoms in the same sample. These findings are compatible with the results of our present study. We believe that depression and anxiety symptoms can interact with major atherosclerosis risk factors in many complicated and long-term processes, at present mostly undefined, in the development of CAD.
Limitations
By its nature, a cross-sectional study cannot show a definite causal relationship between CAD and depression or anxiety disorder. However, we think that our findings are clinically relevant because we also showed, in the same sample. some associations between atherosclerosis risk factors and symptoms of depression and anxiety. We classified coronary angiographic findings into 5 categories for the sake of simplicity. The final 3 subclasses (Groups 2, 3, and 4) were in general compatible with coronary angiographic risk stratifications used in well-known guidelines14 and clinical trials,29 but we defined them slightly differently. For control, we used Group 0 patients (normal coronary arteries) either by themselves or in combination with Group 1 patients (nonobstructive atherosclerotic lesions or slow coronary flow or both).
Conclusions
Our sample shows some correlations between depression score and abnormal coronary angiographic findings, definitive CAD, or both. Patients with higher depression scores (estimated before the procedure) had a significantly increased risk of abnormal coronary angiographic findings or definitive CAD. This is compatible with our previous report in which depression and anxiety symptoms were associated with major atherosclerosis risk factors in the same sample. Anxiety symptoms were found to be extreme only in patients with slow coronary flow. Future research with better study designs is needed for definitive conclusions.
Footnotes
Address for reprints: Dr. Mutlu Vural, Bayar cad. Pinar sok. Catalpinar sitesi, B blok 8/27 Kozyatagi, 34742 Kadikoy, Istanbul, Turkey. E-mail: heppikalp@yahoo.com
*Licensed Clinical Psychologist
References
- 1.Ferketich AK, Schwartzbaum JA, Frid DJ, Moeschberger ML. Depression as an antecedent to heart disease among women and men in the NHANES I study. National Health and Nutrition Examination Survey. Arch Intern Med 2000;160(9): 1261–8. [DOI] [PubMed]
- 2.Ariyo AA, Haan M, Tangen CM, Rutledge JC, Cushman M, Dobs A, Furberg CD. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Cardiovascular Health Study Collaborative Research Group. Circulation 2000;102(15):1773–9. [DOI] [PubMed]
- 3.Smith TW, Ruiz JM. Psychosocial influences on the development and course of coronary heart disease: current status and implications for research and practice. J Consult Clin Psychol 2002;70(3):548–68. [DOI] [PubMed]
- 4.Tennant C, McLean L. The impact of emotions on coronary heart disease risk. J Cardiovasc Risk 2001;8(3):175–83. [DOI] [PubMed]
- 5.Valkamo M, Hintikka J, Niskanen L, Viinamaki H. Psychiatric morbidity and the presence and absence of angiographic coronary disease in patients with chest pain. Acta Psychiatr Scand 2001;104(5):391–6. [DOI] [PubMed]
- 6.Katon W, Hall ML, Russo J, Cormier L, Hollifield M, Vitaliano PP, Beitman BD. Chest pain: relationship of psychiatric illness to coronary arteriographic results. Am J Med 1988;84 (1):1–9. [DOI] [PubMed]
- 7.Cormier LE, Katon W, Russo J, Hollifield M, Hall ML, Vitaliano PP. Chest pain with negative cardiac diagnostic studies. Relationship to psychiatric illness. J Nerv Ment Dis 1988;176 (6):351–8. [DOI] [PubMed]
- 8.Beitman BD, Mukerji V, Lamberti JW, Schmid L, DeRosear L, Kushner M, et al. Panic disorder in patients with chest pain and angiographically normal coronary arteries. Am J Cardiol 1989;63(18):1399–403. [DOI] [PubMed]
- 9.Carney RM, Freedland KE, Ludbrook PA, Saunders RD, Jaffe AS. Major depression, panic disorder, and mitral valve prolapse in patients who complain of chest pain. Am J Med 1990;89(6):757–60. [DOI] [PubMed]
- 10.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561–71. [DOI] [PubMed]
- 11.Hisli N. Validity and accuracy of Beck depression inventory among university students [in Turkish]. Psikoloji Dergisi 1989;7:3–13.
- 12.Carney RM, Rich MW, Tevelde A, Saini J, Clark K, Jaffe AS. Major depressive disorder in coronary artery disease. Am J Cardiol 1987;60(16):1273–5. [DOI] [PubMed]
- 13.Ulusoy M, Sahin NH, Erkmen H. Turkish version of the Beck Anxiety Inventory: psychometric properties. J Cogn Psycother Int Q 1998;12:163–72.
- 14.Fox K, Garcia MA, Ardissino D, Buszman P, Camici PG, Crea F, et al. Guidelines on the management of stable angina pectoris: executive summary: the Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. Eur Heart J 2006;27(11):1341–81. [DOI] [PubMed]
- 15.Kane FJ Jr, Harper RG, Wittels E. Angina as a symptom of psychiatric illness. South Med J 1988;81(11):1412–6. [DOI] [PubMed]
- 16.Beitman BD, Basha I, Flaker G, DeRosear L, Mukerji V, Trombka L, Katon W. Atypical or nonanginal chest pain. Panic disorder or coronary artery disease? Arch Intern Med 1987;147(9):1548–52. [PubMed]
- 17.Goel PK, Gupta SK, Agarwal A, Kapoor A. Slow coronary flow: a distinct angiographic subgroup in syndrome X. Angiology 2001;52(8):507–14. [DOI] [PubMed]
- 18.Ketterer MW, Brymer J, Rhoads K, Kraft P, Kenyon L, Foley B, et al. Emotional distress among males with “syndrome X”. J Behav Med 1996;19(5):455–66. [DOI] [PubMed]
- 19.Potts SG, Bass CM. Psychological morbidity in patients with chest pain and normal or near-normal coronary arteries: a long-term follow-up study. Psychol Med 1995;25(2):339–47. [DOI] [PubMed]
- 20.Richter JE, Bradley LA. Chest pain with normal coronary arteries. Another perspective. Dig Dis Sci 1990;35(12):1441–4. [DOI] [PubMed]
- 21.Pickering TG. Should studies of patients undergoing coronary angiography be used to evaluate the role of behavioral risk factors for coronary heart disease? J Behav Med 1985;8(3): 203–13. [DOI] [PubMed]
- 22.Appels A. Depression and coronary heart disease: observations and questions. J Psychosom Res 1997;43(5):443–52. [DOI] [PubMed]
- 23.Vural M, Basar E. Impact of psychological factors on development and course of coronary heart disease: should negative psychological factors be altered? [in Turkish]. Anadolu Kardiyol Derg 2006;6(1):55–9. [PubMed]
- 24.Rutledge T, Reis SE, Olson M, Owens J, Kelsey SF, Pepine CJ, et al. Psychosocial variables are associated with atherosclerosis risk factors among women with chest pain: the WISE study. Psychosom Med 2001;63(2):282–8. [DOI] [PubMed]
- 25.Gulseren L, Hekimsoy Z, Gulseren S, Bodur Z, Kultur S. Depression-anxiety, quality of life, and disability in patients with diabetes mellitus. Turkish Psikiyatri Dergisi 2001;12(2): 89–98.
- 26.Kaplan MS, Nunes A. The psychosocial determinants of hypertension. Nutr Metab Cardiovasc Dis 2003;13(1):52–9. [DOI] [PubMed]
- 27.Papakostas GI, Petersen T, Sonawalla SB, Merens W, Iosifescu DV, Alpert JE, et al. Serum cholesterol in treatment-resistant depression. Neuropsychobiology 2003;47(3):146–51. [DOI] [PubMed]
- 28.Vural M, Satiroglu O, Akbas B, Goksel I, Karabay O. Association between depression and anxiety symptoms and major atherosclerosis risk factors in patients with chest pain. Tohoku J Exp Med 2007;212(2):169–75. [DOI] [PubMed]
- 29.Emond M, Mock MB, Davis KB, Fisher LD, Holmes DR Jr, Chaitman BR, et al. Long-term survival of medically treated patients in the Coronary Artery Surgery Study (CASS) Registry. Circulation 1994;90(6):2645–57. [DOI] [PubMed]


