Abstract
Myocardial infarction complicates approximately 1 in 10,000 pregnancies. Although coronary artery dissection is the leading cause of pregnancy-related myocardial infarction during the postpartum period, the pathogenesis of coronary dissection during this period remains uncertain.
Herein, we report the case of a 52-year-old black postmenopausal woman with no apparent cardiovascular risk factors who gave birth to twins after in vitro fertilization. Ten days after delivery, she presented with an acute coronary syndrome. Coronary angiography revealed dissection of all 3 coronary arteries. Despite aggressive medical management, the patient experienced recurrent myocardial ischemia. Repeat coronary angiography revealed progression of the dissection process, which required urgent coronary artery bypass surgery. The patient's postoperative course was uneventful. To our knowledge, this report is the 1st description of pregnancy-associated coronary artery dissections in a postmenopausal woman, and the 1st such event in a pregnancy that resulted from in vitro fertilization.
Key words: Chest pain/etiology; fertilization in vitro; myocardial infarction/complications; maternal age; postpartum period; pregnancy, high-risk; pregnancy complications, cardiovascular/diagnosis/etiology/radiography/therapy; postmenopause; puerperal disorders/complications/etiology/surgery; risk factors; rupture, spontaneous
Myocardial infarction complicates approximately 1 in 10,000 pregnancies.1 Coronary artery dissection is the leading cause of pregnancy-related myocardial infarction during the postpartum period.2 The pathogenesis of coronary dissection during this period remains uncertain. Hormonal factors may directly affect the coronary vasculature and confer vulnerability to the vascular walls, which are exposed to the increased hemodynamic stress of the pregnancy. Advanced maternal age has also been linked with this cardiovascular complication.3 Here, we report the postpartal dissection of all 3 coronary arteries in an in vitro-fertilized, 52-year-old postmenopausal woman who, after giving birth to twins by cesarean section, presented with myocardial infarction and required urgent coronary artery bypass surgery. To our knowledge, this is the 1st description of pregnancy-associated coronary artery dissections in a postmenopausal woman, and the 1st such reported event in a pregnancy that resulted from in vitro fertilization.
Case Report
A 52-year-old black postmenopausal woman (gravida 2, para 1) conceived after in vitro fertilization and gave birth to twins via emergency cesarean section in her 34th week of pregnancy. From the 26th week of gestation, she had undergone tocolysis with oral nifedipine and subsequently with intravenous magnesium sulfate. There was nothing unusual in her medical history, and no cardiovascular risk factors were identified. The delivery was uneventful. Ten days postpartum, the woman was admitted to the hospital with a diagnosis of acute inferior myocardial infarction. Electrocardiography revealed ST-segment elevation in leads II, III, and aVF, and cardiac markers were substantially elevated.
Immediate coronary angiography revealed dissections of all 3 coronary arteries. The right coronary artery (RCA) was affected in its proximal portion (Fig. 1A). A dissection line that extended from the left main trunk to the diagonal branch was seen, the lumen of the entire left anterior descending coronary artery (LAD) was narrowed, and involvement of the left circumflex coronary artery (LCx) was evident at the level of the 1st marginal branch (Fig. 1B). The angiographic appearance of the other coronary segments was smooth, suggesting the absence of atherosclerotic coronary disease. Left ventricular function was preserved (ejection fraction, 0.69), with no segmental wall-motion abnormalities. On the basis of the preserved coronary flow in all segments and the absence of symptoms at the time of cardiac catheterization, the patient was treated conservatively. In addition to β-blockers, calcium antagonists, and nitrates, she was given combined antithrombotic therapy of aspirin, clopidogrel, and full-dose unfractionated heparin. Due to residual vaginal blood loss, no platelet glycoprotein IIb/IIIa receptor antagonist was administered.
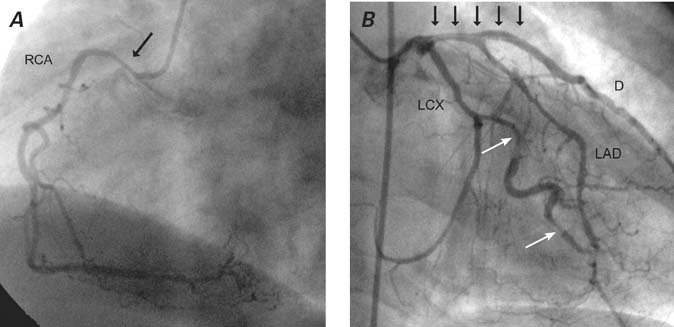
Fig. 1 Coronary angiography shows A) the right coronary artery (RCA) affected in its proximal portion (arrow), and B) a dissection line (black arrows) that extends from the left main trunk to the diagonal branch (D), with narrowing of the lumen of the entire left anterior descending coronary artery (LAD) and involvement of the left circumflex coronary artery (LCX) at the level of the 1st marginal branch (white arrows).
Despite aggressive medical treatment, the patient experienced recurrent chest pain 2 days after the catheterization. Repeat coronary angiography revealed a severe progression of the dissections in the left coronary circulation, now causing total occlusion of the middle LAD (Fig. 2). The angiographic appearance of the LCx and RCA was unchanged. After the placement of an intra-aortic balloon pump to improve coronary perfusion, the patient immediately underwent coronary artery bypass surgery. Her postoperative course was uneventful.

Fig. 2 Coronary angiography shows that the severe progression of dissections in the left coronary circulation caused total occlusion of the middle left anterior descending coronary artery (arrow).
Discussion
Pregnancy-related myocardial infarction is rare, occurring in 1 of every 10,000 pregnancies.1 In the postpartum period, most myocardial infarctions are due to coronary dissections,2 all reports of which have involved premenopausal women. To our knowledge, our case report is unique in 2 distinct aspects. It is the 1st report of postpartum coronary artery dissection in a patient of any age who was fertilized in vitro. Moreover, it is the 1st reported pregnancy-related dissection in a postmenopausal woman.
Pregnancy-associated coronary artery dissections may have a mortality rate as high as 50%.4 Patients who survive the acute phase generally have a good long-term prognosis.4 The coronary vessel most frequently involved is the LAD (78%). Dissections of the left main trunk have been reported in approximately 25% of cases. In up to 40% of cases, dissection may involve multiple coronary vessels, as it did in our patient.3
The cause of pregnancy-associated coronary dissection remains unclear. Approximately one third of patients possess 1 or more conventional risk factors for coronary artery disease.3 Putative mechanisms include pregnancy-induced degeneration of connective tissue, hemodynamic stress (particularly at the time of delivery), primary rupture of the vasa vasorum, and medial eosinophilic angiitis. Advanced maternal age also appears to be a risk factor for coronary artery dissection in pregnancy.3
The optimal management approach for spontaneous coronary artery dissection has not yet been defined. In the presence of ongoing myocardial ischemia, the recommendations are to administer aspirin, unfractionated heparin, β-blockers, and nitroglycerin, and to perform immediate coronary angiography. In accordance with the patient's coronary anatomy and response to medical management, therapy options range from a conservative approach to percutaneous coronary intervention or coronary artery bypass surgery. Because percutaneous and surgical revascularizations may be very challenging in the presence of coronary dissections, and because complete healing has resulted after a conservative approach,3 medical management should be considered the 1st-line treatment in the absence of ongoing ischemia.
The choice of a percutaneous5 or surgical approach6 depends on the severity of the coronary involvement, impairment of left ventricular function, and associated comorbidities. The high mortality rate that accompanies bypass surgery is due in part to the complexity of the operation.6 Rarely, spontaneous coronary artery dissection can require cardiac transplantation.7,8 A review of the medical literature revealed reports of 3 patients who experienced pregnancy-associated dissections of all coronary arteries.7,9,10 Two of these patients were treated conservatively. In one, 6-month follow-up coronary angiography revealed complete healing of the dissections in the RCA and LCx and of an aneurysmal formation in the LAD, with no signs of ischemia upon stress-testing.9 The 2nd patient developed angina and heart failure.10 The 3rd patient required heart transplantation because of persistent cardiogenic shock.7
In vitro-fertilization pregnancies in women of advanced maternal age are increasing in number. Further studies are required to determine the degree of risk that these pregnancies confer in regard to the potentially catastrophic complication of spontaneous coronary artery dissection.
Footnotes
Address for reprints: Bilgehan Karadag, MD, Division of Cardiology, Cerrahpasa School of Medicine, Istanbul University, 34098 Istanbul, Turkey. E-mail: karadag@istanbul.edu.tr
References
- 1.Mabie WC, Freire CM. Sudden chest pain and cardiac emergencies in the obstetric patient. Obstet Gynecol Clin North Am 1995;22(1):19–37. [PubMed]
- 2.Roth A, Elkayam U. Acute myocardial infarction associated with pregnancy. Ann Intern Med 1996;125(9):751–62. [DOI] [PubMed]
- 3.Koul AK, Hollander G, Moskovits N, Frankel R, Herrera L, Shani J. Coronary artery dissection during pregnancy and the postpartum period: two case reports and review of literature. Catheter Cardiovasc Interv 2001;52(1):88–94. [DOI] [PubMed]
- 4.DeMaio SJ Jr, Kinsella SH, Silverman ME. Clinical course and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol 1989;64(8):471–4. [DOI] [PubMed]
- 5.Madu EC, Kosinski DJ, Wilson WR, Burket MW, Fraker TD Jr, Ansel GM. Two-vessel coronary artery dissection in the peripartum period. Case report and literature review. Angiology 1994;45(9):809–16. [DOI] [PubMed]
- 6.Elming H, Kober L. Spontaneous coronary artery dissection. Case report and literature review. Scand Cardiovasc J 1999; 33(3):175–9. [DOI] [PubMed]
- 7.Mather PJ, Hansen CL, Goldman B, Inniss S, Pina I, Norris R, et al. Postpartum multivessel coronary dissection. J Heart Lung Transplant 1994;13(3):533–7. [PubMed]
- 8.Curiel P, Spinelli G, Petrella A, Gori A, De Maria R, Bonacina E, Gronda E. Postpartum coronary artery dissection followed by heart transplantation. Am J Obstet Gynecol 1990; 163(2):538–9. [DOI] [PubMed]
- 9.Rensing BJ, Kofflard M, van den Brand MJ, Foley DP. Spontaneous dissections of all three coronary arteries in a 33-week-pregnant woman. Catheter Cardiovasc Interv 1999; 48(2):207–10. [DOI] [PubMed]
- 10.Verkaaik AP, Visser W, Deckers JW, Lotgering FK. Multiple coronary artery dissections in a woman at term. Br J Anaesth 1993;71(2):301–2. [DOI] [PubMed]


