Abstract
Plasmodium berghei ANKA (PbA) infection in susceptible inbred mouse strains is the most commonly used experimental model to study pathogenesis of cerebral malaria (CM). Indeed, many concepts on mechanisms related to this complication have arisen from works using this model. Although inbred strains present several advantages and are indicated for most studies, the use of outbred models can show unique usefulness in a number of approaches such as fine post-quantitative trait loci mapping and discovery of genes relevant to CM susceptibility or resistance, as well as pharmacological and vaccine studies. Here we describe the features of PbA infection and CM incidence, and characterize the associated multiorgan pathology in the outbred Swiss Webster mouse. This model showed a sizeable (62.7%) and reproducible incidence of CM demonstrated by clinical signs and histopathological changes in brain (microhaemorrhages, oedema and vessel plugging by mononuclear cells). Major pathological changes were also observed in lungs, liver, thymus and spleen, analogous to those observed in inbred strains. Parasitaemia levels were associated with the risk of CM development, the risk being significantly higher in mice showing higher values of parasitaemia on days 6–7 of infection. This outbred CM model is then suitable for genetic, vaccine and drug studies targeting this malaria complication.
Keywords: cerebral malaria, histopathology, murine models, Plasmodium berghei ANKA, Swiss Webster
Plasmodium falciparum infections in humans can lead to a range of clinical manifestations including deadly complications claiming more than 1 million lives every year, especially under-5-year-old children in sub-Saharan Africa. The most frequent complications are severe malarial anaemia and cerebral malaria (CM), the latter defined as unrousable coma not attributable to other causes in patients with P. falciparum infection (Molyneux et al. 1989). Postmortem analysis reveals brain microhaemorrhages and vessel occlusion by adherent parasitized red blood cells (pRBC) (Pongponratn et al. 1991) and, to some extent, by leucocytes (Patnaik et al. 1994), suggesting a role for ischaemia and hypoxia in CM. However, the mechanisms underlying CM pathogenesis are far from being well understood.
Many concepts about the pathogenesis of CM have arisen from studies in murine models. The most commonly used mouse model of CM is Plasmodium berghei ANKA (PbA) infection in susceptible inbred mouse strains including CBA and C57BL/6 (Rest 1982; Grau et al. 1986; Neill & Hunt 1992). The PbA-infected susceptible mice develop a lethal neurological syndrome occurring 6–12 days after infection with a cumulative incidence of 50–100%. Some other strains are weakly susceptible, with lower incidence (Balb/c), or resistant (DBA/2), to CM (Lou et al. 2001; Bagot et al. 2002a,b). Cerebral pathology in mice developing CM includes microhaemorrhages and vessel obstruction mostly by activated monocytes (Lou et al. 2001) and, less prominently, pRBC (Hearn et al. 2000). CM in this model results from an extraordinary inflammatory response, and a number of key players and mediators such as T cells (Hunt & Grau 2003; Nitcheu et al. 2003), monocytes (Carvalho et al. 2000) and their derived cytokines (Clark & Rockett 1994), platelets (Lou et al. 1997), nitric oxide (Gramaglia et al. 2006) and carbon monoxide (Pamplona et al. 2007), among others, have been described as playing pathological or protective roles in the syndrome. Although considerable advance has been achieved with these models, there is still a long way until a comprehensive knowledge of CM pathogenesis is attained and potentially transferred to the human situation, allowing the development of more effective prophylactic, therapeutic or adjunctive therapies. A major difficulty resides in the complex, multifactorial nature of this complication, the ultimate outcome being affected by factors related to the host (Lovegrove et al. 2006,2007), the parasite and the environment (Fortin et al. 2002; Good et al. 2005).
The existence of CM susceptible and resistant strains of mice shows that the genetic makeup is central in determining the outcome of infection. Given the complex nature of CM, it is likely that several genes and regulators, functioning as discrete traits, contribute to the final susceptibility status of any given host. Susceptibility to CM is not determined by the H-2 haplotype (Bagot et al. 2002a,b). On the other hand, two loci were found to be associated with resistance to CM in genetic studies using a cross between susceptible C57Bl/6 and resistant WLA inbred mice (Bagot et al. 2002a,b). Quantitative trait loci (QTL) mapping resolution, however, rarely goes beyond chromosome regions and narrowing the QTL to a small number of candidate genes is extremely difficult (Flint et al. 2005; Wu & Lin 2006). This limitation has been overcome with the use of outbred stocks of mice combined with a number of genetic resources, which led for instance to the identification of the gene Rgs2 as modulating anxiety in mice (Yalcin et al. 2004). The availability of a well characterized outbred model for CM can then be a useful resource for the location and identification of QTLs and genes influencing susceptibility to this deadly complication of malaria infection. In addition, although subjected to criticism (Chia et al. 2005), there are several other approaches in biomedical research where outbred mice are commonly used such as pharmacological and toxicological studies and evaluation of new vaccines and drugs, which are expected to be effective in populations of different genetic backgrounds.
The outbred Swiss mouse has long been used in experimental malaria studies, but reports of its use in CM studies are scarce (Gupta et al. 1988; Kaul et al. 1994; Franke-Fayard et al. 2005) and description of PbA infection in this mouse stock lacks details on the course of infection, CM incidence and histopathological alterations. In this study, we describe the occurrence of CM in the outbred Swiss Webster mouse and characterize the associated multiorgan pathology by histology. We focused on the brain, liver and lungs, known to be severely affected during PbA infection in other mouse strains (Rest 1982; Carvalho et al. 2000) and on lymphoid organs, which act both as targets and as players in CM pathogenesis (Urban et al. 2005; Carvalho et al. 2006,2007).
Materials and methods
Mice
Five- to eight-week-old female Swiss Webster and CBA mice were obtained from CECAL/Fiocruz (Rio de Janeiro, Brazil). All mice were bred under specific pathogen-free (SPF) conditions and housed in groups of five maximum, in plastic cages with autoclaved sawdust bedding. The mice received autoclaved food (Nuvital, Brazil) and filtered and autoclaved water ad libitum, refreshed every 2 days. All experimental protocols were reviewed and approved by the Fiocruz Ethics Committee on Animal Use (license number P-0155-03).
Parasite and infection
Plasmodium berghei ANKA strain was maintained in Alsever's solution in liquid nitrogen until use. The sample was thawed and 100 μl of the sample was injected intraperitoneally (i.p.) into a donor mouse of the same age and sex as the experimental mice. A few days later, blood was collected and 1 × 106 pRBC were inoculated i.p. in each animal of the experimental groups. Thin blood smears were daily made with a blood drop collected from the tip of the tail, stained according to the Panoptic method (Laborclin, Brazil) and examined under a light microscope (BH2, Olympus: Melville, New York, USA) with an oil immersion lens (1000× final magnification). Parasitaemia was determined by counting the number of pRBC in 2000 RBC.
Experimental design and histopathology
A total of 59 Swiss Webster (51 infected and eight controls) mice were used in four separate experiments. As a positive control for clinical CM development and comparative histological analysis, the inbred CBA strain was used (35 mice – 29 infected and six controls). In the first two experiments, groups of Swiss Webster and CBA mice were inoculated and the course of parasitaemia and clinical CM expression (defined as the presentation of neurological disorders like roll over, convulsions, limb paralysis or coma) were evaluated, with the determination of CM incidence and survival curve. After that, two other experiments were conducted where groups of mice were inoculated and nine Swiss Webster as well as nine CBA mice presenting clinical CM on days 6–9 of infection were anaesthetized (ketamine 150 mg/kg; xylazine 10 mg/kg) and exsanguination was performed by the dissection of the axillary artery. Organs (brain, lungs, liver, thymus, spleen and lymph nodes) were carefully collected and fixed in Millonig's buffered formalin pH 7.4 until processed for histology. After fixation, organs were cleaved, embedded in paraffin, cut into tissue sections of 3 or 5 μm, deparaffinized and hydrated before staining. All the material was stained with haematoxylin–eosin (HE) and Lennert's Giemsa. The histology slides were analysed with a light microscope (BH2, Olympus). Pictures were made with a photomicroscope III (Zeiss, Jena, Germany) and a CCD camera Hamamatsu C5810 (1014 × 721 pixels). Microsoft Photoeditor was used to edit the pictures.
Statistical analyses
The chi-square test was used to compare the cumulative incidence of CM between the Swiss Webster stock and CBA strain. The non-parametric log-rank test was used to evaluate the equality of the survival curves between the two strains (Bland & Altman 2004). The results of parasitaemia and survival were expressed as means and standard errors of the mean (SEM) and the Mann–Whitney test was used to compare the values of parasitaemia on days 2–10 between CM and non-CM mice in the Swiss Webster stock and the CBA strain. A univariate Cox proportional hazard regression, a semi-parametric model, was used to assess if the values of parasitaemia on days 2–10 predict the risk of CM. A P-value of less than 0.05 was considered to indicate statistical significance of results. All statistical analyses were performed using Stata 9.0.
Results
CM development
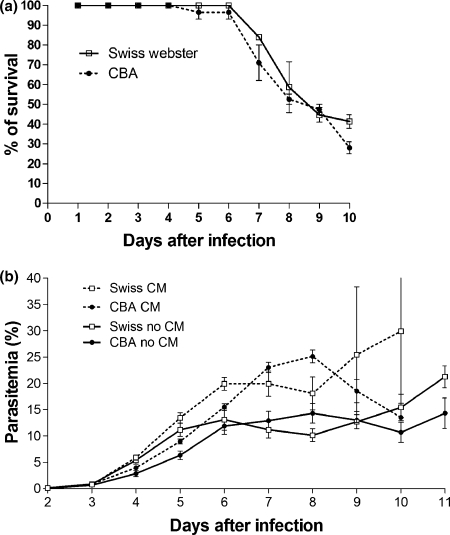
Inoculation of P. berghei ANKA to Swiss Webster and CBA mice resulted in a lethal infection with a 100% cumulative risk of death on day 17. Both Swiss Webster and CBA mice displayed, on days 5–10 of infection, clinical signs of CM including ataxia, disorientation, paraplegia, roll-over and coma. These mice died shortly thereafter, usually within a few hours. The cumulative incidence of clinical CM was 62.7% in the Swiss Webster mice and 67.1% in the CBA. The remaining surviving mice although not affected by CM, died later on days 12–17 by other malaria-related pathologies (hyperparasitaemia, severe anaemia). There was no difference in the survival curves between the two strains (P > 0.5; Figure 1a).
Figure 1.
Survival curve (a) and course of parasitaemia (b) of Swiss Webster and CBA mice infected with 1 × 106Plasmodium berghei ANKA-parasitized red blood cells. CM, mice with cerebral malaria; no-CM, mice that did not develop cerebral malaria. Results are expressed as means ± SEM.
Course of parasitaemia
Parasitaemia was first detected three days after infection and grew rapidly for all infected mice up to day 5 of infection. The behaviour of parasitaemia in the subsequent days was critical for the outcome in terms of CM development. Indeed, parasitaemia in the Swiss Webster mice with CM on days 6–8 was significantly higher as compared with those without CM (P < 0.01 in all time points). The same was true for CBA mice on days 4–8 (P < 0.05 on days 4–6; P < 0.001 on days 7–8) (Figure 1b). No significant differences in parasitaemia between CM and non-CM mice were observed in the other days of the follow-up.
A summary of the univariate Cox proportional hazard regression is shown in Table 1. When considering only the Swiss Webster stock, data strongly indicate that the value of parasitaemia of each mouse on days 6–7 is associated with the risk of CM development. The results were similar for the CBA strain on days 6–8 of infection (Table 1). One example of the associative strength of the hazard ratio for parasitaemia was observed for Swiss Webster stock on day 6 (1.104), when an increase of the value of parasitaemia by one unit raised the risk of CM development by 10.4% (Table 1).
Table 1.
Univariate Cox proportional hazard regression used to assess if the values of parasitaemia on days 2–10 of infection predict the risk of CM development in Swiss Webster stock, CBA strain and both groups pooled (Swiss Webster and CBA)
| Swiss Webster |
CBA |
Swiss Webster and CBA |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Days postinfection | HR | P-value | 95% CI | HR | P-value | 95% CI | HR | P-value | 95% CI |
| 2 | 0.204 | 0.507 | 0.017–2.364 | 0.120 | 0.522 | 0.0001–96.8 | 0.186 | 0.351 | 0.005–6.870 |
| 3 | 0.804 | 0.656 | 0.308–2.098 | 1.219 | 0.541 | 0.649–2.289 | 1.077 | 0.786 | 0.627–1.851 |
| 4 | 1.057 | 0.455 | 0.913–1.224 | 1.155 | 0.107 | 0.970–1.376 | 1.069 | 0.185 | 0.969–1.180 |
| 5 | 1.130 | 0.056 | 0.986–1.296 | 1.137 | 0.134 | 1.021–1.268 | 1.084 | 0.012 | 1.016–1.158 |
| 6 | 1.104 | 0.005 | 1.027–1.187 | 1.072 | 0.046 | 1.000–1.149 | 1.082 | 0.0009 | 1.033–1.134 |
| 7 | 1.088 | 0.007 | 1.021–1.158 | 1.127 | <0.0001 | 1.057–1.202 | 1.107 | <0.0001 | 1.060–1.156 |
| 8 | 1.047 | 0.094 | 0.997–1.100 | 1.133 | 0.0004 | 1.047–1.226 | 1.070 | 0.0007 | 1.030–1.111 |
| 9 | 1.060 | 0.127 | 0.993–1.133 | 1.079 | 0.186 | 0963–1.210 | 1.059 | 0.054 | 1.007–1.114 |
| 10 | 1.088 | 0.133 | 0.974–1.216 | 1.067 | 0.680 | 0.775–1.469 | 1.081 | 0.103 | 0.991–1.179 |
HR, Hazard Ratio; 95% CI, 95% Confidence Interval for the Hazard Ratio.
Histopathology
Brain
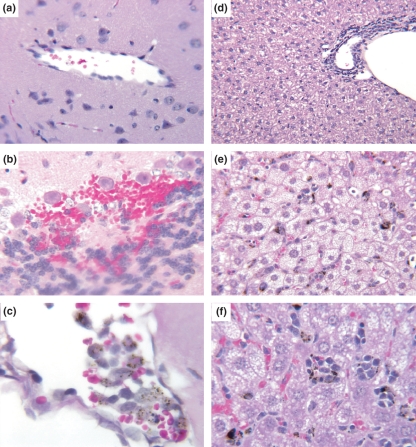
Uninfected control mice showed characteristic brain histology without any sign of abnormal features such as haemorrhages, oedema or intravascular cell adhesion (Figure 2a).The brain of infected Swiss Webster mice with clinical CM showed alterations characteristic of CM, particularly micro- and perivascular haemorrhages especially in areas such as the cerebellum. Large subarachnoid and cerebellar haemorrhages were also eventually observed (Figure 2b). This was in accordance with the presence of haemorrhages seen on the brain surface by macroscopical examination. Perivascular oedema was frequently observed. Brain (including cerebral and cerebellar) vessels contained both pigmented and non-pigmented mononuclear cells. The majority of the mononuclear cells were monocytes containing malaria pigment in their cytoplasm. These monocytes were activated, showing adherence to each other, to the endothelium and to erythrocytes (Figure 2c). Lymphocytes including activated and proliferating cells were also found in the brain vessels in both strains (Figure 2c). Obvious sequestration of pRBC to the endothelium was neither observed in the CBA nor in the Swiss Webster stock.
Figure 2.
Brain and liver of Swiss Webster mice. (a) Panoramic view of non-infected control mouse brain with a clean large vessel. Haematoxylin–eosin, 200×. (b) Infected mouse, large haemorrhage in cerebellum, Purkinje cell area. Haematoxylin–eosin, 400×. (c) Infected mouse, brain vessel full of pigment-containing monocytes. Parasitized and non-parasitized RBC can be observed adherent to activated monocytes. Haematoxylin–eosin, 500×. (d) Panoramic view of a normal mouse liver, showing typical architecture, clean sinusoids and resting Kupffer cells. Haematoxylin–eosin, 200×. (e) Infected mouse, moriform vacuolization of hepatocytes and pigmented Kupffer cells. Haematoxylin–eosin, 200×. (f) Detail of moriform vacuolization, hypertrophic Kupffer cells containing malarial pigment and intra-sinusoidal clusters of mononuclear cells. Haematoxylin–eosin, 400×.
Liver
Uninfected mice showed liver sections with typical architecture and colour, clean sinusoids with few cells and resting Kupffer cells (Figure 2d). Swiss Webster and CBA mice with clinical CM presented an enlarged liver laden with malaria pigment. The sinusoids, especially in infected Swiss Webster mice, presented adhesion of activated, pigment-containing, monocytes to the endothelium, lymphocytes and erythroid cells forming cell clusters (Figure 2d,e). The large liver vessels contained many clusters of adherent mononuclear cells with some of them containing malaria pigment. Kupffer cells were hypertrophic and saturated with malarial pigment in both strains. Moriform vacuolization of hepatocytes, more intense in Swiss Webster mice, was a common finding (Figure 2d,e), especially in areas close to the central-lobular vein (zone 3). Megakaryocytes were occasionally found in the sinusoids.
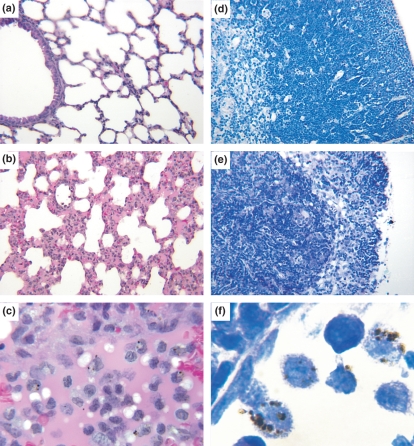
Lungs
Uninfected control mice showed lungs with normal aspects, with thin alveoli walls and clean blood vessels (Figure 3a).The most striking feature of the lungs of infected mice with clinical CM was the increased thickness of the alveoli septa (Figure 3b). In one of eight Swiss mice, the alveoli were almost closed. The septal thickening was caused by the infiltration mainly of mononuclear and, eventually, polymorphonuclear cells; in some cases, intra-alveolar oedema (Figure 3C) and also haemorrhages were observed. In addition, pulmonary vessels showed cytoadherence mainly of mononuclear cells and, to a lesser degree, of neutrophils. Lymphocyte nodules were found in some infected CBA mouse.
Figure 3.
Lungs and thymus of Swiss Webster mice. (a) Panoramic view of non-infected control mouse lung with thin alveoli walls and clean blood vessels. Haematoxylin–eosin, 200×. (b) Panoramic view of the lung of an infected mouse, showing thickening of alveoli walls by the infiltration of mononuclear and polymorphonuclear cells. Haematoxylin–eosin, 200×. (c) Detail of septal thickening in an infected mouse lung, showing predominance of mononuclear cells. Haematoxylin–eosin, 400×. (d) Panoramic view of a normal mouse thymus, showing the cortical area plenty of thymocytes and the internal medullar area with a lower cellularity. Giemsa, 200×. (e) Panoramic view of the thymus of a infected mouse, showing intense thymocyte depletion in the cortical area, with only a few remaining thymocytes between the framework of epithelial cells, and an increase in the medullar cellularity resulting in cortico-medullar inversion. Giemsa, 200×. (f) Pronounced monocyte adherence on the endothelium of thymus medullary vessels of infected mice. Monocytes look like macrophages and contain malarial pigment. Giemsa, 1000×.
Thymus
Thymuses of uninfected control mice showed normal macroscopical appearance and size, and lobes could be well distinguished. Histological analysis showed a good differentiation between the cortex and the medulla. In the cortical region, small thymocytes were well organized, without evident foci of apoptosis and several mitotic figures were observed (Figure 3d). Thymuses of infected Swiss Webster and CBA mice presented macroscopically evident atrophy on days 6–9 of infection. Histopathological analysis revealed cell death of thymocytes in the cortex (Figure 3e), varying from mild to intense, in some cases leading to thymocyte depletion. The intensity of cortical apoptosis, as previously described by Carvalho et al. (2006), could be divided in three patterns: (i) the cortex presented widespread foci of thymocyte death resulting in a ‘starry-sky’ pattern of diffuse apoptosis with maintenance of cortical-medullary structure; (ii) intense apoptosis with cortical atrophy, with absence of large cells – only small thymocytes could be seen; and (iii) severe cortical thymocyte depletion, resulting in cortical-medullary inversion; only residual clusters of small thymocytes were observed within the framework of epithelial cells (Figure 3e). In addition, less mitotic figures were present in the cortex of infected mice compared with control mice.
Changes in thymus microenvironment led also to the appearance, in the cortical area, of foci of myelopoiesis and the recruitment of different cell types such as mast cells and granulocytes, especially eosinophils. These changes in the thymic microenvironment were more strikingly evidenced by the presence of myelopoiesis. These events were especially evident in the Swiss mouse strain. The thymus medulla of infected mice seemed to contain more Hassall's corpuscles and presented more cell death than control mice. Vascular plugging with adherence of pigmented mononuclear cells to each other and to the endothelium was also found in the thymus vessels of infected mice (Figure 3f).
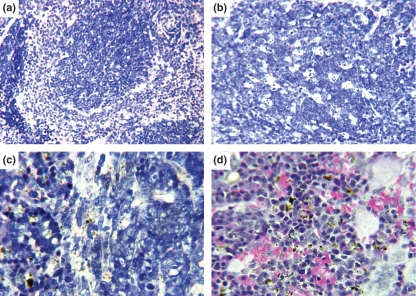
Spleen
Uninfected mice presented evident distinction between red pulp, resting follicles and marginal zone (MZ). The follicle consisted of well-organized small cells (Figure 4a). In contrast to the thymus, during infection, the size of the spleen was grossly increased because of an overall enlargement of the red and the white pulp in both strains. The white pulp of infected mice presented loss of the follicle germinal centres (GC) typical architecture acquiring a disorganized aspect, without clear limitations of dark and light zones (Figure 4b). Disorganized GCs presented intense centroblast activation and proliferation with little centrocytic transformation, several phagocytic-centres with apoptotic bodies (Figure 4b), centripetal penetration of small lymphocytes from the periphery and several perifollicular mitosis. The mantle and MZ disappeared and the borders between the B-cell follicles and the red pulp were blurred (Figure 4b). Centroblasts and centrocytes were considered according to Lennert's morphological characteristics (Lennert 1978). CBA and Swiss Webster mice showed an increased number of immunoblasts (activated T cells) and intense plasmacytogenesis in the T-cell area on days 6–9 of infection, especially in the Swiss Webster stock (Figure 4c). Infected mice also showed lots of malaria pigment in the red pulp, mainly within macrophages, and, in a lesser extent, in the MZ (Figure 4d). The red pulp also was hypertrophic and contained a great variety of cells, mainly blood cell precursors like erythroblasts in different stages of maturation, monoblasts, promonocytes and megakaryocytes distinguishing zones of intense erythropoiesis and foci of monocytopoiesis close to septae. As in the previous described organs, the spleen also represented cytoadherence in the vessels, mainly of monocytes containing malaria pigment.
Figure 4.
Spleen of Swiss Webster mice. (a) Panoramic view of non-infected control mouse spleen. White and red pulps with well-defined limits. One B-cell resting follicle with surrounding thick marginal zones. Giemsa, 200×. (b) Panoramic view of infected mouse spleen. Disorganized germinal centre with intense centroblast activation, proliferation, apoptosis, without centrocyte differentiation and definition of light and dark areas, absence of marginal zone and blurred limits between white and red pulps. Giemsa, 200×. (c) T-cell area (periarteriolar lymphoid sheath) of infected mouse. Centroblasts. Giemsa, 400×. (d) Infected mouse, malarial pigment in red pulp macrophages. Giemsa 400×.
Discussion
The present study provides consistent data supporting the susceptibility of the Swiss Webster mouse to CM induced by P. berghei ANKA infection, making available an outbred model for investigating pathogenic features of this malaria complication. The characteristic features of the P. berghei ANKA infection in the inbred CBA mice were present in the Swiss Webster model. First, this model showed a sizeable (62.7%) and reproducible incidence of CM, in a time course similar to that observed in inbred strains, and all mice died within a few hours after presenting the clinical signs of neurological involvement. Second, the course of parasitaemia was similar to that observed in the PbA-CBA model. Third, Swiss Webster mice with CM showed histopathological changes in brain (e.g., micro- and perivascular haemorrhages, vessel plugging by mononuclear cells and perivascular oedema) similar to those observed during PbA infection in CBA mice (Carvalho et al. 2000; Lou et al. 2001). Fourth, the other histopathological changes in all organs analysed, including leucocyte sequestration in brain, lungs, liver, thymus and spleen vessels, were also analogous to the PbA-CBA model.
Indeed, in addition to affecting the central nervous system, PbA infection in the Swiss Webster mouse was characterized by systemic damage, impinging on several organs such as the lungs, liver and lymphoid organs, as it may happen in human malaria (Taylor & White 2002; Kochar et al. 2003). Here we provide detailed description of the changes in these organs that were similar to changes observed in PbA-inbred mouse models (Rest 1982; Carvalho et al. 2000,2006,2007). The thickening of the lung interalveolar septa in Swiss Webster stock and CBA strain may explain some of the clinical signs, like difficulty in breathing and loss in activity, and contribute to the acidosis found in murine and human CM. Moreover, histopathological changes in liver, mainly the moriform vacuolization of hepatocytes, provide evidence of liver damage, as also observed in P. berghei K173 infection (Eling et al. 1977; Van Zon et al. 1978), and help explaining hepatic dysfunction during PbA infection (De-Oliveira et al. 2006). To which extent this may influence CM remains unclear. According to the WHO, signs of hepatic dysfunction are unusual and clinical signs of liver failure such as asterixis or ‘liver flap’ are never seen in CM (2000). However, in recent years, many isolated case reports and studies with definite evidence of hepatic dysfunction in patients with P. falciparum malaria have been reported from different parts of the world (Anand et al. 1992; Mishra et al. 1992; Ahsan et al. 1993; Srivastava et al. 1996; Premaratna et al. 2001; Kochar et al. 2003; Bhalla et al. 2006; Guha et al. 2006). Metabolic changes suggestive of hepatic encephalopathy have also been shown late in the course of infection by PbA in Balb/c mice not developing classical CM (Penet et al. 2007). Extensive alterations in lymphoid organs, as previously reported in CBA mice such as including thymic atrophy as a result of thymocyte apoptotic depletion and germinal centre architecture disturbance in the spleen (Carvalho et al. 2006,2007; or during P. berghei K173 infection in six different mouse strains (Eling et al. 1977; Van Zon et al. 1978), were also observed in the PbA-infected Swiss Webster mouse.
This newly characterized mouse–parasite combination adds to a number of existing murine models of CM, mostly using the PbA strain in several inbred mouse strains, such as the CBA and the C57Bl/6, and also others using different rodent plasmodial species (de Kossodo & Grau 1993; de Souza & Riley 2002). This is the case, for instance, for the infection of Balb/c or Swiss Webster mice by Plasmodium yoelii, claimed to be models in which pRBC sequestration occurs (Kaul et al. 1994). In addition, extensive characterization of P. berghei infection in the Swiss Webster mouse was performed in the early works of Jerusalem and Desowitz (Van Zon et al. 1978; Jerusalem et al. 1983). However, these authors worked with a different P. berghei strain, the K173, which has been used in many works as a control strain that does not cause CM, although it is reported to induce cerebral pathology when a low inoculum dose is used (Golenser et al. 1997; Hermsen et al. 1997; Postma et al. 1999; Rae et al. 2004; Mitchell et al. 2005; Potter et al. 2005). Experimental animal models cannot reproduce all the features of human diseases, and this is particularly true for CM (Lou et al. 2001). However, animal models are key in guiding the discovery of mechanisms of disease and potential targets for prophylactic or therapeutic interventions, and they are as well a critical step in testing new developed curative or preventive interventions. Thus, the availability of different host–parasite combinations, each with particular characteristics that makes them suitable for specific approaches, is welcome in biomedical research. The availability of different models may also provide opportunity for comparing the mechanisms of disease between these models, which can potentially provide relevant data for understanding the physiopathogenesis of CM.
A major application for an outbred model for CM can be on QTL research (Chia et al. 2005). Indeed, although the QTL approach has been largely used by geneticists to localize and identify complex traits in a variety of diseases and conditions (Manenti et al. 2003; Yalcin et al. 2004; Chia et al. 2005; Flint et al. 2005; Wu & Lin 2006), only a few studies on malaria have been reported, including studies on mouse susceptibility or resistance to high parasitaemia (Fortin et al. 1997; Hernandez-Valladares et al. 2004a,b; Campino et al. 2005) and drug resistance (Ferdig et al. 2004; Sen & Ferdig 2004; Bennett et al. 2007) and one study on murine CM (Bagot et al. 2002a,b). The challenge is to narrow these and other potential loci to the underlying genes conferring resistance or susceptibility. Since the work of Yalcin et al. (2004), describing a method to dissect QTL down to a single gene linked to a particular phenotype (in this case, Rsg2 gene and anxiety) using genotyping and phenotype assessment of the MF1 outbred stock of mouse together with haplotype reconstruction, the great potential of outbred mouse strains for the identification of genes linked to particular phenotypes has been noticed (Chia et al. 2005). Thus, QTL approach followed by in-depth analysis using the here described and characterized PbA-infected outbred Swiss Webster mouse has the potential of being an useful resource to track as yet unidentified genetic factors determining the expression of CM.
Another potential application for this outbred mouse model of CM is on the testing of vaccines or new and existing drugs aimed at preventing or treating this type of malaria complication. Although the use of outbred stocks for these purposes has been criticized (Chia et al. 2005), many researchers still take advantage of this approach to evaluate pharmacological and toxicological responses in genetically heterogeneous populations. One of its main uses can be on the development and evaluation of adjunctive therapies for CM, for which there is an urgent need as 10–20% of CM patients die even when hospitalized and receive proper anti-malarial treatment (McIntosh & Olliaro 2000).
We must point out that, although the genetic makeup of the host is a crucial factor determining susceptibility to CM, non-genetic-related factors are also important and have to be taken very carefully when mapping loci for resistance or susceptibility. This is clearly ascertained by the fact that even the most susceptible strains rarely present 100% CM incidence. Here we showed that parasitaemia levels were associated with the risk of CM development, that is, the risk of CM is significantly higher in mice that show higher values of parasitaemia within a given strain. This is not a straightforward conclusion as it may appear at first sight, especially because CM in PbA-infected mice occurs at a time when parasitaemia is not particularly high (about 10–25%; non-CM survivor mice can go higher than 60%). Indeed, no previous work has clearly determined this association. Our data also evidence the importance of timing, as a late rise in parasitaemia in those mice that did not reach the ‘CM-related threshold of parasitaemia’ on days 6–10 is not capable of inducing CM at the later time. Previous studies related CM development with parasite forms encountered in blood smears, with few schizonts detectable on blood films from CM susceptible mice (Hearn et al. 2000). However, survival analysis techniques were not employed to describe the association between the course of parasitaemia and the risk of developing CM. Some other works considered the importance of a higher level of parasitaemia for the neurological syndrome to develop, but assumptions were mostly made considering differences of parasitaemia between two different mouse strains (Bagot et al. 2002b). Genetic studies using crosses of CM susceptible and resistant mice showed that resistance to high parasitaemia is genetically controlled, with the resistant loci mapped to chromosome 1 and co-localizing with a previously identified locus of resistance to CM (Campino et al. 2005). However, courses of parasitaemia by P. berghei ANKA can be quite variable even within a homogeneous group of inbred mice, and variations would lead to different outcomes unrelated to the genetic background.
Our data thus suggest that a threshold of parasite burden on days 6–8, with release of considerable amounts of parasite antigens and toxins, is necessary to exacerbate the inflammatory response to a point intense enough to result in cerebral damage. Inflammation is indeed a key feature of CM (Clark & Cowden 2003; van der Heyde et al. 2006). In addition, a higher level of parasitaemia will result in higher amounts of free haemoglobin and free haeme released, both shown to be involved in CM pathogenesis (Gramaglia et al. 2006; Pamplona et al. 2007).
Finally, as some works have suggested that PbA sequester in the deep vasculature of the brain and other tissues (Hearn et al. 2000; Franke-Fayard et al. 2005; Amante et al. 2007), peripheral parasitaemia may not reflect the total parasite burden and thus would not be a reliable measure to associate with CM development. Nevertheless, PbA sequestration in the brain deep vasculature during CM is still a matter of debate, and even if present it seems to occur to a minor extent (Lou et al. 2001). Chemiluminescence studies with transgenic PbA parasites expressing luciferase have shown apparent discrepant results. Franke-Fayard et al. (2005) reported that sequestration occurs in the lungs, spleen and adipose tissue and that an increase in luciferase activity in the brains of mice just before and during cerebral complications was never detected. On the other hand, Amante et al. (2007) reported significant chemiluminescence detection in the brain and other tissues of PbA-infected mice on day 5 of infection. Using histological examination, we have not observed direct parasite sequestration to the endothelium in the present and in previous works (Carvalho et al. 2000). However, we observed pRBC attached to the surface of endothelium-adherent monocyte-macrophages (Figure 2c), which also showed intense parasite phagocytosis. As intense mononuclear cell sequestration is observed in the brain vessels of CM mice, macrophage-trapped parasites may then account at least in part for parasites detected in the brain vasculature during CM. In any case, whether direct parasite sequestration does or does not occur, the fact that peripheral parasitaemia levels differ in CM and non-CM mice during a time window on days 6–8 of infection opens the possibility to construct a mathematic model based on this parameter to predict the risk of a susceptible animal to develop CM.
In summary, this study makes available a characterized model of CM in an outbred mouse stock that can prove useful for a variety of studies. It also shows that the histopathological changes in brain, lungs, liver and lymphoid organs in CM-susceptible Swiss Webster mice are similar to changes observed in inbred models and statistically proves that the value of parasitaemia of each mouse on defined infection time points are associated with the risk of CM development.
Acknowledgments
To Marilene Damazio dos Santos and Luiz Carlos da Silva from the Leônidas Deane Animal House for caring mice. To Belmira Santos from the Fiocruz Animal House for providing the Swiss Webster and the CBA mice. To Rodrigo Mexes from the Service of Image Treatment and Production for treating the images. This work was supported with funds of the Laboratory of Malaria Research and the Department of Pathology (POM) and of the Conselho Nacional de Desenvolvimento Tecnológico (CNPq) – Brazil. YCM and CTDR were receivers of fellowships from CNPq.
References
- Ahsan T, Rab SM, Shekhani MS. Falciparum malaria or fulminant hepatic failure? J. Pak. Med. Assoc. 1993;43:206–208. [PubMed] [Google Scholar]
- Amante FH, Stanley AC, Randall LM, et al. A role for natural regulatory T cells in the pathogenesis of experimental cerebral malaria. Am. J. Pathol. 2007;171:548–559. doi: 10.2353/ajpath.2007.061033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand AC, Ramji C, Narula AS, Singh W. Malarial hepatitis: a heterogeneous syndrome? Natl. Med. J. India. 1992;5:59–62. [PubMed] [Google Scholar]
- Bagot S, Campino S, Penha-Goncalves C, Pied S, Cazenave PA, Holmberg D. Identification of two cerebral malaria resistance loci using an inbred wild-derived mouse strain. Proc. Natl. Acad. Sci. U.S.A. 2002a;99:9919–9923. doi: 10.1073/pnas.152215199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagot S, Idrissa Boubou M, Campino S, et al. Susceptibility to experimental cerebral malaria induced by Plasmodium berghei ANKA in inbred mouse strains recently derived from wild stock. Infect. Immun. 2002b;70:2049–2056. doi: 10.1128/IAI.70.4.2049-2056.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett TN, Patel J, Ferdig MT, Roepe PD. Plasmodium falciparum Na+/H+ exchanger activity and quinine resistance. Mol. Biochem. Parasitol. 2007;153:48–58. doi: 10.1016/j.molbiopara.2007.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhalla A, Suri V, Singh V. Malarial hepatopathy. J. Postgrad. Med. 2006;52:315–320. [PubMed] [Google Scholar]
- Bland JM, Altman DG. The logrank test. BMJ. 2004;328:1073. doi: 10.1136/bmj.328.7447.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campino S, Bagot S, Bergman ML, et al. Genetic control of parasite clearance leads to resistance to Plasmodium berghei ANKA infection and confers immunity. Genes Immun. 2005;6:416–421. doi: 10.1038/sj.gene.6364219. [DOI] [PubMed] [Google Scholar]
- Carvalho LJ, Lenzi HL, Pelajo-Machado M, Oliveira DN, Daniel-Ribeiro CT, Ferreira-da-Cruz MF. Plasmodium berghei: cerebral malaria in CBA mice is not clearly related to plasma TNF levels or intensity of histopathological changes. Exp. Parasitol. 2000;95:1–7. doi: 10.1006/expr.2000.4508. [DOI] [PubMed] [Google Scholar]
- Carvalho LJ, Ferreira-da-cruz MF, Daniel-Ribeiro CT, Pelajo-Machado M, Lenzi HL. Plasmodium berghei ANKA infection induces thymocyte apoptosis and thymocyte depletion in CBA mice. Mem. Inst. Oswaldo Cruz. 2006;101:523–528. doi: 10.1590/s0074-02762006000500007. [DOI] [PubMed] [Google Scholar]
- Carvalho LJ, Ferreira-da-Cruz MF, Daniel-Ribeiro CT, Pelajo-Machado M, Lenzi HL. Germinal center architecture disturbance during Plasmodium berghei ANKA infection in CBA mice. Malar. J. 2007;6:59. doi: 10.1186/1475-2875-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia R, Achilli F, Festing MF, Fisher EM. The origins and uses of mouse outbred stocks. Nat. Genet. 2005;37:1181–1186. doi: 10.1038/ng1665. [DOI] [PubMed] [Google Scholar]
- Clark IA, Cowden WB. The pathophysiology of falciparum malaria. Pharmacol. Ther. 2003;99:221–260. doi: 10.1016/s0163-7258(03)00060-3. [DOI] [PubMed] [Google Scholar]
- Clark IA, Rockett KA. The cytokine theory of human cerebral malaria. Parasitol. Today. 1994;10:410–412. doi: 10.1016/0169-4758(94)90237-2. [DOI] [PubMed] [Google Scholar]
- De-Oliveira AC, Da-Matta AC, Paumgartten FJ. Plasmodium berghei (ANKA): infection induces CYP2A5 and 2E1 while depressing other CYP isoforms in the mouse liver. Exp. Parasitol. 2006;113:256–261. doi: 10.1016/j.exppara.2006.01.013. [DOI] [PubMed] [Google Scholar]
- Eling W, van Zon A, Jerusalem C. The course of a Plasmodium berghei infection in six different mouse strains. Z. Parasitenkd. 1977;54:29–45. doi: 10.1007/BF00380634. [DOI] [PubMed] [Google Scholar]
- Ferdig MT, Cooper RA, Mu J, et al. Dissecting the loci of low-level quinine resistance in malaria parasites. Mol. Microbiol. 2004;52:985–997. doi: 10.1111/j.1365-2958.2004.04035.x. [DOI] [PubMed] [Google Scholar]
- Flint J, Valdar W, Shifman S, Mott R. Strategies for mapping and cloning quantitative trait genes in rodents. Nat. Rev. Genet. 2005;6:271–286. doi: 10.1038/nrg1576. [DOI] [PubMed] [Google Scholar]
- Fortin A, Belouchi A, Tam MF, et al. Genetic control of blood parasitaemia in mouse malaria maps to chromosome 8. Nat. Genet. 1997;17:382–383. doi: 10.1038/ng1297-382. [DOI] [PubMed] [Google Scholar]
- Fortin A, Stevenson MM, Gros P. Complex genetic control of susceptibility to malaria in mice. Genes Immun. 2002;3:177–186. doi: 10.1038/sj.gene.6363841. [DOI] [PubMed] [Google Scholar]
- Franke-Fayard B, Janse CJ, Cunha-Rodrigues M, et al. Murine malaria parasite sequestration: CD36 is the major receptor, but cerebral pathology is unlinked to sequestration. Proc. Natl Acad. Sci. U.S.A. 2005;102:11468–11473. doi: 10.1073/pnas.0503386102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golenser J, Domb A, Teomim D, et al. The treatment of animal models of malaria with iron chelators by use of a novel polymeric device for slow drug release. J. Pharmacol. Exp. Ther. 1997;281:1127–1135. [PubMed] [Google Scholar]
- Good MF, Xu H, Wykes M, Engwerda CR. Development and regulation of cell-mediated immune responses to the blood stages of malaria: implications for vaccine research. Annu. Rev. Immunol. 2005;23:69–99. doi: 10.1146/annurev.immunol.23.021704.115638. [DOI] [PubMed] [Google Scholar]
- Gramaglia I, Sobolewski P, Meays D, et al. Low nitric oxide bioavailability contributes to the genesis of experimental cerebral malaria. Nat. Med. 2006;12:1417–1422. doi: 10.1038/nm1499. [DOI] [PubMed] [Google Scholar]
- Grau GE, Piguet PF, Engers HD, Louis JA, Vassalli P, Lambert PH. L3T4+ T lymphocytes play a major role in the pathogenesis of murine cerebral malaria. J. Immunol. 1986;137:2348–2354. [PubMed] [Google Scholar]
- Guha M, Kumar S, Choubey V, Maity P, Bandyopadhyay U. Apoptosis in liver during malaria: role of oxidative stress and implication of mitochondrial pathway. FASEB J. 2006;20:1224–1226. doi: 10.1096/fj.05-5338fje. [DOI] [PubMed] [Google Scholar]
- Gupta N, Sehgal R, Mahajan RC, Banerjee AK, Ganguly NK. Role of immune complexes in cerebral malaria. Pathology. 1988;20:373–376. doi: 10.3109/00313028809085222. [DOI] [PubMed] [Google Scholar]
- Hearn J, Rayment N, Landon DN, Katz DR, de Souza JB. Immunopathology of cerebral malaria: morphological evidence of parasite sequestration in murine brain microvasculature. Infect. Immun. 2000;68:5364–5376. doi: 10.1128/iai.68.9.5364-5376.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermsen C, van de Wiel T, Mommers E, Sauerwein R, Eling W. Depletion of CD4+ or CD8+ T-cells prevents Plasmodium berghei induced cerebral malaria in end-stage disease. Parasitology. 1997;114(Pt 1):7–12. doi: 10.1017/s0031182096008293. [DOI] [PubMed] [Google Scholar]
- Hernandez-Valladares M, Naessens J, Gibson JP, et al. Confirmation and dissection of QTL controlling resistance to malaria in mice. Mamm. Genome. 2004a;15:390–398. doi: 10.1007/s00335-004-3042-4. [DOI] [PubMed] [Google Scholar]
- Hernandez-Valladares M, Rihet P, ole-MoiYoi OK, Iraqi FA. Mapping of a new quantitative trait locus for resistance to malaria in mice by a comparative mapping approach with human Chromosome 5q31-q33. Immunogenetics. 2004b;56:115–117. doi: 10.1007/s00251-004-0667-0. [DOI] [PubMed] [Google Scholar]
- van der Heyde HC, Nolan J, Combes V, Gramaglia I, Grau GE. A unified hypothesis for the genesis of cerebral malaria: sequestration, inflammation and hemostasis leading to microcirculatory dysfunction. Trends Parasitol. 2006;22:503–508. doi: 10.1016/j.pt.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Hunt NH, Grau GE. Cytokines: accelerators and brakes in the pathogenesis of cerebral malaria. Trends Immunol. 2003;24:491–499. doi: 10.1016/s1471-4906(03)00229-1. [DOI] [PubMed] [Google Scholar]
- Jerusalem C, Polder T, Wijers-Rouw M, et al. Comparative clinical and experimental study on the pathogenesis of cerebral malaria. Contrib. Microbiol. Immunol. 1983;7:130–138. [PubMed] [Google Scholar]
- Kaul DK, Nagel RL, Llena JF, Shear HL. Cerebral malaria in mice: demonstration of cytoadherence of infected red blood cells and microrheologic correlates. Am. J. Trop. Med. Hyg. 1994;50:512–521. doi: 10.4269/ajtmh.1994.50.512. [DOI] [PubMed] [Google Scholar]
- Kochar DK, Agarwal P, Kochar SK, et al. Hepatocyte dysfunction and hepatic encephalopathy in Plasmodium falciparum malaria. QJM. 2003;96:505–512. doi: 10.1093/qjmed/hcg091. [DOI] [PubMed] [Google Scholar]
- de Kossodo S, Grau GE. Profiles of cytokine production in relation with susceptibility to cerebral malaria. J. Immunol. 1993;151:4811–4820. [PubMed] [Google Scholar]
- Lennert K. Malignant Lymphoma Other Than Hodgkin's Disease. Berlin: Springer-Verlag; 1978. [Google Scholar]
- Lou J, Donati YR, Juillard P, et al. Platelets play an important role in TNF-induced microvascular endothelial cell pathology. Am. J. Pathol. 1997;151:1397–1405. [PMC free article] [PubMed] [Google Scholar]
- Lou J, Lucas R, Grau GE. Pathogenesis of cerebral malaria: recent experimental data and possible applications for humans. Clin. Microbiol. Rev. 2001;14:810–820. doi: 10.1128/CMR.14.4.810-820.2001. table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovegrove FE, Pena-Castillo L, Mohammad N, Liles WC, Hughes TR, Kain KC. Simultaneous host and parasite expression profiling identifies tissue-specific transcriptional programs associated with susceptibility or resistance to experimental cerebral malaria. BMC Genomics. 2006;7:295. doi: 10.1186/1471-2164-7-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovegrove FE, Gharib SA, Patel SN, Hawkes CA, Kain KC, Liles WC. Expression microarray analysis implicates apoptosis and interferon-responsive mechanisms in susceptibility to experimental cerebral malaria. Am. J. Pathol. 2007;171:1894–1903. doi: 10.2353/ajpath.2007.070630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manenti G, Galbiati F, Noci S, Dragani TA. Outbred CD-1 mice carry the susceptibility allele at the pulmonary adenoma susceptibility 1 (Pas1) locus. Carcinogenesis. 2003;24:1143–1148. doi: 10.1093/carcin/bgg065. [DOI] [PubMed] [Google Scholar]
- McIntosh HM, Olliaro P. Artemisinin derivatives for treating severe malaria. Cochrane Database Syst. Rev. 2000 doi: 10.1002/14651858.CD000527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra SK, Mohanty S, Das BS, et al. Hepatic changes in P. falciparum malaria. Indian J. Malariol. 1992;29:167–171. [PubMed] [Google Scholar]
- Mitchell AJ, Hansen AM, Hee L, et al. Early cytokine production is associated with protection from murine cerebral malaria. Infect. Immun. 2005;73:5645–5653. doi: 10.1128/IAI.73.9.5645-5653.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molyneux ME, Taylor TE, Wirima JJ, Borgstein A. Clinical features and prognostic indicators in paediatric cerebral malaria: a study of 131 comatose Malawian children. Q. J. Med. 1989;71:441–459. [PubMed] [Google Scholar]
- Neill AL, Hunt NH. Pathology of fatal and resolving Plasmodium berghei cerebral malaria in mice. Parasitology. 1992;105(Pt 2):165–175. doi: 10.1017/s0031182000074072. [DOI] [PubMed] [Google Scholar]
- Nitcheu J, Bonduelle O, Combadiere C, et al. Perforin-dependent brain-infiltrating cytotoxic CD8+ T lymphocytes mediate experimental cerebral malaria pathogenesis. J. Immunol. 2003;170:2221–2228. doi: 10.4049/jimmunol.170.4.2221. [DOI] [PubMed] [Google Scholar]
- Pamplona A, Ferreira A, Balla J, et al. Heme oxygenase-1 and carbon monoxide suppress the pathogenesis of experimental cerebral malaria. Nat. Med. 2007;13:703–710. doi: 10.1038/nm1586. [DOI] [PubMed] [Google Scholar]
- Patnaik JK, Das BS, Mishra SK, Mohanty S, Satpathy SK, Mohanty D. Vascular clogging, mononuclear cell margination, and enhanced vascular permeability in the pathogenesis of human cerebral malaria. Am. J. Trop. Med. Hyg. 1994;51:642–647. [PubMed] [Google Scholar]
- Penet MF, Kober F, Confort-Gouny S, et al. Magnetic resonance spectroscopy reveals an impaired brain metabolic profile in mice resistant to cerebral malaria infected with Plasmodium berghei ANKA. J. Biol. Chem. 2007;282:14505–14514. doi: 10.1074/jbc.M608035200. [DOI] [PubMed] [Google Scholar]
- Pongponratn E, Riganti M, Punpoowong B, Aikawa M. Microvascular sequestration of parasitized erythrocytes in human falciparum malaria: a pathological study. Am. J. Trop. Med. Hyg. 1991;44:168–175. doi: 10.4269/ajtmh.1991.44.168. [DOI] [PubMed] [Google Scholar]
- Postma NS, Hermsen RC, Crommelin DJ, Eling WM, Zuidema J. Thiolated recombinant human tumor necrosis factor-alpha protects against Plasmodium berghei K173-induced experimental cerebral malaria in mice. Antimicrob. Agents Chemother. 1999;43:1027–1033. doi: 10.1128/aac.43.5.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter SM, Mitchell AJ, Cowden WB, et al. Phagocyte-derived reactive oxygen species do not influence the progression of murine blood-stage malaria infections. Infect. Immun. 2005;73:4941–4947. doi: 10.1128/IAI.73.8.4941-4947.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Premaratna R, Gunatilake AK, de Silva NR, Tilakaratne Y, Fonseka MM, de Silva HJ. Severe hepatic dysfunction associated with falciparum malaria. Southeast Asian J. Trop. Med. Public Health. 2001;32:70–72. [PubMed] [Google Scholar]
- Rae C, McQuillan JA, Parekh SB, et al. Brain gene expression, metabolism, and bioenergetics: interrelationships in murine models of cerebral and noncerebral malaria. FASEB J. 2004;18:499–510. doi: 10.1096/fj.03-0543com. [DOI] [PubMed] [Google Scholar]
- Rest JR. Cerebral malaria in inbred mice. I. A new model and its pathology. Trans. R. Soc. Trop. Med. Hyg. 1982;76:410–415. doi: 10.1016/0035-9203(82)90203-6. [DOI] [PubMed] [Google Scholar]
- Sen S, Ferdig M. QTL analysis for discovery of genes involved in drug responses. Curr. Drug Targets Infect. Disord. 2004;4:53–63. doi: 10.2174/1568005043480916. [DOI] [PubMed] [Google Scholar]
- de Souza JB, Riley EM. Cerebral malaria: the contribution of studies in animal models to our understanding of immunopathogenesis. Microbes Infect. 2002;4:291–300. doi: 10.1016/s1286-4579(02)01541-1. [DOI] [PubMed] [Google Scholar]
- Srivastava A, Khanduri A, Lakhtakia S, Pandey R, Choudhuri G. Falciparum malaria with acute liver failure. Trop. Gastroenterol. 1996;17:172–174. [PubMed] [Google Scholar]
- Taylor WR, White NJ. Malaria and the lung. Clin. Chest Med. 2002;23:457–468. doi: 10.1016/s0272-5231(02)00004-7. [DOI] [PubMed] [Google Scholar]
- Urban BC, Hien TT, Day NP, et al. Fatal Plasmodium falciparum malaria causes specific patterns of splenic architectural disorganization. Infect. Immun. 2005;73:1986–1994. doi: 10.1128/IAI.73.4.1986-1994.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Zon A, Eling W, Jerusalem C. Histo- and immunopathology of a malaria (Plasmodium berghei) infection in mice. Isr. J. Med. Sci. 1978;14:659–672. [PubMed] [Google Scholar]
- Wu R, Lin M. Functional mapping - how to map and study the genetic architecture of dynamic complex traits. Nat. Rev. Genet. 2006;7:229–237. doi: 10.1038/nrg1804. [DOI] [PubMed] [Google Scholar]
- Yalcin B, Willis-Owen SA, Fullerton J, et al. Genetic dissection of a behavioral quantitative trait locus shows that Rgs2 modulates anxiety in mice. Nat. Genet. 2004;36:1197–1202. doi: 10.1038/ng1450. [DOI] [PubMed] [Google Scholar]