Abstract
Menthol is a controversial cigarette additive because its’ physiological or pharmacologic effects may possibly increase the risk of cancer and its targeted market is the black community. In a community-based cross-sectional study of 525 black and white volunteers, we compared levels of urinary and plasma cotinine, plasma thiocyanate, urinary 4-(N-nitrosomethylamino)-1-(3-pyridyl)-1-butanol (NNAL) and its detoxified form NNAL-Gluc between menthol and nonmenthol smokers. In regression models that adjusted for daily cigarette intake, no significant differences were observed in the concentration of these biomarkers by menthol status in both races. There was no significant association between high Fagerstrom nicotine dependence scores and the use of menthol cigarettes (odds ratio [OR] = 1.1, 95% confidence intervals [CI] 0.6–2.0), but an increased risk was observed with smoking a cigarette soon (≤30 minutes) after waking (OR = 2.1, 95% CI 1.0–3.8). The ratio of NNAL-Gluc to NNAL, a possible indicator of lung cancer risk, was significantly lower in menthol vs. nonmenthol smokers. The NNAL-Gluc/NNAL ratio was 34% lower in whites (P<0.01) and 22% lower in blacks. In subsequent human liver microsome studies, menthol inhibited the rate of both NNAL-O-glucuronidation and NNAL-N-glucuronidation. Collectively, these results show that menthol does not affect biological exposure to tobacco smoke constituents, but indicates that menthol might inhibit the detoxification of the potent lung carcinogen NNAL.
INTRODUCTION
Numerous flavoring agents are added to tobacco during the manufacturing process. Most cigarette additives are approved for use in foods but their possible toxic effects in a complex mixture of chemical constituents in tobacco smoke is difficult to assess (1–4). Menthol in tobacco smoke may theoretically increase cancer risk by cooling the upper airways, causing a depression in respiratory activity and subsequent increase in exposure to tobacco smoke toxins (5), but menthol cigarettes have not been shown to increase lung and esophageal cancer risk vs. non-menthol cigarettes (6–11). Menthol and other additives mask the harshness of tobacco smoke, which has been implicated in the marketing of cigarettes to youth and increased nicotine delivery in young smokers (12). Menthol increases the in vitro absorption of the tobacco carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) (13), and inhibits the glucuronidation of nicotine, which may lead to a decrease in nicotine dependence (14,15). Conflicting data have been reported on whether menthol smokers are less likely to quit smoking than smokers of nonmentholated cigarettes (16–21).
The H.R. 1108: Family Smoking Prevention and Tobacco Control Act is being considered by the U.S. Congress. The bill would provide the Food and Drug Administration with some authority to regulate tobacco products including the banning of most flavor additives. Menthol is currently exempted from this bill as it is currently written, although the Centers for Disease Control and others have identified menthol as an important issue in health research (22,23). Although there have been substantial investigations on the chemical and pharmacological properties of menthol, the health risks to humans is still debatable because the epidemiologic studies were not designed to detect a small effect size that would be expected in comparing the risk of cancer from one cigarette brand/formulation to another. As an alternative or complimentary approach to estimating the hazards associated with menthol smoking, the use of exposure and intermediate biomarkers can be used to address several important questions on this issue including 1.) Does menthol increase biological exposure to tobacco smoke constituents and carcinogens? 2.) Is menthol associated with behavioral measures of nicotine dependence? and 3.) Does menthol affect the detoxification of the potent tobacco-specific lung carcinogen NNAL?
METHODS
Human subjects-Study Recruitment
The research methods and procedures including inclusion/exclusion criteria, blood collection procedures, blood processing protocols, and analytic methods for cotinine, NNAL and NNAL-Gluc, and thiocyanate (SCN) have been described in detail elsewhere (24). In brief, a community-based cross-sectional study of cigarette smoke metabolism was conducted to determine whether racial differences in tobacco smoke exposure and metabolism may help explain the higher SEER rates of lung cancer in blacks than in whites. The study was conducted in lower Westchester County, NY, including the cities/towns of Mt. Vernon, Yonkers, and White Plains. Subjects were recruited using fliers, newspaper advertisements, WEB-based announcements, word of mouth, and recommendations from community and church leaders. Three community locations were established to meet subjects including a church, YMCA and the laboratories of the American Health Foundation (AHF) in Valhalla. Subjects were healthy volunteers who smoked at least five cigarettes per day and were not taking antidepressants or other medications thought to inhibit liver enzyme function. Subjects were asked to fast and abstain from smoking from 12:00 a.m. the previous night. Urine collection was scheduled at 9:00 a.m. the following day. Trained interviewers administered a structured questionnaire that contained detailed items on cigarette smoking history including the brand of cigarette, the number of cigarettes smoked per day (cpd), the number of minutes after waking up that the first cigarette is smoked and other questions that comprise the 6-item Fagerstrom Test for Nicotine Dependence (FTND) (25). All subjects signed a consent form approved by the AHF Institutional Review Board and received remuneration. Smoking cessation literature and referrals to smoke cessation programs were also offered to participants. The current analysis is based on 525 smokers with a cigarette brand that could be classified according to FTC menthol status, and either a plasma or urinary cotinine determination. Among these subjects, we administered the FTND for 278 subjects. There were 456 subjects with both a plasma and urinary cotinine determination. Urinary NNAL levels were determined for 147 subjects. Based on our findings of menthol and total NNAL glucuronidation, we subsequently conducted in vitro studies using human liver microsomes to determine the effects of menthol on the rates of NNAL-N-glucuronidation and NNAL-O-glucuronidation.
In vitro methods
NNAL was purchased from Toronto Research Labs (Toronto, Canada), and menthol and alamethicin from Sigma-Aldrich (St. Louis, MO). All other chemicals were purchased from Fisher Scientific (Pittsburgh, PA) unless specified otherwise. The three normal human liver tissue specimens used for these studies have been described previously (26). Liver microsomes were prepared through differential centrifugation as previously described (27) and stored (10–20 mg protein/mL) at −80 °C. Microsomal protein concentrations were measured using the BCA assay.
Glucuronidation assays were performed similarly as previously described (28). HLM (25 μg protein) was initially incubated with alamethicin (50 μg/mg protein) for 15 min in an ice bath. A serial dilution of menthol was made in 60% DMSO, and the final concentration of DMSO in reaction was 1.5%. Incubations (20 μL) with 0.5 mM of NNAL were subsequently performed at 37°C in 50 mM Tris buffer (pH 7.5), 10 mM MgCl2, 4 mM UGPGA, and different concentration menthol for 2 hr. Reactions were terminated by the addition of 100 μL of cold acetonitrile. Protein was then removed by centrifugation at 13,000 g for 10 min at 4°C. The NNAL-O-gluc and NNAL–N-gluc formed by HLM toward NNAL were determined by LC-MS/MS MRM analysis.
Samples (10μL) were analyzed for NNAL-O-gluc, NNAL-N-gluc and NNAL by Ultra Performance liquid chromatographic (UPLC) coupled to a TQD (Waters) tandem mass spectrometer with an electrospray interface. The UPLC system (Waters) consisting of a binary gradient pump, an autosampler (4°C) and a column oven (35°C) were used for separation. A 100 × 2.1 mm i.d. Acquity UPLC HILIC column with 1.7 μm particles (Waters) was used for separation. A 0.2 □m pre-filter was installed before the column. Eluents were (A) 5 mM NH4AC in 50% acetonitrile at pH6.7, and (B) 5 mM NH4AC in 90% acetonitrile at pH6.7. The flow-rate was 0.5 mL/min. Sample volumes of 10 μL were injected. Gradient conditions were as follows: 0–2 min, 20% A; 2–3 min, linear gradient to 100% A; 3–5min, 100% B.
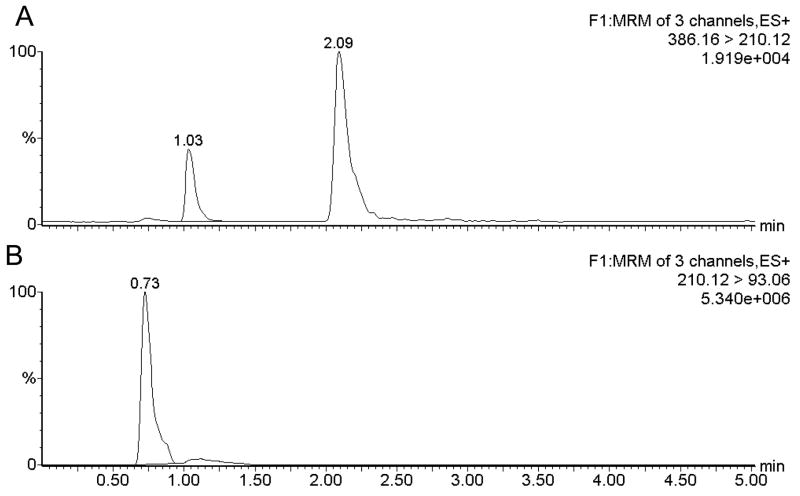
The mass spectrometer was operated in the multiple reaction monitoring (MRM) mode for quantitative analyses. Argon was used as the collision gas. Nitrogen was used both as desolvation gas and cone gas. During the run the system was in positive ESI-mode. The source temperature was 140 °C. The curtain gas was 20 L/Hr. The desolvation gas Flow was 760 L/Hr, and desolvation temperature was 450°C. Collision gas flow rate is 0.1mL/min. The capillary voltage was 0.64 kV. The mass transitions for NNAL-O-gluc and NNAL-N-gluc was m/z 386→210 with cone voltage of 25 V and collision energy was 15 eV. The mass transitions for NNAL was m/z 210→93, with cone voltage of 25 V and collision energy of 20 eV. As show in Figure 1, retention times for NNAL-O-gluc, NNAL-N-gluc and NNAL, were 1.03, 2.09 and 0.73 minutes. The peak areas from each of these peaks were obtained, and ratios of the NNAL-O-gluc and NNAL-N-gluc to NNAL were calculated.
Figure 1.
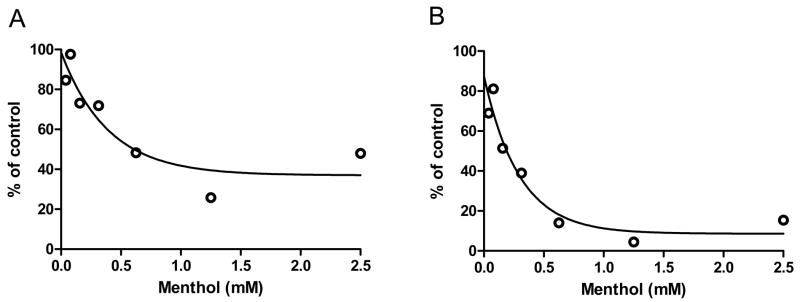
For the estimation of IC50 values, glucuronidation assays were performed at a fixed concentration of NNAL (0.5mM), which is close to the KM for glucuronidation of NNAL by human liver microsomes (0.85mM) (28). The concentrations of menthol ranged from 0 to 2.5 mM. The IC50 was calculated by Prism Version 4.01 software (GraphPad Software, San Diego, CA, USA), using log(inhibitor) vs response --variable slope.
Statistical analyses
The statistical analysis was conducted using SAS software (version 9.13, Cary, NC). Univariate statistics included means, standard deviations, and frequency distributions. There were no significant differences in urinary creatinine concentrations between menthol and nonmenthol smokers. Bivariate analysis included correlations, parametric t-tests and chi-square tests. The validity of self-reported smoking amount was previously described (r = 0.95 in blacks and 0.83 in whites) (29). Multiple least-square regression models for biomarkers were fitted where the independent effects of menthol were determined after adjusting for cigarettes smoked per day, age, and sex. Separate models were fit for blacks and whites. The relationship between cpd and biomarker level was nonlinear, and for most models quadratic and cubic terms were fitted. For each biomarker, we modeled the effects of cpd using all subjects that had a measurement, regardless if they did not have measurements for other biomarkers. The Fagerstrom Index scores were grouped into three categories for descriptive purposes (0–3 points: Low; 4–5 points: medium and ≥6 points: high), and two categories (0–6 points: Low/moderate dependence; 7–10 points: High dependence) in odds ratio calculations. The response categories for a component of the Fagerstrom Index, the time to first cigarette after waking up, are ≤ 5 minutes, 6–30 minutes, 31–60 minutes, ≥ 60 minutes. These were then collapsed into two categories (≤30 minutes vs. > 30 minutes) for odds ratio calculations. Smokers with low glucuronidation capacity are considered at increased risk of lung cancer, and we therefore tested the third aim by comparing NNAL-Gluc/NNAL ratios between smokers of mentholated and nonmentholated cigarettes.
RESULTS
Subject characteristics
Table 1 shows the smoking characteristics of the subjects by race and sex including mean years smoked, cigarettes per day, percent menthol smokers, FTND scores, and the time between waking up and the first cigarette smoked. There were no significant differences in the years of smoking between black and white subjects. About 86% of black subjects smoked menthol cigarettes while 28% of whites smoked menthol (P<0.01). Whites smoked significantly more menthol and nonmenthol cigarettes per day, respectively, than blacks (P<0.01). There were no significant differences in FTND categories between blacks and whites, whereas more whites reported smoking their first cigarette ≥30 minutes after waking up (P=.05).
Table 1.
Smoking characteristics by race and sex
| Black Men | Black women | White Men | White Women | |
|---|---|---|---|---|
| N=124 | N=113 | N=134 | N=154 | |
| Years smoked | 18.6±9.8 | 18.0±8.9 | 16.4±10.5 | 16.0±10.3 |
| Menthol (%)1 | 111 (90) | 93 (82) | 33 (25) | 47 (31) |
| Cigarettes per day1 | 16.0±7.9 | 16.1±9.0 | 22.5 ±12.2 | 19.0±8.4 |
| Nonmenthol1 | 18.8±9.0 | 13.5±6.1 | 23.7±13.3 | 19.7±9.6 |
| Menthol1 | 14.9±8.2 | 13.7±7.0 | 21.9±9.0 | 19.8±7.5 |
| FTND | ||||
| Low | 16 (27) | 19 (38) | 22 (28) | 36 (40) |
| Medium | 21 (36) | 11 (22) | 20 (26) | 29 (32) |
| High | 22 (37) | 20 (40) | 36 (46) | 26 (29) |
| Time since first cigarette2 | ||||
| <5 minutes | 25 (43) | 21 (43) | 31 (40) | 30 (33) |
| 6–30 minutes | 23 (40) | 15 (29) | 23 (29) | 31 (34) |
| 31–60 | 5 (9) | 4 (8) | 16 (21) | 19 (21) |
| >60 minutes | 5 (9) | 10 (20) | 8 (10) | 12 (13) |
P<0.01 for differences between black men and women combined vs. white men and women combined.
P=0.05 for differences between black men and women combined vs. white men and women combined.
Menthol and smoking exposure
Table 2 compares the mean concentrations of cigarette smoke metabolites between smokers of mentholated cigarettes and non-mentholated cigarettes. There were no significant differences in the mean concentrations of all cigarette smoke metabolites between menthol and nonmenthol smokers in both blacks and whites, after adjustment for sex and other factors. In all models, except for SCN in whites, sex was not a significant predictor of biomarker levels. White women had significantly higher adjusted SCN levels than white men.
Table 2.
Differences in mean levels of cotinine, thiocyanate, and total NNAL levels by cigarette type
| Blacks | Whites | All Subjects | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Metabolite | N | Menthol | N | Non-menthol | P-value | N | Menthol | N | Non-menthol | P-value | N | Menthol | N | Non-menthol | P-value |
| Plasma cotinine(ng/ml) | 186 | 389±261 | 31 | 348±261 | 0.09 | 69 | 323±220 | 195 | 328±248 | 0.56 | 255 | 371±252 | 226 | 330±249 | 0.49 |
| Urinary Cotinine (μg) | 194 | 4418±42 | 30 | 4206±38 | 0.19 | 76 | 3807±39 | 200 | 4191±46 | 0.51 | 270 | 4246±41 | 230 | 4193±45 | 0.97 |
| 29 | 99 | 08 | 29 | 43 | 32 | ||||||||||
| SCN (μm/L) | 168 | 162±48 | 93 | 155±49 | 0.33 | 59 | 176±47 | 165 | 169±50 | 0.97 | 227 | 166±48 | 193 | 167±50 | 0.34 |
| NNAL+NNAL-Gluc (pmol/mg creatinine) | 50 | 3.0±2.3 | 11 | 3.2±1.4 | 0.43 | 17 | 2.7±1.3 | 69 | 3.2±2.3 | 0.44 | 67 | 2.9±2.1 | 80 | 3.2±2.2 | 0.23 |
P-values adjusted for age, BMI, cigarettes per day2, race, and sex (all subject models).
Menthol and nicotine dependence
The association between high FTND scores and menthol was 1.1 (95% CI 0.6–2.1, Table 3). In multivariate analysis, younger age was the only significant predictor of high nicotine dependence scores. The association between smoking within the first 30 minutes after waking up and menthol was 2.1 (95% CI 0.96–3.8). Race was not a significant predictor in these models. Menthol was not a significant predictor of daily cigarette amount, or heavy smoking (OR = 0.8, 95% CI 0.5–1.4) after adjusting for race, sex and other factors. In race specific models, the inverse association of menthol with heavy smoking was slightly greater in blacks (OR = 0.702, 95% CI 0.144--3.426) than in whites (OR = 0.855, 95% CI 0.459--1.591).
Table 3.
Association between high nicotine dependence and menthol cigarettes
| Measure | Menthol | Nonmenthol | OR | 95% CI |
|---|---|---|---|---|
| Low/Medium FTND | 96 (45) | 56 (46) | 1 | |
| High FTND | 78 (55) | 48 (53) | 1.1 | 0.6, 2.1 |
| TTF>30′ | 26 (21%) | 53 (34%) | 1 | |
| TTF ≤30′ | 98 (79%) | 102 (66%) | 2.1 | 0.96, 3.8 |
The FTND and the time to first cigarette after waking were moderately correlated with levels of plasma cotinine (r=0.28, P<0.01; r=0.26, P<0.01), urinary cotinine/creatinine (r = 0.27, P<0.01; r=0.26, P<0.01) and total NNAL (r=0.21, P=0.08;r=0.15, P=0.23).
When subjects were asked about their reasons for not quitting, the responses were similar between menthol and nonmenthol smokers. Similar percentages reported that it was a nervous habit, they enjoyed smoking too much, the craving was too great, and fear of weight gain (data not shown). The only difference in reported reason for continued smoking was that more menthol smokers “never thought about quitting” than nonmenthol smokers (17% vs. 3.6%).
Menthol and NNAL glucuronidation
Table 4 compares the race-specific differences in the ratio of NNAL-Gluc/NNAL levels between smokers of mentholated and nonmentholated cigarettes. The mean substrate ratio was 34% lower in whites (P<0.01) and 22% lower in blacks. The difference in blacks did not reach statistical significance. For all subjects combined, the difference was statistically significant after controlling for race and other factors.
Table 4.
NNAL-G/NNAL ratio levels by race and menthol status
| Black | White* | All Subjects* | |||||
|---|---|---|---|---|---|---|---|
| Menthol | Non-Menthol | Menthol | Non-Menthol | Menthol | Non-Menthol | ||
| N=50 | N=11 | N=17 | N=69 | N=67 | N=80 | ||
|
| |||||||
| NNAL-G/NNAL | 3.1±1.7 | 4.0±2.1 | 2.5±1.1 | 3.8±2.6 | 3.0±1.6 | 3.8±2.5 | |
P<0.05. Adjusted for age, race (all subjects model), sex, education and cigarettes/day.
Menthol and NNAL glucuronidation in vitro
The inhibitory effects of menthol on NNAL O-glucuronidation and N-glucuronidation were assessed in three human liver microsomes. Figure 1 are representative LC-MS/MS MRM chromatograms for determination of NNAL-O-glucuronide and NNAL-N-glucuronide and NNAL in human liver microsome reacted with NNAL. NNAL-O-glucuronide and NNAL-N-glucuronide was detected by transition m/z 386→210 with retention times of 1.03 min and 2.09 min, respectively (Figure 1A). NNAL was detected by transition m/z 210→93 at 0.73 min (Figure 1 B). Menthol inhibit NNAL O-glucuronidation with IC50 values of 0.41±0.10 mM, inhibit NNAL N-glucuronidation with IC50 values of 0.26 ± 0.04 mM. Representative NNAL glucuronidation inhibition profiles in human liver microsome from one subject are presented in Figure 2. Figure 2A and 2B shows NNAL-O-glucuronide and NNAL-N-glucuronide formation in human liver microsome are decreased with increasing concentration of menthol.
Figure 2.
DISCUSSION
The pooled odds ratio (OR) from four case-control studies of lung cancer associated with menthol vs. nonmenthol cigarettes was 0.93 (95% confidence interval 0.82–1.05) (4). Menthol was not associated with an increased risk for other cancers (30,31). Menthol is not pyrolized during tobacco combustion (http://tobaccodocuments.org/product_design/504331475-1477.html), and does not induce tumors in animals via intraperitoneal injection (32) or drinking water supplementation (24). Menthol may not be a direct carcinogen or co-carcinogen, but it causes several pharmacologic and physiological effects that may affect cancer risk (33). Despite the lack of increased risk in the case-control studies, the effect size and statistical power to detect differences of one type of cigarette relative to another is likely to be small. However even a small relative effect of menthol could cause substantial numbers of cancers since millions of Americans smoke menthol cigarettes.
Consequently, biomarker and mechanistic studies are seemingly important tools for indirectly assessing possible risks. One of the limitations of studying the effects of menthol has been separating its effects from race. The majority of blacks who smoke prefer menthol, and studies of smoking topography or cotinine levels may have controlled for race but did not examine the race-specific effects of menthol (34–36). The current study examined the race-specific levels of several tobacco smoke biomarkers between menthol and nonmenthol smokers. We found no significant differences in mean cotinine and thiocyanate levels.
A limitation of the study is that it included subjects who smoked at least five cigarettes per day. The mean cotinine levels were higher than that reported for NHANES data (37), where about 25% of smokers reported smoking 7 or fewer cigarettes daily. The current study therefore does not address possible differences in biomarker levels by menthol status among very light smokers. We observed no significant differences in the urinary levels of the lung carcinogen NNAL between menthol and nonmenthol smokers in race-specific analyses, although the number of blacks who smoked nonmenthol cigarettes was relatively small and the differences in NNAL by menthol status was not significant. Assuming the same effect size and variances that were observed, the study would have required about 6 times the number of nonmenthol black smokers to detect significant differences. However, if the effect size is similar to that what was observed in whites, much smaller numbers would be needed.
Menthol has been studied in relation to increased addiction to nicotine. In a two-week randomized pharmacokinetic crossover study of 14 smokers who switched from menthol to nonmenthol or nonmenthol to menthol, menthol was on average unrelated to blood levels of unlabelled nicotine (14). The effect of menthol on behavioral measures of nicotine dependence such as the FTND was negligible in adolescent smokers (38). The current study showed similar findings in adult smokers. It has been suggested that the amount of time between waking up and smoking the first cigarette is possibly a better measure of nicotine dependence than smoking amount or the FTND since it was shown to be a better predictor of plasma cotinine concentrations than daily smoking amount in adults (39). However, in our data, the correlations of cotinine (both plasma and urinary) were very similar between cigarettes per day, time since waking and FTND. We did observe that menthol smokers were more likely to smoke cigarettes within 30 minutes after waking up than nonmenthol smokers, which is similar to findings in the adolescent smoker study, but differs from the Community Intervention Trial for Smoking Cessation (COMMIT) which found a longer time to first cigarette after waking for menthol smokers (16). The literature is inconsistent in this area and more studies might be helpful to understand this relationship. Menthol may inhibit quitting (19, 22), although other large scale studies show similar quit rates between menthol and nonmenthol smokers (17).
Another limitation is the interpretation of these analyses is that menthol content varies by cigarette brand, and younger smokers have been reported to smoke menthol brands with lower menthol content than older menthol smokers (40). In the present study, cigarettes were classified as menthol or nonmenthol, and therefore the magnitude of the effects (or lack thereof) associated with menthol reported here may not necessarily be generalizeable to all smokers.
We previously reported no racial differences in the ratio of NNAL-Gluc/NNAL levels in men, although in a subgroup of nine women who had a very high NNAL-Gluc/NNAL ratio (≥6), eight were white (29). We examined the cigarette brands of these women and found that only one subject was a menthol smoker so it is possible that the racial differences in NNAL glucuronidation in women could be attributed to menthol.
In the current study, menthol smokers had lower urinary ratios of NNAL-Gluc/NNAL than nonmenthol smokers, and menthol inhibited the glucuronidation of both NNAL-N-Gluc and NNAL-O-Gluc formation in vitro. These effects might be mediated by UGT2B10, which is the major enzyme involved in the N-glucuronidation of NNAL (41), and by UGT2B17 and UGT2B7 which are the major enzymes involved in NNAL O-glucuronidation (42, 43). While UGT2B7 genotype was not associated with human liver microsomal glucuronidation activity against menthol (44), in vitro studies have demonstrated that UGT2B7 is active against menthol and could be potentially inhibited by this substrate (45,46). The potential exists that menthol could therefore act as a substrate and inhibitor of other UGTs as well. Studies by Benowitz et al have demonstrated that menthol significantly inhibits nicotine-glucuronide formation in vivo (14). Since UGT2B10 is the major enzyme responsible for the N-glucuronidation of both nicotine and NNAL, it is likely that UGT2B10 may be the target for the inhibitory effects of menthol on nicotine and NNAL glucuronidation activity in vivo. Studies examining the interaction between menthol and NNAL/nicotine glucuronidation in cells specifically over-expressing UGTs 2B7, 2B10 and 2B17 are currently planned. The major limitation of in vitro studies that attempt to identify the underlying mechanisms in epidemiologic data is that it is difficult to mimic in vivo conditions experimentally. In particular the human liver microsomes are not equivalent to ER in intact cells and do not interact similarly with other cellular components and vascular supply, and nutrients. The levels of exposure in the in vitro model may not reflect in vivo exposure. Despite these limitations, cellular pathways are often activated similarly in both in vitro and in vivo systems and human liver microsomes are commonly used to screen for drug interactions in pharmacologic research (47).
In summary, these data indicate that menthol is not associated with a higher exposure to tobacco smoke carcinogens but the findings on nicotine dependence are inconclusive. Menthol may not be more hazardous than other cigarette formulations for most smokers, although it cannot be ruled out at this time that some menthol smokers are possibly at increased risk of lung cancer due to selective inhibition of UGT enzymes.
References
- 1.Paschke T, Scherer G, Heller WD. Effects of ingredients on cigarette smoke composition and biological activity: a literature overview. Beitr Tabak Int. 2002;20:107–247. [Google Scholar]
- 2.Rodgman A. Some studies of the effects of additives on cigarette mainstream smoke properties. I Flavorants Beitr Tabak In. 2002;20:83–103. [Google Scholar]
- 3.Baker RR, Massey ED, Smith G. An overview of the effects of tobacco ingredients on smoke chemistry and toxicity. Food Chem Toxicol. 2004;42(Suppl):S53–83. doi: 10.1016/j.fct.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 4.Werley MS, Coggins CR, Lee PN. Possible effects on smokers of cigarette mentholation: a review of the evidence relating to key research questions. Regul Toxicol Pharmacol. 2007;47:189–203. doi: 10.1016/j.yrtph.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Garten S, Falkner RV. Role of mentholated cigarettes in increased nicotine dependence and greater risk of tobacco-attributable disease. Prev Med. 2004;38:793–8. doi: 10.1016/j.ypmed.2004.01.019. [DOI] [PubMed] [Google Scholar]
- 6.Hebert JR, Kabat GC. Menthol cigarette smoking and oesophageal cancer. Int J Epidemiol. 1989;18:37–44. doi: 10.1093/ije/18.1.37. [DOI] [PubMed] [Google Scholar]
- 7.Kabat GC, Hebert JR. Use of mentholated cigarettes and lung cancer risk. Cancer Res. 1991;51:6510–3. [PubMed] [Google Scholar]
- 8.Sydney S, Tekawa IS, Friedman GD, Sadler MC, Tashkin DP. Mentholated cigarette use and lung cancer. Arch Intern Med. 1995;55:727–732. [PubMed] [Google Scholar]
- 9.Carpenter CL, Jarvik ME, Morgenstern H, McCarthy WJ, London SJ. Mentholated cigarette smoking and lung-cancer risk. Ann Epidemiol. 1999;9:114–20. doi: 10.1016/s1047-2797(98)00042-8. [DOI] [PubMed] [Google Scholar]
- 10.Brooks DR, Palmer JR, Strom BL, Rosenberg L. Menthol cigarettes and risk of lung cancer. Am J Epidemiol. 2003;158:609–16. doi: 10.1093/aje/kwg182. [DOI] [PubMed] [Google Scholar]
- 11.Stellman SD, Chen Y, Muscat JE, et al. Lung cancer risk in white and black Americans. Ann Epidemiol. 2003;13:294–302. doi: 10.1016/s1047-2797(02)00420-9. [DOI] [PubMed] [Google Scholar]
- 12.Kreslake JM, Wayne GF, Alpert HR, Koh HK, Connolly GN. Tobacco Industry Control of Menthol in Cigarettes and Targeting of Adolescents and Young Adults. Am J Public Health. 2008 Jul; doi: 10.2105/AJPH.2007.125542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Azzi C, Zhang J, Purdon CH, et al. Permeation and reservoir formation of 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) and benzo[a]pyrene (B[a]P) across porcine esophageal tissue in the presence of ethanol and menthol. Carcinogenesis. 2006;27:137–45. doi: 10.1093/carcin/bgi173. [DOI] [PubMed] [Google Scholar]
- 14.Benowitz NL, Herrera B, Jacob P., 3rd Mentholated cigarette smoking inhibits nicotine metabolism. J Pharmacol Exp Ther. 2004;310:1208–15. doi: 10.1124/jpet.104.066902. [DOI] [PubMed] [Google Scholar]
- 15.Henningfield JE, Benowitz NL, Ahijevych K, Garrett BE, Connolly GN, Wayne GF. Does menthol enhance the addictiveness of cigarettes? An agenda for research Nicotine Tob Res. 2003;5:9–11. doi: 10.1080/1462220031000070543. [DOI] [PubMed] [Google Scholar]
- 16.Hyland A, Garten S, Giovino GA, Cummings KM. Mentholated cigarettes and smoking cessation: findings from COMMIT. Community Intervention Trial for Smoking. Cessation Tob Control. 2002;11:135–9. doi: 10.1136/tc.11.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muscat JE, Richie JP, Jr, Stellman SD. Mentholated cigarettes and smoking habits in whites and blacks. Tob Control. 2002;11:368–71. doi: 10.1136/tc.11.4.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris KJ, Okuyemi KS, Catley D, Mayo MS, Ge B, Ahluwalia JS. Predictors of smoking cessation among African-Americans enrolled in a randomized controlled trial of bupropion. Prev Med. 2004;38:498–502. doi: 10.1016/j.ypmed.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 19.Pletcher MJ, Hulley BJ, Houston T, Kiefe CI, Benowitz N, Sidney S. Menthol cigarettes, smoking cessation, atherosclerosis, and pulmonary function: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Arch Intern Med. 2006;166:1915–22. doi: 10.1001/archinte.166.17.1915. [DOI] [PubMed] [Google Scholar]
- 20.Okuyemi KS, Faseru B, Sanderson Cox L, Bronars CA, Ahluwalia JS. Relationship between menthol cigarettes and smoking cessation among African American light smokers. Addiction. 2007;102:1979–86. doi: 10.1111/j.1360-0443.2007.02010.x. [DOI] [PubMed] [Google Scholar]
- 21.Fu SS, Okuyemi KS, Partin MR, et al. Menthol cigarettes and smoking cessation during an aided quit attempt. Nicotine Tob Res. 2008;10:457–62. doi: 10.1080/14622200801901914. [DOI] [PubMed] [Google Scholar]
- 22.Giovino GA, Sidney S, Gfroerer JC, O’Malley PM, Allen JA, Richter PA, Cummings KM. Epidemiology of menthol cigarette use. Nicotine Tob Res. 2004;6(Suppl 1):S67–81. doi: 10.1080/14622203710001649696. [DOI] [PubMed] [Google Scholar]
- 23.Clark PI, Gardiner PS, Djordjevic MV, Leischow SJ, Robinson RG. Menthol cigarettes: setting the research agenda. Nicotine Tob Res. 2004;6(Suppl 1):S5–9. doi: 10.1080/14622200310001649441. [DOI] [PubMed] [Google Scholar]
- 24.Richie JP, Jr, Carmella SG, Muscat JE, Scott DG, Akerkar SA, Hecht SS. Differences in the urinary metabolites of the tobacco-specific lung carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone in black and white smokers. Cancer Epidemiol Biomarkers Prev. 1997;6:783–90. [PubMed] [Google Scholar]
- 25.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 26.Wiener D, Fang JL, Dossett N, Lazarus P. Correlation between UDP-glucuronosyltransferase genotypes and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone glucuronidation phenotype in human liver microsomes. Cancer Res. 2004;64:1190–6. doi: 10.1158/0008-5472.can-03-3219. [DOI] [PubMed] [Google Scholar]
- 27.Coughtrie MW, Burchell B, Bend JR. A general assay for UDP glucuronosyltransferase activity using polar amino-cyano stationary phase HPLC and UDP[U-14C]glucuronic acid. Anal Biochem. 1986;159:198–205. doi: 10.1016/0003-2697(86)90328-3. [DOI] [PubMed] [Google Scholar]
- 28.Chen G, Dellinger RW, Sun D, Spratt TE, Lazarus P. Glucuronidation of tobacco-specific nitrosamines by UGT2B10. Drug Metab Dispos. 2008;36:824–30. doi: 10.1124/dmd.107.019406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muscat JE, Djordjevic MV, Colosimo S, Stellman SD, Richie JP., Jr Racial differences in exposure and glucuronidation of the tobacco-specific carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) Cancer. 2005;103:1420–6. doi: 10.1002/cncr.20953. [DOI] [PubMed] [Google Scholar]
- 30.Friedman GD, Sadler M, Tekawa IS, Sidney S. Mentholated cigarettes and non-lung smoking related cancers in California, USA. J Epidemiol Community Health. 1998;52:202. doi: 10.1136/jech.52.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murray RP, Connett JE, Skeans MA, Tashkin DP. Menthol cigarettes and health risks in Lung Health Study data. Nicotine Tob Res. 2007;9:101–7. doi: 10.1080/14622200601078418. [DOI] [PubMed] [Google Scholar]
- 32.Stoner GD, Shimkin MB, Kniazeff AJ, Weisburger JH, Weisburger EK, Gori GB. Test for carcinogenicity of food additives and chemotherapeutic agents by the pulmonary tumor response in strain A mice. Cancer Res. 1973;33:3069–85. [PubMed] [Google Scholar]
- 33.Ahijevych K, Garrett BE. Menthol pharmacology and its potential impact on cigarette smoking behavior. Nicotine Tob Res. 2004;6(Suppl 1):S17–28. doi: 10.1080/14622200310001649469. [DOI] [PubMed] [Google Scholar]
- 34.Clark PI, Gautam S, Gerson LW. Effect of menthol cigarettes on biochemical markers of smoke exposure among black and white smokers. Chest. 1996;110:1194–8. doi: 10.1378/chest.110.5.1194. [DOI] [PubMed] [Google Scholar]
- 35.Ahijevych K, Gillespie J. Nicotine dependence and smoking topography among black and white women. Res Nurs Health. 1997;20:505–14. doi: 10.1002/(sici)1098-240x(199712)20:6<505::aid-nur5>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 36.Jarvik ME, Tashkin DP, Caskey NH, McCarthy WJ, Rosenblatt MR. Mentholated cigarettes decrease puff volume of smoke and increase carbon monoxide absorption. Physiol Behav. 1994;56:563–70. doi: 10.1016/0031-9384(94)90302-6. [DOI] [PubMed] [Google Scholar]
- 37.Caraballo RS, Giovino GA, Pechacek TF, Mowery PD, Richter PA, Strauss WJ, Sharp DJ, Eriksen MP, Pirkle JL, Maurer KR. Racial and ethnic differences in serum cotinine levels of cigarette smokers:Third National Health and Nutrition Examination Survey, 1988–1991. JAMA. 1998;280:135–9. doi: 10.1001/jama.280.2.135. [DOI] [PubMed] [Google Scholar]
- 38.Collins CC, Moolchan ET. Shorter time to first cigarette of the day in menthol adolescent cigarette smokers. Addict Behav. 2006:31. doi: 10.1016/j.addbeh.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 39.Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84:791–9. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 40.Kreslake JM, Ferris Wayne G, Alpert HR, Koh HK, Connolly GN. Tobacco Industry Control of Menthol in Cigarettes and Targeting of Adolescents and Young Adults. Am J Public Health. 2008 Jul 16; doi: 10.2105/AJPH.2007.125542. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ren Q, Murphy SE, Zheng Z, Lazarus P. O-Glucuronidation of the lung carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL) by human UDP-glucuronosyltransferases 2B7 and 1A9. Drug Metab Dispos. 2000;28:1352–60. [PubMed] [Google Scholar]
- 42.Lazarus P, Zheng Y, Aaron Runkle E, Muscat JE, Wiener D. Genotype-phenotype correlation between the polymorphic UGT2B17 gene deletion and NNAL glucuronidation activities in human liver microsomes. Pharmacogenet Genomics. 2005;15:769–78. doi: 10.1097/01.fpc.0000175596.52443.ef. [DOI] [PubMed] [Google Scholar]
- 43.Chen G, Blevins-Primeau AS, Dellinger RW, Muscat JE, Lazarus P. Glucuronidation of nicotine and cotinine by UGT2B10: loss of function by the UGT2B10 Codon 67 (Asp>Tyr) polymorphism. Cancer Res. 2007;67:9024–9. doi: 10.1158/0008-5472.CAN-07-2245. [DOI] [PubMed] [Google Scholar]
- 44.Bhasker CR, McKinnon W, Stone A, Lo AC, Kubota T, Ishizaki T, Miners JO. Genetic polymorphism of UDP-glucuronosyltransferase 2B7 (UGT2B7) at amino acid 268: ethnic diversity of alleles and potential clinical significance. Pharmacogenetics. 2000;10:679–85. doi: 10.1097/00008571-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 45.Jin C-J, Miners JO, Lillywhite KJ, Mackenzie PI. Complementary deoxyribonucleic acid cloning and expression of a human liver uridine diphosphate–glucuronosyltransferase glucuronidating carboxylic acid-containing drugs. J Pharmacol Exp Ther. 1993;264:475–479. [PubMed] [Google Scholar]
- 46.Ritter JK, Sheen YY, Owens IS. Cloning and expression of human liver UDP-glucuronosyltransferase in COS-1 cells. J Biol Chem. 1989;265:7900–7906. [PubMed] [Google Scholar]
- 47.Devlin RB, Frampton ML, Ghio AJ. In vitro studies: What is their role in toxicology? Experimental and Toxicologic Pathology. 2005;57:183–188. doi: 10.1016/j.etp.2005.05.018. [DOI] [PubMed] [Google Scholar]