Abstract
Background:
HIV-1 infection of the CSF space is nearly universal in untreated systemic infection, and correlates strongly with intrathecal and systemic immunoactivation and CSF pleocytosis. Based on the potential immunomodulatory and antiviral properties of HMG-CoA reductase inhibitors (statins), we examined the effect of atorvastatin on CSF HIV-1 infection and associated CSF abnormalities in a small pilot study.
Methods:
Seven male HIV-1-infected, antiretroviral-naïve subjects with a mean blood CD4+ T cell count of 473 cells/μL were studied in an open-label, single-arm pilot study to assess the effects of 80 mg atorvastatin daily for 8 weeks. The primary endpoint was the change in CSF HIV-1 RNA levels, both absolutely and relative to plasma HIV-1 RNA, at 4 and 8 weeks of treatment. Other outcome measures included CSF white blood cell counts and neopterin concentrations as indices of intrathecal immunoactivation, and blood HIV-1 RNA levels, neopterin concentrations, and T lymphocyte counts. Effects on blood lipids were used to monitor the established biologic effects of atorvastatin and treatment adherence.
Results:
No significant changes in CSF virologic and inflammatory indices or in systemic HIV-1 infection were observed during atorvastatin treatment despite potent reduction of blood lipids.
Conclusion:
Atorvastatin showed no appreciable effect on CSF HIV-1 infection or intrathecal immunoactivation in this small uncontrolled study and thus appears to have little promise as an immunomodulatory adjuvant therapy for CNS HIV-1 infection, at least in neuroasymptomatic subjects with preserved CD4+ T cell counts.
GLOSSARY
- ADC
= AIDS dementia complex;
- ART
= antiretroviral therapy;
- HIVE
= HIV encephalitis;
- HMG-CoA
= 3-hydroxy-3-methylglutaryl coenzyme A;
- LP
= lumbar puncture;
- WBC
= white blood cell.
HIV-1 infection of the CSF space is a nearly universal aspect of untreated HIV-1 infection, from primary exposure through advanced AIDS.1 Though usually clinically silent and seemingly benign, in some individuals infection evolves to more invasive HIV encephalitis (HIVE) accompanied by the cognitive and motor function abnormalities of the AIDS dementia complex (ADC).2 While combination antiretroviral therapy (ART) is effective in suppressing CSF infection in most patients, even in the setting of drug resistance,3 the effect of HIV-1 on the CNS remains a clinical problem. Patients not treated with ART still present with ADC. Moreover, in concert with the increased survival related to therapy, the prevalence of milder neurocognitive impairment may have actually increased,4 perhaps in part related to early subclinical brain injury or ongoing injury despite treatment. This has led to the search for adjuvant modes of treatment to mitigate brain injury by interfering with virus-driven immunopathologic pathways downstream from infection.5
We undertook this pilot study to test whether atorvastatin, a 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitor, might be a candidate adjuvant treatment through modulation of CSF HIV-1 infection and intrathecal immunoactivation. In addition to impairing cholesterol synthesis, HMG-CoA reductase inhibitors reduce biosynthesis of isoprenoid pyrophosphatases involved in the post-translational prenylation of key regulatory proteins involved in immune responses.6 On this basis statins have been recommended for clinical trials in a number of immunologic diseases. Conflicting evidence suggests statins may also more directly inhibit HIV-1 replication.7
METHODS
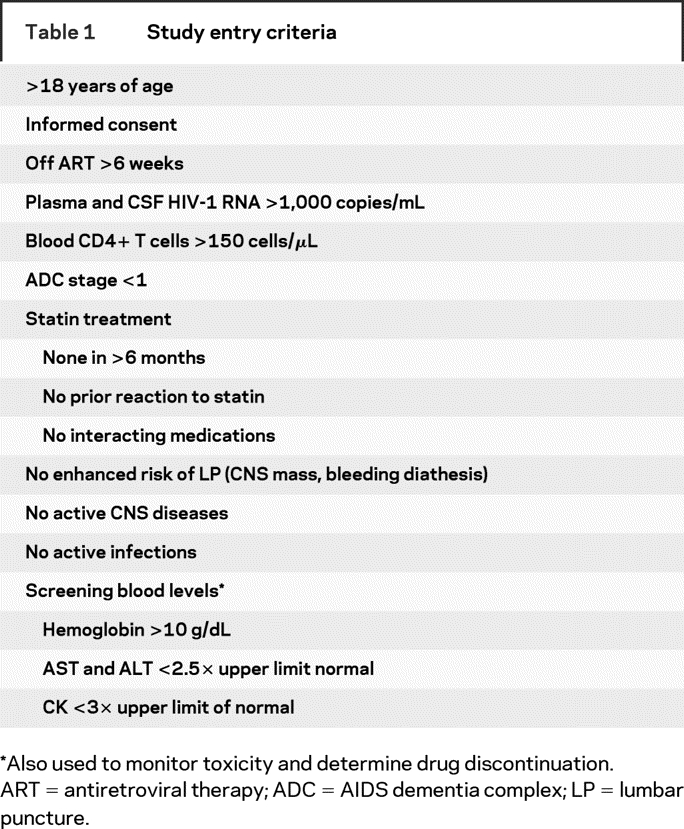
This open-label, uncontrolled pilot study examined the effects of atorvastatin at the high end of standard dosage for 8 weeks. Subject entry criteria are summarized in table 1. Primary outcomes were the changes from baseline in CSF HIV-1 RNA levels and in the difference between plasma and CSF HIV-1 log10 RNA levels. Secondary outcomes included changes in CSF white blood cell (WBC) counts and neopterin concentrations, and in blood HIV-1 RNA and neopterin levels. We also measured effects on blood CD4+ and CD8+ T cells and on the CSF:blood albumin ratio as an index of blood–brain barrier integrity.8 Serum cholesterol, LDL cholesterol, and triglycerides were used to monitor the known biologic effects of atorvastatin and treatment adherence. This study was approved by the University of California San Francisco Committee on Human Research, and informed consent was obtained from all subjects.
Table 1 Study entry criteria
After meeting eligibility criteria, subjects began atorvastatin 80 mg/day for the next 8 weeks. At baseline, weeks 4 and 8, and after a 6-week drug washout period, study visits included a lumbar puncture (LP) and concurrent blood sampling using previously described methods.3,5 HIV-1 RNA and neopterin concentrations were measured in cell-free CSF and plasma as previously described,5 while other measurements were performed in the San Francisco General Hospital Clinical Laboratories using standard clinical methods.
Changes from baseline to subsequent study visits were analyzed by simple paired t tests and repeated measures analysis of variance with Dunnet post hoc comparison. All p values were two-sided with values <0.05 considered significant in this initial comparison. Statistical analyses used Prism 5 (GraphPad Software Inc, San Diego, CA) while power calculations used GraphPad StatMate 2.00.
RESULTS
Of 16 subjects screened, 8 were excluded because of low CSF HIV-1 RNA (n = 5), elevated serum transaminase (n = 3), or elevated serum CK (n = 1). The remaining 8 subjects entered the study and were prescribed atorvastatin. One electively discontinued participation at week 4; his blood lipid profiles showed no drug effect, and he was excluded from analysis for therapy nonadherence.
Table 2 summarizes the baseline characteristics of the remaining seven subjects. Six completed the study without adverse event. One subject discontinued atorvastatin from week 4 (included in analysis) through week 8 (excluded from analysis) of the study due to elevations in serum transaminases, but continued study participation through the washout period and week 14 visit. For repeated measures analysis of variance analysis, his 4-week results were carried forward and included in the 8-week data.
Table 2 Baseline subject characteristics

Changes from baseline in the outcome measures are shown in the figure. There were no significant changes in the virological measures: plasma HIV-1 RNA remained steady (A), and a minor but insignificant reduction in the mean CSF HIV-1 RNA (B) and increase in the plasma:CSF log10 difference (C) were noted. There were no significant changes in blood CD4+ and CD8+ T cells or in blood–brain barrier permeability to albumin (D–F) or in CSF WBC count (G) and neopterin (H) or in blood neopterin (I). The absence of virologic and anti-inflammatory effects contrasted with substantial reductions in serum cholesterol, LDL, and triglycerides (J–L) that returned to baseline values during the washout.
Figure Changes in viral, immune, and lipid measurements during atorvastatin treatment
Panels show the mean changes from baseline and 95% CIs for (A) plasma HIV-1 RNA, (B) CSF HIV-1 RNA, and (C) plasma:CSF log10 difference in HIV-1 RNA concentrations; (D) blood CD4+ T cells, (E) blood CD8+ T cells, and (F) CSF:plasma albumin ratio; (G) CSF WBC counts; (H) blood neopterin, and (I) CSF neopterin concentrations; and serum (J) cholesterol, (K) LDL cholesterol, and (L) triglyceride levels. The designations of significance (*p < 0.05; **p < 0.01) derive from paired t test using observed values. Analysis of variance analysis with post hoc testing showed similar results with significant changes confined to the lipid measurements.
DISCUSSION
This pilot study was undertaken as an initial step in exploring statins as an adjuvant treatment of CNS HIV-1 infection, and more particularly in assessing whether atorvastatin might reduce CSF HIV-1 infection and intrathecal immunoactivation through its immunomodulatory properties. Our underlying mechanistic hypotheses involved the following reasoning: 1) if CSF levels of HIV-1 RNA reflect local viral production by trafficking short-lived CD4+ T cells,9 and 2) if both traffic of these cells into the CSF and their viral output are enhanced by immune activation,5 and 3) if atorvastatin is capable of down-modulating these processes, then 4) atorvastatin should reduce CSF HIV-1 RNA concentrations absolutely and in relation to the plasma viral load. We noted neither of these latter effects: CSF and plasma HIV-1 RNA (and their ratio) were not significantly altered by treatment, despite potent effects of atorvastatin on blood lipids.
We also hypothesized that atorvastatin would mitigate the characteristic CNS immune activation of chronic HIV-1 infection, and would reduce the increased CSF WBC counts and elevations in CSF neopterin, a soluble biomarker of intrathecal immune activation.5,10 However, these markers also remained unchanged through the course of treatment. Our group also recently completed a randomized, placebo-controlled pilot study focused on the effect of atorvastatin on T cell activation in blood (n = 10); this also failed to show an effect (unpublished data). Thus, while atorvastatin can exert immunomodulatory activity in vivo, this either does not counteract the mechanisms operating in HIV-1 infection or is too weak in relation to this potent HIV-1 effect.
This pilot study was subject to the inherent limitations of its size, duration, and absence of an untreated control group for comparison, raising concern for Type II error. A small though insignificant decrease in CSF HIV-1 and increase in the plasma:CSF difference (figure, B and C) were noted, and we cannot fully dismiss the possibility that the study was underpowered to detect a mild effect of the drug or that CSF HIV-1 would decline further with longer exposure. However, if the observed CSF virologic changes were indeed real, based on these pilot results a controlled study would require 50–70 subjects in each of two arms to have an 80% power to detect this difference between groups. Moreover, even if they had proved significant, these effects were too weak to justify a study of this size, especially in the absence of an effect on CSF WBC or neopterin levels or on systemic HIV-1 replication—particularly when viewed in comparison to the potent effects of combination ART on these variables.3
If CNS immune activation is an important component in the pathogenesis of ADC/HIVE, our study suggests that statin therapy has little promise as an immunomodulatory adjuvant therapy in this setting.
Address correspondence and reprint requests to Dr. Richard W. Price, Neurology Service, Rm 4M62, San Francisco General Hospital (SFGH), 1001 Potrero Avenue, San Francisco, CA 94117 rwprice@sfgh.ucsf.edu
Supported by National Institutes of Health R01 MH62701 and K23 MH074466, and the UCSF/SFGH CTSI Clinical Research Center (CCRC) and the Biostatistics, Research Ethics and Design Program (BREAD) programs supported by UL1 RR024131.
Disclosure: The authors report no disclosures.
Received January 25, 2008. Accepted in final form May 5, 2008.
REFERENCES
- 1.Ellis RJ, Hsia K, Spector SA, et al. Cerebrospinal fluid human immunodeficiency virus type 1 RNA levels are elevated in neurocognitively impaired individuals with acquired immunodeficiency syndrome. HIV Neurobehavioral Research Center Group. Ann Neurol 1997;42:679–688. [DOI] [PubMed] [Google Scholar]
- 2.Navia BA, Jordan BD, Price RW. The AIDS dementia complex, I: clinical features. Ann Neurol 1986;19:517–524. [DOI] [PubMed] [Google Scholar]
- 3.Spudich S, Lollo N, Liegler T, Deeks SG, Price RW. Treatment benefit on cerebrospinal fluid HIV-1 levels in the setting of systemic virological suppression and failure. J Infect Dis 2006;194:1686–1696. [DOI] [PubMed] [Google Scholar]
- 4.Antinori A, Arendt G, Becker JT, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology 2007;69:1789–1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sinclair E, Ronquillo R, Lollo N, et al. Antiretroviral treatment effect on immune activation reduces cerebrospinal fluid HIV-1 infection. J Acquir Immune Defic Syndr 2008;47:544–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenwood J, Steinman L, Zamvil SS. Statin therapy and autoimmune disease: from protein prenylation to immunomodulation. Nat Rev Immunol 2006;6:358–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Negredo E, Clotet B, Puig J, et al. The effect of atorvastatin treatment on HIV-1-infected patients interrupting antiretroviral therapy. AIDS 2006;20:619–621. [DOI] [PubMed] [Google Scholar]
- 8.Tibbling G, Link H, Ohman S. Principles of albumin and IgG analyses in neurological disorders, I: establishment of reference values. Scand J Clin Lab Invest 1977;37:385–390. [DOI] [PubMed] [Google Scholar]
- 9.Harrington PR, Haas DW, Ritola K, Swanstrom R. Compartmentalized human immunodeficiency virus type 1 present in cerebrospinal fluid is produced by short-lived cells. J Virol 2005;79:7959–7966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wirleitner B, Schroecksnadel K, Winkler C, Fuchs D. Neopterin in HIV-1 infection. Mol Immunol 2005;42:183–194. [DOI] [PubMed] [Google Scholar]



