Abstract
Background: Consumption of liquid calories from beverages has increased in parallel with the obesity epidemic in the US population, but their causal relation remains unclear.
Objective: The objective of this study was to examine how changes in beverage consumption affect weight change among adults.
Design: This was a prospective study of 810 adults participating in the PREMIER trial, an 18-mo randomized, controlled, behavioral intervention trial. Measurements (weight, height, and 24-h dietary recall) were made at baseline, 6 mo, and 18 mo.
Results: Baseline mean intake of liquid calories was 356 kcal/d (19% of total energy intake). After potential confounders and intervention assignment were controlled for, a reduction in liquid calorie intake of 100 kcal/d was associated with a weight loss of 0.25 kg (95% CI: 0.11, 0.39; P < 0.001) at 6 mo and of 0.24 kg (95% CI: 0.06, 0.41; P = 0.008) at 18 mo. A reduction in liquid calorie intake had a stronger effect than did a reduction in solid calorie intake on weight loss. Of the individual beverages, only intake of sugar-sweetened beverages (SSBs) was significantly associated with weight change. A reduction in SSB intake of 1 serving/d was associated with a weight loss of 0.49 kg (95% CI: 0.11, 0.82; P = 0.006) at 6 mo and of 0.65 kg (95% CI: 0.22, 1.09; P = 0.003) at 18 mo.
Conclusions: These data support recommendations to limit liquid calorie intake among adults and to reduce SSB consumption as a means to accomplish weight loss or avoid excess weight gain. This trial was registered at clinicaltrials.gov as NCT00000616.
INTRODUCTION
It has been projected that 75% of US adults will be overweight or obese by 2015 (1). One factor contributing to this obesity epidemic may be an increased dietary energy intake from beverages. Today, Americans consume 150–300 more calories per day than they did 30 y ago, and caloric beverages account for ≈50% of this increase (2, 3). Energy intake from beverages currently represents 21% of total daily energy intake in the general American population (4). Evidence from short-term human studies suggests that calories consumed in liquid form (ie, liquid calories) have weak satiety properties and elicit poor energy compensation compared with calories from solid foods (ie, solid calories) (5–8). These results suggest that an increase in consumption of liquid calories may result in weight gain, and, conversely, that a reduction in liquid calorie intake may lead to weight loss. However, there is a scarcity of strong scientific evidence supporting these hypotheses, particularly from long-term prospective studies. This paucity of evidence has impeded policymaking.
The type of beverage may also influence body weight. For sugar-sweetened beverages (SSBs), some longitudinal studies suggest a positive association between consumption and body weight (9–14). However, many of these studies either failed to control for important confounding factors, such as physical activity, or used unreliable dietary assessment methods. Likewise, recent reviews on the topic had reached different conclusions: 2 (15, 16) proposed that the consumption of SSBs was positively associated with body weight, whereas 6 others (17–20) concluded that there was insufficient evidence. Some studies suggest that milk intake may aid voluntary weight loss (21–24), whereas others found the opposite effect or no effect (25–30).
The objectives of the present study were to determine 1) how changes in liquid calorie intake affect body weight, 2) whether liquid calories are more obesogenic than are solid calories, and 3) how changes in consumption of specific beverages affect body weight among adults.
SUBJECTS AND METHODS
Study population
PREMIER is a completed, 18-mo multicenter randomized trial designed to test the blood pressure–lowering effects of 2 multicomponent behavioral interventions in adults with prehypertension or stage 1 hypertension (a systolic blood pressure of 120–159 mm Hg and a diastolic blood pressure of 80–95 mm Hg). The cohort consisted of 810 men and women aged 25–79 y, recruited from 4 study centers (Baltimore, MD, Baton Rouge, LA, Durham, NC, and Portland, OR). Individuals who used antihypertensive medications, weight-loss medications, or oral steroids routinely were excluded. Other exclusion criteria included diabetes, a history of a cardiovascular event, congestive heart failure, current symptoms of angina or peripheral vascular disease by Rose Questionnaire, cancer diagnosis or treatment in past 2 y (except for nonmelanoma skin cancer), renal insufficiency, or a psychiatric hospitalization within the past 2 y. Detailed information regarding the study methods and main results can be found in our previous publications (31, 32). Eligible participants were randomly assigned to 1 of 3 groups: (A) an “Advice Only” comparison group that received information but no behavioral counseling on weight loss, increased physical activity, sodium reduction, and the DASH (Dietary Approaches to Stop Hypertension) dietary pattern (33); (B) a behavioral intervention group, termed “Established,” that received counseling on how to lose weight, increase physical activity, and reduce sodium intake; or (C) a behavioral intervention group, termed “Established Plus DASH,” that received counseling on the same lifestyle goals as the Established group along with counseling on the DASH dietary pattern. The weight-loss approaches in the Established group focused on increased physical activity and reduced energy intake. In contrast, the weight-loss approach in the Established Plus DASH group focused on increased physical activity, reduced energy intake, and substitution of fruit and vegetables for high-fat, high-calorie foods. Except for the advice to increase the intake of low-fat dairy products in the Established Plus DASH group, no other advice regarding beverage consumption was given to any of the groups. Regarding the contact pattern, participants in the Advice Only group received two 30-min individual advice sessions, one at randomization and the other after the 6-mo data collection. Both the Established and Established Plus DASH groups received behavioral interventions derived from the social cognitive theory. The intervention format and contact pattern of the 2 groups were identical: 14 group meetings were conducted weekly in the initial 14 wk; 6 group meetings were conducted every other week plus a single individual session in the next 14 wk; monthly group meetings and 3 quarterly individual counseling sessions were conducted in the last 48 wk. The PREMIER study was conducted from January 2000 through November 2002. All 810 study participants enrolled at baseline were included in this analysis.
Measurement of dietary and beverage intake
Dietary intake was measured by unannounced 24-h dietary recall conducted by telephone interviews. Two recalls (one on a weekday and the other on a weekend day) per participant were obtained at baseline and at 6 and 18 mo. A multiple-pass technique and portion size estimation aids were used. Intakes of nutrients and food groups were calculated by using the Nutrition Data System for Research, version NDS-R 1998 (University of Minnesota, Minneapolis, MN).
We divided beverages into 7 categories based on calorie content and nutritional composition: 1) SSBs (regular soft drinks, fruit drinks, fruit punch, or any other high-calorie beverage sweetened with sugar), 2) diet drinks (diet soda and other “diet” drinks sweetened with artificial sweeteners), 3) milk (whole milk, 2% reduced-fat milk, 1% low-fat milk, and skim milk), 4) 100% juice (100% fruit and vegetable juice), 5) coffee and tea with sugar (CTS: coffee and tea sweetened with sugar), 6) coffee and tea without sugar (CT: unsweetened coffee and tea or coffee and tea sweetened with artificial sweeteners), and 7) alcoholic beverages (beer, wine, spirits, and other alcoholic drinks). Each participant's daily nutrient, energy, and beverage intakes were calculated by taking the average of 2 recalls per time point. Liquid calorie intake was calculated as the sum of calories from the 7 beverage categories. Solid calorie intake was calculated by subtracting liquid calories from total calories.
Measurement of outcomes and covariates
Weight and height were measured with a calibrated scale and a wall-mounted stadiometer while the subjects were wearing light clothing and no shoes. Fitness was assessed using a 2-stage 10-min submaximal treadmill stress test and defined as the heart rate (beats/min) at a fixed workload (stage 2). Physical activity (estimated energy expenditure; in kcal · kg−1 · d−1) was assessed by using a 7-d diet recall questionnaire (34). Other data, such as age, sex, race-ethnicity, income, education, employment, marriage status, and smoking habits were collected at baseline.
Statistical analysis
All statistical analyses were performed by using STATA version 9.0 (Stata Corp, College Station, TX). Statistical significance was set at P ≤ 0.05 (2-tailed). The analyses were conducted by combining all participants and adding intervention assignment as a covariate in all models.
The 2 main exposures of interest were 1) changes in consumption of liquid calories and 2) changes in consumption of individual types of beverages, each assessed from baseline to 6 and 18 mo separately. Key outcome variables were weight changes from baseline to 6 and 18 mo. For the primary analysis, exposure and outcome variables were modeled as continuous variables. Additional analyses with exposures modeled as categorical variables were carried out to assess the patterns of dose response. In model 1, changes in consumption of solid and liquid calories were simultaneously included with adjustments for baseline age, sex, race, income, education, marital and employment status, body mass index (BMI; in kg/m2) status, intervention allocation, and concurrent changes in fitness and physical activity. In model 2 the primary exposure variable was percentage of liquid calories, and the model was adjusted for the same covariates as in model 1. In model 3, we assessed the role of individual beverages by including each type of beverage; in this model, we adjusted for total energy intake and the covariates included in model 1. Additional adjustment for smoking status (never, past, or current) and dietary factors such as fat and carbohydrate intakes and energy density did not change the results. Therefore, these variables were not included in the final models. Missing values were not imputed in primary analyses. In sensitivity analyses, we used the baseline observation carried forward method to assess the effect of missing values on study results. The study protocol was approved by the institutional review boards of each of the participating centers and was monitored by an external data safety committee.
RESULTS
Baseline characteristics and retention to follow-up
The baseline characteristics of the participants are shown in Table 1. There were 62% women and 34% African Americans, with an average age of 50 y. Fifty-seven percent of participants had college degrees or above, 65% were married, and 70% had a household income >$45,000/y. Most of the participants were current nonsmokers (95%), 29% were overweight (BMI: 25–29.9), and 65% were obese (BMI ≥ 30). At 18 mo, 94% of the participants had a weight measurement, and 90% had at least one dietary recall.
TABLE 1.
Baseline characteristics of the PREMIER participants (n = 810)
| Characteristic | |
| Age (y) | 50.0 ± 8.91 |
| Female (%) | 61.7 |
| Race (%) | |
| African American | 34.4 |
| Non-Hispanic white | 64.2 |
| All others | 1.4 |
| Education, college degree or above (%) | 57.2 |
| Household income >$45,000/y (%) | 70.0 |
| Marital status, married (%) | 65.2 |
| Current smoking (%) | 4.8 |
| Fitness (heart rate/min) | 130.5 ± 14.5 |
| Physical activity (kcal · kg−1 · d−1) | 33.7 ± 2.9 |
| Body weight (kg) | 95.2 ± 18.8 |
| BMI (kg/m2) | 33.1 ± 5.8 |
| BMI classification (%) | |
| Normal weight, BMI < 25 kg/m2 | 5.4 |
| Obese, BMI ≥ 30 kg/m2 | 65.2 |
Mean ± SD (all such values).
Beverage consumption and changes in body weight during follow-up
The mean (±SD) body weight was 95.2 ± 1.8 kg at baseline, 91.2 ± 18.9 kg at 6 mo, and 91.7 ± 19.7 kg at 18 mo. Across all groups, the mean (±SD) weight loss was 3.5 ± 5.2 kg at 6 mo and 3.0 ± 6.1 kg at 18 mo.
The consumption of beverages at baseline and at 6 and 18 mo is shown in Table 2. The mean liquid calorie intake at baseline was 355.6 kcal/d, or 19.0% of the total caloric intake. At baseline, SSBs were the leading source of liquid calories (131.1 kcal/d, 37% of liquid calories), followed by 100% juice (60.5 kcal/d), alcoholic beverages (52.4 kcal/d), CTS (46.5 kcal/d), milk (42.5 kcal/d), CT (16.2 kcal/d), and diet drinks (6.4 kcal/d). There was a decrease in liquid calorie intake during follow-up.
TABLE 2.
Mean beverage consumption at baseline, 6 mo, and 18 mo by PREMIER participants1
| Time |
||||
| Beverage intake | Baseline | 6 mo | 18 mo | P for trend2 |
| Liquid calories | ||||
| Absolute amount (kcal/d) | 355.6 ± 236.8 | 307.9 ± 244.63 | 293.9 ± 210.32 | <0.001 |
| Total energy intake (%) | 19.0 ± 11.5 | 18.6 ± 14.3 | 17.3 ± 11.22 | 0.002 |
| Individual beverage type (mL/d) | ||||
| SSBs | 310.5 ± 354.8 | 140.0 ± 298.73 | 227.7 ± 301.63 | <0.001 |
| Diet drinks | 331.2 ± 414.0 | 278.0 ± 366.73 | 381.5 ± 440.63 | 0.003 |
| Milk | 94.6 ± 183.3 | 150.8 ± 283.93 | 100.5 ± 177.4 | 0.43 |
| 100% Juice | 139.0 ± 201.1 | 183.3 ± 307.53 | 133.1 ± 176.4 | 0.58 |
| CTS | 183.3 ± 301.6 | 165.6 ± 356.03 | 140.0 ± 266.13 | <0.001 |
| CT | 162.6 ± 289.8 | 174.5 ± 103.5 | 121.2 ± 194.13 | <0.001 |
| Alcoholic beverages | 100.5 ± 248.4 | 97.6 ± 221.8 | 91.7 ± 218.8 | 0.31 |
Values are means ± SDs. SSBs, sugar-sweetened beverages; CTS, coffee and tea with sugar; CT, coffee and tea without sugar.
Test for time trend was performed by using the generalized estimating equation model with beverage consumption regressed on time.
Significantly different from baseline, P ≤ 0.05 (paired t test).
At baseline, the most-consumed beverages by volume were diet drinks (331.2 mL/d), followed by SSBs (310.5 mL/d), CTS (183.3 mL/d), CT (162.6 mL/d), 100% juice (139.0 mL/d), alcoholic beverages (100.5 mL/d), and milk (94.6 mL/d). Significant changes in beverage consumption were observed at 6 and 18 mo, and the changes varied by beverage type and time. At 6 mo, the consumption of SSBs, diet drinks, and CTS decreased significantly; of juice and milk increased; and of CT and alcoholic beverages did not change. From baseline to 18 mo, the consumption of SSBs, CTS, and CT decreased; of diet drinks increased; and of milk, juice, and alcoholic beverages did not change. We also performed a test of trend for each beverage category across the 3 time points. Overall, consumption of SSBs, CTS, and CT decreased with time, whereas the consumption of diet drinks increased.
Association between beverage consumption and weight loss
The longitudinal associations between changes in body weight and in intakes of liquid calories, solid calories, and individual beverages are shown in Table 3. We also examined these associations in cross-sectional analyses and found them similar to those in the longitudinal analyses (data not shown).
TABLE 3.
Longitudinal associations between changes from baseline (Δ) in beverage consumptions and in weight at 6 and 18 mo1
| ΔBody weight (kg/unit exposure) |
||||||
| 6 mo |
18 mo |
|||||
| Exposure | βL | 95% CI | P | βL | 95% CI | P |
| Model 12 | ||||||
| ΔLiquid calories (100 kcal/d) | 0.25 | 0.11, 0.39 | <0.001 | 0.24 | 0.06, 0.41 | 0.008 |
| ΔSolid calories (100 kcal/d) | 0.06 | 0.002, 0.14 | 0.04 | 0.09 | 0.005, 0.16 | 0.003 |
| Model 23 | ||||||
| ΔPercentage of liquid calories in total calories (%) | 0.04 | 0.01, 0.06 | 0.005 | 0.02 | −0.01, 0.06 | 0.2 |
| Model 34 | ||||||
| Beverage category (1 serving/d)5 | ||||||
| ΔSSBs | 0.49 | 0.11, 0.82 | 0.006 | 0.65 | 0.22, 1.09 | 0.003 |
| ΔDiet drinks | −0.27 | −0.60, 0.05 | 0.11 | −0.38 | −0.22, 0.01 | 0.06 |
| ΔMilk | 0.16 | −0.27, 0.60 | 0.48 | 0.11 | −0.76, 1.03 | 0.79 |
| ΔJuice | −0.05 | −0.44, 0.27 | 0.71 | 0.005 | −0.65, 0.65 | 0.99 |
| ΔCTS | −0.16 | −0.49, 0.22 | 0.42 | −0.11 | −0.54, 0.38 | 0.73 |
| ΔCT | 0.22 | −0.12, 0.65 | 0.25 | 0.33 | −0.93, 0.33 | 0.31 |
| ΔAlcoholic beverages | −0.38 | −0.82, 0.05 | 0.10 | −0.49 | −1.03, 0.08 | 0.93 |
βL, regression coefficient; SSBs, sugar-sweetened beverages; CTS, coffee and tea with sugar; CT, coffee and tea without sugar.
Changes in liquid and solid calories were simultaneously included in the model, adjusted for baseline sex, race, age, income, education, marital and employment status, BMI status, intervention group, and concurrent change in fitness and physical activity.
Liquid calorie intake was expressed as a percentage of calorie intake [(liquid calories/total calories) × 100], adjusted for baseline sex, race, age, income, education, marital and employment status, BMI status, intervention group, and concurrent change in fitness and physical activity.
Changes in all beverages were simultaneously included in the model, adjusted for baseline sex, race, age, income, education, marital and employment status, BMI status, intervention group, concurrent change in fitness, physical activity, and total calorie intake.
One serving = 12 fl oz, or 355 mL.
Change in consumption of liquid and solid calories and change in body weight
When both liquid and solid calories were included in the analysis (model 1), changes in these variables were significantly and positively associated with weight change. A reduction of 100 kcal/d in liquid calorie intake was associated with 0.3 kg of weight loss (95% CI: 0.1, 0.4; P < 0.001) at 6 mo and of 0.2 kg (95% CI: 0.06, 0.4; P = 0.008) at 18 mo. A reduction in solid calorie intake by 100 kcal/d was associated with a 0.06-kg weight loss (95% CI: 0.002, 0.14; P = 0.04) at 6 mo and of 0.09 kg (95% CI: 0.005, 0.16; P = 0.003) at 18 mo. A reduction in liquid calorie intake had a stronger effect on weight loss than did a reduction in solid calorie intake, but the difference was statistically significant only at 6 mo (P value for the test of βliquid − βsolid > 0 was 0.006 at 6 mo and 0.09 at 18 mo). This finding was also supported by the results from model 2 (Table 3). A reduction in the percentage of liquid calories from total calories by 1% was associated with a weight loss of 0.04 kg (95% CI: 0.01, 0.06; P = 0.005) at 6 mo and of 0.02 kg (95% CI: −0.01, 0.06; P = 0.2) at 18 mo. We further conducted a stratified analyses based on participants' race (white or black), sex (male or female), baseline BMI (<30 or ≥30), or age group (<50 or ≥50 y). The results are shown in Table 4. Liquid calories apparently had a stronger effect on weight loss in blacks than in whites; however, there was no evidence to suggest that the difference was statistically significant (P for interaction = 0.6 at 6 mo and 0.8 at 18 mo).
TABLE 4.
Longitudinal associations between changes from baseline (Δ) in beverage consumption (exposure) and in body weight (exposure) by race, sex, baseline BMI status, and age group among participants in the PREMIER study1
| ΔBody weight (kg/unit exposure) |
||||||||
| Race2 |
Sex3 |
Baseline BMI status4 |
Age5 |
|||||
| Exposure | White | Black | Men | Women | <30 kg/m2 | ≥30 kg/m2 | <50 y | ≥50 y |
| ΔLiquid calorie intake (100 kcal/d) | ||||||||
| 6 mo | 0.216 | 0.376 | 0.226 | 0.306 | 0.246 | 0.266 | 0.226 | 0.246 |
| 18 mo | 0.19 | 0.536 | 0.22 | 0.296 | 0.19 | 0.296 | 0.286 | 0.356 |
| ΔSolid calorie intake (100 kcal/d) | ||||||||
| 6 mo | 0.07 | 0.05 | 0.05 | 0.056 | 0.04 | 0.06 | 0.04 | 0.02 |
| 18 mo | 0.116 | 0.05 | 0.05 | 0.126 | 0.07 | 0.08 | 0.05 | 0.08 |
| ΔSSBs (servings/d)7 | ||||||||
| 6 mo | 0.386 | 0.596 | 0.27 | 0.706 | 0.22 | 0.596 | 0.486 | 0.24 |
| 18 mo | 0.816 | 0.54 | 0.38 | 1.086 | 0.43 | 1.086 | 0.60 | 0.726 |
SSBs, sugar-sweetened beverages. A likelihood ratio test was used to test for interactions.
Test for interaction between race and liquid calories was not significant (P = 0.6 at 6 mo and 0.2 at 18 mo).
Test for interaction between sex and SSB intake was not significant (P = 0.2 at 6 mo and 0.2 at 18 mo).
Test for interaction between BMI and SSB intake was not significant (P = 0.08 at 6 mo and 0.06 at 18 mo).
Test for interaction between age and SSB intake was not significant (P = 0.3 at 6 mo and 0.9 at 18 mo).
P < 0.05.
Changes in liquid and solid calories were simultaneously included in the model, adjusted for baseline sex, race, age, income, education, marital and employment status, BMI status, intervention group, and change in fitness and physical activity. Change in all beverages were simultaneously included in the model, adjusting for baseline sex, race, age, income, education, marital and employment status, BMI status, intervention group, and change in fitness, physical activity and total calorie intake. One serving = 12 fl oz, or 355 mL.
Consumption of individual beverages and change in body weight
In another model (model 3), in which the exposures were individual beverages, only the change in consumption of SSBs was significantly associated with weight change at both 6 and 18 mo. A reduction in SSBs by 1 serving/d (355 mL, or12 fl oz) was associated with a weight loss of 0.5 kg (95% CI: 0.1, 0.8; P = 0.006) at 6 mo and of 0.7 kg (95% CI: 0.2, 1.1; P = 0.003) at 18 mo. Changes in the consumption of diet drinks and alcoholic beverages were inversely associated with weight loss, both at 6 and 18 mo, but were not statistically significant. None of the other beverage types was significantly associated with weight change at follow-up (Table 3). In the stratified analyses, the positive association between SSB consumption and weight loss was also consistent across each strata. No test for interaction was statistically significant (Table 4).
Change in body weight and change in consumption of liquid calories and SSBs
We examined dose-response patterns for body weight and changes in consumption of liquid calories and SSBs by dividing participants into tertiles based on their 6- or 18-mo change in consumption of liquid calories or SSBs (persons in the first tertile had the greatest reduction). We calculated the model-adjusted mean change and 95% CIs in body weight for participants in each tertile.
Liquid calories
At both 6 and 18 mo, participants in the first tertile had a greater mean weight loss (6-mo change: 0.8 kg, P = 0.006; 18-mo change: 1.5 kg; P < 0.001) than did those in the third tertile (Figure 1). A significant dose-response trend between change in body weight and change in liquid calorie intake was observed for both the 6-mo change (P = 0.01) and the 18-mo change (P < 0.001).
FIGURE 1.
Model-adjusted mean weight change and 95% CIs (6 mo − baseline) by tertile of 6-mo liquid calorie intake change and 18-mo weight change (18 mo – baseline) by tertile of 18-mo liquid calorie intake change. At 6 mo, the median change in liquid calorie intake was −271 kcal/d in the first tertile, −47 kcal/d in the second tertile, and 169 kcal/d in the third tertile. At 18 mo, the corresponding change in liquid calorie intake in each tertile was −267, −48, and 138 kcal/d, respectively. Models were adjusted for baseline age, sex, race, education, income, BMI status, intervention groups, concurrent change in fitness, physical activity, and solid calorie intake (test for trend was conducted by Wilcoxon's rank-sum test).
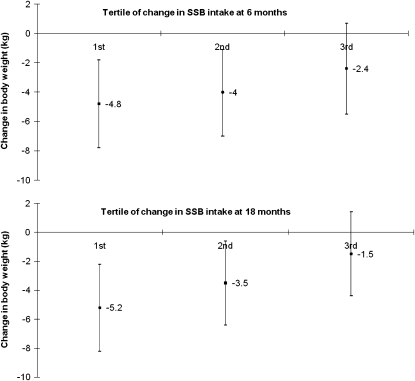
SSBs
At both 6 and 18 mo, participants in the first tertile had a greater mean weight loss than did those in the second (6-mo change: 0.7 kg; P = 0.006; 18-mo change: 1.6 kg; P < 0.001) and third (6-mo change: 2.4 kg; P < 0.001; 18-mo change: 3.6 kg; P < 0.001) tertiles (Figure 2). A significant dose-response trend between change in body weight and change in SSB intake was observed at both 6 mo (P < 0.001) and 18 mo (P < 0.001).
FIGURE 2.
Model-adjusted mean 6-mo weight change and 95% Cls (6 mo – baseline) by tertile of 6-mo sugar-sweetened beverage (SSB) intake change and 18-mo weight change (18 mo – baseline) by tertile of 18-mo SSB intake change. At 6 mo, the median change in SSB intake was −479.0 mL/d in the first tertile, 0 mL/d in the second tertile, and 260.2 mL/d in the third tertile. At 18 mo, the median change in SSB intake in each tertile was −366.7, 0, and 248.3 mL/d, respectively. Models were adjusted for baseline age, sex, race, education, income, BMI status, intervention group, current change in physical activity, fitness, other beverages intake, and total calorie intake (test for trend was conducted by Wilcoxon's rank-sum test).
Sensitivity analysis
During the follow-up, 1 participant began antihypertensive drug treatment between 3 and 6 mo, 4 participants began antihypertensive drug treatment between 12 and 18 mo, and 6 and 9 participants began insulin/hypoglycemic drug treatment by the 6 and 18 mo visits, respectively. Exclusion of these individuals from our analyses did not change the results. We also applied the baseline observation carried forward method to check the potential influence of missing values. The differences between estimates with and without imputation were very small. For example, the β regression coefficient for change in one serving of SSB consumption at 6 mo was 0.489 (kg/d) without imputation and 0.485 (kg/d) with imputation.
DISCUSSION
Four principal findings emerged from our study. First, a reduction in liquid calorie intake was significantly associated with weight loss at both 6 and 18 mo. Second, the weight-loss effect of a reduction in liquid calorie intake was stronger than that of a reduction in solid calorie intake. Third, a reduction in SSB intake was significantly associated with weight loss at both 6 and 18 mo. Fourth, no other beverage type was associated with weight change. On average, a reduction in liquid calorie intake of 100 kcal/d was associated with a 0.3-kg weight loss at 6 mo and a 0.2-kg weight loss at 18 mo. A reduction in SSB intake of 1 serving/d was associated with a 0.5-kg weight loss at 6 mo and a 0.7-kg weight loss at 18 mo.
To our knowledge, our study was the first to document the relative effects of calories from liquids compared with those of calories from solid food on weight loss in free-living adults over an extended period, 18 mo. Previously, evidence on this topic came primarily from animal studies (35–37). The only trial in humans was a 4-wk crossover study of 15 individuals, in which weight gain occurred during the liquid load period, but not during the solid load period (38).
Our study was also one of the few prospective studies to evaluate the effects of a reduction in SSB consumption on weight loss. Two trials investigated the effects of a reduction in SSB intake on weight change in children. Neither reported significant results, but methodologic issues, including inadequate power, may hinder their interpretation.
One explanation for the different satiating effects of beverages and solid foods is the absence of mastication when beverages are consumed (39). The absence of chewing and swallowing when ingesting beverages might result in decreased pancreatic exocrine and endocrine responses compared with the ingestion of solid foods. Second, beverages are also emptied from the stomach at a higher rate than are solids and may induce weaker signals in the gastrointestinal tract that would lead to inhibition of further food intake (40).
Another proposed link between SSB consumption and body weight is related to the high fructose content of SSBs. Long-term consumption of a large amount of fructose can promote fat storage and excessive food intake through an increase in de novo lipogenesis (41) and changes in postprandial hormonal patterns (42).
There are several possible explanations for why the consumption of other caloric beverages was not associated with body weight. First, beverages can differ in their effects on satiety and energy intake (43). It has been proposed that the addition of protein, fat, or fiber to a beverage enhances satiety, perhaps by slowing stomach emptying. Milk, for example, might be expected to have more satiating effects than soft drinks because it contains protein and fat in addition to carbohydrate (44). Second, the effect of individual beverages on weight may also be mediated by their nutrient composition. For example, studies have suggested that calcium from milk can favor weight loss by increasing lipolysis and thermogenesis and by decreasing fatty acid absorption (45). Third, energy from alcohol can be preferentially oxidized and contribute less to storage energy (46). Last, it is possible that certain behaviors and/or lifestyle factors associated with milk, juice, tea, coffee, or alcohol consumptions play a role in mediating their effects on body weight.
One potential limitation of our study was the focus on individuals with either prehypertension or stage I hypertension; however, together, these segments of the population account for approximately two-thirds of US adults. Second, the study population included few Hispanics and Asians. Strengths of our study included its longitudinal design, its sample size, its duration, the availability of six 24-h diet recalls (one from a weekday and one from a weekend day at each of the 3 time points over 18 mo) to measure dietary intake, the high rates of retention, and our ability to evaluate a variety of beverages.
In conclusion, our study supports policy recommendations and public health efforts to reduce intakes of liquid calories, particularly from SSBs, in the general population.
Supplementary Material
Acknowledgments
We thank the PREMIER participants and staff for their contributions to the study.
The authors' responsibilities were as follows—LC: conducted the analyses and the first draft of the manuscript. All authors: conceived of and designed the study, interpreted the analyses, and revised the manuscript. None of the authors reported any personal or financial conflict of interests.
REFERENCES
- 1.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6–28 [DOI] [PubMed] [Google Scholar]
- 2.Briefel RR, Johnson CL. Secular trends in dietary intake in the United States. Annu Rev Nutr 2004;24:401–31 [DOI] [PubMed] [Google Scholar]
- 3.Nielsen SJ, Siega-Riz AM, Popkin BM. Trends in energy intake in U.S. between 1977 and 1996: similar shifts seen across age groups. Obes Res 2002;10:370–8 [DOI] [PubMed] [Google Scholar]
- 4.Nielsen SJ, Popkin BM. Changes in beverage intake between 1977 and 2001. Am J Prev Med 2004;27:205–10 [DOI] [PubMed] [Google Scholar]
- 5.De Castro JM. The effects of the spontaneous ingestion of particular foods or beverages on the meal pattern and overall nutrient intake of humans. Physiol Behav 1993;53:1133–44 [DOI] [PubMed] [Google Scholar]
- 6.Mattes RD. Dietary compensation by humans for supplemental energy provided as ethanol or carbohydrate in fluids. Physiol Behav 1996;59:179–87 [DOI] [PubMed] [Google Scholar]
- 7.Tournier A, Louis-Sylvestre J. Effect of the physical state of a food on subsequent intake in human subjects. Appetite 1991;16:17–24 [DOI] [PubMed] [Google Scholar]
- 8.Mourao DM, Bressan J, Campbell WW, Mattes RD. Effects of food form on appetite and energy intake in lean and obese young adults. Int J Obes (Lond) 2007;31:1688–95 [DOI] [PubMed] [Google Scholar]
- 9.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet 2001;357:505–8 [DOI] [PubMed] [Google Scholar]
- 10.Berkey CS, Rockett HR, Field AE, Gillman MW, Colditz GA. Sugar-added beverages and adolescent weight change. Obes Res 2004;12:778–88 [DOI] [PubMed] [Google Scholar]
- 11.Phillips SM, Bandini LG, Naumova EN, et al. Energy-dense snack food intake in adolescence: longitudinal relationship to weight and fatness. Obes Res 2004;12:461–72 [DOI] [PubMed] [Google Scholar]
- 12.Bes-Rastrollo M, Sanchez-Villegas A, Gomez-Gracia E, Martinez JA, Pajares RM, Martinez-Gonzalez MA. Predictors of weight gain in a Mediterranean cohort: the Seguimiento Universidad de Navarra Study 1. Am J Clin Nutr 2006;83:362–70 [DOI] [PubMed] [Google Scholar]
- 13.Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 2004;292:927–34 [DOI] [PubMed] [Google Scholar]
- 14.Striegel-Moore RH, Thompson D, Affenito SG, et al. Correlates of beverage intake in adolescent girls: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr 2006;148:183–7 [DOI] [PubMed] [Google Scholar]
- 15.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 2006;84:274–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health 2007;97:667–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bachman CM, Baranowski T, Nicklas TA. Is there an association between sweetened beverages and adiposity? Nutr Rev 2006;64:153–74 [DOI] [PubMed] [Google Scholar]
- 18.Drewnowski A, Bellisle F. Liquid calories, sugar, and body weight. Am J Clin Nutr 2007;85:651–61 [DOI] [PubMed] [Google Scholar]
- 19.Forshee RA, Anderson PA, Storey ML. Sugar-sweetened beverages and body mass index in children and adolescents: a meta-analysis. Am J Clin Nutr 2008;87:1662–71 [DOI] [PubMed] [Google Scholar]
- 20.Pereira MA, Jacobs DR., Jr Sugar-sweetened beverages, weight gain and nutritional epidemiological study design. Br J Nutr 2008;99:1169–70 [DOI] [PubMed] [Google Scholar]
- 21.Summerbell CD, Watts C, Higgins JP, Garrow JS. Randomised controlled trial of novel, simple, and well supervised weight reducing diets in outpatients. BMJ 1998;317:1487–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pereira MA, Jacobs DR, Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA 2002;287:2081–9 [DOI] [PubMed] [Google Scholar]
- 23.Zemel MB, Thompson W, Milstead A, Morris K, Campbell P. Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes Res 2004;12:582–90 [DOI] [PubMed] [Google Scholar]
- 24.Zemel MB, Richards J, Milstead A, Campbell P. Effects of calcium and dairy on body composition and weight loss in African-American adults. Obes Res 2005;13:1218–25 [DOI] [PubMed] [Google Scholar]
- 25.Barr SI, McCarron DA, Heaney RP, et al. Effects of increased consumption of fluid milk on energy and nutrient intake, body weight, and cardiovascular risk factors in healthy older adults. J Am Diet Assoc 2000;100:810–7 [DOI] [PubMed] [Google Scholar]
- 26.Berkey CS, Rockett HR, Willett WC, Colditz GA. Milk, dairy fat, dietary calcium, and weight gain: a longitudinal study of adolescents. Arch Pediatr Adolesc Med 2005;159:543–50 [DOI] [PubMed] [Google Scholar]
- 27.Gunther CW, Legowski PA, Lyle RM, et al. Dairy products do not lead to alterations in body weight or fat mass in young women in a 1-y intervention. Am J Clin Nutr 2005;81:751–6 [DOI] [PubMed] [Google Scholar]
- 28.Liebman M, Pelican S, Moore SA, et al. Dietary intake, eating behavior, and physical activity-related determinants of high body mass index in rural communities in Wyoming, Montana, and Idaho. Int J Obes Relat Metab Disord 2003;27:684–92 [DOI] [PubMed] [Google Scholar]
- 29.Phillips SM, Bandini LG, Cyr H, Colclough-Douglas S, Naumova E, Must A. Dairy food consumption and body weight and fatness studied longitudinally over the adolescent period. Int J Obes Relat Metab Disord 2003;27:1106–13 [DOI] [PubMed] [Google Scholar]
- 30.Thompson WG, Rostad Holdman N, Janzow DJ, Slezak JM, Morris KL, Zemel MB. Effect of energy-reduced diets high in dairy products and fiber on weight loss in obese adults. Obes Res 2005;13:1344–53 [DOI] [PubMed] [Google Scholar]
- 31.Appel LJ, Champagne CM, Harsha DW, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 2003;289:2083–93 [DOI] [PubMed] [Google Scholar]
- 32.Elmer PJ, Obarzanek E, Vollmer WM, et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med 2006;144:485–95 [DOI] [PubMed] [Google Scholar]
- 33.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997;336:1117–24 [DOI] [PubMed] [Google Scholar]
- 34.Blair SN, Haskell WL, Ho P, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol 1985;122:794–804 [DOI] [PubMed] [Google Scholar]
- 35.Archer ZA, Corneloup J, Rayner DV, Barrett P, Moar KM, Mercer JG. Solid and liquid obesogenic diets induce obesity and counter-regulatory changes in hypothalamic gene expression in juvenile Sprague-Dawley rats. J Nutr 2007;137:1483–90 [DOI] [PubMed] [Google Scholar]
- 36.Sclafani A, Xenakis S. Influence of diet form on the hyperphagia-promoting effect of polysaccharide in rats. Life Sci 1984;34:1253–9 [DOI] [PubMed] [Google Scholar]
- 37.Ramirez I. Feeding a liquid diet increases energy intake, weight gain and body fat in rats. J Nutr 1987;117:2127–34 [DOI] [PubMed] [Google Scholar]
- 38.DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord 2000;24:794–800 [DOI] [PubMed] [Google Scholar]
- 39.Almiron-Roig E, Chen Y, Drewnowski A. Liquid calories and the failure of satiety: how good is the evidence? Obes Rev 2003;4:201–12 [DOI] [PubMed] [Google Scholar]
- 40.Spiegel TA, Kaplan JM, Alavi A, Kim PS, Tse KK. Effects of soup preloads on gastric emptying and fullness ratings following an egg sandwich meal. Physiol Behav 1994;56:571–5 [DOI] [PubMed] [Google Scholar]
- 41.Elliott SS, Keim NL, Stern JS, Teff K, Havel PJ. Fructose, weight gain, and the insulin resistance syndrome. Am J Clin Nutr 2002;76:911–22 [DOI] [PubMed] [Google Scholar]
- 42.Teff KL, Elliott SS, Tschop M, et al. Dietary fructose reduces circulating insulin and leptin, attenuates postprandial suppression of ghrelin, and increases triglycerides in women. J Clin Endocrinol Metab 2004;89:2963–72 [DOI] [PubMed] [Google Scholar]
- 43.St-Onge MP, Rubiano F, DeNino WF, et al. Added thermogenic and satiety effects of a mixed nutrient vs a sugar-only beverage. Int J Obes Relat Metab Disord 2004;28:248–53 [DOI] [PubMed] [Google Scholar]
- 44.Rolls BJ, Castellanos VH, Halford JC, et al. Volume of food consumed affects satiety in men. Am J Clin Nutr 1998;67:1170–7 [DOI] [PubMed] [Google Scholar]
- 45.Zemel MB. Calcium and dairy modulation of obesity risk. Obes Res 2005;13:192–3 [DOI] [PubMed] [Google Scholar]
- 46.Jequier E. Alcohol intake and body weight: a paradox. Am J Clin Nutr 1999;69:173–4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.