Abstract
With the recent advances in imaging techniques, increased numbers of hepatic lesions are found today, and surgeons are asked frequently for the best course of management. Benign hepatic tumors sometimes cause life-threatening complications and more often trigger disabling or annoying symptoms in otherwise healthy individuals. Although various imaging techniques are quite accurate in identifying cysts and hemangiomas, other benign hepatic lesions, such as adenomas, focal nodular hyperplasia and other benign solid tumors, cannot be differentiated from malignant lesions with a high degree of confidence.
Until ten to 15 years ago, the operative mortality and morbidity rates with extensive hepatic resections were too great to justify their use if a less dangerous, even though unsatisfactory, alternative was available. This is, however, no longer a supportable point of view in the 1980s. Our experience with hepatic resections performed upon 219 patients with benign hepatic lesions is summarized herein with emphasis on the safety and effectiveness of excisional therapy for benign hepatic lesions. The results of parts of our experience have been published elsewhere (1–10).
METHODS
From October 1964 to June 1989, 547 consecutive patients underwent hepatic resection at the University of Colorado Health Sciences Center (1964 to 1980) and the University Health Center of Pittsburgh (1981 to 1989). The number of hepatic resections has increased sharply through the years, and more than 100 hepatic resections will be carried out this year.
The patients ranged in age from 11 months to 81 years. Thirty of the 547 patients were younger than 18 years of age, and 26 of these 30 were younger than 12 years.
Of those 547 patients, 219 had benign hepatic lesions that were exised for therapeutic reasons or because malignant growths could not be ruled out preoperatively. The remaining 328 patients had hepatic resection for malignant disease, of which 143 tumors were primary to the liver and 185 were metastases to the liver from various origins.
The diagnoses of 219 benign hepatic lesions are listed in Table I. Cavernous hemangioma was, by far, the most common, followed by liver cell adenoma, focal nodular hyperplasia and congenital hepatic cyst.
TABLE I.
BENIGN HEPATIC LESIONS
| No. | |
|---|---|
| Cavernous hemangioma | 114 |
| Liver cell adenoma | 25 |
| Focal nodular hyperplasia | 23 |
| Congenital cyst | 23 |
| Polycystic disease, 6 | |
| Nonpolycystic disease, 14 | |
| Cystic adenoma, 3 | |
| Trauma | 13 |
| Abscess | 5 |
| Hydatid cyst | 5 |
| Caroli’s disease | 5 |
| Fibroma | 1 |
| Leiomyoma | 1 |
| Mesenchymal hamartoma | 1 |
| Mesenchymoma | 1 |
| Regenerative nodule | 1 |
| Organized hematoma | 1 |
| Total | 219 |
KINDS OF HEPATIC RESECTIONS
There were six categories of hepatic resections: right and left trisegmentectomy, right and left lobectomy, left lateral segmentectomy and non-anatomic local resection. “Extended” right and left lobectomy, which removed only a portion of the medial segment or anterior segment, respectively, were considered as right or left lobectomy in this study. Our operative techniques have been reported in detail elsewhere (1–3). Some of the nonanatomic local excisions were those of huge benign hepatic lesions and were often more difficult than anatomic resections. The types of hepatic resection used for various benign hepatic lesions are summarized in Table II.
TABLE II.
DIAGNOSIS, EXTENT OF RESECTION AND OPERATIVE MORTALITY IN 219 PATIENTS WITH BENIGN HEPATIC LESION
| Right trisegmentectomy, No. of pts. | Left trisegmentectomy, No, of pts. | Right lobectomy, No. of pts. | Left lobectomy, No. of pts. | Left lateral segmentectomy, No. of pts. | Local excision, No. of pts. | Total, No. of pts. | |
|---|---|---|---|---|---|---|---|
| Hemangioma | 14 (0) | 1 (0) | 32 (0) | 6 (0) | 7 (0) | 54 (0) | 114 (0) |
| Adenoma | 8 (0) | 1 (0) | 9 (0) | 4 (0) | 0 (0) | 2 (0) | 25 (0) |
| Focal nodular hyperplasia | 4 (0) | 0 (0) | 3 (0) | 3 (0) | 1 (0) | 12 (0) | 23 (0) |
| Congenital cyst | 4 (0) | 0 (0) | 8 (0) | 2 (0) | 2 (0) | 7 (0) | 23 (0) |
| Trauma | 4 (2) | 0 (0) | 6 (0) | 1 (0) | 1 (0) | 1 (0) | 13 (2) |
| Hydatid cyst | 1 (0) | 0 (0) | 1 (0) | 1 (0) | 1 (0) | 1 (0) | 5 (0) |
| Abscess | 1 (1) | 0 (0) | 3 (1) | 0 (0) | 0 (0) | 1 (0) | 5 (2) |
| Caroli’s disease | 0 (0) | 0 (0) | 0 (0) | 1 (0) | 2 (0) | 1 (0) | 5 (0) |
| Others | 2 (0) | 0 (0) | 1 (1) | 1 (0) | 0 (0) | 2 (0) | 6 (1) |
| Total | 38 (3) | 2 (0) | 64 (2) | 20 (0) | 14 (0) | 81 (0) | 219 (5) |
Numbers in parentheses are operative mortalities.
FOLLOW-UP STUDY
The follow-up period ranged from three months to 19 years with a median of 4.5 years. As of September 1989, only 25 patients have been lost to follow-up study one to 11 years after hepatic resection.
RESULTS
Cavernous hemangioma
There were 114 patients with cavernous hemangiomas that were surgically excised (Table II). Twenty-seven were men and 87 were women. The ages of the patients ranged from 21 to 77 years, with a mean age of 46 years. Twenty-five of the 114 patients had multiple hemangiomas. The size of hemangiomas ranged from 4 to 41 centimeters in its largest diameter with a mean of 12 centimeters. Focal nodular hyperplasia coexisted in four women and hamartoma in two men.
Indications for surgical excision (Table III)
TABLE III.
REASONS FOR EXCISION OF CAVERNOUS HEMANGIOMAS AND OUTCOME
| Reason, symptom | No. of pts. | Complete relief* |
|---|---|---|
| Severe pain with rupture | 10 | 100 |
| Severe pain with internal hemorrhage | 22 | 100 |
| Moderate to severe pain | 51 | 96 |
| With necrotic center | 17 | 100 |
| Vague but annoying symptoms | 17 | 79 |
| Diagnosis uncertain | 14 | – |
| History of cancer | 11 | – |
Percentage of patients who had complete symptomatic relief after excision.
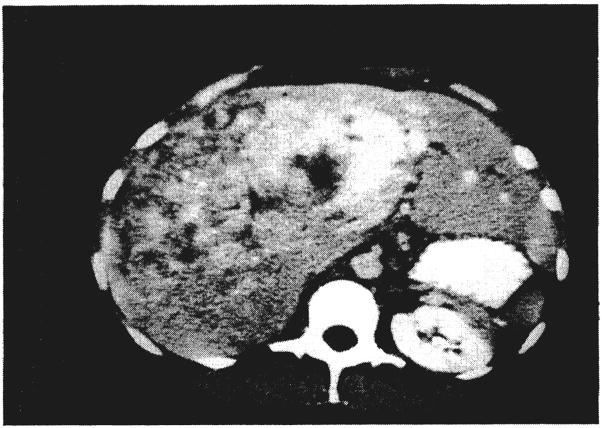
The surgical removal of the hemangioma was carried out in 32 patients because of severe pain associated with rupture or hemorrhage into the necrotic center of the tumor (group 1). Spontaneous rupture of the hemangioma was experienced in two patients, resulting in hemoperitoneum or hemobilia. In eight patients, hemorrhage occurred after unwise percutaneous needle biopsy or open biopsy were performed. In the remaining 22 patients hemorrhage occurred spontaneously into the necrotic center of the giant hemangioma and, in these patients, preoperative dynamic computed tomographic (CT) scan predicted the pathologic findings accurately (Fig. 1). The patients with this complication experienced attacks of severe abdominal pain, accompanied by enlarging abdominal mass or hepatomegaly.
Fig. 1.
A large cavernous hemangioma with central necrosis and hemorrhage is shown.
The indication for excision was moderate to severe pain in 51 patients (group 2). The pain was often colicky in nature, almost always located in the right upper quadrant or the epigastrium and frequently radiated to the back and the shoulder. The diagnostic work-up study of gallbladder disease or peptic ulcer disease often led to the discovery of hepatic lesions. In 17 of the 51 patients, the CT scan demonstrated a necrotic center of the hemangioma.
The main indication for surgical treatment in 17 patients was vague but annoying symptoms of long duration, caused by a large abdominal mass (group 3). These symptoms consisted of all or any combinations of shortness of breath, abdominal fullness, pressure and dull ache, early satiety, nausea, vomiting, fatigue, night sweats, fever and weight loss.
In 14 patients, the hemangiomas were relatively or completely asymptomatic (group 4). Eleven of these 14 patients had a history of malignant lesions and the specific diagnosis could not be made with certainty in spite of an extensive work-up evaluation. In the remaining three patients, the CT scan revealed a large central necrosis in the relatively asymptomatic giant cavernous hemangioma.
Hematologic abnormalities were noted in 15 patients; 11 patients had chronic anemia with a hemoglobin value of less than 10 grams per deciliter, three had a platelet count of less than 100,000 per cubic millimeter and one patient had been diagnosed as having primary fibrinolysis for several years. These findings were not main indications for excisional therapy, but they were corrected after the removal of hemangioma in all but one patient with leukopenia and thrombocytopenia.
Operative mortality and morbidity rates
There was no operative death (death within a month) after 15 trisegmentectomies, 38 lobectomies, seven left lateral segmentectomies and 54 nonanatomic resections (Table II). There were, however, a total of 14 significant complications that occurred after hepatic resection for hemangioma. Three patients had postoperative bleeding develop that required re-exploration (one after right trisegmentectomy, one after right lobectomy and one after local excision), four patients had prolonged (one to two months) bile leak (one after right trisegmentectomy, one after left trisegmentectomy, one after right lobectomy and one after local excision), five patients had subphrenic abscess (one after right trisegmentectomy, three after right lobectomy and one after local excision) and two patients had acute viral hepatitis with recovery long after operation (Table IV). All of the complications were resolved after treatment.
TABLE IV.
OPERATIVE MORBIDITY AFTER EXCISION OF BENIGN HEPATIC LESION
| Hemangioma | Adenoma | FNH | Cyst* | Others | |
|---|---|---|---|---|---|
| Postoperative bleeding | 3 | 2 | 1 | – | 1 |
| Abscess | 5 | 3 | – | 1 | 2 |
| Bile leak | 4 | 1 | 1 | 1 | – |
| Viral hepatitis | 2 | – | – | – | – |
| Bile duct stricture | – | – | 1 | – | – |
| CVA | – | – | – | 1 | – |
Congenital hepatic cyst or cysts.
CVA, Cerebrovascular accident, and FNH, focal nodular hyperplasia.
Late deaths
Six deaths were confirmed as of September 1989. Four patients died of malignant lesions that had been diagnosed before hepatic resection: one each of chronic lymphocytic leukemia, carcinoma of the testis, carcinoma of the lung and hypernephroma. A fifth patient died of carcinoma of the lung and a sixth patient died of carcinoma of the colon that was diagnosed four and six years, respectively, after hepatic resection.
Symptomatic relief
Ninety-four of the 114 patients who had hepatic resection for cavernous hemangioma were contacted in September 1989, three months to 15 years after the operation (median of 4.5 years). Six of the 114 patients died and 14 patients were lost to follow-up study. Twenty-eight of the 94 patients had had rupture or hemorrhage into the necrotic center of the hemangioma with severe symptoms (group 1), 45 had had moderate to severe symptoms (group 2) and 14 had had vague but annoying symptoms (group 3) and seven had vague symptoms or were completely asymptomatic (group 4).
All 28 patients in group 1 were free of previous symptoms, as were 43 of the 45 patients in group 2. Two of the 45 patients in group 2 continued to experience some of the previous symptoms with less severity than that before operation. Eleven of the 14 patients in group 3 were completely relieved from the vague but annoying symptoms, but three patients continued to experience some of the symptoms. All of the seven patients who did not have significant symptoms (group 4) thought that they were doing better than before the operation because the malignant tumor was ruled out, or stated that they were doing as well as before the operation.
Liver cell adenoma
There were 25 patients with adenomas that were surgically removed. Five were men and 20 were women. The ages ranged from 16 to 60 years, with a mean age of 31 years. Twelve of the 20 women had a history of using birth control pills or estrogen therapy. Five of the 25 patients, two men and three women, had multiple adenomas. Tumor size ranged from 5 to 27 centimeters in the greatest diameter, with a mean of 12 centimeters. One man had an adenoma of the parathyroid gland and one woman had a focal nodular hyperplasia.
Indications for surgical excision (Table V)
TABLE V.
REASONS FOR EXCISION OF LIVER CELL ADENOMAS AND OUTCOME
| Reason, symptom | No. of pts. | Complete relief* |
|---|---|---|
| Severe pain with rupture | 6 | 100† |
| Severe pain with internal hemorrhage | 4 | 100‡ |
| Moderate to severe pain | 7 | 100 |
| Vague but annoying symptoms | 5 | 80 |
| Diagnosis uncertain | 3 | – |
Percentage of patients who had complete symptomatic relief after excision.
One patient with widespread adenomas required hepatic transplantation (see text).
Two patients with widespread adenomas became symptomatic two to three years after excision (see text).
Six patients were presented to us with hemoperitoneum from spontaneous rupture of the adenoma. Four patients with spontaneous hemorrhage into the necrotic center had a sudden onset of excruciating pain. Seven patients had moderate to severe pain and five patients had vague but annoying gastrointestinal symptoms or symptoms related to a large abdominal mass similar to those of cavernous hemangioma, or both. Only three patients were relatively or completely asymptomatic, their solid tumors being found incidentally during the examination for an unrelated illness or during abdominal exploration for another lesion. These asymptomatic adenomas were excised because of their large size, or because a definitive diagnosis could not be established preoperatively.
Operative mortality and morbidity rates
There was no operative death (death within a month) after nine trisegmentectomies, 13 lobectomies, one left lateral segmentectomy and two nonanatomic local excisions (Table II). There were, however, six significant complications that occurred after hepatic resection for adenoma. Two patients had postoperative bleeding that required re-exploration (one after right trisegmentectomy and one after right lobectomy), three patients had subphrenic abscess (two after right trisegmentectomy and one after right lobectomy) and one patient had prolonged (one to two months) bile leak after left lobectomy. All of the complications were successfully treated (Table IV).
Late deaths
Two patients were dead and 23 were alive and well as of September 1989. One man with multiple adenomas died of liver failure because of multiple adenomas of the retained left lateral segment six years after right trisegmentectomy. Another woman with multiple adenomas died five years after right trisegmentectomy from cryptococcal infection, a complication of acquired immune deficiency syndrome (AIDS).
Symptomatic relief
The follow-up study was completed in all of the 25 patients with adenoma from nine months to 19 years after hepatic resection, with a median of six years. Five of the six patients with ruptured adenoma and two of the four patients with hemorrhage into the necrotic center of the adenoma were free of symptoms after hepatic resection. One of the six patients with ruptured adenoma required hepatic transplantation one year after right trisegmentectomy, because of the enlargement and new growth of multiple adenomas in the remaining left lateral segment. The symptomatic relief of this patient was accomplished for only six months. This patient is alive and well, without the recurrence of adenoma, seven and one-half years after hepatic transplantation. The other two patients, who also had multiple adenomas involving all four segments of the liver, had significant symptoms two years after right trisegmentectomy because of the enlargement and new growth of adenomas in the remaining left lateral segment. One patient died of liver failure six years later and another died with AIDS, as mentioned previously.
All seven patients who had had moderate to severe symptoms were completely relieved from the symptoms after hepatic resection. Four of the five patients who had had vague but annoying symptoms also became free of symptoms, but one patient continued to have annoying dull ache in the right upper part of the abdomen. All of the three patients without symptoms continued to do well.
Of the five patients with multiple adenomas, two had complete removal of the lesions and three had incomplete removal, leaving some lesions in the left lateral segment. The former patients continued to be free of symptoms, but the latter became symptomatic as described previously. There has been no recurrence of adenoma after complete removal of single or multiple lesions.
Focal nodular hyperplasia
Twenty-three patients had excisional therapy for focal nodular hyperplasia (FNH). All but one were women. Their ages ranged from 22 to 52 years, with a mean of 32 years. Twenty patients had used birth control pills. The size of the tumors ranged from 4 to 17 centimeters, with a mean of 8 centimeters in the greatest diameter. Five of the 23 patients had multiple lesions.
Indications of surgical excision
Symptoms were usually milder in patients with FNH than in those with cavernous hemangioma or adenomas. There was no spontaneous rupture of FNH, nor hemorrhage into the necrotic center.
Eight patients had moderate to severe pain and 11 patients had vague but annoying symptoms, as already described. Four patients were relatively or completely asymptomatic, and the lesions were discovered incidentally during the investigation of other illnesses (Table VI). One patient had had carcinoma of the ovaries and another had had a malignant histiocytoma of the skin. Percutaneous biopsies were performed on two lesions and were misdiagnosed as liver cell adenomas before operation.
TABLE VI.
REASONS FOR EXCISION OF FOCAL NODULAR HYPERPLASIA AND OUTCOME
| Reason, symptom | No. of pts. | Complete relief |
|---|---|---|
| Moderate to severe pain | 8 | 100 |
| Vague but annoying symptoms | 11 | 78 |
| Diagnosis uncertain | 4 | – |
| History of cancer | 3 | – |
Percentage of patients who had complete symptomatic relief after excision.
Operative mortality and morbidity rates
There was no operative death (death within a month) after four trisegmentectomies, six lobectomies, one left lateral segmentectomy and 12 nonanatomic local excisions (Table II). There was one episode each of postoperative bleeding, prolonged bile leak and bile duct stricture, which all developed in one patient. They were all corrected successfully (Table IV).
Symptomatic relief and long term follow-up study
Twenty patients were contacted in September 1989, and three patients were lost to follow-up study between one and three years. The follow-up periods ranged from three months to 15 years, with a median of four years. No death has been confirmed and the two patients who had had a malignant lesion were alive.
All of the eight patients with moderate to severe symptoms were relieved of the symptoms after operation. Seven of the nine patients with vague but annoying symptoms who were contacted in September 1989 were free of complaints after the operation, but two patients still complained of similar symptoms. Three of the four patients without significant symptoms remained free of complaint, and one patient was lost to follow-up study (Table VI).
Congenital hepatic cysts
Twenty-three patients with congenital cysts were treated by excisional therapy. Two patients had widespread polycystic disease and four patients had multiple cysts that were limited to the resected specimen. Fourteen patients had a single congenital cyst and three others had a single cystadenoma. Twenty patients were female and three were male. The ages ranged from two years to 76 years, with a mean of 47 years.
Indications for surgical excision
All but one of the 23 patients had significant symptoms and had had repeated aspiration of cystic fluid. This one patient had had carcinoma of the colon, and the lesion was misdiagnosed as a metastasis. Five patients had had sclerotherapy of the cystic wall (Table VII).
TABLE VII.
REASONS FOR EXCISION OF CONGENITAL HEPATIC CYST OR CYSTS AND OUTCOME
| Reason, symptom | No. of pts. | Complete relief |
|---|---|---|
| Severe pain | 2 | 100† |
| Moderate to severe pain and mass-related symptoms | 20 | 90 |
| Diagnosis uncertain | 1 | – |
| History of cancer | 1 | – |
| Fever and chills | 15 | 100 |
| Jaundice | 7 | 100 |
Percentage of patients who had complete symptomatic relief after excision.
Both patients had potycystic disease of the liver and the complete relief of symptoms lasted for only one to two years (see text).
Two patients with widespread polycystic disease had required intravenous alimentation for nutrition and the continuous administration of narcotics for severe pain. Other than pain and mass-related symptoms, 15 of the 22 patients had fever and chills, and seven of them had jaundice (Table VII).
Operative mortality and morbidity rates
There was no operative mortality (death within a month) after four trisegmentectomies, ten lobectomies, two left lateral segmentectomies and seven nonanatomic local excisions (Table II). There were, however, one instance each of prolonged bile leak, subphrenic abscess and a rupture of intracranial aneurysm. All of them were treated successfully (Table IV).
Follow-up study and symptomatic relief
Twenty-one patients were contacted in September 1989 and two patients were lost to follow-up study one to two years after operation.
The follow-up periods ranged from six months to 11 years, with a median of four years. No death has been confirmed. One patient with an asymptomatic cyst, who had had carcinoma of the colon, is alive.
The two patients with severe polycystic disease had right trisegmentectomy or right lobectomy, leaving some cysts behind. There was marked symptomatic relief for several years, eventually there was enlargement of the remaining cysts to the original size. One of these patients required orthotopic hepatic transplantation eight years after right lobectomy. In contrast with the recurrence after partial resection of widespread polycystic disease, symptomatic relief after complete resection of single or multiple cysts was permanent and complete. Only two of the 20 patients had minor complaints after surgical treatment in September 1989 (Table VII).
Other benign hepatic lesions
Thirteen patients had hepatic resection for trauma, five patients each for abscess, hydatid cyst and unilobar Caroli’s disease, and one patient each for fibroma, leiomyoma, mesenchymal hamartoma, mesenchymoma, regenerative nodule in the cirrhotic liver and organized hematoma (Table I).
Operative mortality and morbidity rates
Five of the 34 patients died within a month after hepatic resection (operative death) (Table II), two patients after hepatic resection for trauma, two of hepatic abscess and one of pseudohepatoma (a regenerative nodule in the cirrhotic liver which was misdiagnosed as a hepatoma).
There was one instance of postoperative bleeding and two of subphrenic abscess after hepatic resection. All of the patients who had these complication died within a month (operative death).
Follow-up study
One patient with hydatid cyst died of carcinoma of the pancreas one year after hepatic resection. Six patients were lost to follow-up study between one and five years after hepatic resection at which time they were all doing well. The remaining 22 patients were alive and well in September 1989.
DISCUSSION
The great majority of hepatic solid or cystic lesions do not cause any trouble, and would go undiscovered throughout life. In general, it is safe to observe an incidentally found, asymptomatic benign hepatic lesion of small to moderate size, as long as the benignity is certain and the lesions are closely observed for years. Liver cell adenoma is excluded from this general rule. A high incidence of spontaneous hemorrhage of adenomas is documented in this article (40 per cent). Moreover, the differentiation of adenoma from hepatoma is quite difficult particularly with specimens taken at small needle biopsy. Even with large excisional specimens, we have had two patients whose diagnosis of adenoma was changed to hepatoma after recurrence of the tumor. For these reasons, liver cell adenomas of any size should be excised with adequate margins (Table VIII).
TABLE VIII.
INDICATION FOR EXCISION OF BENIGN HEPATIC LESIONS
| Cavernous hemangioma |
|---|
| Rupture |
| Hemorrhage into the necrotic center |
| Significant symptoms related to a large mass |
| Relatively asymptomatic hemangioma with central necrosis |
| Changes in size and character by imaging technique |
| Hematologic abnormality |
| Diagnosis uncertain |
| Liver cell adenoma |
| Rupture |
| Hemorrhage into the necrotic center |
| Significant symptoms related to a large mass |
| Safe to excise all adenomas regardless of size and symptoms beause of high incidence of rupture and hemorrhage |
| Diagnosis uncertain |
| Focal nodular hyperplasia |
| Significant symptoms related to a large mass |
| Changes in size and character by imaging technique |
| Diagnosis uncertain |
| Congenital cyst or cysts |
| Significant symptoms related to a large mass |
| Fever and chills; infection |
| Jaundice |
| Irregular cystic wall; suspicious of a malignant lesion |
Asymptomatic cavernous hemangiomas of several centimeters can be observed safely, because spontaneous rupture is uncommon. Percutaneous needle biopsy of suspected hemangiomas must be avoided, as the danger of hemorrhage is real and the diagnosis usually cannot be confirmed by this procedure. Various imaging techniques are reliable in establishing the diagnosis. Once the observation has been made, the hemangiomas should be observed closely with an imaging technique of one kind or another. When the size or character changes, or both, the lesion must be reinvestigated thoroughly, and the plan of management should be reassessed accordingly (Table VIII). Too often, in our experience, the imaging diagnosis of cavernous hemangioma was found to be incorrect at operation. Tragic errors of our own occurred in one patient with adrenal carcinoma, one patient with epithelioid hemangioendothelioma and one patient with angiosarcoma that were observed as cavernous hemangiomas.
Symptomatic hemangiomas can be treated most effectively and safely by excisional therapy as well-documented in this study. There was no operative death in treating 114 patients and 90 per cent of symptomatic patients were completely relieved from their complaints. Legation, embolization and radiation therapy of the hepatic artery have lost their roles in the treatment of cavernous hemangiomas.
Aspiration, sclerotherapy, internal drainage, marsupialization and fenestration have all been recommended for use in treating congenital hepatic cysts. These therapeutic methods can no longer be a justifiable treatment for single or localized multiple cysts because complete excision can be performed safely and effectively. The problem of missed diagnosis was also experienced in four of the patients with hepatic cysts whom we studied. In three of the four patients, the cysts had been internally drained through jejunal Roux limbs at other institutions. By the time we performed excision of the cysts for recurrent pain and fever, squamous cell carcinoma of the cystic wall had spread regionally in these patients. They all died of carcinomatosis in six to 16 months. The only survivor had excisional therapy after repeated aspirations. The examination of the cystic wall after complete excision revealed a small adenocarcinoma. The patient is well and tumor-free for more than two years after operation.
Focal nodular hyperplasia usually does not cause extreme symptoms. It is safe to observe the tumor if the diagnosis is established with certainty. However, its differentiation from adenoma or fibrolamellar hepatoma by imaging techniques is often difficult. The results of a small specimen taken at biopsy misguided us to the diagnosis of adenoma twice and fibrolamellar hepatoma once. If a tumor causes definite symptoms, it should be excised entirely (Table VIII).
Our general approach to incidental solid hepatic tumors of less than 3 cenitmeters in diameter has been close observation and repeat ultrasonography or CT scan examination if there is no reason to be suspicious of a malignant condition. Any increase in its size or changes in imaging characteristics should be a signal for excision. Larger incidental tumors, with possible exceptions of hemangioma and focal nodular hyperplasia, usually should be excised.
A case can be made for observing large cavernous hemangiomas. Hemangiomas exceeding 10 centimeters in diameter and have central necrosis can rupture or bleed internally. Two of the 31 patients with this type of lesion had emergent operation for rupture and 15 others required urgent operation because of an acutely enlarging painful mass. More and more frequently, we have come to the conclusion that this type of large hemangioma justifies excision before severe complications occur.
SUMMARY
Hepatic resection was performed without an operative death occurring in 114 patients with cavernous hemangioma, 25 patients with liver cell adenoma, 23 patients with focal nodular hyperplasia, 23 patients with congenital cyst, five patients with hydatid cyst, five patients with Caroli’s disease and five patients with other solid tumors. Only five of the 219 patients with benign hepatic lesions died within a month after operation: two patients with acute trauma, two with hepatic abscess and one patient with cirrhosis.
Twenty-five significant but successfully treated complications developed in 14 of 219 patients. Complete symptomatic relief was achieved in 90 per cent of the patients and partial relief in 10 per cent after excision of benign hepatic lesions.
Acknowledgments
This study was supported by Research Grants from the Veterans Administration and Project Grant No. DK 29961 from the National Institutes of Health, Bethesda, Maryland.
References
- 1.Starzl TE, Bell RH, Beart RW, et al. Hepatic trisegmentectomy and liver resections. Surg Gynecol Obstet. 1975;141:429–437. [PMC free article] [PubMed] [Google Scholar]
- 2.Starzl TE, Koep IJ, Weil R, III, et al. Right trisegmentectomy for hepatic neoplasma. Surg Gynecol Obstet. 1980;150:1–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Starzl TE, Iwatsuki S, Shaw BW, Jr, et al. Left hepatic trisegmentectomy. Surg Gynecol Obstet. 1982;155:21–27. [PMC free article] [PubMed] [Google Scholar]
- 4.Starzl TE, Koep IJ, Weil IER, et al. Excisional treatment of cavernous hemangiomas of the liver. Ann Surg. 1980;192:25–27. doi: 10.1097/00000658-198007000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Starzl TE, Iwatsuki S, Shaw BW, Jr, et al. Treatment of fibrolamellar hepatoma with partial or total hepatectomy and transplantation of the liver. Surg Gynecol Obstet. 1986;162:145–148. [PMC free article] [PubMed] [Google Scholar]
- 6.Weil R, III, Koep IJ, Starzl TE. Liver resection for hepatic adenoma. Arch Surg. 1979;114:178–180. doi: 10.1001/archsurg.1979.01370260068010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iwatsuki S, Shaw BW, Jr, Starzl TE. Experience with 150 liver resections. Ann Surg. 1983;197:247–253. doi: 10.1097/00000658-198303000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iwatsuki S, Esquivel CO, Gordon RG, et al. Liver resection for metastatic colorectal cancer. Surgery. 1986;100:804–810. [PMC free article] [PubMed] [Google Scholar]
- 9.Iwatsuki S, Starzl TE. Personal experience with 411 hepatic resections. Ann Surg. 1988;208:421–434. doi: 10.1097/00000658-198810000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iwatsuki S, Sheahan DG, Starzl TE. The changing face of hepatic resection. Curr Probl Surg. 1989;26:283–379. doi: 10.1016/0011-3840(89)90022-1. [DOI] [PMC free article] [PubMed] [Google Scholar]