Introduction
Doctors are trained to diagnose and treat ill health. Within the confines of the one‐to‐one relationship with patients behind the closed door of the consulting room most clinicians fulfil this role highly successfully. But the traditional role of the doctor is carried out within a broader historical, organizational, social and political context – where the diagnosis and treatment of system failures can be as important as clinical interactions with individual patients. Unless doctors are willing to understand and influence this wider context, their ability to improve health outcomes in an increasingly complex environment will be challenged. This understanding can be achieved by engaging with the emerging science of Quality Improvement. In this paper we describe the medical profession's current approach to improving quality and assess where this approach has got us. We then compare current practice with an alternative approach which focuses not only on patients but also on the wider health system and we examine the opportunities and challenges that this presents to the medical profession.
How doctors view quality
Most doctors see providing high quality care as not only a professional responsibility but also as their raison d'être; delivering quality is their work.1,2 For many, their focus is usually on the patient in front of them, sometimes on populations. They tend to concentrate on clinical effectiveness and safety, often leaving wider dimensions of quality, such as efficiency, equity, patient‐responsiveness, access and coordination to others. The profession has increasingly been encouraged to adopt a standards‐based approach and regard discrete phases of education – undergraduate, postgraduate and continuing professional education – as the mechanism by which these standards are delivered. They are trained as scientists and regard the randomized controlled trial as the gold standard of evidence. Progress is achieved by rolling out trial findings and therefore occurs in intermittent but large steps.
What has this approach to quality achieved?
Many would argue that this view of quality has got us a long way and that the NHS is significantly better now than it was 10 or 20 years ago. But there is no shortage of evidence describing deficiencies in the health service: one in 10 patients admitted to hospital experiences iatrogenic harm;3 wide variations in quality of care exist across the country;4 some health inequalities are getting worse rather than better;5 care is often poorly coordinated and patients do not always experience the level of care that doctors would regard as acceptable for themselves or their families;6 resources are wasted, and parts of the workforce demoralized.7
Some doctors claim that these problems are not their responsibility; that they did not enter medicine to ‘become a manager’. Most clinicians respond like Boxer, the carthorse in George Orwell's Animal Farm,8 by just working harder – and in doing so there is a risk that they are heading for the same fate. But neither of these approaches are helpful and an increasing number of people are recognizing that significant change in how services are designed and care is provided is required if these deficiencies are to be overcome.9
A different approach to quality
The science of quality improvement is well established in the commercial world and is central to business success. The car manufacturer Toyota, one of the leaders in the field, has developed a system of working practices which enables every employee to function as a ‘scientist’ performing continual improvement experiments.10 If applied to the health sector this approach has the potential to build on the strengths of the medical profession by equipping all doctors to continuously address local difficulties on a day‐to‐day basis, while enabling some to tackle whole system change. The traditional and new approaches differ in a number of ways ( Table 1):
Of course delivering a high standard of care is a professional responsibility but professionalismmust also encompass a commitment to continuously striving for better ways ofworking. This needs to be embedded at an early stage of medical training in the way that the University of Chicago Pritzker School of Medicine has achieved11 so that in the future clinicians recognize that they have two jobs – doing their work and improving how they do their work;12
In addition to clinical effectiveness, doctors must accept responsibility for other dimensions of quality. Indeed, a defining role of the doctor of the future – and a justification for their intensive training, status and remuneration – should be their willingness to balance the inherent tensions between providing all possible care for individuals and designing systems which make clinically effective care available to whole populations;
In addition to influencing patients and populations, doctors will need to influence the systems within which care is provided, even if this partially removes them from face‐to‐face patient care and results in doctors having to make difficult decisions about resources;
In addition to a commitment to standards and to traditional medical education, doctors must commit themselves and their peers to continuous learning and to the creation of what has been described as ‘learning organizations’;13
In addition to a commitment to bio‐science, doctors must understand the contribution of the behavioural sciences, accept both the strengths and weaknesses of different types of evidence and use whatever knowledge is appropriate to address the problem in hand. This will include a commitment to small scale change and rapid cycle testing characteristic of quality improvement. It will require a commitment to measurement and an understanding of statistical techniques used in the field of quality improvement such as statistical process control and the differentiation between common cause and special cause variation.14
Table 1.
Comparison of the traditional and a new approach of the medical profession to improving quality
| Traditional approach | New approach | |
|---|---|---|
| Attitude | Quality is what we do | Quality is what we strive for |
| Scope | Clinical effectiveness | Multiple dimensions of quality |
| Focus | Patients (populations) | Patients/populations and systems |
| Requisites | Standards delivered by high quality education | Continuous improvement through learning |
| Knowledge base | Bio‐science based on the scientific method | Biomedicine plus behavioural sciences |
| Scale | Large scale ‘roll‐out’ of evidence | Small scale testing and context‐specific spread |
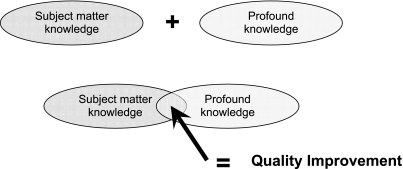
WE Deming, a scion of the Quality Improvement world, described why he saw that the methods used for quality improvement, which draw on a wide range of established disciplines, should be regarded as a scientific discipline in their own right.14 He identified the core features of the discipline as thinking about systems, understanding variation, a commitment to the behavioural sciences and a broad appreciation of what constitutes ‘knowledge’ and he called them ‘profound knowledge’. While doctors are well versed in the basic medical sciences and the clinical method, few possess the knowledge or skills to put profound knowledge into practice and even fewer are able to bring together their medical expertise with improvement expertise in a way which allows them to optimize their working environment for the benefit of patients ( Figure 1).
Figure 1.
How improving quality requires bringing together subject matter knowledge and profound knowledge
Recommendations
There are plenty of examples of organizations and clinicians contributing to improvement initiatives. Many organizations have introduced local referral guidelines and established networks to improve the management of common conditions for problems such as diabetes or substance abuse. Others have reorganized local services to reduce waiting times and improve clinical outcomes. There are some notable national initiatives, such as the introduction of the Picture Archiving and Communication System (PACS) which is revolutionizing the delivery of radiology services in the NHS. But at present only a small number of clinicians have the will, capacity or capability to contribute at the level required to produce sustained system‐wide improvement. We recommend that the following approaches will help clinicians to engage more fully.
Education and training in improvement science
Since a lack of knowledge and skills about improvement science is one of the key barriers to improving quality,2 educational solutions are key. There is evidence that educational interventions to improve quality of care are effective,15,16 particularly when integrated throughout the established curriculum, rather than ‘bolted‐on’ as a separate module.12,17 The science of improvement will need to become part, not only of the undergraduate and specialist training curricula, but also of continuing professional development programmes so that the current workforce has the skills to operate effectively.
Learning about improvement differs from traditional medical education not only in terms of content but also in ethos and style. The principles are those of adult learning, with a strong emphasis on active learning rather than passive teaching, on experimentation, self‐reflection and on feedback.12,18 The NESC (NHS Education South Central) Professional Programme in the UK, and the Brigham & Women's Hospital Physician Leadership Programme taught at Harvard Business School in the USA, are examples of progressive educational initiatives meeting the needs of young and mid‐career doctors. More of these programmes are needed, learning from existing programmes needs to be shared and they must be properly evaluated to construct effective evidence‐based education.
Incentives
There are currently few incentives for doctors to make a significant contribution to system improvement beyond face‐to‐face clinical care. Becoming an expert in quality improvement is a low status career choice in comparison with becoming a researcher or an educator.2,19 The narrow pursuit of clinical targets tends to focus attention on current service delivery, rather than on designing future system change. Clinicians who take up senior management roles often experience a drop in salary and the Clinical Excellence Award system does not adequately recognize a broader contribution to service improvement. Aligning both financial and non‐financial incentives to improvement activities will help to attract the most able doctors into the new discipline.
Leadership from professional organizations
Only a small number of the medical Royal Colleges and specialist societies are demonstrating active leadership of the quality improvement agenda. The Royal College of Psychiatrists is a shining example of what can be done. In recent years it has reorganized itself internally to give a high profile to improvement activities and it has initiated a number of innovative improvement programmes. Leadership of improvement science provides an important vehicle for professional bodies to work together and to demonstrate the potential of collective professional action.
Revalidation
US doctors are well ahead of their UK colleagues in learning about and applying quality improvement methods and one of the main drivers has been professional re‐accreditation. The reform of professional regulation in the UK provides an opportunity to raise the profile of improvement science. There are already plans to revitalize clinical audit as a central component of appraisal and therefore a prerequisite for revalidation.20 Audit is just one component of the science of improvement and so the opportunity should be seized to ensure that quality improvement is a more explicit and more integrated component of the General Medical Council's Good Medical Practice, which forms the basis of revalidation.
Improvement at all levels
System change can occur at various levels – from small local initiatives at ward or practice level, to whole system change at a national level. Every doctor should have the skills to influence change in their immediate working environment, and some should be supported to influence change at a regional or national level as evidenced by the direction that NHS South Central has taken to become a clinically‐focused organization.
Conclusions
As the delivery of healthcare becomes more complex and the role of doctors within the system evolves, it will become increasingly clear that most doctors are only partially trained for the challenges that they face. In the future it will not be possible to be an effective clinician without both a theoretical and a practical understanding of the science of quality improvement. The profession, the academic community, the NHS and policy‐makers must rise to this challenge.
Footnotes
DECLARATIONS —
Competing interests None declared
Funding This work was made possible by the Commonwealth Fund of New York and The Health Foundation, London who supported PMH as a Harkness Fellow in the United States
Ethical approval Not applicable
Guarantor MNM
Contributorship MNM originally formulated the project's broad scope and PMH wrote the first draft. Both authors then reviewed and contributed to successive drafts. Both authors had full input into all stages of this work
Acknowledgements
The opinions expressed in this article are not necessarily those of either the Commonwealth Fund or the Health Foundation who had no involvement in the preparation of this paper
References
- 1.Checkland K. National Service Frameworks and UK general practitioners: street‐level bureaucrats at work? Sociol Health Illn. 2004;26:951–75. doi: 10.1111/j.0141-9889.2004.00424.x. [DOI] [PubMed] [Google Scholar]
- 2.Davies H, Powell A, Rushmer R. Healthcare professionals' views on clinician engagement in quality improvement. London: The Health Foundation; 2007. [Google Scholar]
- 3.Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ. 2001;322:517–19. doi: 10.1136/bmj.322.7285.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.London: The Health Foundation; Quest for Quality and Improved Performance. See www.health.org.uk/current_work/research_development/qquip.html. [Google Scholar]
- 5.Shaw M, Davey Smith G, Dorling D. Health inequalities and New Labour: how the promises compare with real progress. BMJ. 2005;330:1016–21. doi: 10.1136/bmj.330.7498.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.London: The Healthcare Commission; 2007. National survey of adult inpatients 2007. See www.healthcarecommission.org.uk/healthcareproviders/nationalfindings/surveys/healthcareproviders/surveysofpatients/acutecare/surveyofadultinpatients2007.cfm. [Google Scholar]
- 7.Smith R. Why are doctors so unhappy? There are probably many causes, some of them deep. BMJ. 2001;322:1073–4. doi: 10.1136/bmj.322.7294.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orwell G. Animal Farm. London: Secker and Warburg; 1945. [Google Scholar]
- 9.New York: The Commonwealth Fund; 2007. 2007 International Health Policy Survey in Seven Countries. See www.commonwealthfund.org/surveys/surveys_show.htm?doc_id=568326. [Google Scholar]
- 10.Spear S, Bowen H. Decoding the DNA of the Toyota Production System. Harvard Business Review. 1999;Sept–Oct:95–106. [Google Scholar]
- 11.Humphrey HJ, Smith K, Reddy S, Scott D, Madara JL, Arora VM. Promoting an environment of professionalism: the University of Chicago “Roadmap”. Acad Med. 2007;82:1098–107. doi: 10.1097/01.ACM.0000285344.10311.a8. [DOI] [PubMed] [Google Scholar]
- 12.Batalden P, Davidoff F. Teaching quality improvement: the devil is in the details. JAMA. 2007;298:1059–61. doi: 10.1001/jama.298.9.1059. [DOI] [PubMed] [Google Scholar]
- 13.Davies HT, Nutley SM. Developing learning organisations in the new NHS. BMJ. 2000;320:998–1001. doi: 10.1136/bmj.320.7240.998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deming W. Out of the Crisis. Cambridge, MA: MIT, Center for Advanced Educational Services; 1982. [Google Scholar]
- 15.Jamtvedt G, Young JM, Kristoffersen DT, O'Brien MA, Oxman AD. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2006;(2) doi: 10.1002/14651858.CD000259.pub2. CD000259. [DOI] [PubMed] [Google Scholar]
- 16.Stone EG, Morton SC, Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: a meta‐analysis. Ann Intern Med. 2002;136:641–51. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 17.Boonyasai RT, Windish DM, Chakraborti C, Feldman LS, Rubin HR, Bass EB. Effectiveness of teaching quality improvement to clinicians: a systematic review. JAMA. 2007;298:1023–37. doi: 10.1001/jama.298.9.1023. [DOI] [PubMed] [Google Scholar]
- 18.Batalden PB, Davidoff F. What is “quality improvement” and how can it transform healthcare? Qual Saf Health Care. 2007;16:2–3. doi: 10.1136/qshc.2006.022046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grol R, Berwick DM, Wensing M. On the trail of quality and safety in health care. BMJ. 2008;336:74–6. doi: 10.1136/bmj.39413.486944.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Department of Health. Good doctors, safer patients. London: Department of Health; 2006. See www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4137232. [Google Scholar]