Abstract
We investigated mediators hypothesized to account for the effects of two eating disorder prevention programs using data from 355 adolescent females who were randomized to a dissonance or healthy weight intervention or an active control condition. The dissonance intervention produced significant reductions in outcomes (body dissatisfaction, dieting, negative affect, bulimic symptoms) and the mediator (thin-ideal internalization), change in the mediator correlated with change in outcomes and usually occurred before change in outcomes, and intervention effects became significantly weaker when change in the mediator was partialed, providing support for the hypothesized mediators and this new approach to testing mediation in randomized trials. Findings provided somewhat less support for the hypothesis that change in healthy eating and exercise mediated the healthy weight intervention effects.
Keywords: bulimic symptoms, eating disorders, prevention, mediation
Approximately 10% of adolescent females experience threshold or subthreshold eating disorders, which are characterized by a chronic course, medical complications, and functional impairment, and increases risk for future onset of obesity, depression, suicide attempts, anxiety disorders, substance abuse, and health problems (Johnson, Cohen, Kasen, & Brook, 2002; Lewinsohn, Streigel-Moore, & Seeley, 2000; Stice, Cameron, Killen, Hayward, & Taylor, 1999). Although numerous eating disorder prevention programs have been evaluated in controlled trials, only six have produced significant reductions in current or future symptoms that persisted over follow-up, and only two produced effects that replicated across labs (Stice & Shaw, 2004).
The first intervention that produced replicable effects is a dissonance-based program, in which at-risk girls with body image concerns who have internalized the thin-ideal voluntarily engage in verbal, written, and behavioral exercises in which they critique this ideal. These counter-attitudinal activities theoretically result in psychological discomfort that motivates them to reduce their thin-ideal internalization to restore cognitive consistency, which in turn decreases eating disorder risk factors and bulimic symptoms. Controlled trials indicate that the dissonance intervention results in significantly greater reductions in thin-ideal internalization, body dissatisfaction, negative affect, and bulimic symptoms than a waitlist control condition through 6-month follow-up and significantly greater reductions in thin-ideal internalization and body dissatisfaction than an alternative intervention (Becker, Smith, & Ciao, 2005; Matusek, Wendt, & Wiseman, 2004; Stice, Chase, Stormer, & Appel, 2001; Stice, Mazotti, Weibel, & Agras, 2000; Stice, Trost, & Chase, 2003).
The second intervention that produced replicable effects is a healthy weight management program that promotes lasting healthy changes to dietary intake and physical activity as a way of achieving a healthy body weight and body satisfaction among at-risk girls with body image concerns. Independent trials have found that this intervention produces reductions in body dissatisfaction, dieting, negative affect, and bulimic symptoms that are often larger than reductions observed in waitlist control groups and that most effects persist through 6-month follow-up (Matusek et al., 2004; Stice, Chase et al., 2001; Stice, et al., 2003). Parenthetically, the dissonance and healthy weight interventions have targeted at-risk girls because selected prevention programs tend to produce larger effects than universal programs (Stice & Shaw, 2004).
Because the dissonance and healthy weight interventions appear to be the only two prevention programs to produce significant intervention effects for eating pathology in independent trials, we initiated a large efficacy trial of these two interventions that addressed certain methodological limitations of prior studies. We (1) compared our interventions to an active control intervention to rule out the possibility that intervention effects were due to demand characteristics, expectancies, or attention, (2) used blinded diagnostic interviews to assess eating pathology, (3) used a long-term follow-up, and (4) used a larger and more ethnically diverse sample relative to prior trials. In this 4-group trial, 481 adolescent females were randomly assigned to the dissonance intervention, the healthy weight intervention, an expressive writing active control condition, or an assessment-only control condition. An initial report focusing on the main effects through 1-year follow-up indicated that dissonance participants showed greater reductions in eating disorder risk factors (thin-ideal internalization, body dissatisfaction, negative affect, and dieting) and bulimic symptoms than healthy weight, expressive writing, and assessment-only participants, and healthy weight participants showed greater reductions in these outcomes than expressive writing and assessment-only participants, though some effects faded over follow-up (Stice, Shaw, Burton, & Wade, 2006). Participants in both interventions also showed lower binge eating and obesity onset and decreased mental health service utilization than expressive writing and assessment-only controls.
The present report sought to test hypotheses regarding the mediators that theoretically account for the intervention effects for the dissonance and healthy weight interventions on the main outcomes. Mediation analyses provide a test of the mechanisms that putatively underlie intervention effects (Coie et al., 1993). If the interventions decrease bulimic symptoms in the absence of changes in the hypothesized mediators, or decrease the mediators in the absence of effects on bulimic symptoms, it would suggest a problem with the intervention theory. These analyses also test whether the mediators that are theoretically specific to an intervention account for the intervention effects. Additionally, these analyses may suggest ways to further improve the intervention, such as providing evidence that it is not sufficient to change particular mediators.
To our knowledge, only one previous eating disorder prevention trial examined the mediators of intervention effects. Bearman, Stice, and Chase (2003) tested whether change in body dissatisfaction mediated the effects of a body acceptance intervention on change in depressive and bulimic symptoms. Results indicated that (1) treatment condition (versus waitlist condition) predicted pre to post decreases in body satisfaction (r = .32), (2) treatment condition predicted pre to post decreases in depressive (r = .30) and bulimic symptoms (r = .30), (3) pre to post decreases in body dissatisfaction correlated with pre to post decreases in depressive (r = .38) and bulimic symptoms (r = .41), and (4) that the treatment effects on pre to post decreases in depressive (r′ = .18, a 40% reduction in effect size) and bulimic symptoms (r′ = .16 a 47% reduction in effect size) were no longer significant when decreases in body dissatisfaction were statistically controlled. Because the intervention effects on change in depression and bulimic symptoms in these last two models were not equal to zero, results suggest that change in body dissatisfaction partially mediated the effects of the intervention on change in depressive and bulimic symptoms.
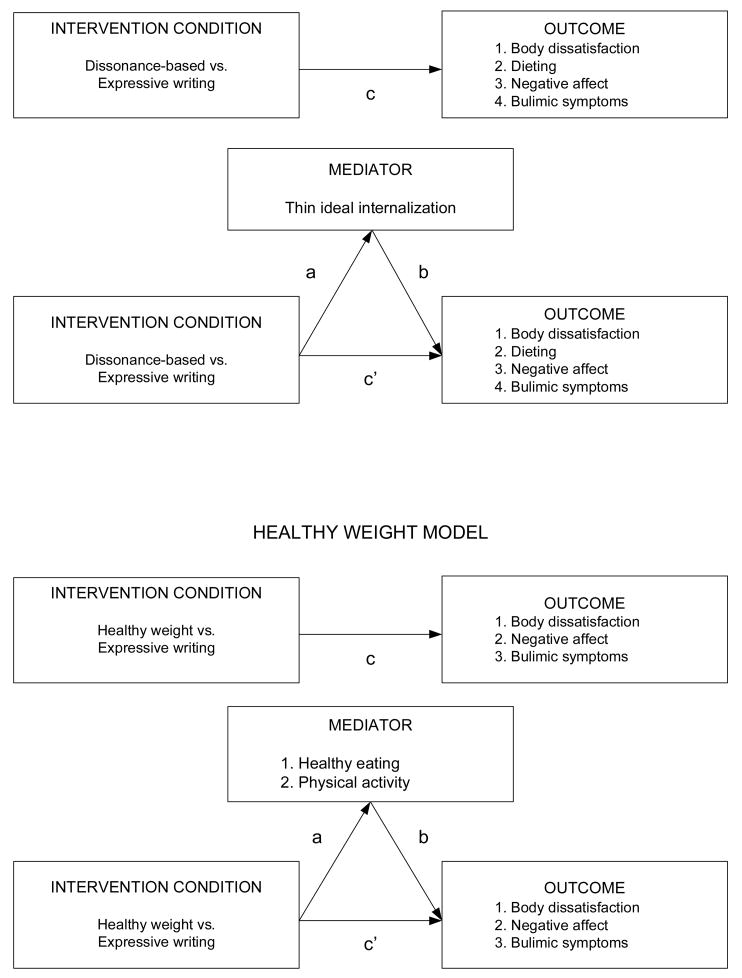
Given that most eating disorder prevention trials have not tested the hypothesized factors that mediate the intervention effects, the primary aim of this report was to conduct an in-depth test of mediation using data from a large randomized trial of the dissonance and healthy weight prevention programs. We hypothesized that reductions in thin-ideal internalization would mediate the effects of the dissonance intervention, versus the expressive writing control condition, on reductions in body dissatisfaction, dieting, negative affect, and bulimic symptoms (Figure 1). Because the dissonance intervention was designed to reduce thin-ideal internalization, we focused on this factor as the sole mediator of any intervention effects. Based on the dual pathway model of bulimic pathology (Stice, Mazotti et al., 2001), we expected a reduction in thin-ideal internalization to result in subsequent decreases in body dissatisfaction, dieting, negative affect, and bulimic symptoms. Theoretically, elevated internalization of the thin-ideal produces body dissatisfaction and negative affect because this ideal is difficult to attain and appearance is a central evaluative dimension for females in our culture. Thin-ideal internalization is also thought to result in dieting as a means of achieving the thin-ideal. Those who have internalized the thin-ideal may resort to radical compensatory behaviors, such as vomiting or laxative abuse, for weight control purposes. Negative affect and dietary restraint are also thought to increase the risk for binge eating.
Figure 1.
Graphical representation of the hypothesized mediators of the dissonance-based and healthy weight interventions.
We hypothesized that improvements in healthy eating and physical activity would mediate the effects of the healthy weight intervention, versus the expressive writing control condition, on reductions in body dissatisfaction, negative affect, and bulimic symptoms (Figure 1). The healthy weight intervention was expected to produce lasting improvements in dietary intake and physical activity because these were the primary targets of this intervention. Improvements in healthy eating and physical activity theoretically foster feelings of control over body shape and promote body satisfaction, as body mass is a key predictor of body satisfaction (Jones, 2004). Improvements in dietary intake and activity were also expected to reduce negative affect, based on results of prior trials of interventions targeting these factors (Klem, Wing, Simkin-Silverman, & Kuller, 1997). Further, an intervention that promotes limited consumption of high-fat and high-sugar foods and encourages healthy weight control behaviors (regular exercise) should decrease the risk for binge eating and for unhealthy weight control behaviors such as vomiting.1
The secondary aim of this report was to propose a more rigorous test of mediation for randomized trials. Although advances have been made with regard to techniques for testing mediation, we believe a more rigorous test is possible. Extending Baron and Kenny’s (1986) criteria for mediation to the context of randomized trials, we propose that the strongest case for mediation would be made when these five conditions are satisfied:
Participants in the intervention condition show significantly greater decreases on the outcome over time than controls (treatment condition predicts change in the outcome; path c in Fig. 1).
Participants in the intervention condition show significantly greater decreases on the mediator over time than controls (treatment condition predicts change in the mediator; path a).
Change in the mediator over time is significantly correlated with change in the outcome over time in the intervention condition (path b).
The predictive effect of intervention condition on change in the outcome, controlling for change in the mediator (path c′), is significantly reduced (for partial mediation) or eliminated (for complete mediation), relative to when the outcome is regressed only on intervention condition (path c).
Meaningful change in the mediator occurs before meaningful change in the outcome significantly more frequently than would be expected based on chance in the intervention condition.
Several investigators have proposed using the first three (e.g., Kraemer, Wilson, Fairburn, & Agras, 2002) or four criteria for testing mediation in randomized controlled trials (e.g., Bearman et al., 2003; Gillham, Reivich, Jaycoxm & Seligman, 1995; Hinshaw, 2002; Kaufman, Rohde, Seeley, Clarke, & Stice, 2005). Although this general approach is more rigorous than prior techniques for testing mediation in randomized trials, it does not provide evidence of the hypothesized temporal sequencing in which the mediator changes before the outcome. It is thus possible that change in the outcome preceded change in the mediator for the majority of cases, which, seems incompatible with the concept of mediation. It has been noted that it is vital to document that change in the mediator precedes change in the outcome in order to establish mediation in randomized trials (Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001). The addition of our fifth criterion for mediation provides one potential approach to testing whether change in the mediator precedes change in the outcome.
We also tested whether there was evidence of specificity for the putative mediators for each intervention. Documenting that the theorized mediators are specific to each intervention, but not alternative interventions, is an important and necessary component for demonstrating mechanisms of change in randomized trials (Kazdin & Nock, 2003).
We tested for mediation from pre to post because this is typically the period in which the most pronounced intervention effects occur. It is also often the case that there are linear changes in the outcome from pre to post, but that intervention effects tend to level out or erode during follow-up, which makes modeling change more difficult. Thus, in accordance with the recommendations of Hinshaw (2002), we collected weekly measures of the mediators and outcomes during the 4-week pre to post period to provide a sensitive test of whether change in the hypothesized mediators occurred before change in the outcomes. We used data from the expressive writing control condition, rather than the assessment-only control condition, because it reduces the chances that any intervention effects could be due to expectancies, demand characteristics, or attention.
Methods
Participants and Procedure
Participants were 355 adolescent females (M age = 17.1, SD = 1.4). We focused on females because they are at high risk for eating pathology (Lewinsohn et al., 2000). The sample was 11% Asian/Pacific Islander, 5% Black, 17% Hispanic, 61% Caucasian, and 6% who specified “other” or mixed racial heritage; which was representative of the schools from which we sampled (65% Caucasian). Parental education, a proxy for socioeconomic status, ranged from high school graduate or less (17%) to graduate/professional degree (28%), with a mode of college graduate (31%), which was representative of the city from which we sampled (34% high school graduate or less; 25% some college; 26% college graduate; 15% graduate degree).
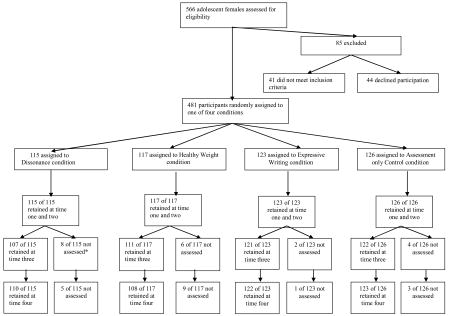
Participants were recruited from high schools and a university using direct mailings, flyers, and leaflets inviting females between the ages of 14 and 19 with body image concerns to participate in a study evaluating interventions designed to promote body acceptance. Informed written consent was obtained from all participants (and their parents for minors). For inclusion, the students had to endorse body image concerns during a phone screen. This approach attracted at-risk females with elevated body dissatisfaction and thin-ideal internalization compared to mean scores on these variables from a normative sample (Stice et al., 2006). Participants who met criteria for DSM-IV anorexia nervosa, bulimia nervosa, or binge eating disorder at pretest were given a treatment referral and excluded. The Flowchart in the Appendix provides details about participants who were excluded from this trial. Participants were randomized to the dissonance intervention, healthy weight intervention, expressive writing control intervention, or assessment-only control condition, although we did examine the last condition for this report. The dissonance and healthy weight interventions consisted of 3 weekly 1-hour group sessions with 6–10 participants. A scripted manual was developed for both interventions. The expressive writing condition consisted of 3 weekly 45-minute individual writing sessions. We used an expressive writing control intervention to isolate the effects of demand characteristics and expectancy effects from non-specific factors (e.g., social support from group members), because we believe the latter factors contribute to the beneficial effects of group-based prevention programs such as the dissonance and healthy weight programs. Although participants completed clinical interviews, this report focuses on data collected via surveys completed one week before the first session, at the end of the first session, at the end of the second session, and at the end of the third and final session (T1, T2, T3, and T4). Participants received $10 for completing each survey. The University of Texas Institutional Review Board approved this project. See Stice et al, (2006) for details about interviewer training, diagnostic reliability, facilitator training, and intervention content.
Dissonance intervention
In this intervention, participants voluntarily engage in verbal, written, and behavioral exercises in which they critique the thin-ideal ideal. These exercises were conducted in sessions and in between-session homework activities. For example, participants wrote a counter-attitudinal essay about the costs associated with pursuit of the thin-ideal and engaged in a counter-attitudinal role-play in which they attempted to dissuade facilitators from pursuing the thin-ideal.
Healthy weight intervention
In this intervention, participants were encouraged to make healthy and lasting changes to their diet and physical activity level as a way of balancing their energy needs with their energy intake, and thereby achieving a healthier weight and body satisfaction. With support from the facilitator and other group members, each participant initiated an individual lifestyle change plan to reduce intake of fat and sugar and to increase physical activity. Food and exercise diaries were used to identify behaviors to target in this lifestyle modification and to monitor change. Motivational interviewing was also used to enhance motivation for behavioral change.
Expressive writing control intervention
In this condition, which is based on the work of Pennebaker (1997), participants wrote about emotionally significant topics in three individual weekly 45-minute sessions. They were told that research has found that body dissatisfaction is linked to emotional issues and that expressive writing helps resolve these issues. Sample topics included relationships or goals. They were told that their work would not be read and were asked to write continuously for the duration of the session about an emotionally important topic.
Measures
Thin-ideal internalization
The eight-item Ideal-Body Stereotype Scale-Revised assessed thin-ideal internalization (Stice, Fisher et al., 2004). Items used a response format ranging from 1 = strongly disagree to 5 = strongly agree. Items were averaged for this scale and those described below. This scale has shown internal consistency (α = .91), test-retest reliability (r = .80), and predictive validity for bulimic symptom onset (Stice, Fisher et al., 2004).
Healthy eating
We generated four items assessing healthy eating behaviors (I have reduced the amount of fat in my diet, I have eaten more fruits and vegetables, I have chosen low fat foods in my diet, I have cut down on the amount of carbohydrates I eat). Response options ranged from 1 = strongly disagree to 5 = strongly agree. These items were averaged to form an overall healthy eating composite. This scale was internally consistent (α = .82) at pretest and temporally reliable in this study (1-month test-retest r = .63 for assessment-only controls).
Physical activity
We generated two items assessing weekly frequency of exercise (How many days did you exercise during the past week) and duration of exercise (On average, how long did you exercise during the past week). These two items were multiplied to form a quantity × frequency measure of exercise behavior at each assessment. This scale was temporally reliable in this study (1-month test-retest r = .61 for assessment-only controls). Such quantity-by-frequency measures have been used to provide reliable and valid measures of other health behaviors, such as substance use (Grant, Tonigan, & Miller, 1995).
Body dissatisfaction
Body dissatisfaction was assessed with eight items from of the Satisfaction and Dissatisfaction with Body Parts Scale (Berscheid, Walster, & Bohrnstedt, 1973). Participants indicate their level of satisfaction with body parts (e.g., stomach and hips) on scales ranging from 1 = extremely satisfied to 6 = extremely dissatisfied. This scale has shown internal consistency (α = .94), 3-week test-retest reliability (r = .90), and predictive validity for bulimic symptom onset (Stice, Fisher et al., 2004).
Dieting
The 10-item Dutch Restrained Eating Scale assessed dieting (DRES; van Strien, Frijters, van Staveren, Defares, & Deurenberg, 1986). Participants indicated the frequency of dieting behaviors using scales ranging from 1 = never to 5 = always. The DRES has shown internal consistency (α = .95), 2-week test-retest reliability (r = .82), convergent validity with self-reported caloric intake (though it shows weaker relations to objectively measured intake), and predictive validity for bulimic symptom onset (Stice, Fisher et al., 2004; van Strien et al., 1986).
Negative affect
Negative affect was assessed with 20 items from the sadness, guilt, and fear/anxiety subscales from the Positive Affect and Negative Affect Scale-Revised (Watson & Clark, 1992). Participants reported how much they had felt various negative emotional states on scales ranging from 1 = very slightly or not at all to 5 = extremely. This scale has shown internal consistency (α = .95), 3-week test-retest reliability (r = .78), convergent validity, and predictive validity for bulimic symptom onset (Stice et al., 2003; Watson & Clark, 1992).
Bulimic symptoms
The diagnostic symptoms of bulimia nervosa were assessed with the Eating Disorder Diagnostic Scale (EDDS; Stice, Telch, & Rizvi, 2000). Ten items assessing frequency of binge eating, frequency of compensatory behaviors (e.g., vomiting, laxative/diuretic abuse, fasting, and excessive exercise), and overvaluation of weight and shape were summed to form an overall eating disorder symptom composite. The EDDS has shown high agreement (κ = .78 – .83) with eating disorder diagnoses made with the Eating Disorder Examination (EDE; Fairburn & Cooper, 1993), internal consistency (α = .89), 1-week test-retest reliability (r = .87), sensitivity to detecting intervention effects, and predictive validity for future onset of eating pathology and depression (Stice, Fisher et al., 2004; Stice, Telch et al., 2000).
Statistical Analyses
In this study repeated assessments (level 1) are nested within participants (level 2). To account for the correlations between nested units, a hierarchical linear modeling approach (Raudenbush & Bryk, 2002) was used to assess criteria 1–5 of mediation with the Hierarchical Linear Modeling (HLM) 6 program (Raudenbush, Bryk, & Congdon, 2004). We specified linear growth models based on a priori expectations. The four assessment points representing Time in the equations below were coded such that the intercept reflects the initial level of the variable at pretest (i.e., one week prior to the first session). Group in the equations below represents a dichotomous variable (intervention = 1, control = 0). A common intercept was assumed for all treatment groups because Time was coded with zero as the baseline and randomization was found to produce initially equivalent groups. Because multilevel models do not provide standardized regression coefficients, partial correlation coefficients, computed based on t-values and degrees of freedom (Moscovitch, Hofman, Suvak, & In-Albon, 2005), are provided as an estimate of effect size.
Criterion 1, the effect of the intervention condition on the outcome (Figure 1 path c) and Criterion 2, the effect of the intervention condition on the mediator (path a) were estimated with the following composite multilevel model for change:
Yij is the value of the outcome (path c) or the mediator (path a) for person i at time j. The first set of brackets represents the structural portion of the model; the four fixed effects are average initial status (γ00,), average rate of change (γ10,), effect of condition on initial status (γ01), and effects of condition on rate of change (γ11). The second set of brackets represents the stochastic portion of the model; the three random effects are the unexplained portions of initial status (ζ0i), rate of change (ζ1i), and individual i’s outcome at time j (ζij).
Criterion 3, a relation in the intervention condition between change in the mediator and change in the outcome (path b) was estimated with the following composite multilevel model for change:
Yij is the value of the outcome for person i in the intervention condition at time j. The fixed effects are initial status (γ00), average rate of change (γ10), effect of change in the mediator (γ01), and effect of change in the mediator on rate of change in the outcome, (γ11). Change in the mediator, (γ01), was modeled as a level-2 variable and generated from the Empirical Bayes slope estimates produced from HLM during the testing of criterion 2. The random effects are the unexplained portions of initial status (ζ0i), average rate of change (ζ1i), and individual i’s outcome at time j (ζij).
Criterion 4, the effect of the treatment condition on the outcome controlling for the change in the mediator (path c′) was estimated with the following composite multilevel model for change:
Yij is the value of the outcome for person i at time j controlling for the change in the mediator. The fixed effects are average initial status (γ00), average rate of change (γ10), effect of intervention condition on initial status (γ01), change in the mediator (γ02), effect of condition on rate of change (γ11), and effect of the condition on the change in the mediator (γ12). Change in the mediator, (γ02), was modeled as a level-2 variable and generated from the Empirical Bayes slope estimates produced during the testing of criterion 2. The random effects are the unexplained portions of initial status (ζ0i), rate of change (ζ1i), and individual i’s outcome at time j (ζij). The standard error formula from Freedman & Schatzkin (1992) was used to generate a t-test for determining whether c–c′ was significantly different from zero.
Criterion 5 was assessed using empirical best linear unbiased slope coefficients from the HLM models to estimate the time in weeks to obtain a meaningful change in the mediator compared to a meaningful change in the outcome. We defined meaningful change as a .5 SD reduction in the variables, on an a priori basis, because this corresponds to a medium effect size (Cohen, 1988).2 We calculated time in weeks to a .5 SD reduction in the variables by dividing the value corresponding to .5 SD (from pretest values) by the slope coefficient for that variable for each participant, which was generated from the four weekly measures of the variable from pre to post. This yielded a time in weeks that it took each participant to show a .5 SD in the variable. Among participants in the intervention condition that showed a .5 SD decline in the outcome, we calculated the percentage showing a .5 SD reduction in the mediator before they showed a .5 SD reduction in the outcome; they received a score of 1. Participants who showed a .5 SD decrease in the mediator after they showed a .5 SD decrease in the outcome and those who did not show a .5 SD decrease in the mediator received a score of 0. Participants who did not show a .5 SD decrease in the outcome were excluded from these analyses, as it is not possible to test hypotheses about the timing of change in the mediator relative to the outcome if the outcome does not show meaningful change. We then used a binomial test to determine whether the proportion of participants who showed a meaningful change in the mediator before showing a meaningful change in the outcome was greater than .50 among intervention participants who showed a meaningful reduction on the outcome.
Results
Preliminary Analyses
We verified that the groups did not differ significantly in terms of age, ethnicity, parental education, or any of the mediators or outcomes at pretest, suggesting that randomization created initially equivalent groups. We confirmed that there were no significant differences in ancillary psychiatric treatment or attendance across conditions. A randomly selected 10% of the sessions were audio recorded and coded by a research assistant to assess intervention fidelity; ratings verified that 100% of these sessions covered the main exercises in the intervention manuals. The 4% of participants who dropped from the trial by T4 did not differ from the 96% of participants retained in the trial on any demographic factors or study variables at pretest and attrition did not differ across conditions, suggesting that attrition was not systematic. Nonetheless, we used full information maximum likelihood estimation from HLM to impute missing data because this approach produces more accurate and efficient parameter estimates than list-wise deletion or other imputation approaches (e.g., last-observation-carried-forward; Schafer & Graham, 2002). Results also confirmed that participants perceived the interventions as equally credible, with the exception that the expressive writing condition was perceived as significantly less likely to be beneficial than the healthy weight intervention (see Stice et al., 2006 for details). We confirmed that the linear slopes fit the data and that it was not necessary to introduce quadratic terms. The means in Table 1 corroborate the there was linear change from pre to post.
Table 1.
Means and Standard Deviations for the Raw Mediators and Outcomes at Each of the Weekly Assessments, as well as Mean Intercept and Slope Parameters
| Mean | SD | Mean Intercept | Mean Slope | |
|---|---|---|---|---|
| Thin-ideal internalization | 3.75 | −.14 | ||
| T1 | 3.74 | .52 | ||
| T2 | 3.62 | .58 | ||
| T3 | 3.46 | .62 | ||
| T4 | 3.31 | .71 | ||
| Healthy eating | 2.88 | .06 | ||
| T1 | 2.88 | .80 | ||
| T2 | 2.95 | .86 | ||
| T3 | 2.98 | .77 | ||
| T4 | 3.08 | .83 | ||
| Physical activity | 21.54 | .59 | ||
| T1 | 21.40 | 17.62 | ||
| T2 | 22.24 | 17.82 | ||
| T3 | 22.93 | 18.06 | ||
| T4 | 23.13 | 17.54 | ||
| Body dissatisfaction | 3.50 | −.11 | ||
| T1 | 3.49 | .81 | ||
| T2 | 3.41 | .82 | ||
| T3 | 3.24 | .81 | ||
| T4 | 3.17 | .83 | ||
| Dieting | 2.74 | −.15 | ||
| T1 | 2.74 | .91 | ||
| T2 | 2.60 | .96 | ||
| T3 | 2.43 | .90 | ||
| T4 | 2.29 | .93 | ||
| Negative affect | 2.12 | −.16 | ||
| T1 | 2.15 | .88 | ||
| T2 | 1.94 | .83 | ||
| T3 | 1.76 | .79 | ||
| T4 | 1.68 | .77 | ||
| Bulimic symptoms | 21.07 | −3.54 | ||
| T1 | 21.81 | 12.44 | ||
| T2 | 16.82 | 11.22 | ||
| T3 | 13.21 | 9.89 | ||
| T4 | 11.21 | 9.75 |
Test of Hypothesized Mediators
Criterion 1
To test whether condition predicted future change in outcomes (path c), HLM models tested whether the dummy-coded vector representing treatment condition predicted the slope parameter for each outcome controlling for the intercept of the respective outcome. Condition-by-time effects confirmed that dissonance participants showed significantly greater reductions in body dissatisfaction, dieting, negative affect, and bulimic symptoms than expressive writing controls (Table 2) and that the healthy weight participants showed significantly greater reductions in body dissatisfaction, negative affect, and bulimic symptoms than expressive writing controls (Table 3).
Table 2.
Test of Hypothesized Mediators of the Dissonance Intervention Effects.
| Criteria | Fixed Effects | Random Effects | ||||
|---|---|---|---|---|---|---|
| Level-2 | Level-1 | |||||
| B | SE | T-ratio | pr | Between Subjects Variance | Within Subjects Variance | |
| 1. Effect of the treatment on the outcome (path c); γ11 | ||||||
| Dissonance → Δ body dissatisfaction | −0.20 | 0.03 | −6.29 | .38 | 0.03 | 0.12 |
| Dissonance → Δ dieting | −0.14 | 0.03 | −4.71 | .29 | 0.03 | 0.14 |
| Dissonance → Δ negative affect | −0.14 | 0.02 | −4.51 | .28 | 0.03 | 0.13 |
| Dissonance → Δ bulimic symptoms | −2.04 | 0.46 | −4.41 | .28 | 8.55 | 20.96 |
| 2. Effect of the treatment on the mediator (path a); γ11 | ||||||
| Dissonance → Δ thin ideal internalization | −0.12 | 0.02 | −5.16 | .32 | 0.02 | 0.08 |
| 3. Relation between change in mediator and outcome (path b); γ11 | ||||||
| Δ thin ideal internalization → Δ body dissatisfaction | 0.69 | 0.21 | 3.24 | .32 | 0.03 | 0.17 |
| Δ thin ideal internalization → Δ dieting | 0.88 | 0.19 | 4.80 | .41 | 0.02 | 0.14 |
| Δ thin ideal internalization → Δ negative affect | 0.34 | 0.20 | 1.68 | .16 | 0.03 | 0.14 |
| Δ thin ideal internalization → Δ bulimic symptoms | 7.04 | 3.52 | 2.00 | .20 | 12.14 | 23.66 |
| 4a. Effect of treatment on outcome controlling for change in mediator (path c′); γ11 | ||||||
| Dissonance → Δ body dissatisfaction | thin ideal internalization | −0.16 | 0.04 | −4.51 | 0.28 | 0.04 | 0.15 |
| Dissonance → Δ dieting | thin ideal internalization | −0.08 | 0.04 | −2.15 | 0.14 | 0.03 | 0.12 |
| Dissonance → Δ negative affect | thin ideal internalization | −0.08 | 0.03 | −2.25 | 0.15 | 0.03 | 0.13 |
| Dissonance → Δ bulimic symptoms | thin ideal internalization | −1.41 | 0.50 | −2.81 | 0.18 | 8.30 | 20.95 |
| T-ratio | Δ pr | |||||
| 4b. Effect of treatment on outcome, controlling for change in mediator (path c′) significantly reduced or eliminated compared to effect of the treatment on the outcome (path c) | ||||||
| Dissonance → Δ body dissatisfaction | Δ thin ideal internalization | −3.69 | 26% | ||||
| Dissonance → Δ dieting | Δ thin ideal internalization | −5.10 | 48% | ||||
| Dissonance → Δ negative affect | Δ thin ideal internalization | −6.72 | 46% | ||||
| Dissonance → Δ bulimic symptoms | Δ thin ideal internalization | −5.16 | 36% | ||||
| 5. Percent Showing .5 SD decrease in mediator before .5 SD in outcome | % Showing | p-value | ||||
| Decrease in thin ideal internalization before decrease in body dissatisfaction | 70 | <.001 | ||||
| Decrease in thin ideal internalization before decrease in dieting | 74 | <.001 | ||||
| Decrease in thin ideal internalization before decrease in negative affect | 74 | <.001 | ||||
| Decrease in thin ideal internalization before decrease in bulimic symptoms | 61 | .019 | ||||
Notes. B = beta coefficient; SE = standard error; pr = partial correlation coefficient; Δ = change; | = controlling for. T-ratio < 1.96 indicates statistical significance at p <.05.
Table 3.
Test of Hypothesized Mediators of the Healthy Weight Intervention Effects.
| Criteria | Fixed Effect | Random Effects | ||||
|---|---|---|---|---|---|---|
| Level-2 | Level-1 | |||||
| B | SE | T-ratio | pr | Between Subjects Variance | Within Subjects Variance | |
| 1. Effect of the treatment on the outcome (path c); γ11 | ||||||
| Healthy weight → Δ body dissatisfaction | −0.12 | 0.03 | −4.04 | .25 | 0.03 | 0.13 |
| Healthy weight → Δ negative affect | −0.08 | 0.02 | −2.46 | .16 | 0.03 | 0.11 |
| Healthy weight → Δ bulimic symptoms | −1.50 | 0.39 | −3.81 | .24 | 5.59 | 18.53 |
| 2. Effect of the treatment on the mediator (path a); γ11 | ||||||
| Healthy weight → Δ healthy eating | 0.18 | 0.04 | 4.59 | .29 | 0.05 | 0.23 |
| Healthy weight → Δ physical activity | 4.07 | 0.63 | 6.43 | .39 | 13.65 | 51.52 |
| 3. Relation between change in mediator and outcome (path b); γ11 | ||||||
| Δ healthy eating → Δ body dissatisfaction | −0.20 | 0.15 | −1.40 | .13 | 0.03 | 0.13 |
| Δ healthy eating → Δ negative affect | −0.10 | 0.16 | −0.64 | .06 | 0.04 | 0.10 |
| Δ healthy eating → Δ bulimic symptoms | 2.46 | 2.01 | 1.22 | .11 | 6.40 | 18.67 |
| Δ physical activity → Δ body dissatisfaction | −0.02 | 0.01 | −2.64 | .24 | 0.03 | 0.13 |
| Δ physical activity → Δ negative affect | −0.03 | 0.01 | −3.40 | .30 | 0.04 | 0.10 |
| Δ physical activity → Δ bulimic symptoms | −0.50 | 0.10 | −1.98 | .18 | 6.19 | 18.65 |
| 4a. Effect of treatment on outcome controlling for change in mediator (path c′); γ11 | ||||||
| Healthy weight → Δ body dissatisfaction | Δ healthy eating | −0.10 | 0.03 | −2.74 | .18 | 0.03 | 0.13 |
| Healthy weight → Δ body dissatisfaction | Δ physical activity | −0.10 | 0.04 | −2.65 | .17 | 0.03 | 0.13 |
| Healthy weight → Δ negative affect | Δ healthy eating | −0.05 | 0.03 | −1.35 | .09 | 0.03 | 0.11 |
| Healthy weight → Δ negative affect | Δ physical activity | −0.05 | 0.05 | −0.93 | .06 | 0.03 | 0.11 |
| Healthy weight → Δ bulimic symptoms | Δ healthy eating | −1.60 | 0.47 | −3.45 | .22 | 5.62 | 18.53 |
| Healthy weight → Δ bulimic symptoms | Δ physical activity | −1.47 | 0.49 | −2.99 | .19 | 5.63 | 18.54 |
| T-ratio | Δ pr | |||||
| 4b. Effect of treatment on outcome, controlling for change in mediator (path c′) significantly reduced or eliminated compared to effect of the treatment on the outcome (path c) | ||||||
| Healthy weight → Δ body dissatisfaction | Δ healthy eating | −2.37 | 28% | ||||
| Healthy weight → Δ body dissatisfaction | Δ physical activity | −2.00 | 32% | ||||
| Healthy weight → Δ negative affect | Δ healthy eating | −2.74 | 44% | ||||
| Healthy weight → Δ negative affect | Δ physical activity | −1.03 | 63% | ||||
| Healthy weight → Δ bulimic symptoms | Δ healthy eating | 0.77 | 8% | ||||
| Healthy weight → Δ bulimic symptoms | Δ physical activity | −0.17 | 21% | ||||
| 5. Percent Showing .5 SD decrease in mediator before .5 SD in outcome | % Showing | p-value | ||||
| Increase in healthy eating before decrease in body dissatisfaction | 94 | <.001 | ||||
| Increase in physical activity before decrease in body dissatisfaction | 96 | <.001 | ||||
| Increase in healthy eating before decrease in negative affect | 88 | <.001 | ||||
| Increase in physical activity before decrease in negative affect | 94 | <.001 | ||||
| Increase in healthy eating before decrease in negative affect | 93 | <.001 | ||||
| Increase in physical activity before decrease in negative affect | 93 | <.001 | ||||
Notes. B = beta coefficient; SE = standard error; pr = partial correlation coefficient; Δ = change. T-ratio < 1.96 indicates statistical significance at p <.05.
Criterion 2
To test whether condition predicted future change in mediators (path a), HLM models tested whether treatment condition predicted the slope parameter for each mediator controlling for the intercept of the respective mediator. Condition-by-time effects confirmed that dissonance participants showed significantly greater decreases in thin-ideal internalization than expressive writing controls (Table 2) and that healthy weight participants showed significantly greater increases in healthy eating and physical activity than expressive writing controls (Table 3).
Criterion 3
To test whether change in the mediator correlates with change in the outcome in the intervention condition (path b), HLM models tested whether the slope of the mediator correlated with the slope of the outcome controlling for the intercept of the outcome. Change in thin-ideal internalization correlated significantly with change in body dissatisfaction, dieting, and bulimic symptoms, but not negative affect, for the dissonance intervention (Table 2). Separate models tested whether change in healthy eating and physical activity in the healthy weight intervention correlated with change in the outcomes because change in the mediators for an intervention will be artificially correlated because they share a common cause– the intervention, which would attenuate the unique effects for the relations between change in each mediator and change in the outcome if mediators were included simultaneously. Change in physical activity correlated significantly with change in body dissatisfaction, negative affect, and bulimic symptoms, but change in healthy eating did not correlate with change in these outcomes (Table 3).
Criterion 4
To assess whether the predictive effects of condition on change in the outcome (path c) is significantly reduced when change in the mediator is statistically partialed (path c′) we tested the null hypothesis c–c′ is equal to zero. The estimate of c–c′ is divided by a standard error developed by Freedman and Schatzkin (1992) and compared to a t distribution to test for significance. The significant effects of the dissonance intervention on body dissatisfaction, dieting, negative affect, and bulimic symptoms were significantly reduced when change in the mediator was statistically controlled. These effects represent partial mediation because the main effect the dissonance intervention on the outcomes (c′) remained significant and the percent reduction in the main effect ranged from 26% to 48% (Table 2). The results for the healthy weight intervention were mixed. The first three out of the six t-ratios for the c–c′ test indicated that the effect of the healthy weight intervention was significantly reduced when the effects of change in these mediators were statistically controlled (Table 3). The percent reduction in these partial correlation coefficients ranged from 28% to 44%. The effect of healthy weight intervention on change in negative affect became non-significant when the effect of change in healthy eating was partialed, but the effects of condition on change in body dissatisfaction controlling for the effects of change in healthy eating and change in physical activity remained significant. These effects appear to represent partial mediation because the main effect of condition in these models was not reduced to zero. The group-by-mediator interaction from the models testing criterion 4 were non-significant in seven of the ten models. The interaction term was significant in three models and indicated that change in thin-ideal internalization only predicted change in dieting, negative affect, and bulimic symptoms in the dissonance condition. Kraemer et al. (2002) noted that these types of interactions might occur if the intervention changes the nature of the relation between the mediator and outcome, which is compatible with the concept of mediation.
Criterion 5
Our fifth criterion for mediation specifies that meaningful reductions in the mediator occur before meaningful reductions in the outcome more frequently than expected based on chance. Results indicated that among the 111 participants in the dissonance condition that showed a .5 SD decrease in body dissatisfaction, 70% showed a .5 SD reduction in thin-ideal internalization before they showed a .5 SD reduction in body dissatisfaction (Table 2). Among the 113 dissonance participants who showed a .5 SD decrease in dieting, 74% showed a .5 SD reduction in thin-ideal internalization before they showed the .5 SD reduction in dieting. Among the 113 dissonance participants who showed a .5 SD decrease in negative affect, 74% showed a .5 SD reduction in thin-ideal internalization before they showed the .5 SD reduction in negative affect. Among the 113 dissonance participants who showed a .5 SD decrease in bulimic symptoms, 61% showed a .5 SD reduction in thin-ideal internalization before they showed the .5 SD reduction in bulimic symptoms. All four of these proportions were significantly greater than the .50 proportion that would be expected based on chance (Table 2).
Among the 107 healthy weight participants who showed a .5 SD decrease in body dissatisfaction, 94% showed a .5 SD increase in healthy eating before they showed the .5 SD reduction in body dissatisfaction (Table 3). Among the 107 healthy weight participants who showed a .5 SD decrease in body dissatisfaction, 96% showed a .5 SD increase in physical activity before they showed the .5 SD reduction in body dissatisfaction. Among the 107 healthy weight participants who showed a .5 SD decrease in negative affect, 88% showed a .5 SD increase in healthy eating before they showed the .5 SD reduction in negative affect. Among the 109 healthy weight participants who showed a .5 SD decrease in negative affect, 94% showed a .5 SD increase in physical activity before they showed the .5 SD reduction in negative affect. Among the 117 healthy weight participants who showed a .5 SD decrease in bulimic symptoms, 93% showed a .5 SD increase in healthy eating before they showed the .5 SD reduction in bulimic symptoms. Finally, among the 117 healthy weight participants who showed a .5 SD decrease in bulimic symptoms, 93% showed a .5 SD increase in physical activity before they showed the .5 SD reduction in bulimic symptoms. All six of these proportions were significantly greater than the .50 proportion that would be expected based on chance (Table 3).
Specificity of Mediators
Because we evaluated two distinct prevention programs, we tested for specificity of the variables that putatively mediate the effects of each intervention. The dissonance intervention significantly increased healthy eating (B = −.09, SE = .04, p = .014, pr = −.16), but this effect was significantly weaker than the effect of the healthy weight intervention on this outcome (p < .05). The dissonance intervention did not have a significant impact on change in physical activity (B = .74, SE = .61, p = .229, pr = .08): this effect was significantly weaker than the effect of the healthy weight intervention on this outcome (p < .05). The healthy weight intervention did not have a significant effect on change in thin-ideal internalization (B = −.04, SE = .02, p = .077, pr = −.11): this effect was significantly weaker than the effect of the dissonance intervention on this outcome (p < .05).
Discussion
Test of Hypothesized Mediators of Dissonance Intervention
Results provided reasonable support for the hypothesis that the dissonance intervention partially affects the outcomes by reducing thin-ideal internalization. This intervention produced significant reductions in all outcomes (body dissatisfaction, dieting, negative affect, and bulimic symptoms) and the mediator (thin-ideal internalization), change in the mediator correlated with change in most outcomes and typically occurred before change in outcomes, and intervention effects became significantly weaker when change in the mediators was statistically partialed. Most of the effects corresponded to medium to large effect sizes. These results are largely consistent with the dual pathway model of bulimic pathology (Stice, 2001), which posits that thin-ideal internalization occurs early in the causal chain of risk factors in the prediction of bulimic symptoms. Theoretically, the act of voluntarily taking a stance against the thin-ideal results in cognitive dissonance that motivated participants to reduce their subscription to this ideal, which results in a consequent reduction in body dissatisfaction, dieting, negative affect, and bulimic symptoms. In support of the notion that dissonance is responsible for the change in thin-ideal internalization, Green, Scott, Divankova, Gasser, and Pederson (2005) found that participants assigned to a high dissonance induction version of this intervention showed greater reductions in these outcomes than did participants assigned to a low dissonance version of the same intervention.
There were two aspects of the findings, however, that provided limited support for hypotheses. First, the effect of the dissonance intervention on the outcomes (c′) was still significant after controlling for change in the mediator and the mediated effects only accounted for a 26% to 48% reduction in the main effects, suggesting that change in thin-ideal internalization only partially mediated the intervention effects. It is possible that the thin-ideal internalization scale that we used was not sufficiently sensitive to reliably model change in this mediator. Other measures that provide a broader assessment of the construct of internalization, such as the Sociocultural Attitudes Towards Appearance Questionnaire (Heinberg, Thompson, & Stormer, 1995) might have provided stronger support for our hypotheses. It is also possible that other factors partially mediated the intervention effects. For example, the intervention may have directly reduced body dissatisfaction, which had a subsequent effect on the downstream variables.3 Finally, non-specific factors, such as social support from group members, may partially mediate the intervention effects.
A second aspect of the findings that provided only partial support for hypotheses was that 26% to 39% of the participants did not show the expected sequencing of effects, in that they showed reductions in the outcome before they showed reductions in the mediator. It is possible that using slopes to model the time it takes for individuals to show meaningful change provides only a rough estimate of the timing of change. If the changes in the mediator and outcome occurred at about the same time, the change parameters based on weekly assessments may not have been sufficiently sensitive to determine the temporal ordering of change. It is also possible that there are bidirectional effects between the mediator and the outcomes, wherein reductions in the outcomes (e.g., bulimic symptoms) also contribute to subsequent reductions in the mediator (thin-ideal internalization). Another possibility is that a subset of participants may first show reductions on the outcomes, which then result in reductions in the mediator– an interpretation that is consistent with moderated mediation. It would be useful if future studies explored these possibilities.
Test of Hypothesized Mediators of Healthy Weight Intervention
The mediation analyses provided somewhat mixed support for the hypothesis that the healthy weight intervention affects the outcomes by increasing healthy eating and exercise behaviors. On the one hand, results provided consistent evidence that the healthy weight intervention produced significant reductions in all outcomes (body dissatisfaction, negative affect, and bulimic symptoms) and both mediators (healthy eating and physical activity), and that change in mediators almost always occurred before change in outcomes. These effects were small to medium effect sizes. On the other hand, change in the mediators was only correlated with change in the outcome in three of the six tests and the main effects of the intervention on change in the outcomes were significantly reduced when change in the mediator was controlled statistically in only three out of the six tests. This pattern of findings implies that changes in these mediators were inconsistently coupled with changes in the outcomes, despite the fact that the changes appear to typically occur in the hypothesized sequence. These results may suggest that the apparent change in the mediators are a product of demand characteristics, rather than the intervention, which may explain why change in these measures do not track with change in the outcome. There is considerable evidence that self-reports of dietary intake and physical activity are biased (e.g., Bandini, Schoeller, Cyr, & Dietz, 1990). It is also possible that changes in internalization of the healthy ideal, resulting from the motivational enhancement component of the intervention, was the key factor that explained the reductions in body dissatisfaction, negative affect, and bulimic symptoms. Alternatively, change in body dissatisfaction may have mediated the effects of the healthy weight intervention on the downstream outcomes.
Specificity of Mediators
It is encouraging that the mediators of the two interventions showed evidence of specificity. The healthy weight intervention did not produce significant reductions in thin-ideal internalization and the dissonance intervention did not produce significant increases in physical activity. Although the dissonance intervention did appear to produce small improvements in healthy eating, the effect was significantly weaker than the effects in this mediator produced by the healthy weight intervention. These findings suggest that the mediators were reasonably specific to the two interventions, which increases the confidence that can be placed in the hypotheses regarding the factors that mediate the effects of these interventions. Whereas both interventions produce significant reductions in the outcomes, they appear to do so via different mechanisms. By understanding the processes through which intervention effects occur, we may be better able to maximize these effects and ensure that the critical features of the intervention are generalized to clinical practice. Additionally, understanding how these interventions work can also help identify potential moderators that may impact their effectiveness.
New Approach to Testing Mediation in Randomized Trials
The secondary aim of the present study was to propose a more rigorous test of mediation for randomized trials, which includes direct tests of temporal precedence and temporal sequencing. Although it is possible that there may be more reliable or sensitive methods for modeling change and the timing of change, this approach seems to represent an improvement over previous approaches to testing mediation in randomized trials. We hope that future researchers will devise ways to improve upon this general approach because a more complete understanding of the mechanisms that account for intervention effects may aid in the design of more effective preventive and treatment interventions. It would be particularly useful to consider alternative ways of defining meaningful change in the mediators and outcomes.
It is important to consider the assumptions of this new approach. First, it assumes linear growth. If there were evidence of significant nonlinear growth, such as a quadratic trend indicating that intervention effects reach a maximum and then begin to erode, it would not be appropriate to use the present approach because the linear slope would not accurately describe the change over time. This implies that it may be difficult to apply this approach to change in the mediators and outcomes that occur after intervention termination because effects tend to erode over follow-up. A second assumption is that the mediators and outcomes are assessed with sufficient frequency to model the timing of change accurately (e.g., with weekly assessments during the intervention). A third assumption is that a common intercept can be used for all treatment conditions for each mediator and outcome. Although random assignment should result in similar pretest values on all variables, randomization can fail, particularly in small samples. Condition-specific intercepts should be used if there is evidence that randomization did not produce groups that are initially equivalent. A fourth assumption is that no variables are confounded with treatment condition. If randomization does not produce groups that are equivalent on a certain variable at pretest, it would be necessary to statistically control for this variable when generating slope and intercept coefficients for moderators and outcomes. A fifth assumption is that there is adequate statistical power to detect effects in all five steps for testing mediation. It is important to ensure that adequate numbers of participants will show meaningful change in the mediators and outcomes so that the temporal sequencing of this change can be tested. This is vital because the binomial test has limited sensitivity. It may be necessary to select a different definition of meaningful change, rather than the .5 SD cut point used in this report, to ensure that a sufficient portion of participants will show meaningful change during the observation period. As long as the same cut point is applied to the mediators and outcomes, this should still yield objective evidence of the most common temporal sequencing of change in these variables. These various cut points should be specified a priori.
We think it is important to propose a more rigorous approach to testing factors that mediate the effects of an intervention in randomized trials because it is not possible to experimentally manipulate the mediators to examine this question. Although experiments provide the most rigorous test of causal relations, they cannot provide a test of whether an intervention produced the changes on the outcome by changing the mediator, as change in the mediator would be a function of the latter manipulation, rather than the intervention. Still, we think there is great value in testing whether direct manipulations of the putative mediators produce the expected effects on the outcomes because it would provide an inferentially rigorous complement to the original trial.
Limitations
There were several limitations of the present study. First, the reliance on self-report data may have biased the magnitude of the relations. Second, there was limited data on the reliability and validity of the healthy eating and physical activity measures. Third, our design does not permit us to definitively rule out the possibility of bidirectional effects between change in the mediators and change in the outcomes. Finally, we did not assess non-specific factors that may partially account for intervention effects, which is a limitation that should be addressed in future trials.
Conclusions and Implications for Future Research
The present findings provided reasonable support for the hypothesis that changes in thin-ideal internalization mediate the effects of the dissonance intervention on the outcomes, but provided mixed support for the hypothesis that changes in healthy eating and physical activity mediate the effects of the healthy weight intervention on the outcomes. Moreover, the findings suggest that our proposed method of evaluating mediation that includes a test of temporal sequencing of effects is potentially useful in testing mediation effects from randomized trials and may represent a more rigorous test than prior approaches.
With regard to research implications, findings suggest that it will be important for future prevention trials to investigate the mediators that account for intervention effects, particularly non-specific factors. This information would be useful in determining which intervention components contribute most strongly to improvements in outcome and would aid in intervention refinement. A second direction for future research will be to investigate moderators of prevention program effects because it may provide additional guidance for determining which individuals would benefit most from each intervention. The evidence from the present study that some individuals may have shown decreases on the outcomes before showing decreases on the mediators implies that it might be fruitful to test whether there are qualitatively distinct subgroups for whom there are different mediators that account for intervention effects. To the best of our knowledge, prior eating disorder prevention programs have not tested for moderated mediation. Finally, future research should attempt to refine the approach to testing mediation within randomized trials because elucidating the mechanisms responsible for change may result in further improvements to eating disorder prevention programs. It would be particularly useful to extend the recommended approach so that it could directly test for bidirectional effects between change in the mediator and change in the outcome.
Acknowledgments
This study was supported by a research grants (MH/DK6195 and MH70699) and a National Research Service Award (MH64254) from the National Institutes of Health.
We thank project managers Erin Martinez and Emily Wade, project research assistants Cassie Goodin, and Natalie McKee, our undergraduate volunteers, the Austin Independent School District, and the participants who made this study possible.
Appendix PARTICIPANT FLOW
Footnotes
The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/ccp.
We did not hypothesize that dieting would mediate the effects of the healthy weight intervention because the dieting measure that we used assessed transient, rather than lasting, changes in dietary intake. We therefore decided to create a scale assessing lasting healthy changes to dietary intake for this trial (see Measures section).
We considered using the time it took to show reliable change in the mediator and outcomes using the reliable change index (Jacobson & Truax, 1991), but this approach produced average times to the occurrence of this degree of change that regularly fell outside of the pre to post interval in the present prevention trial. This was problematic because we were functionally extrapolating beyond the pre to post assessment period in which our weekly measures were conducted, which decreased our confidence in the timing variables. The reliable change index may provide a better index of meaningful change in treatment trials, given that individuals with psychiatric disorders typically show greater improvements on the outcomes relative to participants from prevention trials.
On a post hoc basis, we tested whether the effects of the dissonance intervention on change in dieting, negative affect, and bulimic symptoms were mediated by change in body dissatisfaction. Although the first 4 criteria were supported for these effects, there was less support for criterion 5. Specifically, meaningful change in body dissatisfaction occurred before meaningful change in negative affect for 65% of the participants in this condition, which was significantly greater than chance (p = .003). However, meaningful change in body dissatisfaction did not occur before meaningful change in dieting or bulimic symptoms more frequently than chance (56%, p = .310 and 50%, p = 1.00 respectively). We also tested whether the effects of the healthy weight intervention on change in negative affect and bulimic symptoms were mediated by change in body dissatisfaction. Although the first 4 criteria were supported, criterion 5 was not supported: meaningful change in body dissatisfaction did not occur before meaningful change in negative affect or bulimic symptoms more frequently than chance (52%, p = .824 and 57%, p = .172 respectively). Thus, there was limited support for the possibility that change in body dissatisfaction mediated the effects of the interventions on these outcomes.
References
- American Psychological Association (APA) Task Force on Psychological Intervention Guidelines. Template for developing guidelines: Interventions for mental disorders and psychological aspects of physical disorders. Washington, DC: APA; 1995 . [Google Scholar]
- Bandini LG, Schoeller DA, Cyr HN, Dietz WH. Validity of reported energy intake in obese and nonobese adolescents. American Journal of Clinical Nutrition. 1990;52:421–425. doi: 10.1093/ajcn/52.3.421. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bearman SK, Stice E, Chase A. Effects of body dissatisfaction on depressive and bulimic symptoms: A longitudinal experiment. Behavior Therapy. 2003;34:277–293. doi: 10.1016/S0005-7894(03)80001-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker CB, Smith L, Ciao AC. Reducing eating disorder risk factors in sorority members: A randomized trial. Behavior Therapy. 2005;36:245–254. [Google Scholar]
- Berscheid E, Walster E, Bohrnstedt G. The happy American body: A survey report. Psychology Today. 1973;7:119–131. [Google Scholar]
- Bryk AS, Raudenbush SW, Congdon RT. HLM 6: Hierarchical linear and nonlinear modeling. Chicago: Scientific Software, Inc; 2004. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Coie J, Watt N, West S, Hawkins D, Asarnow J, Markman H, Ramey S, Shore M, Long B. The science of prevention: A conceptual framework and some directions for a national research program. American Psychologist. 1993;48:1013–1022. doi: 10.1037//0003-066x.48.10.1013. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The eating disorder examination. In: Fairburn C, Wilson G, editors. Binge eating: Nature, assessment, and treatment. 12. NY: Guilford; pp. 317–360. [Google Scholar]
- Freedman LS, Schatzkin A. Sample size for studying intermediate endpoints within intervention trials of observational studies. American Journal of Epidemiology. 1992;136:1148–1159. doi: 10.1093/oxfordjournals.aje.a116581. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Reivich K, Jaycox L, Seligman ME. Prevention of depressive symptoms in schoolchildren: Two-year follow-up. Psychological Science. 1995;6:343–351. [Google Scholar]
- Grant KA, Tonigan JS, Miller WR. Comparison of three alcohol consumption measures: A concurrent validity study. Journal of Studies on Alcohol. 1995;56:168–172. doi: 10.15288/jsa.1995.56.168. [DOI] [PubMed] [Google Scholar]
- Green M, Scott N, Diyankova I, Gasser C, Pederson E. Eating disorder prevention: An experimental comparison of high level dissonance, low level dissonance, and no-treatment control. Eating Disorders. 2005;13:157–170. doi: 10.1080/10640260590918955. [DOI] [PubMed] [Google Scholar]
- Heinberg LJ, Thompson JK, Stormer S. Development and validation of the sociocultural attitudes towards appearance questionnaire. International Journal of Eating Disorders. 1995;17:81–89. doi: 10.1002/1098-108x(199501)17:1<81::aid-eat2260170111>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP. Intervention research, theoretical mechanisms, and causal processes related to externalizing behavior patterns. Development and Psychopathology. 2002;14:789–818. doi: 10.1017/s0954579402004078. [DOI] [PubMed] [Google Scholar]
- Jacobson N, Truax P. Clinical significance: A statistical approach to defining change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Brook JS. Eating disorders during adolescence and the risk for physical and mental disorders during early adulthood. Archives of General Psychiatry. 2002;59:545–552. doi: 10.1001/archpsyc.59.6.545. [DOI] [PubMed] [Google Scholar]
- Jones DC. Body image among adolescent girls and boys: A longitudinal study. Developmental Psychology. 2004;40:823–835. doi: 10.1037/0012-1649.40.5.823. [DOI] [PubMed] [Google Scholar]
- Kaufman NK, Rohde P, Seeley JR, Clarke GN, Stice E. Mediators of cognitive behavioral treatment for adolescents with comorbid major depression and conduct disorders. Journal of Consulting and Clinical Psychology. 2005;73:38–46. doi: 10.1037/0022-006X.73.1.38. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Klem ML, Wing RR, Simkin-Silverman L, Kuller LH. The psychological consequences of weight gain prevention in healthy, premenopausal women. International Journal of Eating Disorders. 1997;21:167–174. doi: 10.1002/(sici)1098-108x(199703)21:2<167::aid-eat7>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Kupfer D. How do risk factors work? Mediators, moderators, independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Striegel-Moore RH, Seeley JR. Epidemiology and natural course of eating disorders in young women from adolescence to young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1284–92. doi: 10.1097/00004583-200010000-00016. [DOI] [PubMed] [Google Scholar]
- Matusek JA, Wendt SJ, Wiseman CV. Dissonance thin-ideal and didactic healthy behavior eating disorder prevention programs: Results from a controlled trial. International Journal of Eating Disorders. 2004;36:376–388. doi: 10.1002/eat.20059. [DOI] [PubMed] [Google Scholar]
- Moscovitch DA, Hofmann SG, Suvak MK, In-Albon T. Mediation of changes in anxiety and depression during treatment of social phobia. Journal of Consulting and Clinical Psychology. 2005;73:945–952. doi: 10.1037/0022-006X.73.5.945. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW. Writing about emotional experiences as a therapeutic process. Psychological Science. 1997;8:162–166. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Stice E, Cameron R, Killen JD, Hayward C, Taylor CB. Naturalistic weight reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. Journal of Consulting and Clinical Psychology. 1999;67:967–974. doi: 10.1037//0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- Stice E, Chase A, Stormer S, Appel A. A randomized trial of a dissonance-based eating disorder prevention program. International Journal of Eating Disorders. 2001;29:247–262. doi: 10.1002/eat.1016. [DOI] [PubMed] [Google Scholar]
- Stice E, Fisher M, Martinez E. Eating disorder diagnostic scale: Additional evidence of reliability and validity. Psychological Assessment. 2004;16:60–71. doi: 10.1037/1040-3590.16.1.60. [DOI] [PubMed] [Google Scholar]
- Stice E, Mazotti L, Weibel D, Agras WS. Dissonance prevention program decreases thin-ideal internalization, body dissatisfaction, dieting, negative affect, and bulimic symptoms: A preliminary experiment. International Journal of Eating Disorders. 2000;27:206–217. doi: 10.1002/(sici)1098-108x(200003)27:2<206::aid-eat9>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Stice E, Shaw H. Eating disorder prevention programs: A meta-analytic review. Psychological Bulletin. 2004;130:206–227. doi: 10.1037/0033-2909.130.2.206. [DOI] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Telch CF, Rizvi SL. Development and validation of the Eating Disorder Diagnostic Scale: A brief self-report measure for anorexia, bulimia, and binge eating disorder. Psychological Assessment. 2000;12:123–131. doi: 10.1037//1040-3590.12.2.123. [DOI] [PubMed] [Google Scholar]
- Stice E, Trost A, Chase A. Healthy weight control and dissonance-based eating disorder prevention programs: Results from a controlled trial. International Journal of Eating Disorders. 2003;33:10–21. doi: 10.1002/eat.10109. [DOI] [PubMed] [Google Scholar]
- van Strien T, Frijters JE, Van Staveren WA, Defares PB, Deurenberg P. The predictive validity of the Dutch Restrained Eating Scale. International Journal of Eating Disorders. 1986;5:747–755. [Google Scholar]
- Watson D, Clark LA. Affects separable and inseparable: On the hierarchical arrangement of the negative affects. Journal of Personality and Social Psychology. 1992;62:489–505. [Google Scholar]