Abstract
Objective To assess the effect of general practitioner testing for C reactive protein (disease approach) and receiving training in enhanced communication skills (illness approach) on antibiotic prescribing for lower respiratory tract infection.
Design Pragmatic, 2×2 factorial, cluster randomised controlled trial.
Setting 20 general practices in the Netherlands.
Participants 40 general practitioners from 20 practices recruited 431 patients with lower respiratory tract infection.
Main outcome measures The primary outcome was antibiotic prescribing at the index consultation. Secondary outcomes were antibiotic prescribing during 28 days’ follow-up, reconsultation, clinical recovery, and patients’ satisfaction and enablement.
Interventions General practitioners’ use of C reactive protein point of care testing and training in enhanced communication skills separately and combined, and usual care.
Results General practitioners in the C reactive protein test group prescribed antibiotics to 31% of patients compared with 53% in the no test group (P=0.02). General practitioners trained in enhanced communication skills prescribed antibiotics to 27% of patients compared with 54% in the no training group (P<0.01). Both interventions showed a statistically significant effect on antibiotic prescribing at any point during the 28 days’ follow-up. Clinicians in the combined intervention group prescribed antibiotics to 23% of patients (interaction term was non-significant). Patients’ recovery and satisfaction were similar in all study groups.
Conclusion Both general practitioners’ use of point of care testing for C reactive protein and training in enhanced communication skills significantly reduced antibiotic prescribing for lower respiratory tract infection without compromising patients’ recovery and satisfaction with care. A combination of the illness and disease focused approaches may be necessary to achieve the greatest reduction in antibiotic prescribing for this common condition in primary care.
Trial registration Current Controlled Trials ISRCTN85154857.
Introduction
Contrasting broad approaches to improved management in general medicine have been emphasised.1 A disease focused approach seeks to improve diagnosis, whereas the illness focused, patient centred approach emphasises understanding the whole patient and sharing decisions, which may be more contingent on clear information about prognosis rather than making an accurate diagnosis.2 3 A combination of these approaches, however, may be required to achieve the best outcome for patients. We evaluated the effect of two interventions on achieving evidence based management of lower respiratory tract infections in primary care.
Lower respiratory tract infection is one of the commonest acute reasons to consult, accounting for 17 million consultations in the European Union and 11 million in the United States each year.4 5 6 Acute bronchitis accounts for 80% of lower respiratory tract infections6 7 and despite evidence of little or no benefit from antibiotics, up to 80% of patients consulting for this condition are prescribed them.8 9 10 Moreover, lower respiratory tract infection is associated with increasing use of broad spectrum antibiotics.8 11 Everyday decisions about whether or what antibiotic to prescribe for lower respiratory tract infection therefore constitute an important part of the burden of antibiotic use that drives antimicrobial resistance.9 12 13
Diagnostic or disease focused solutions address the limited value of medical history and physical examination in differentiating between pneumonia and self limiting acute bronchitis.14 15 16 Diagnostic uncertainty increases the chances of inappropriate antibiotic prescribing,17 and general practitioners often prescribe to give patients “the benefit of the doubt” in the face of possible pneumonia and possible clinical benefit18 especially since routinely requesting chest radiography for all patients with lower respiratory tract infection is neither feasible nor appropriate in most primary care settings. C reactive protein is a promising biomarker for improving the assessment of lower respiratory tract infection in primary care: it performs better in predicting the diagnosis of pneumonia than any individual or combination of clinical symptoms and signs in lower respiratory tract infection. Furthermore, it is feasible and robust as a point of care test, making it the best available biomarker to enhance the diagnosis of lower respiratory tract infection in primary care.15 16 19 20 However, there is no evidence from pragmatic trials that testing for C reactive protein safely reduces antibiotic prescribing for lower respiratory tract infection in primary care.
Illness focused solutions, including enhanced clinician-patient communication, recognise the importance of non-medical influences on the decision to prescribe antibiotics for lower respiratory tract infection, and emphasise eliciting and responding to patients’ feelings, ideas, fears, and expectations about their illness experience.3 General practitioners are often unable to satisfactorily deal with these influences to achieve evidence based prescribing decisions in time pressured consultations.21 22 23 24 25 The resulting inappropriate prescribing of antibiotics reinforces misconceptions that impact on future help seeking and expectations for antibiotics.26 27 28 Shared decision making, building on a patient centred approach to understand better patients’ perspectives and achieve enhanced clinician-patient communication, may be useful in achieving evidence based decisions on prescribing, particularly in the face of diagnostic certainty.3 Exploring the illness experience and finding common ground are particular tasks of the patient centred consultation that may be relevant to illness focused solutions to over-prescribing of antibiotics.29 Training clinicians to elicit patients’ concerns about their illness and asking their views on antibiotics increased patients’ participation in consultations.30 However, no pragmatic clinical trial has evaluated this shared decision making approach for lower respiratory tract infections in primary care.
Interventions to enhance the quality of decisions on antibiotic prescribing for lower respiratory tract infection have generally focused on either reducing diagnostic uncertainty (disease perspective)31 32 33 or on educational, often multifaceted, interventions tackling non-medical influences (illness perspective).33 34 35 36 37 38
We evaluated the effect of general practitioners using a point of care test for C reactive protein and being trained in enhanced communication skills, separately and combined, on antibiotic prescribing for lower respiratory tract infection and on patient recovery. We hypothesised that either intervention alone would be more effective than their controls and that the combined intervention would show a combined positive effect on reducing antibiotic prescribing for lower respiratory tract infection in primary care.
Methods
This study was a pragmatic, cluster randomised, factorial, controlled trial. While recognising certain limitations,39 we chose a cluster randomisation design to optimise the pragmatic nature of the study and to minimise contamination: once general practitioners within a practice had been trained in new communication skills they could not switch at random between using these skills and usual consulting practice. A 2×2 factorial design was used to assess the effect of each intervention and to explore the effect of the interventions combined.40 Such trials require a prespecified factorial analysis plan with assessments for treatment interactions. We selected this design because we planned to test two treatment hypotheses. The four allocated groups were general practitioners’ use of C reactive protein testing (1), training in enhanced communication skills (2), the interventions combined (3), and usual care (4). The groups were combined for analysis as follows: factor A, C reactive protein test (cells 1 and 3) compared with no test (2 and 4) (controlling for the effect of general practitioners’ training in enhanced communication skills in the model); and factor B, training in enhanced communication skills (2 and 3) compared with no training (1 and 4) (controlling for the effects of C reactive protein testing in the model).
Outcomes, sample size, and randomisation
The primary outcome was antibiotic prescribing in the index consultation. Our study required 400 patients with lower respiratory tract infection to detect a reduction in antibiotic prescribing from 80% to 60% (power 80%, α 0.05, follow-up 90%) when adjusted for clustering at practice level (intracluster coefficient 0.06). The sample size was for the main effects only and assumed no interaction between the two interventions. Secondary outcomes were antibiotic prescribing during 28 days’ follow-up, reconsultation, clinical recovery, and patients’ satisfaction and enablement. Cost effectiveness will be reported separately. We planned to recruit 20 general practices with two participating general practitioners per practice within a large suburban region of the Netherlands. All practices and general practitioners were recruited and provided written consent before randomisation.
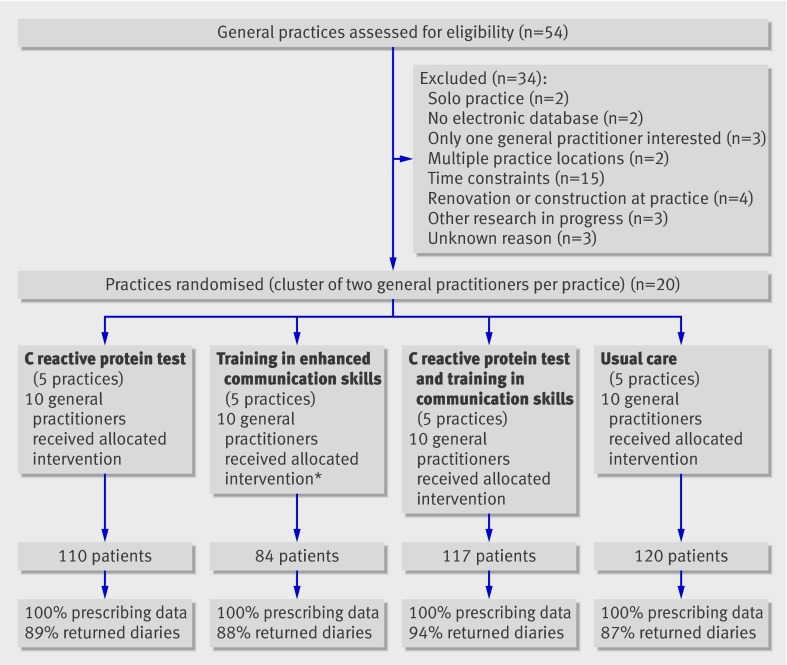
Practices were randomised into two groups of 10 practices per intervention, balanced for recruitment potential, resulting in four trial arms (fig 1). The balancing factor used for randomisation was the amount of general practitioners’ consultation time (expressed as full time equivalent) that the practice was contributing to the study, and this equated to between one and two full time equivalents for clinical contact time. The randomisation was balanced for those with 1.5 or less full time equivalents and those with more than 1.5 full time equivalents. The Dutch guideline for managing acute cough, including diagnostic and therapeutic advice for lower respiratory tract infection, is distributed to all general practitioners in the Netherlands and informs usual care.41
Fig 1 Trial profile. *Three general practitioners went on maternity leave halfway through study. It was not feasible for general practitioners to keep a log of those eligible patients not approached or those approached who declined and the reasons for declining
Interventions
The interventions and study methods are described in detail elsewhere.39 Both interventions were targeted at the level of the general practitioner. The clinicians were given devices to test for C reactive protein (NycoCard II Reader; Axis-Shield, Norway), according to the manufacturer’s instructions. A result can be available within three minutes, using a drop of blood obtained by finger prick. The validity and robustness of this test is established in primary care.20 General practitioners were given guidance on how to use the test results within the consultation during a 30 minute practice based training session delivered by the study team. The additional value of C reactive protein in ruling out serious infection was emphasised.39 An eight week run-in period enabled familiarisation with the devices before patient recruitment to the trial began.
The communication skills intervention was built around 11 key tasks (for example, exploring patients’ fears and expectations, asking patients’ opinion on antibiotics, and outlining the natural duration of cough in lower respiratory tract infection), with information exchange throughout based on the elicit-provide-elicit framework from counselling in behaviour change.42 Key features of the training programme were the brevity of workshop based training, its context rich nature, and the innovative use of peer reviewing colleagues’ transcripts of the consultations with simulated patients. A full description of the components of the training and demonstration of general practitioners’ sustained competence in implementing the acquired skills in daily practice after training has been reported.43
Procedures
General practitioners were asked to recruit sequential eligible adults within regular consultation hours during the winters of 2005-6 and 2006-7. Patients were eligible if they had a suspected lower respiratory tract infection with a cough lasting less than four weeks together with one focal and one systemic symptom.39 Patients provided written informed consent after the study had been explained by their general practitioner, and written information was provided. Apart from the point of care C reactive protein tests the general practitioners decided on investigations and treatment according to their usual practice. Patients rated symptoms (cough, phlegm, shortness of breath, disturbance of daily activities, sleeping problems, and generally feeling unwell) on a 7 point scale in a daily diary for 28 days. This diary was validated for use in a randomised controlled trial on management of lower respiratory tract infection in primary care.44 The diary also included a Likert scale question on satisfaction, and the patient enablement index.45 On days 4, 14, and 28 the participants received a telephone or postcard reminder about diary completion. Patients who were still unwell after 28 days were followed-up, up to a maximum of 10 weeks, until they reported recovery. Antibiotic prescribing and reconsultation data for the 28 days of follow-up were obtained from the participants’ medical records. Data were double entered, with discrepancies resolved by checking the original data.
Data analysis
Discrete variables were expressed as percentages (counts) and continuous variables as means (standard deviations), unless stated otherwise. The primary analysis was intention to treat and assessed the predefined effects of the two interventions on antibiotic prescribing at the index consultation, incorporating an interaction effect, which we included to test and correct for a synergistic or antagonistic relation between the two interventions. Analysis was done using a three level logistic regression model to account and correct for variation at the level of the practice, general practitioner, and patient using a second order penalised quasi-likelihood approach. To correct for the effects on secondary outcomes we used a three level model, linear or logistic where appropriate. To explore simplification of the model we carried out analyses to investigate if the general practitioner level could be left out of the multilevel approach. Exploratory analyses investigating the influence of patients’ and practitioners’ characteristics on the main effects were carried out as sensitivity analyses. Results are presented as rates with corresponding P values (see web extra table for full logistic models).
Scores for each of the individual items on symptoms were added to create a total daily symptom score that ranged from 0% to 100%. We plotted the median daily symptom scores for the treatment groups. The Cronbach α for the full scale was greater than 0.7. A four level autoregressive moving average (1,1) model was fitted to the symptom scores (logged) to account for practice, general practitioner, patient, and repeated measurements over time using restrictive maximum likelihood. This modelled the correlation between repeated assessments within individual patients to allow for greater correlation between assessments that were closer in time. The effects of the interventions on recovery were studied by comparing the slopes of symptom scores over time in the groups.46 Analysis was done using SPSS 13.0, R, and Mlwin 2.0.
Our trial follows the consolidated standards of reporting trials guidelines, extended for cluster randomised controlled trials.47 Further details of the trial protocol, including descriptions of the C reactive protein test and training in enhanced communication are described elsewhere.39 43
Results
All 30 general practitioners received the allocated intervention, and 10 general practitioners were assigned to the usual care arm (fig 1). All the general practitioners recruited patients. Three general practitioners in the training group went on maternity leave halfway through the study. The characteristics of the general practitioners were similar across the groups and comparable to Dutch general practitioners (table 1). In total, 431 patients with lower respiratory tract infection were recruited (factor A, 227 to the C reactive protein test group v 204 to the no test group, and factor B, 201 to the training in enhanced communication skills group v 230 to the no training group), and for all of these, data for the primary outcome measure were available. Diary data were available for 90% of participants (fig 1). Table 2 shows patients’ baseline characteristics.
Table 1.
Characteristics of study general practitioners in practices allocated to point of care testing for C reactive protein (CRP), training in enhanced communication skills, interventions combined, and usual care. Values are means (SD) unless stated otherwise
| Characteristics | CRP test (n=10) | Communication skills training (n=10) | CRP test and communication skills training (n=10) | Usual care (n=10) | All general practitioners in trial (n=40) | Netherlands* (n=8495) |
|---|---|---|---|---|---|---|
| Men (%) | 60 | 50 | 60 | 70 | 60 | 66 |
| Age (years) | 42.4 (7.0) | 46.5 (9.4) | 45.7 (4.9) | 47.0 (9.9) | 45.4 (8.0) | 47.4 |
| Patient list size | 1770 (260) | 1920 (690) | 1925 (560) | 2050 (570) | 1920 (540) | 1725 (for 0.75 full time equivalent) |
| Full time equivalent | 0.71 (0.13) | 0.78 (0.18) | 0.74 (0.21) | 0.77 (0.18) | 0.75 (0.17) | 0.75 |
| Years in general practice | 12.9 (8.5) | 12.9 (9.7) | 16.2 (6.4) | 17.9 (10.5) | 15.0 (8.9) | 10 |
*Numbers derived from Netherlands Institute for Health Services Research, 2006 (www.nivel.nl).
Table 2.
Characteristics of patients managed by general practitioners in intervention (point of care C reactive protein (CRP) testing or training in enhanced communication skills) and control arms. Values are numbers (percentages) unless stated otherwise
| Characteristics | CRP test (n=227) | No CRP test (n=204) | Communication skills training (n=201) | No communication skills training (n=230) | |
|---|---|---|---|---|---|
| Women | 134 (59.0) | 131 (64.2) | 130 (64.7) | 135 (58.7) | |
| Mean (SD) age (years) | 49.4 (14.7) | 50.3 (16.0) | 51.4 (15.3) | 48.5 (15.1) | |
| Education level: | |||||
| Lower education | 67 (33.3) | 67 (39.2) | 66 (37.1) | 68 (35.1) | |
| Secondary education | 75 (37.3) | 61 (35.7) | 69 (38.8) | 67 (34.5) | |
| Higher education | 59 (29.4) | 43 (25.1) | 43 (24.2) | 59 (30.4) | |
| Current smoking | 49 (23.7) | 61 (34.3) | 47 (25.8) | 63 (31.0) | |
| Signs and symptoms: | |||||
| Shortness of breath | 152 (67.0) | 120 (58.8) | 110 (54.7) | 162 (70.4) | |
| Wheezing | 80 (35.2) | 78 (38.2) | 73 (36.3) | 85 (37.0) | |
| Chest pain | 143 (63.0) | 110 (53.9) | 120 (59.7) | 133 (57.8) | |
| Abnormalities on auscultation | 106 (46.7) | 123 (60.3) | 104 (51.7) | 125 (54.3) | |
| Fever | 99 (43.6) | 76 (37.3) | 81 (40.3) | 94 (40.9) | |
| Perspiration | 112 (49.3) | 82 (40.2) | 79 (39.3) | 115 (50.0) | |
| Headache | 108 (47.6) | 99 (48.5) | 86 (42.8) | 121 (52.6) | |
| Myalgia | 117 (51.5) | 84 (41.2) | 94 (46.8) | 107 (46.5) | |
| Generally feeling unwell | 181 (79.7) | 158 (77.5) | 160 (79.6) | 179 (77.8) | |
| Duration of cough (days): | |||||
| Mean (SD) | 10.1 (6.6) | 10.3 (6.5) | 11.0 (6.7) | 9.4 (6.2) | |
| Median (interquartile range) | 7 (5-14) | 9 (5-14) | 10 (5-14) | 7 (5-14) | |
| Comorbidity | |||||
| Chronic obstructive pulmonary disease | 17 (7.5) | 14 (6.9) | 11 (5.5) | 20 (8.7) | |
| Asthma | 23 (10.1) | 16 (7.8) | 19 (9.5) | 20 (8.7) | |
| Diabetes mellitus | 9 (4.0) | 9 (4.4) | 10 (5.0) | 8 (3.5) | |
| Heart disease | 11 (4.8) | 9 (4.4) | 10 (5.0) | 10 (4.3) |
Interventions
C reactive protein was measured in all 227 patients recruited by general practitioners allocated to point of care testing (range <8-225 mg/l). Overall, 69% of patients had test results of <20 mg/l, 24% of 20-99 mg/l, and 7% of greater than 100 mg/l. This distribution is similar to previous findings for lower respiratory tract infection in primary care.15 Standard laboratory testing for C reactive protein was not ordered for any patient in the no test group. Overall, 66% of the patients recruited by general practitioners allocated to training in enhanced communication skills recalled their doctors using at least three of four specific communication skills (asking opinions on antibiotics, exploring worries, eliciting expectations, and providing information on the natural course and duration of lower respiratory tract infection) compared with 19% of patients in the no training group.
Effects on antibiotic prescribing and reconsultation
General practitioners in the C reactive protein test group prescribed significantly fewer antibiotics than those in the no test group (31% v 53%, P=0.02; table 3). Similarly, general practitioners in the communication skills training group prescribed significantly fewer antibiotics than those in the no training group (27% v 54%, P<0.01). The two interventions showed no statistically significant interaction effect (P=0.78), although there was a trend for a synergistic effect. Adjustment at the level of the general practitioner in a simplified two level model led to improvement of model fit, so analyses were done according to the predefined three level model strategy (see web extra table).
Table 3.
Effects of interventions on antibiotic prescribing at index consultation and antibiotic prescribing and reconsultation during 28 days’ follow-up
| Variables | Intervention groups | Control groups | P value† | Intracluster coefficient | |||
|---|---|---|---|---|---|---|---|
| No of patients | Percentage (crude 95% CI*) | No of patients | Percentage (crude 95% CI*) | ||||
| C reactive protein test: | n=227 | n=204 | |||||
| Antibiotics at index consultation | 70 | 30.8 (21.8 to 39.8) | 108 | 52.9 (43.0 to 62.8) | 0.02 | 0.12 | |
| Antibiotics at days 1 to 28 | 102 | 44.9 (35.2 to 54.6) | 119 | 58.3 (48.5 to 68.1) | <0.01 | 0.12 | |
| Reconsultation within 28 days | 79 | 34.8 (28.3 to 41.3) | 62 | 30.4 (23.8 to 37.0) | 0.50 | 0.01 | |
| Communication skills training: | n=201 | n=230 | |||||
| Antibiotics at index consultation | 55 | 27.4 (25.6 to 36.6) | 123 | 53.5 (43.8 to 63.2) | <0.01 | 0.12 | |
| Antibiotics at days 1 to 28 | 76 | 37.8 (28.1 to 47.5) | 145 | 63 (53.6 to 72.4) | <0.001 | 0.12 | |
| Reconsultation within 28 days | 56 | 27.9 (21.4 to 34.4) | 85 | 37.0 (30.4 to 43.6) | 0.14 | 0.01 | |
*Calculated and inflated for clustering by using standard deviation inflated by variance inflation factor.53
†Calculated from second order penalised quasi-likelihood multilevel logistic regression model adjusted for variance at general practitioner and practice level (random intercept at practice and general practitioner level). Models included both interventions and interaction term of interventions. See web extra for corresponding β coefficients.
The interventions showed no statistically significant difference in reconsultations. Prescribing during the 28 days after the index consultation was slightly lower for patients in the communication skills training group. After adjusting for clustering, however, this effect was not statistically significant.
Antibiotic prescribing at any point during the 28 days’ follow-up (prescribing rates at the index consultation combined with prescribing rates at reconsultations) remained significantly lower in patients in the C reactive protein test group compared with those in the no test group (45% v 58%, P<0.01) as well as for patients in the communication skills training group compared with patients in the no training group (38% v 63%, P<0.001).
Systemic symptoms were not associated with antibiotic prescribing. Of the signs and symptoms recorded by the general practitioners only abnormal auscultation was associated with antibiotic prescribing when tested in a multiple regression analysis. No associations were found between systemic symptoms and reconsultation in similar analyses. This model was corrected for reconsultations at the general practitioners’ request; 20.6% of reconsultations within 28 days of the index consultation were scheduled by the general practitioner, with the remaining 79.4% initiated by the patient. In total, 47 patients (10.9%) reconsulted more than once within the 28 days. This reconsultation pattern was similar across the groups.
General practitioners prescribed a wide range of antibiotics during the study: doxycycline for 41% of patients, amoxicillin for 26%, amoxicillin-clavulanate for 16%, clarithromycin for 7%, azithromycin for 4%, and others for 6%. Doxycycline and amoxicillin are first line antibiotics for lower respiratory tract infection according to the Dutch national guidelines for acute cough.41
Sensitivity analyses
Although the interaction term was not significant, as this test has low power, an exploratory analysis was carried out to study the magnitude of differences between the four individual trial groups. General practitioners using the C reactive protein point of care test and who were also trained in communication skills prescribed antibiotics to 23% of participants compared with 67% in the usual care group (table 4).
Table 4.
Exploratory analysis of antibiotic prescribing at index consultation by general practitioners; intervention groups: practices allocated to point of care testing for C reactive protein (CRP), training in enhanced communication skills, interventions combined, and usual care
| Antibiotic prescribing at index consultation | CRP test (n=110) | Communication skills training (n=84) | CRP test and communication skills training (n=117) | Usual care (n=120) |
|---|---|---|---|---|
| % (No) of patients | 39 (43) | 33 (28) | 23 (27) | 67 (80) |
| Crude 95% CI* | 25.6 to 52.6 | 19.5 to 47.1 | 11.6 to 34.6 | 53.9 to 79.5 |
Testing for significance was not done as trial was designed as a factorial trial.
*Calculated and inflated for clustering by using standard deviation inflated by variance inflation factor.53
Possible moderation of effect was explored in a sensitivity analysis of the primary end point by including personal factors, case-mix, and relevant comorbidities (table 2) in a multilevel logistic model. This produced similar effects for the interventions as in the primary analysis, suggesting that the interventions were principally responsible for the reduction in antibiotic prescribing. The effect of the interventions was similar during both recruitment winters.
Possible recruitment bias after randomisation was investigated by considering rates for consultation and overall antibiotic prescribing (anatomical therapeutic chemical classification J001) for international classification primary care codes R78 (acute broch(iol)itis) and R81 (pneumonia) for the two recruitment winters in a subsample of 14 study general practitioners who contributed to a regional medical registration database. Antibiotic prescribing for study patients by this subset of general practitioners at index consultations was similar to all their 325 patients registered with lower respiratory tract infection on the international classification primary care database (table 5). Patients recruited to the trial were slightly younger than the registered patients.
Table 5.
Non-inclusion analysis of antibiotic prescribing rates at index consultation and demographics for enrolled and non-enrolled patients with lower respiratory tract infection seen by 14 trial general practitioners during two study winters, 2005-6 and 2006-7. Values are percentages (numbers) unless stated otherwise
| Variables | CRP test (8 general practitioners) | No CRP test (6 general practitioners) | Communication skills training (6 general practitioners) | No communication skills training (8 general practitioners) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Enrolled patients (n=76) | Non-enrolled patients (n=84) | Enrolled patients (n=39) | Non-enrolled patients (n=189) | Enrolled patients (n=46) | Non-enrolled patients (n=101) | Enrolled patients (n=69) | Non-enrolled patients (n=172) | |||
| Antibiotics prescribed at index consultation | 37 (28) | 27 (23) | 44 (17) | 50 (95) | 30 (14) | 27 (27) | 45 (31) | 53 (91) | ||
| Women | 63 (48) | 60 (50) | 69 (27) | 55 (104) | 80 (37) | 59 (60) | 55 (38) | 55 (94) | ||
| Mean (SD) age | 50.2 (14.6) | 61.7 (19.9) | 51.3 (16.2) | 61.3 (18.9) | 53.0 (16.1) | 61.3 (18.9) | 48.9 (14.3) | 55.6 (20.7) | ||
Data were derived from central registration system of Foundation of Primary Health Care Centres Eindhoven (SGE). International classification of primary care codes for acute bronchitis (R78) and pneumonia (R81) were used and antibiotic prescribing per consultation using Anatomical Therapeutic chemical code J001 could be determined. Fourteen of 40 general practitioners were connected to this system at time of the trial.
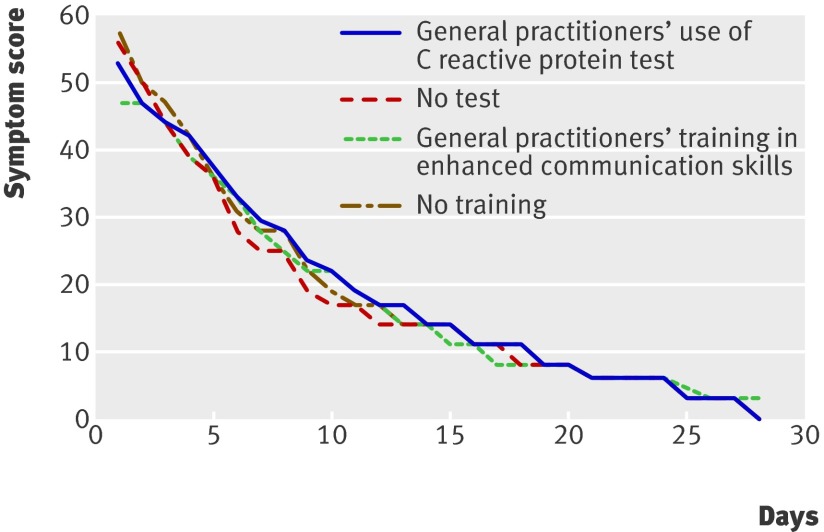
Clinical recovery
The interventions had no discernible effect on recovery, resulting in comparable median daily symptom scores for all four groups of patients. Recovery slopes are presented as median symptom scores per day in figure 2. Clinical recovery based on symptom scores and analysed by a multilevel autoregressive moving average model was similar for all study groups resulting in one recovery slope for all groups (effect of test on recovery P=0.99, effect of training on recovery P=0.97, see web extra figure). Baseline characteristics were similar between patients who completed the symptom scores (90%) and those who did not. Median patient reported time to recovery was 22 days (interquartile range 14-28). Although this trial was not designed to assess safety of either intervention in lower respiratory tract infection, no serious adverse events (death or admission to hospital) occurred.
Fig 2 Median symptom scores (%) for treatment groups (see web extra figure for full four level corrected recovery slopes). Treatment groups had identical clinical recovery despite fewer antibiotics prescribed in intervention groups
Patient satisfaction, enablement, and intention to reconsult
Overall, satisfaction with the index consultation was high, with no statistically significant differences between treatment groups. Fewer patients in the communication skills training group indicated that they would consult with similar symptoms in the future, but differences in future consulting intentions were not statistically significant between groups. The score for the patient enablement index was similar for all groups (table 6).
Table 6.
Effects of interventions on secondary outcomes (assessed after index consultation). Values are percentages (numbers) unless stated otherwise
| Outcomes | CRP test (n=227) | No CRP test (n=204) | P value* | Communication skills training (n=201) | No communication skills training (n=230) | P value* | |
|---|---|---|---|---|---|---|---|
| Patient satisfaction: | |||||||
| % (No) at least very satisfied | 76.8 (159) | 76.0 (136) | 0.53 | 78.7 (144) | 74.4 (151) | 0.88 | |
| Crude 95% CI† | 70.8 to 82.8 | 69.6 to 82.4 | 72.5 to 84.9 | 68.2 to 80.6 | |||
| Future consultation intention: | |||||||
| % (No) likely to reconsult | 75.4 (153) | 78.9 (138) | 0.52 | 73.6 (134) | 80.1 (157) | 0.16 | |
| Crude 95% CI† | 69.2 to 81.6 | 72.8 to 85.0 | 67.0 to 80.2 | 74.4 to 85.8 | |||
| Patient enablement‡: | |||||||
| Median (interquartile range) score | 3 (4) | 3 (4) | — | 3 (4) | 3 (4) | — | |
| Mean (SD) score | 2.97 (2.59) | 3.40 (2.48) | 0.13 | 3.29 (2.52) | 3.06 (2.54) | 0.70 |
CRP=C reactive protein.
*Calculated from models adjusted for variance at general practitioner and practice level.
†Calculated and inflated for clustering by using standard deviation inflated by variance inflation factor.53
‡Maximum score 12.
Discussion
Both general practitioners’ use of point of care testing for C reactive protein and training in enhanced communication skills had a clinically important effect on antibiotic prescribing at the index consultation for lower respiratory tract infection and antibiotic prescribing during the 28 days’ follow-up period, without affecting clinical recovery or patients’ satisfaction.
Strengths and limitations of the study
Factorial designs are efficient for assessing two interventions when they act independently of each other.40 Our results did not show interaction effects between the C reactive protein test and the enhanced communication skills strategy—that is, the combined effect of the test and training was neither synergistic nor antagonistic. We nevertheless included interaction coefficients in all models to correct for possible undetected interactions.
The sustainability of the acquired communication skills may be questioned. We previously reported sustained competence in implementing these skills.43 A sensitivity analysis of the results by winter period (2005-6 and 2006-7) showed that the observed effects on antibiotic prescribing were similar during both periods. Moreover, most patients seeing general practitioners who had been allocated to communication skills training recalled key topics being covered during the consultation. The enhanced communication skills may therefore have become embedded in the general practitioners’ daily routine as the method does not increase mean consultation times, which is crucial in time pressured practice.43 However, general practitioners may need time to gain confidence and experience in interpreting the results of the C reactive protein test in general, and in using the point of care result to guide treatment in particular. At the time of the study, point of care testing for C reactive protein was nearly non-existent in Dutch primary care. We did, however, observe similar effects on antibiotic prescribing across the winters, despite the short run-in and familiarisation period with the test of a maximum of eight weeks before the trial started. Our results contrast with recent findings from Scandinavia where over-prescribing of antibiotics was associated with intermediate elevated test results.48 In addition, excessive C reactive protein testing for self limiting respiratory tract infections such as the common cold is widespread in settings where C reactive protein point of care testing is widely used in primary care.49 Hence a proper introduction to the test with recommendations on the interpretation of the additional diagnostic value for a specific respiratory tract infection as implemented in our trial seems crucial for optimal utilisation.
We recruited 431 patients, with 100% ascertainment of the primary outcome and 90% ascertainment of patient reported outcomes. This higher than expected follow-up rate increased the study power. The target number of patients in the training arm was not achieved because three general practitioners went on maternity leave. Nevertheless, with over 200 patients in both groups we were able to evaluate the effect of training in enhanced communication skills. Validity was increased by taking variation at both practice and doctor levels into account.50 51
A common potential weakness in randomised controlled trials using a cluster design is recruitment bias after randomisation, as differential numbers and types of patient may be enrolled after the intervention has been allocated.52 53 54 However, the baseline characteristics of the recruited patients were similar across the groups, and inclusion of known covariates (personal characteristics and case-mix) in our models did not affect the observed effects. Both suggest that differential recruitment was not an issue in this study. Nevertheless, unmeasured covariates may have influenced outcomes. Individual randomisation, which balances unknown variables, was not an option for our study design because our interventions were targeted at the level of general practitioner, and once trained in enhanced communication skills general practitioners could not be expected to revert to an untrained state at random.
The participation of the general practitioners would have been hampered if they could not have decided on patient recruitment. In studies of acute conditions in primary care it is seldom feasible for anyone other than the treating clinician to identify and recruit suitable patients. Non-inclusion analysis suggests that differential enrolment to our study groups did not occur.
Patients recruited into our trial groups were slightly younger than patients with lower respiratory tract infection in a large database of routine primary care clinical records. This may be explained by our inclusion criteria—for example, patients seen during home visits or in old people’s care homes were ineligible. Strikingly, based on this trial and on the non-inclusion analysis, women were more likely to be enrolled by general practitioners allocated to the training in enhanced communication skills group, shedding interesting light on this sex issue, as most people consulting for lower respiratory tract infection in primary care are female.
Comparison with other studies
While some previous randomised studies failed to find an effect on antibiotic prescribing,32 34 those that did mostly involved multifaceted complex interventions.35 36 38 55 The effect size of both our interventions was greater than in any previous study of which we are aware. Another partly illness focused approach, delayed prescribing, also yielded large effects on antibiotic prescribing. However, the applicability of the largest trial on delayed prescribing for lower respiratory tract infection was limited by its exclusion of patients with a history suggestive of pneumonia, since the difficulty in differentiating pneumonia from acute bronchitis is one of the biggest drivers of unnecessary prescribing in lower respiratory tract infection.37 Other useful biomarkers, such as procalcitonin, have been suggested to guide antibiotic treatment for lower respiratory tract infection. These tests are not yet available at the point of care, however, thereby limiting their applicability to general practice.56 57
Implications
The broad approach exemplified by the interventions evaluated in this trial may enhance management of a wider range of patients than just those with lower respiratory tract infection. Both approaches (excluding serious infections by using a biomarker and eliciting patients’ expectations, concerns, and opinion on antibiotics while providing evidence based information on treatment and clinical course by training doctors in communication skills) could be used for most common infections in primary care. Moreover, the combined effect of the interventions stresses the importance of a shared approach; serious infection needs to be ruled out, and patients’ expectations and worries should be identified and responded to, all without unduly increasing consultation time.43 These interventions not only aim to reduce antibiotic prescribing. Crucially, combining the disease and illness approach implies that decisions on antibiotic prescribing should focus on targeting the drug to the patient while balancing benefits and possible harms of treatment to those with potential societal benefits from restrictive prescribing.58 C reactive protein may contribute to safely withholding antibiotics from most people with low C reactive protein values who most probably would not benefit from antibiotic treatment, while enhanced communication may increase patients’ understanding of prescribing decisions without the feeling of being dismissed with unsatisfactory explanations. This may lead to enhanced self care in the future.
We intended to study effectiveness and not efficacy (as in an explanatory trial).59 The pragmatic nature of our study enhances the generalisability of the results. Our study included the full range of patients with lower respiratory tract infection seen by general practitioners, with all the associated diagnostic uncertainty. If the interventions prove cost effective, implementation on a larger scale will be facilitated by the close to daily practice approach used in the trial. Our results may guide investment in primary care to either C reactive protein test devices or training in communication skills, or a combination of both.
Although the Netherlands has one of the lowest overall prescribing rates for antibiotics worldwide, prescribing for lower respiratory tract infection remains high, with rates similar to other European countries and the United States. As most patients in our study did not undergo chest radiography we do not know the number who had community acquired pneumonia. The characteristics of the patients, however, seem comparable to previous studies on lower respiratory tract infection, in which about 11% of patients had community acquired pneumonia.15 Chest radiography before deciding to prescribe is carried out less often in Dutch primary care than in the United States, therefore requiring all patients to undergo chest radiography in this study would have limited generalisability. We acknowledge that the use of such ancillary tests varies between countries,60 but the method of recruitment, the use of standardised clinical criteria, and the finding of similar prescribing rates for antibiotics between the United States, the Netherlands, and other parts of Europe add weight to the wider applicability of our findings.
The antibiotic prescribing rate of 67% for our usual care group (see table 4) is comparable to other studies in the Netherlands and elsewhere, including the United States and the United Kingdom.8 9 10 Given that 370 000 prescriptions for antibiotics are issued in 550 000 consultations for lower respiratory tract infection (based on 44 adults consulting for lower respiratory tract infection per 1000 adults per year4 61) in the Netherlands each year, up to 240 000 prescriptions may be avoided annually if our findings were to be replicated on a national scale. Reducing antibiotic prescribing in primary care may decrease levels of antibiotic resistance nationally and internationally, but it may also have substantial effects locally. General practices that reduced antibiotic prescribing the most over a seven year period in the United Kingdom showed the greatest reductions in antibiotic resistance locally.62 Implementing the approaches we evaluated for this common condition in primary care in other healthcare settings is feasible.
Conclusions
Both interventions were effective on their own. These effects could have major implications for the management of lower respiratory tract infection. Prescribing fewer antibiotics in the intervention groups did not result in poorer patient outcomes. Both interventions required training clinicians in new skills and have potential applicability in primary care beyond the condition we studied. For example, C reactive protein may effectively guide treatment for other infections and inflammatory conditions. Shared decision making skills are applicable to most medical conditions. Clinical methods in primary care may be most successful in achieving evidence based management if disease focused and illness focused interventions are integrated.
What is already known on this topic
Cough due to lower respiratory tract infection is one of the commonest reasons for prescribing antibiotics
Most such prescriptions in primary care do not benefit patients
Diagnostic uncertainty and patients’ expectations and concerns are major drivers of unnecessary antibiotic prescribing
What this study adds
General practitioners’ use of C reactive protein testing (disease focused approach) and training in communication skills (illness focused approach) both resulted in decreased antibiotic prescribing for lower respiratory tract infection in primary care
Patient recovery and satisfaction with care were not compromised
The two approaches combined resulted in the greatest reduction in antibiotic prescribing
We thank Susanne Hanssen, Paula Rinkens, and Ger Driessen (Maastricht) for their support with data collection and the logistics of the study; Mark Kelly (Cardiff) for his assistance with the analysis of the clinical recovery model; and the participating general practitioners and patients.
Contributors: CCB and G-JD conceived the study. All authors contributed to the design and implementation of the study. CCB drafted the training in communication skills method. RMH drafted the training in use of C reactive protein testing. JWLC ran the project, wrote the first draft of the manuscript, had full access to all the data in the study, takes responsibility for the integrity of the data and the accuracy of the data analysis, and is guarantor. All authors commented on the first draft and all revisions. KH supervised the development of the analysis plan and the statistical analyses. All authors interpreted the data and findings.
Funding: This trial was funded by the Netherlands Organisation for Health Research and Development (grant 945-04010). JWLC is supported by a grant from the Netherlands Organisation for Health Research and Development as a MD-medical research trainee. KH is funded by the Wales Office for Research and Development. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Competing interests: None declared.
Ethical approval: This study was approved by the ethics committee of Catherina Hospital in Eindhoven, the Netherlands.
Cite this as: BMJ 2009;338:b1374
References
- 1.McWhinney IR. A textbook of family medicine. 2nd ed. New York, Oxford: Oxford University Press, 1997.
- 2.Dinant GJ, Buntinx FF, Butler CC. The necessary shift from diagnostic to prognostic research. BMC Fam Pract 2007;8:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Butler CC, Kinnersley P, Prout H, Rollnick S, Edwards A, Elwyn G. Antibiotics and shared decision-making in primary care. J Antimicrob Chemother 2001;48:435-40. [DOI] [PubMed] [Google Scholar]
- 4.Macfarlane J, Holmes W, Gard P, Macfarlane R, Rose D, Weston V, et al. Prospective study of the incidence, aetiology and outcome of adult lower respiratory tract illness in the community. Thorax 2001;56:109-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schappert SM, Burt CW. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001-02. Vital Health Stat 13 2006:1-66. [PubMed]
- 6.Woodhead M, Blasi F, Ewig S, Huchon G, Leven M, Ortqvist A, et al. Guidelines for the management of adult lower respiratory tract infections. Eur Respir J 2005;26:1138-80. [DOI] [PubMed] [Google Scholar]
- 7.Smucny J, Fahey T, Becker L, Glazier R. Antibiotics for acute bronchitis. Cochrane Database Syst Rev 2004;(4):CD000245. [DOI] [PubMed] [Google Scholar]
- 8.Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians JAMA 1997;278:901-4. [PubMed] [Google Scholar]
- 9.Kuyvenhoven MM, Verheij TJ, de Melker RA, van der Velden J. Antimicrobial agents in lower respiratory tract infections in Dutch general practice. Br J Gen Pract 2000;50:133-4. [PMC free article] [PubMed] [Google Scholar]
- 10.Macfarlane J, Lewis SA, Macfarlane R, Holmes W. Contemporary use of antibiotics in 1089 adults presenting with acute lower respiratory tract illness in general practice in the UK: implications for developing management guidelines. Respir Med 1997;91:427-34. [DOI] [PubMed] [Google Scholar]
- 11.Goossens H, Ferech M, Vander Stichele R, Elseviers M. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 2005;365:579-87. [DOI] [PubMed] [Google Scholar]
- 12.Bradley JS, Guidos R, Baragona S, Bartlett JG, Rubinstein E, Zhanel GG, et al. Anti-infective research and development—problems, challenges, and solutions. Lancet Infect Dis 2007;7:68-78. [DOI] [PubMed] [Google Scholar]
- 13.Nordberg P, Monnet DL, Cars O. Antibacterial drug resistance: options for concerted action. Geneva: Department of Medicines Policy and Standards, World Health Organization, 2005:1-48.
- 14.Fischer T, Fischer S, Kochen MM, Hummers Pradier E. Influence of patient symptoms and physical findings on general practitioners’ treatment of respiratory tract infections: a direct observation study. BMC Fam Pract 2005;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hopstaken RM, Muris JWM, Knottnerus JA, Kester ADM, Rinkens PELM, Dinant GJ. Contributions of symptoms, signs, erythrocyte sedimentation rate and C-reactive protein to a diagnosis of pneumonia in acute lower respiratory tract infection. Br J Gen Pract 2003;53:358-64. [PMC free article] [PubMed] [Google Scholar]
- 16.Melbye H, Straume B, Aasebo U, Brox J. The diagnosis of adult pneumonia in general practice. The diagnostic value of history, physical examination and some blood tests. Scand J Prim Health Care 1988;6:111-7. [DOI] [PubMed] [Google Scholar]
- 17.McIsaac WJ, Butler CC. Does clinical error contribute to unnecessary antibiotic use? Med Decis Making 2000;20:33-8. [DOI] [PubMed] [Google Scholar]
- 18.Wood F, Simpson S, Butler CC. Socially responsible antibiotic choices in primary care: a qualitative study of GPs’ decisions to prescribe broad-spectrum and fluroquinolone antibiotics. Fam Pract 2007;24:427-34. [DOI] [PubMed] [Google Scholar]
- 19.Van der Meer V, Neven AK, Broek PJvd, Assendelft WJJ. Diagnostic value of C reactive protein in infections of the lower respiratory tract: systematic review. BMJ 2005;331:26-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dahler Eriksen BS, Lassen JF, Petersen PH, Lund ED, Lauritzen T, Brandslund I. Evaluation of a near-patient test for C-reactive protein used in daily routine in primary healthcare by use of difference plots. Clin Chem 1997;43:2064-75. [PubMed] [Google Scholar]
- 21.Davey P, Pagliari C, Hayes A. The patient’s role in the spread and control of bacterial resistance to antibiotics. Clin Microbiol Infect 2002;8(suppl 2):43-68. [DOI] [PubMed] [Google Scholar]
- 22.Avorn J, Solomon DH. Cultural and economic factors that (mis)shape antibiotic use: the nonpharmacologic basis of therapeutics. Ann Intern Med 2000;133:128-35. [DOI] [PubMed] [Google Scholar]
- 23.Altiner A, Knauf A, Moebes J, Sielk M, Wilm S. Acute cough: a qualitative analysis of how GPs manage the consultation when patients explicitly or implicitly expect antibiotic prescriptions. Fam Pract 2004;21:500-6. [DOI] [PubMed] [Google Scholar]
- 24.Butler CC, Rollnick S, Pill R, Maggs Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ 1998;317:637-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coenen S, Michiels B, Renard D, Denekens J, Van Royen P. Antibiotic prescribing for acute cough: the effect of perceived patient demand. Br J Gen Pract 2006;56:183-90. [PMC free article] [PubMed] [Google Scholar]
- 26.Little P, Dorward M, Warner G, Stephens K, Senior J, Moore M. Importance of patient pressure and perceived pressure and perceived medical need for investigations, referral, and prescribing in primary care: nested observational study. BMJ 2004;328:444-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmonth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ 1997;315:350-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cals JWL, Boumans D, Lardinois RJM, Gonzales R, Hopstaken RM, Butler CC, et al. Public beliefs on antibiotics and respiratory tract infections: an internet-based questionnaire study. Br J Gen Pract 2007;57:942-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stewart M. Patient-centered medicine: transforming the clinical method. 2nd ed. Abingdon: Radcliffe Medical, 2003.
- 30.Rollnick S, Seale C, Rees M, Butler C, Kinnersley P, Anderson L. Inside the routine general practice consultation: an observational study of consultations for sore throats. Fam Pract 2001;18:506-10. [DOI] [PubMed] [Google Scholar]
- 31.Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PPR, Tamm PM, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet 2004;363:600-7. [DOI] [PubMed] [Google Scholar]
- 32.Diederichsen HZ, Skamling M, Diederichsen A, Grinsted P, Antonsen S, Petersen PH, et al. Randomised controlled trial of CRP rapid test as a guide to treatment of respiratory infections in general practice. Scand J Prim Health Care 2000;18:39-43. [DOI] [PubMed] [Google Scholar]
- 33.Samore MH, Bateman K, Alder SC, Hannah E, Donnelly S, Stoddard GJ, et al. Clinical decision support and appropriateness of antimicrobial prescribing: a randomized trial. JAMA 2005;294:2305-14. [DOI] [PubMed] [Google Scholar]
- 34.Briel M, Langewitz W, Tschudi P, Young J, Hugenschmidt C, Bucher HC. Communication training and antibiotic use in acute respiratory tract infections. A cluster randomised controlled trial in general practice. Swiss Med Wkly 2006;136:241-7. [DOI] [PubMed] [Google Scholar]
- 35.Altiner A, Brockmann S, Sielk M, Wilm S, Wegscheider K, Abholz HH. Reducing antibiotic prescriptions for acute cough by motivating GPs to change their attitudes to communication and empowering patients: a cluster-randomized intervention study. J Antimicrob Chemother 2007;60:638-44. [DOI] [PubMed] [Google Scholar]
- 36.Coenen S, Van Royen P, Michiels B, Denekens J. Optimizing antibiotic prescribing for acute cough in general practice: a cluster-randomized controlled trial. J Antimicrob Chemother 2004;54(3):661-72. [DOI] [PubMed] [Google Scholar]
- 37.Little P, Rumsby K, Kelly J, Watson L, Moore M, Warner G, et al. Information leaflet and antibiotic prescribing strategies for acute lower respiratory tract infection: a randomized controlled trial. JAMA 2005;293:3029-35. [DOI] [PubMed] [Google Scholar]
- 38.Welschen I, Kuyvenhoven MM, Hoes AW, Verheij TJM. Effectiveness of a multiple intervention to reduce antibiotic prescribing for respiratory tract symptoms in primary care: randomised controlled trial. BMJ 2004;329:431-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cals JW, Hopstaken RM, Butler CC, Hood K, Severens JL, Dinant GJ. Improving management of patients with acute cough by C-reactive protein point of care testing and communication training (IMPAC3T): study protocol of a cluster randomised controlled trial. BMC Fam Pract 2007;8:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Montgomery A, Peters T, Little P. Design, analysis and presentation of factorial randomised controlled trials. BMC Med Res Method 2003;3:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Verheij TJM, Salomé PL, Bindels PJ, Chavannes AW, Ponsioen BP, Sachs APE, et al. NHG-Standaard Acuut hoesten. [Dutch College of General Practitioners guidelines on acute cough]. Huisarts Wet 2003;46:496-506. [Google Scholar]
- 42.Rollnick S, Kinnersley P, Butler C. Context-bound communication skills training: development of a new method. Med Educ 2002;36:377-83. [DOI] [PubMed] [Google Scholar]
- 43.Cals JW, Scheppers NA, Hopstaken RM, Hood K, Dinant GJ, Goettsch H, et al. Evidence based management of acute bronchitis; sustained competence of enhanced communication skills acquisition in general practice. Patient Educ Couns 2007;68:270-8. [DOI] [PubMed] [Google Scholar]
- 44.Watson L, Little P, Moore M, Warner G, Williamson I. Validation study of a diary for use in acute lower respiratory tract infection. Fam Pract 2001;18:553-4. [DOI] [PubMed] [Google Scholar]
- 45.Howie JG, Heaney DJ, Maxwell M, Walker JJ. A comparison of a patient enablement instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract 1998;15:165-71. [DOI] [PubMed] [Google Scholar]
- 46.Box GEP, Jenkins GM, Reinsel GC. Time series analysis: forecasting and control. 3rd ed. Englewood Cliffs, NJ: Prentice Hall, 1994.
- 47.Campbell MJ. Extending CONSORT to include cluster trials. BMJ 2004;328:654-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Andre M, Schwan A, Odenholt I. The use of CRP tests in patients with respiratory tract infections in primary care in Sweden can be questioned. Scand J Infect Dis 2004;36:192-7. [DOI] [PubMed] [Google Scholar]
- 49.Engstrom S, Molstad S, Lindstrom K, Nilsson G, Borgquist L. Excessive use of rapid tests in respiratory tract infections in Swedish primary health care. Scand J Infect Dis 2004;36:213-8. [DOI] [PubMed] [Google Scholar]
- 50.Mollison J, Simpson JA, Campbell MK, Grimshaw JM. Comparison of analytical methods for cluster randomised trials: an example from a primary care setting. J Epidemiol Biostat 2000;5:339-48. [PubMed] [Google Scholar]
- 51.Campbell MK, Fayers PM, Grimshaw JM. Determinants of the intracluster correlation coefficient in cluster randomized trials: the case of implementation research. Clin Trials 2005;2:99-107. [DOI] [PubMed] [Google Scholar]
- 52.Puffer S, Torgerson D, Watson J. Evidence for risk of bias in cluster randomised trials: review of recent trials published in three general medical journals. BMJ 2003;327:785-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Donner A, Klar N. Design and analysis of cluster randomization trials in health research. London: Arnold, 2000.
- 54.Hahn S, Puffer S, Torgerson DJ, Watson J. Methodological bias in cluster randomised trials. BMC Med Res Methodol 2005;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Arnold SR, Straus SE. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev 2005;(4):CD003539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Christ-Crain M, Muller B. Biomarkers in respiratory tract infections: diagnostic guides to antibiotic prescription, prognostic markers and mediators. Eur Respir J 2007;30:556-73. [DOI] [PubMed] [Google Scholar]
- 57.Holm A, Pedersen SS, Nexoe J, Obel N, Nielsen LP, Koldkjaer O, et al. Procalcitonin versus C-reactive protein for predicting pneumonia in adults with lower respiratory tract infection in primary care. Br J Gen Pract 2007;57:555-60. [PMC free article] [PubMed] [Google Scholar]
- 58.Cosby JL, Francis N, Butler CC. The role of evidence in the decline of antibiotic use for common respiratory infections in primary care. Lancet Infect Dis 2007;7:749-56. [DOI] [PubMed] [Google Scholar]
- 59.Roland M, Torgerson DJ. Understanding controlled trials: what are pragmatic trials? BMJ 1998;316:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cals J, Hopstaken R. Lower respiratory tract infections: treating patients or diagnoses? J Fam Pract 2006;55:545-6; author reply 546-7. [PubMed] [Google Scholar]
- 61.Hak E, Rovers MM, Kuyvenhoven MM, Schellevis FG, Verheij TJ. Incidence of GP-diagnosed respiratory tract infections according to age, gender and high-risk co-morbidity: the second dutch national survey of general practice. Fam Pract 2006;23:291-4. [DOI] [PubMed] [Google Scholar]
- 62.Butler CC, Dunstan F, Heginbothom M, Mason B, Roberts Z, Hillier S, et al. Containing antibiotic resistance: decreased antibiotic-resistant coliform urinary tract infections with reduction in antibiotic prescribing by general practices. Br J Gen Pract 2007;57:785-92. [PMC free article] [PubMed] [Google Scholar]