Abstract
Background/Objective:
To determine whether community integration and/or quality of life (QoL) among people living with chronic spinal cord injury (SCI) are superior among sport participants vs non-sport participants.
Study Design:
Cross-sectional study.
Participants/Methods:
Persons (n = 90) living in the community with SCI (ASIA Impairment Scale A–D), level C5 or below, > 15 years of age, ≥ 12 months postinjury, and requiring a wheelchair for > 1 hours/day were divided into 2 groups based on their self-reported sport participation at interview: sport participants (n = 45) and non-sport participants (n = 45).
Results:
Independent-sample t tests revealed that both Community Integration Questionnaire (CIQ) and Reintegration to Normal Living Index (RNL) total mean scores were higher among sport participants vs non-sport participants (P < 0.05). Significant correlation between CIQ and RNL total scores was found for all participants (Pearson correlation coefficients, P < 0.01). Logistic regression analysis revealed that the unadjusted odds ratio of a high CIQ mean score was 4.75 (95% CI 1.7, 13.5) among current sport participants. Similarly, the unadjusted odds ratio of a high RNL score was 7.00 (95% CI 2.3, 21.0) among current sport participants. Regression-adjusted odds ratios of high CIQ and high RNL scores were 1.36 (95% CI 0.09, 1.45) and 0.15 (95% CI 0.04, 0.55), respectively. The odds ratio for pre-SCI sport participation predicting post-SCI sport participation was 3.06 (95% CI 1.23, 7.65).
Conclusions:
CIQ and QoL scores were higher among sport participants compared to non-sport participants. There was an association between mean CIQ and RNL scores for both groups. Sport participants were 4.75 and 7.00 times as likely to have high CIQ and QoL scores. Both groups had a similar likelihood of high CIQ and RNL scores after adjusting for important confounders. Individuals who participated in sports prior to SCI were more likely to participate in sports post-SCI.
Keywords: Spinal cord injuries, Tetraplegia, Paraplegia, Disability, Sport participation, Wheelchair sports, Community reintegration, Quality of life
INTRODUCTION
It is well established that participation in sports improves psychological well-being among able-bodied individuals (1–5). There is increasing interest in the impact of sport participation on the psychological well-being of individuals with disabilities, particularly individuals with spinal cord injury (SCI). Psychological well-being is defined by the constructs of mood, trait anxiety, self-esteem, and mastery, and these constructs have been validated in studies involving individuals with disabilities (6–8). Recent studies have shown that participation in wheelchair sports improves psychological well-being (6–11) and life satisfaction (12). A number of these studies have examined various individual characteristics of wheelchair sport participants that may influence their improved psychological well-being scores (6,13–16). These characteristics have included age of disability onset (13), socioeconomic status (17), competitive level (6), etiology of impairment (congenital or acquired injury) (14), and type of impairment (tetraplegia vs paraplegia) (15,16).
However, few investigations (18,19) have related this enhanced psychological status of sport participants with SCI to a rehabilitation outcome, specifically community integration or quality of life (QoL). Dijkers has defined community integration as “. . . acquiring/resuming age-/gender-/culture-appropriate roles/statuses, including independence/interdependence in decision making, and productive behaviours performed as part of multivaried relationships with family, friends, and others in natural community settings” (20). Tasiemski et al (18) examined the outcomes of education and employment status in relation to involvement in sports and recreation after SCI and found no significant correlation between sport and recreation involvement and education or employment status. Nemunaitis et al (19) compared 19 individuals with SCI on a wheelchair basketball team to 38 individuals with SCI who were not members of a team. They concluded that membership in a wheelchair basketball team was correlated with improved community integration, based on increased Community Integration Questionnaire (CIQ) (21) productivity subscale scores among the wheelchair basketball team members. The effects of other potential confounding associations with community integration, such as pre-SCI and post-SCI sport participation, have not previously been examined.
Limitations of prior studies include small sample sizes, lack of data describing pre-SCI sport participation, and a lack of details regarding individual vs team sport participation, recreational vs elite sport participation, number of sports played, and the duration of sport participation. There is uncertainty among rehabilitation providers about the impact of sports on CI and QoL after SCI.
The aim of the current study was to determine whether community integration and/or QoL among people with SCI were superior in sport participants when compared to non-sport participants. Secondary objectives were (a) to describe pre-SCI and post-SCI sport participation (number of sports played, mode [type] of sport, competitive level, frequency of participation, and number of years played); (b) to determine whether correlations exist between community integration and QoL scores; (c) to determine the odds of high post-SCI community integration or QoL based on current SCI sport participation; and (d) to determine the odds of sport participation post-SCI based on pre-SCI sport participation. We hypothesized that (a) wheelchair sport participation would be associated with better community integration and QoL outcomes among persons with chronic SCI, and (b) pre-SCI sport participation would predict post-SCI participation.
METHODS
Study Design
A cross-sectional cohort study was conducted to determine the association between sport exposure (pre-SCI and post-SCI) and the outcomes of interest—community integration and QoL—among persons with chronic SCI living in Ontario, Canada. Community integration was measured by the CIQ (21), and QoL was measured by the Reintegration to Normal Living Index (RNL) (22).
Participants and Recruitment
Participants were Canadian residents at least 16 years of age, had injury levels at C5 or below of any etiology (ASIA Impairment Scale (AIS) A to D), had been injured ≥ 12 months prior to the time of the interview, were living in the community, and were wheelchair dependent for at least 1 hour per day outside of sport activities. Neurological level of injury of C5 or below was the criterion chosen, as individuals with this level of impairment comprise the majority of persons participating in wheelchair sports, and individuals with a neurological level above C5 would be less likely to be living in the community. Persons were excluded if they were hospitalized at the time of the interview, even if they had been living in the community immediately prior to the admission. Those with an intercurrent illness not requiring hospitalization (eg, urinary tract infection) were included.
The investigators used 2 sampling strategies to try to capture an equal number of sport (recreational, organized competitive, and elite/professional) and non-sport participants with SCI. All non-sport participants were recruited from outpatient clinic waiting areas at the Toronto Rehab Lyndhurst Centre (TRLC), a tertiary SCI rehabilitation center in Toronto, Ontario, Canada. Sport participants were recruited from outpatient clinic waiting areas at TRLC (approximately 30% of the sport participant group), the fitness center at TRLC (approximately 20% of the sport participant group), and organized wheelchair sporting events (approximately 50% of the sport participant group). The primary investigator (S.M.) attended 4 national wheelchair sporting events and 1 international basketball competition, held within the southern Ontario region between June and August 2004. Recruitment continued until the desired sample size was achieved.
At each sporting venue, the primary investigator spoke with potential participants about the purpose of the study and handed them a letter of introduction to the study. Verbal consent was then obtained to contact the interested individual by telephone within a 4-week period. Eligible individuals were contacted by telephone to arrange for a mutually convenient time to complete the 20- to 60-minute telephone interview. After verbal consent to participate was obtained (recorded in a telephone consent log), the interview was conducted by a single interviewer, each person's sociodemographic characteristic and impairment characteristics, medical status, sport participation, and CIQ and RNL scores were recorded sequentially.
A total of 98 potential participants were identified; 5 declined participation, 93 provided verbal consent for telephone contact, 3 were unable to be contacted by telephone, and 90 completed the telephone interview. This study was approved by the Toronto Rehabilitation Institute Research Ethics Board.
Sample Size
Ninety consenting individuals with SCI were divided into 2 groups based on sport exposure at the time of interview: sport participants (n = 45) and non-sport participants (n = 45). This a priori sample size of 90 with 45 persons in each group was set based upon a sample size calculation, with an anticipated mean difference of 3 in CIQ scores between the sport group and the non-sport group, and a standard deviation of 5, allowing for a P value of 0.05 and a power of 0.8.
Data Collection
Data were obtained from consenting persons via a scripted semistructured telephone interview. The interview gathered RNL; CIQ; and demographic and impairment characteristics including age (16–30 years, 31–50 years, or > 50 years); sex; ethnicity (white vs nonwhite); marital status (single, married/common law, separated/divorced, or widowed); residence (house, condo/apartment); region of residence (village or city); education (grade school, high school, college/vocational or university); employment status, both pre-SCI and current (student, full-time, part-time, unemployed, or retired); living arrangements (alone or with others); home care (yes/no); primary mode of transportation (drives, public transport/taxi, relies on others); years post-SCI; etiology of SCI (motor vehicle accident, fall, sport, gunshot wound or assault, other trauma, and nontrauma); SCI impairment (tetraplegia AIS A, tetraplegia AIS B–D, paraplegia AIS A, paraplegia AIS B–D); mobility status (manual or power wheelchair); duration of inpatient rehabilitation (0, 1–6, or > 6 months); current physiotherapy (if yes, frequency); and current medical issues (related to SCI, unrelated to SCI, and none). Data were collected prospectively; however, the pre-SCI sport participation was retrospective and the post-SCI sport participation was concurrent with the time of interview.
All data regarding sport participation were self-reported. Information pertaining to pre- and post-SCI involvement in sports included number of sports played, mode of sports, highest competitive level achieved, frequency of participation, and number of years played. Pre- and post-SCI sport participation was collected for a maximum of 3 sports per participant. Post-SCI sport participation considered only sport(s) played at the time of the interview. Pre-SCI sport participation included all previous sports played (individual or team, at least 1 to 2 times per week) up to the time of injury from childhood. However, if more than 10 years had passed between the time a person last participated in a particular sport pre-SCI and the time of injury, that sport was not considered. Participants were asked to indicate which sport they considered to be their primary sport or the most prominent in their sport participation history. Competitive sports were grouped into 3 categories: recreational (eg, participation consistent in a nonorganized sport specifically for personal enjoyment), organized competitive (eg, playing in an organized league regularly against other teams or individuals), and elite/professional (eg, competing at national level, had previously participated in international competition, or had qualified for the 2004 Paralympic Games). Frequency of sport participation was classified into 3 categories, as defined by Muraki et al (15): ≥ 3 times per week (high-active), 1 or 2 times per week (middle active), and 1 to 3 times per month (low-active). The number of years of participation in each sport was collected. Persons in the non-sport group who had participated in sports prior to their SCI were asked the reasons why they had not participated in sport following their injury.
Persons were deemed sport participants if they participated in a recreational, organized, or elite/professional sport activity (eg, planned practice, training session, sport activity or event) at least once per month at the time of the interview. Persons were considered non-sport participants if they had not regularly participated in sports since the onset of their SCI.
Outcome Measures
Community integration is commonly measured by the CIQ, developed by Willer et al (21). Although initially developed for patients with severe traumatic brain injury, the CIQ has also been used for measuring community integration among patients with SCI (19,23,24). The CIQ consists of 15 items comprising 3 subscales: home integration, social integration, and productive activity. CIQ subscale scores and total scores (out of 25) are associated with other measures of outcome post-SCI, including the Functional Independent Measure, Functional Assessment Measure, and Disability Rating Scale (23). There has been limited use of the CIQ to assess the community integration of sport participants with SCI.
The RNL (22) was developed to quantitatively assess the degree of reintegration to normal living after incapacitating illness or severe trauma. This measure assesses individuals' perception of their own capabilities in 3 dimensions: physical, social, and psychological performance (22). It consists of 11 statements scored on a 10-point visual analog scale that instructs the individual to rate how accurately the statement describes his/her situation (22). The RNL has high internal consistency, adequate interrater reliability (patient and significant other), and both convergent and discriminant construct validity when assessed against a QoL index and an index of psychological well-being (22). Several studies have used the RNL as an outcome measure to assess QoL in individuals with SCI (25–28); however, no studies have specifically used the RNL among sport participants with SCI.
Analysis
The significance for all statistical analyses was fixed at the 0.05 level of probability, unless otherwise stated. Descriptive statistics were used to summarize the sociodemographic characteristics of the sample as well as the CIQ and RNL data. Pearson chi-square tests were used to determine the similarity of demographic and injury characteristics between the 2 groups. An independent-sample t test was used to compare the CIQ and RNL mean total scores of the 2 groups. Descriptive statistics were used to describe pre-SCI and post-SCI sport participation. For the purpose of analysis, modes of sport were collapsed into 2 categories: team sports vs individual sports. Pearson correlation coefficients were calculated for the CIQ and RNL total scores in both groups (P < 0.01). Threshold values of 20 out of 25 for the CIQ total score (80%) and 88 out of 110 (80%) for the RNL total score were applied to define positive community integration and QoL, respectively. Values below these thresholds indicated poor community integration and poor QoL, respectively. Odds of pre-SCI sport participation among those with high CIQ scores were calculated using logistic regression. The unadjusted and adjusted odds ratios of pre-SCI sport participation among those with high CIQ scores were calculated using multivariate logistic regression. A single dichotomous variable (sport participation: yes = 1, no = 0) was used to predict the response (high or low CIQ score). The covariates considered were age (years), employment (yes/no), transportation (yes/no), region of residence (city/town), and sex (male/female). The odds of obtaining a high CIQ mean score after adjusting for number of sports played, mode (type) of sport(s), competitive level, frequency of participation, and number of years played were calculated.
RESULTS
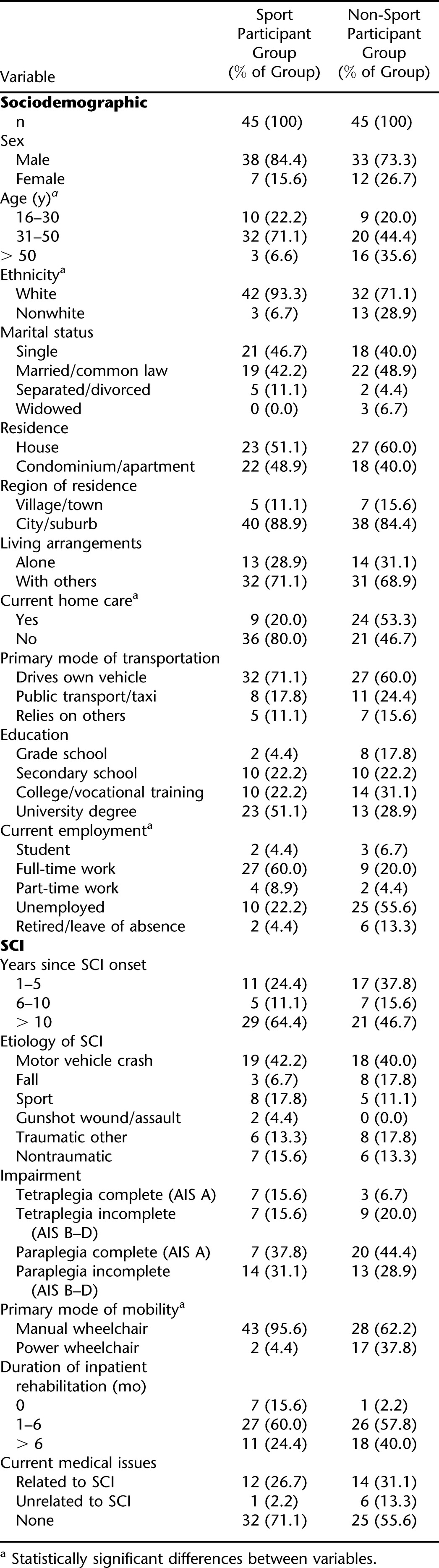
The sociodemographic and impairment characteristics of the sport participants and non-sport participants are shown in Table 1. Statistically significant differences between the 2 groups were found in age and ethnicity. The majority of participants in the sport group were white and < 50 years of age, whereas those in the non-sport group were > 50 years of age and nonwhite. Most participants in the sport group did not receive home care (n = 36, 80%), used a manual wheelchair as the primary mode of mobility (n = 43, 95.6%), and were employed full time (n = 27, 60%). In contrast, the majority of the non-sport group was receiving home care (n = 24, 53.3%) and was unemployed (n = 25, 55.6%). There were also more individuals in the non-sport group using a power wheelchair as primary mode of mobility (n = 17, 37.8%) than in the sport group. Both groups reported a prior inpatient rehabilitation stay following the onset of SCI. There were no significant difference between the sport and non-sport groups with regard to AIS level (A–D), despite the activity differences between the groups.
Table 1.
Sociodemographic Characteristics of Sport and Non-Sport Participants With SCIa
Pre- and post-SCI sport participation of both groups, including the participant's primary sport, is presented in Table 2. Eight persons (18%) in the sport group had not participated in sport pre-SCI, while 20 (44%) had played at least 3 sports prior to their injury. Of the 37 participants in the sport group who had participated in sports pre-SCI, the majority indicated that their primary sport was a team sport (n = 24, 65%); more than half reported playing at the organized competitive level (n = 19, 51%). In addition, 16 (43%) in this group had played their primary sport for more than 10 years, of whom 26 (70%) had played at a high-active frequency.
Table 2.
Sport Participation in Both Groups Pre- and Post-SCIa
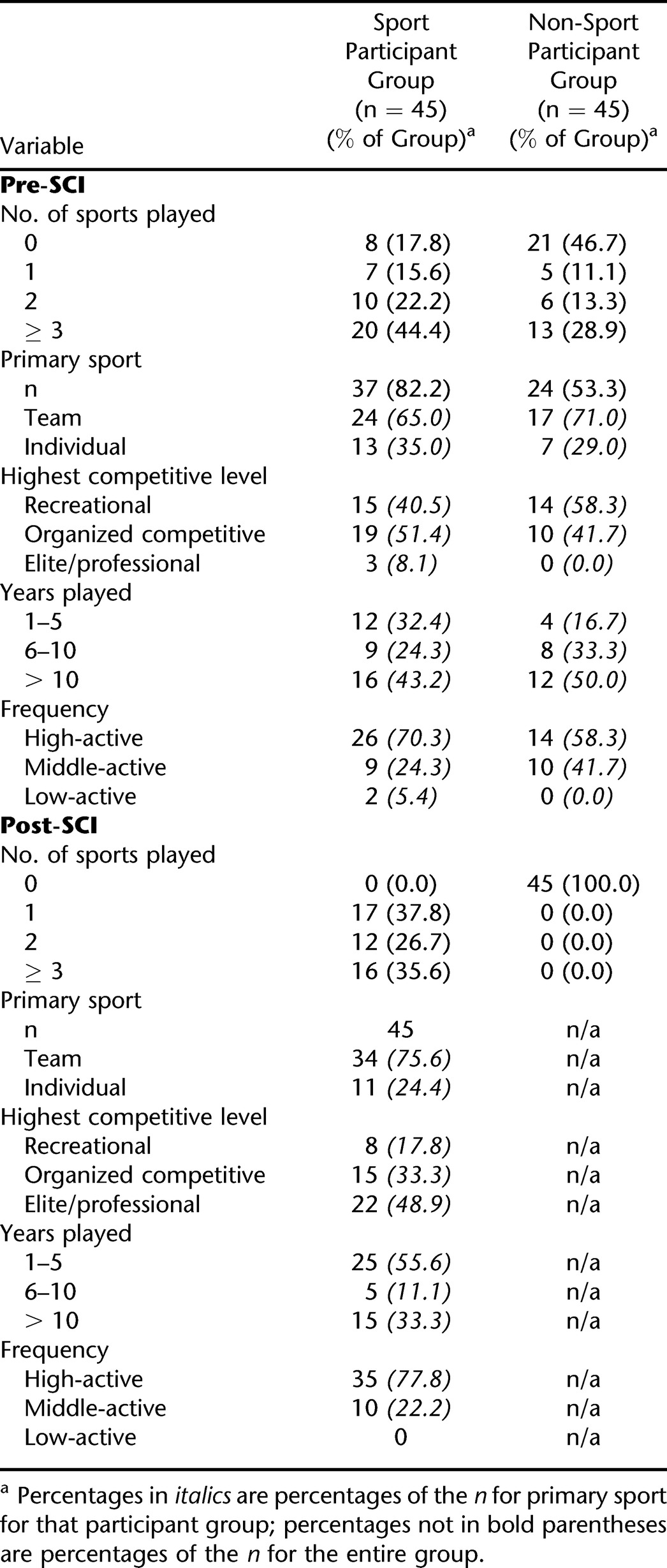
In the non-sport group, 21 persons (47%) had not participated in sports pre-SCI, whereas 13 (29%) had played at least 3 sports prior to their injury. Of the 24 participants in the non-sport group who had participated in sports pre-SCI, the majority reported their primary sport as a team sport (n = 17, 71%), with most having played at the recreational level (n = 14, 58%). Half (n = 12) of this group had played their primary sport for more than 10 years, and 14 (58%) had played at a high-active frequency.
Post-SCI, 34 persons (76%) in the sport group played team sports. Eight (18%) played their primary sport at the recreational level, 15 (33%) at the organized competitive level, and 22 (49%) at the elite/professional level. Most (n = 25, 56%) in the sport group had played their primary sport after SCI for 1 to 5 years, 5 (11%) had played between 6 and 10 years, while the majority (n = 15, 33%) had played more than 10 years. Frequency of sport participation in this group was most commonly in the high-active range, as 35 persons (78%) reported participating in their primary sport at least 3 times per week. Ten participants (22%) took part once or twice per week (middle-active), and none participated from 1 to 3 times per month (low-active).
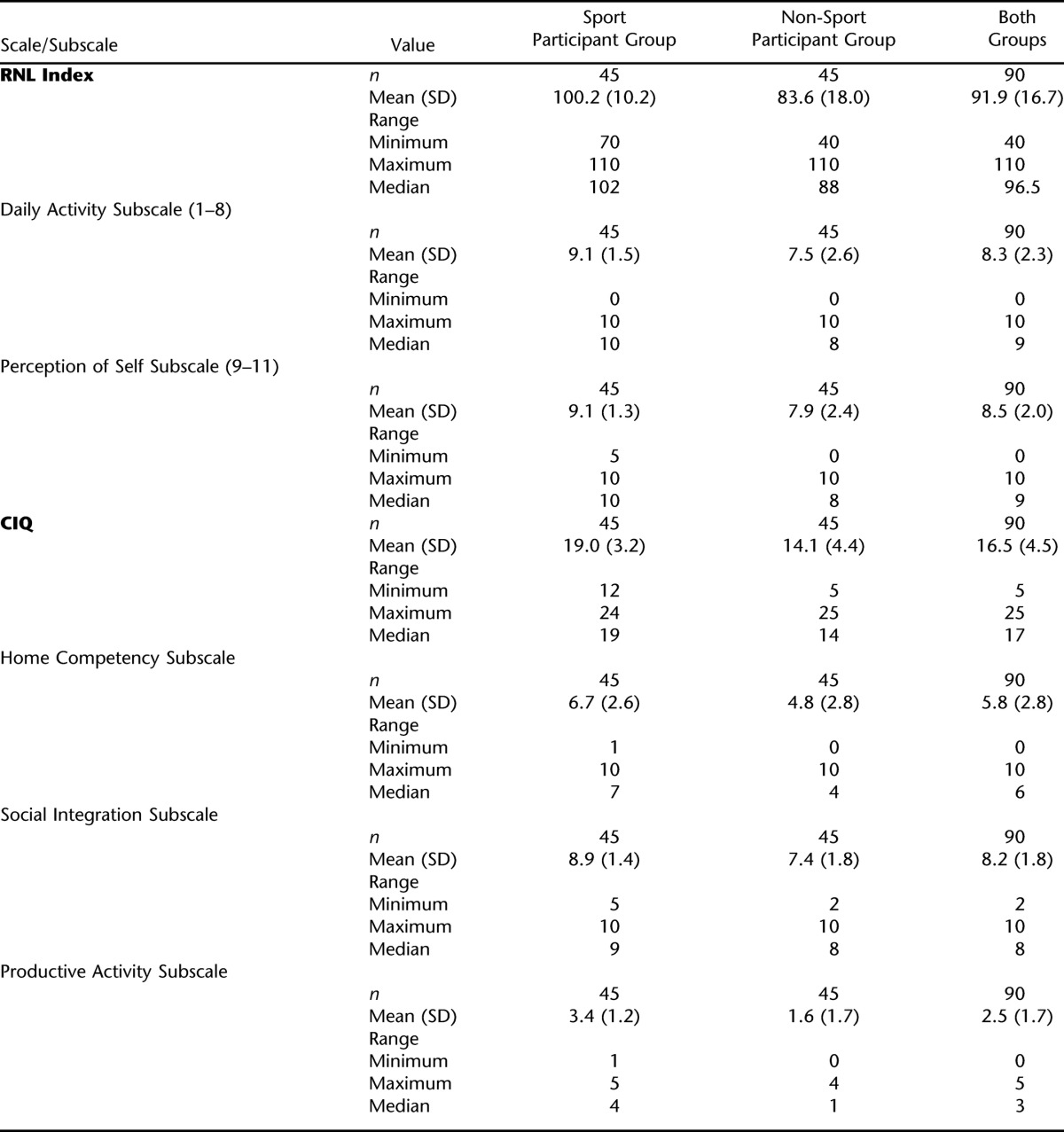
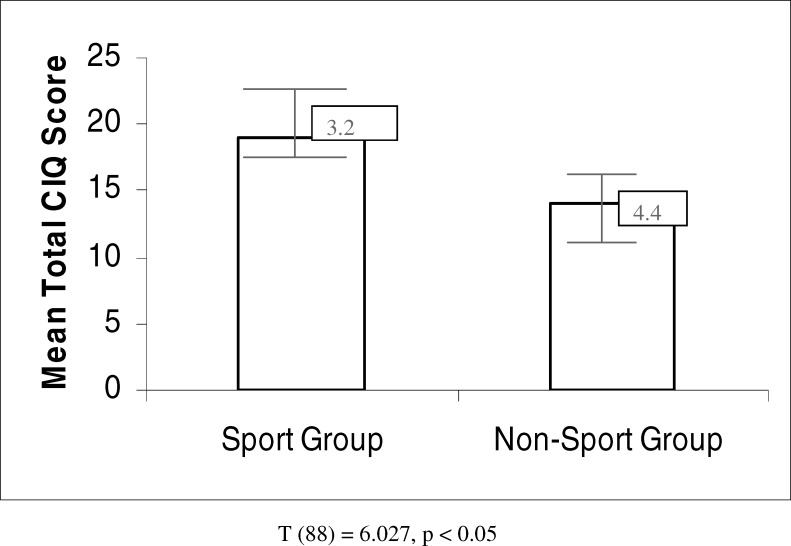
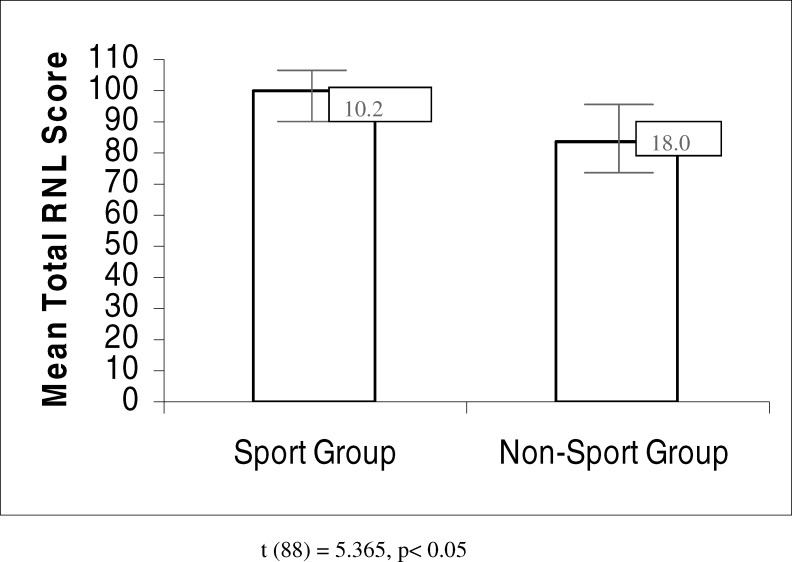
Table 3 displays the mean RNL and CIQ scores and subscale scores for both groups (see also Figures 1 and 2). The difference between CIQ total scores for the sport and non-sport groups was statistically significant (t(88) = 6.027, P < 0.05). A significant difference in RNL total scores for the 2 groups was also evident (t(88) = 5.365, P < 0.05). Notably, RNL total scores were negatively skewed, with the majority of the sample obtaining scores in the higher range (score > 90 out of a possible 110). CIQ total scores were not skewed.
Table 3.
RNL and CIQ Mean Scores and Subscores for Sport and Non-Participants With SCI
Figure 1. Mean total CIQ scores for sport participant and non-sport participant groups (t(88) = 6.027, P < 0.05).
Figure 2. Mean total RNL scores for sport participant and non-sport participant groups (t(88) = 5.365, P < 0.05).
The CIQ subscale scores for the sport group were not significantly correlated to the subscale scores of the non-sport group. The 2 RNL subscale scores for the sport group were not significantly correlated to the subscale scores of the non-sport group. The home and social subscales of the CIQ showed the largest difference in mean subscale scores between the sport and non-sport groups (t(88) = 3.27, P = 0.02; t(88) = 4.42, P = 0.00, respectively), with the sport group demonstrating the higher scores.
The odds of obtaining a high CIQ mean score were higher among those who participated in sports at the elite level, both pre- and post-SCI, compared to those who participated in sports at lower competitive levels (Exp(B) = 2.165). The odds of obtaining a high CIQ mean score were also higher among those who participated in individual sports, both pre- and post-SCI, compared to those who played team sports (Exp(B) = 1.946). There was no association between pre- and post-SCI number of sports played, frequency of sport participation, and number of years playing a sport, and the odds of a higher CIQ mean score. Pre- and post-SCI sport participation did not predict the RNL mean scores.
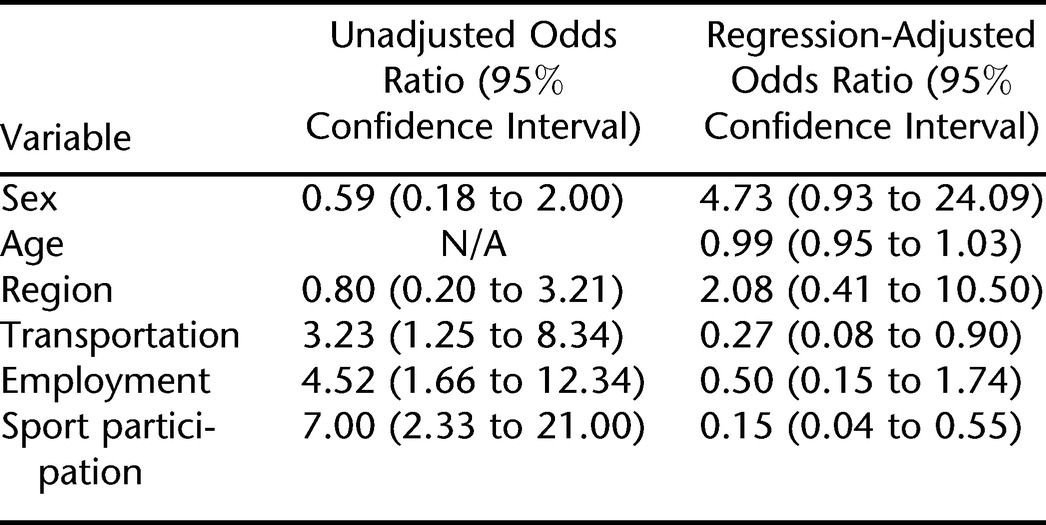
The unadjusted and adjusted odds ratios of high CIQ and high RNL scores are shown in Tables 4 and 5. Logistic regression analysis revealed that the unadjusted odds ratio of a high CIQ mean score was 4.75 (95% confidence interval [CI] 1.7, 13.5) among current sport participants. Similarly, the unadjusted odds ratio of a high RNL score was 7.00 (95% CI 2.3, 21.0) among current sport participants. The regression-adjusted odds ratios of high CIQ and RNL scores were 1.36 (95% CI 0.09, 1.45) and 0.15 (95% CI 0.04, 0.55), respectively, after adjusting for age, transportation, region of residence, and employment.
Table 4.
Unadjusted and Regression-Adjusted Odds Ratios for Participants With Low and High CIQ Scores
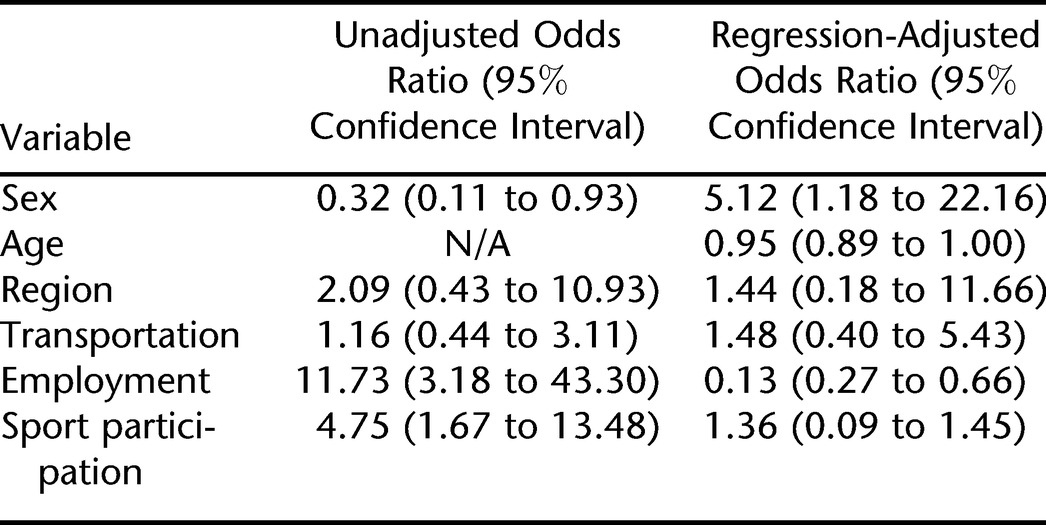
Table 5.
Unadjusted and Regression-Adjusted Odds Ratios for Participants With Low and High RNL Scores
Fifty-nine (65.6%) participants reported high pre-SCI sport participation, and 31 (34.4%) participants reported low pre-SCI sport participation. The odds ratio for pre-SCI sport participation predicting post-SCI sport participation was 3.06 (95% CI 1.23, 7.65).
When asked why they stopped playing sports after their SCI, the non-sport group reported the following reasons: lack of sports teams in their rural setting, too great a distance to travel to access sports teams, fear of further injury occurring with participation in sports, and the perception that their level of injury would prevent participation.
DISCUSSION
Participation in sports after SCI was significantly correlated with both increased community integration, as measured by the CIQ, and improved QoL, as measured by the RNL. These findings were congruent with previous studies showing a positive correlation between wheelchair sports participation and other outcomes, such as employment status, education, and community integration (18,19). With regard to community integration, the findings of the current study were consistent with those by Nemunaitis et al (19), who concluded that membership on a wheelchair basketball team was correlated with increased community integration, specifically in productivity. However, unlike the study of Nemunaitis et al, the present study included individuals playing both individual and team sports and accounted for both pre- and post-SCI sport participation. Further, the present study examined QoL to determine its relationship to community integration among the study sample through comparison of 2 distinct outcome measures (RNL and CIQ, respectively). By including a larger sample of participants in both the sport and non-sport groups, and by including a greater variety of sports, the results of this study may be generalized to a broader segment of the SCI population.
The 2 groups did not differ significantly with respect to baseline sociodemographic characteristics, with a few exceptions: the sport group was younger and more likely to be employed full time. Those in the sport group were also more likely to be using a manual wheelchair as the primary mode of mobility and not receiving home care at the time of the interview, compared to the non-sport group. The non-sport group had a higher rate of power wheelchair use, was more likely to have had an inpatient rehabilitation stay of at least 6 months, and reported an increased frequency of home care. These baseline characteristics are consistent with those found in the literature, which indicate that sport participants with SCI tend to be younger, are more likely to be employed and to report higher incomes, and are less likely to have sustained cervical injuries (17). This latter characteristic of sport participants with SCI in the literature would explain the present study's finding of preponderant use of a manual rather than power wheelchair, a shorter duration of inpatient rehabilitation, and a decreased need for home care in the sport group compared to the non-sport group. However, some of the differences in the baseline characteristics of the groups in the current study may be a limitation. The study findings that the sport group was younger and more likely to be employed full time than the non-sport group was at baseline may reflect that the sport group had a higher level of community integration prior to the study, including participation in sports. A majority of the sport group had participated in sports pre-SCI, while almost half of those in the non-sport group had not participated in sports pre-SCI. This suggests that those involved in sports pre-SCI were more likely to continue to participate in sports post-SCI, and that pre-morbid sport participation may be a predictor of community integration. Additionally, pre-SCI sports participation was found to predict post-SCI sports participation. Furthermore, sports participation pre-SCI demonstrated a trend toward the organized competitive level in the sport group, whereas in the non-sport group, most reported participation in recreational sports pre-SCI. These findings would suggest that those who were less competitive in sport pre-SCI were less likely to pursue sport participation following SCI.
The finding that there was no significant difference in the levels of injury at baseline between the 2 groups was not consistent with that found in the literature. From the published literature, one would anticipate that the sport group would have had a higher number of individuals with paraplegia compared to the non-sport group, which would have been expected to have a higher number of individuals with tetraplegia. This lack of statistically significant difference in neurological level between the groups may be related to the relatively lower number of total participants with tetraplegia compared to those with paraplegia in this cohort. Had there been a greater number of participants with tetraplegia, the difference in levels of injury between the 2 groups may have been significant.
The responses of the non-sport group underscore the need for more sports programs in rural areas and/or increased access through transportation to the areas that do have sports programs. Increased education at the time of inpatient rehabilitation and at outpatient follow-up visits about the potential for sports participation regardless of impairment (paraplegia or tetraplegia) would likely result in heightened interest in sports and improved perception of one's capability to participate in sports after SCI. Increased participation in sports facilitated by increased patient awareness of sporting opportunities may contribute to improvement of rehabilitation outcomes such as community integration and QoL.
With respect to the CIQ subscales, the home and social subscales showed the largest difference in mean subscale scores between the sport and non-sport groups. This suggests that these subscales have the greatest discriminant ability to identify a difference in community integration between sport participants and non-sport participants, and they should be specifically used in future studies evaluating community integration among SCI sporting participants. Only one prior study in the literature has examined CIQ subscale scores in this population; however, subscale scores were not compared between individuals with SCI who did and did not participate in sports. Nemunaitis et al (19) concluded that the productivity subscale scores of the CIQ were the most significantly correlated with increased community integration in those individuals with SCI who were members of a wheelchair basketball team.
Participation at higher competitive levels and participation in individual sports, both pre- and post-SCI, were associated with increased CIQ total scores. It is possible that the greater community integration seen in those participating at higher competitive levels was emphasized by an increased physical ability that allowed these individuals to participate at a higher competitive level and consequently also to have increased integration into the community. Alternatively, sport participation at higher competitive levels may be associated with improved community integration because of the psychological benefits of sports, eliciting further physical adaptation. This was the finding of Muraki et al (15), who determined that the psychological benefits of sporting activity became more prominent when sport participation frequency exceeded 3 times per week. The present study did not find that frequency of sport participation influenced community integration, but it did suggest that participation in higher competitive levels of sports correlated with higher community integration. The finding that sport participation both before and after injury influenced CIQ total scores suggests that both pre- and post-SCI sports participation of an individual must be taken into account when examining the relationship between sports participation and community integration.
Comparison of individual vs team sports and their associations with community integration has not been done in prior studies. In the related investigation that compared the psychological benefits of these different modes of sport (wheelchair basketball, wheelchair tennis, wheelchair racing, and minor modes of sport such as archery and wheelchair table tennis), Muraki et al (15) failed to find differences in psychological variables among these modes of sport activity. Interestingly, the current study found that, of those in both participant groups who had participated in sport pre-SCI, the majority had participated in team sports; however, it was participation in individual sports both pre- and post-SCI that resulted in increased community integration.
Other limitations of the present study include that the majority of the sport group in our sample was involved in sports at the elite level. This may not be an accurate representation of the true extent of sports involvement in the SCI population. Further prospective studies that include stratification based on competitive level are needed to discern whether the association between sports and community integration remains positive across the continuum from recreational to elite sports.
This study likely has a recruitment bias, given that the non-sport group was recruited entirely from outpatient clinics, which may have affected their interview responses, whereas approximately only 30% of the sport group was recruited from outpatient clinics. There is also an element of sampling bias, given that 76% of the sport participant group participated in team sports. The possibility of interviewer bias is also valid, given that the interviewer was the primary investigator of this study with an interest in the value of sport participation.
The choice of 80% as the threshold value for both the CIQ to define positive community integration and for the RNL to define positive QoL was arbitrary, based upon review of the literature and clinician experience. Review of the literature reveals a lack of validation of such threshold values, and thus the threshold values implemented in this study remain arbitrary. Although such simple cut-off threshold scores are useful for identifying associations for positive community integration and QoL, the authors recognize that both community integration and QoL are complex phenomena. Further research is needed to validate these threshold values. Another limitation of this study is that self-reported answers in an interview format can introduce bias; participants may have given answers that they saw as most acceptable to the interviewer or answered as they perceived themselves as achieving, rather than a true reflection of their circumstance. Further, the medical and impairment data collected in this study were self-reported by each participant and were not verified for accuracy.
CONCLUSION
The results of this study indicate that participation in sports after SCI is associated with increased community integration and QoL. Participation in sports should be recognized as an adjunct to current SCI rehabilitation programs, with the potential to contribute to improved rehabilitation outcomes. Pre- and post-SCI sport participation at higher competitive levels and participation in individual sports were associated with increased community integration. Although an individual's pre-SCI sport participation cannot be controlled, this study suggests that the recognition of pre-SCI sport participation can be flagged during the rehabilitation process and be used to assist in promotion of post-SCI sport participation and subsequently possibly contribute to increased community integration.
REFERENCES
- International Society of Sport Psychology. Physical activity and psychological benefits: a position statement. Sport Psychologist. 1992;6(2):199–203. [Google Scholar]
- Roth DL, Holmes DS. Influence of physical fitness in determining the impact of stressful life events on physical and psychological health. Psychosom Med. 1985;47(2):164–173. doi: 10.1097/00006842-198503000-00008. [DOI] [PubMed] [Google Scholar]
- Roth DL, Holmes DS. Influence of aerobic exercise training and relaxation training on physical and psychological health following stressful life events. Psychosom Med. 1987;49(4):355–365. doi: 10.1097/00006842-198707000-00004. [DOI] [PubMed] [Google Scholar]
- Morgan WP, Roberts JA, Brand FR, Finerman AD. Psychological effect of chronic physical activity. Med Sci Sports Exerc. 1970;2(4):213–217. [PubMed] [Google Scholar]
- Martinsen EW. Benefits of exercise for the treatment of depression. Sports Med. 1990;9(6):380–389. doi: 10.2165/00007256-199009060-00006. [DOI] [PubMed] [Google Scholar]
- Campbell E, Jones G. Psychological well-being in wheelchair sport and non-participants. Adapt Phys Activ Quart. 1994;11(4):404–415. [Google Scholar]
- Greenwood CM, Dzewaltowski DA, French R. Self-efficacy and psychological well-being of wheelchair tennis participants and wheelchair non-tennis participants. Adapt Phys Activ Quart. 1990;7(1):12–21. [Google Scholar]
- Paulsen P, French R, Sherrill C. Comparison of wheelchair athletes and non-athletes on selected mood states. Percept Mot Skills. 1990;71((3 Pt 2)):1160–1162. doi: 10.2466/pms.1990.71.3f.1160. [DOI] [PubMed] [Google Scholar]
- Paulsen P, French R, Sherrill C. Comparison of mood states of college able-bodied and wheelchair basketball players. Percept Mot Skills. 1991;73(2):396–398. doi: 10.2466/pms.1991.73.2.396. [DOI] [PubMed] [Google Scholar]
- Monazzi G. Paraplegics and sport: a psychological survey. Int J Sport Psychol. 1982;13(2):85–95. [Google Scholar]
- Slater D, Meade MA. Participation in recreation and sports for persons with spinal cord injury: review and recommendations. NeuroRehabilitation. 2004;19(2):121–129. [PubMed] [Google Scholar]
- Tasiemski T, Kennedy P, Gardner B, Taylor N. The association of sports and physical recreation with life satisfaction in a community sample of people with spinal cord injuries. NeuroRehabilitation. 2005;20(4):253–265. [PubMed] [Google Scholar]
- Hopper CA. Socialization of wheelchair athletes. In: Sherrill C, editor. The 1984 Olympic Scientific Congress Proceedings. Champaign, IL: Human Kinetics Publishers; 1984. pp. 197–202. [Google Scholar]
- Campbell E. Psychological well-being of participants in wheelchair sports: comparison of individuals with congenital and acquired disabilities. Percept Mot Skills. 1995;81(2):563–568. doi: 10.1177/003151259508100241. [DOI] [PubMed] [Google Scholar]
- Muraki S, Tsunawake N, Hiramatsu S, Yamasaki M. The effect of frequency and mode of sports activity on the psychological status in tetraplegics and paraplegics. Spinal Cord. 2000;38(5):309–314. doi: 10.1038/sj.sc.3101002. [DOI] [PubMed] [Google Scholar]
- Gioia M, Cerasa A, Lucente A, Brunelli S, Castellano V, Traballesi M. Psychological impact of sports activity in spinal cord injury patients. Scand J Med Sci Sports. 2006;16(6):412–416. doi: 10.1111/j.1600-0838.2005.00518.x. [DOI] [PubMed] [Google Scholar]
- Foreman PE, Cull J, Kirkby RJ. Sports participation in individuals with spinal cord injury: demographic and psychological correlates. Int J Rehabil Res. 1997;20(2):159–168. doi: 10.1097/00004356-199706000-00005. [DOI] [PubMed] [Google Scholar]
- Tasiemski T, Bergstrom E, Savic G, Gardner B. Sports, recreation and employment following spinal cord injury—a pilot study. Spinal Cord. 2000;38(3):173–184. doi: 10.1038/sj.sc.3100981. [DOI] [PubMed] [Google Scholar]
- Nemunaitis G, Haines M, Rizk T, Clark G. The community integration of wheelchair athletes [abstract] J Spinal Cord Med. 2003;26((suppl 1)):S35. [Google Scholar]
- Dijkers M. Community integration: conceptual issues and measurement approaches in rehabilitation research. Top Spinal Cord Inj Rehabil. 1998;4(1):1–17. [Google Scholar]
- Willer B, Rosenthal M, Kreutzer JS, Gordon WA, Rempel R. Assessment of community integration following rehabilitation for traumatic brain injury. J Head Trauma Rehabil. 1993;8(2):75–87. [Google Scholar]
- Wood-Dauphinee SL, Opzoomer A, Williams JI, Marchand B, Spitzer WO. Assessment of global function: the reintegration to normal living index. Arch Phys Med Rehabil. 1988;69(8):583–590. [PubMed] [Google Scholar]
- Sander AM, Fuchs KL, High WM, et al. The Community Integration Questionnaire revisited: an assessment of factor structure and validity. Arch Phys Med Rehabil. 1999;80(10):1303–1308. doi: 10.1016/s0003-9993(99)90034-5. [DOI] [PubMed] [Google Scholar]
- Johnston M, Nissim EN, Wood K, Hwang K, Tulsky D. Objective and subjective handicap following spinal cord injury: interrelationships and predictors. J Spinal Cord Med. 2002;25(1):11–22. doi: 10.1080/10790268.2002.11753596. [DOI] [PubMed] [Google Scholar]
- Daverat P, Petit H, Kemoun G, Dartigues JF, Barat M. The long-term outcome in 149 patients with spinal cord injury. Paraplegia. 1995;33(11):665–668. doi: 10.1038/sc.1995.139. [DOI] [PubMed] [Google Scholar]
- Harker WF, Dawson DR, Boschen KA, Stuss DT. A comparison of independent living outcomes following traumatic brain injury and spinal cord injury. Int J Rehabil Res. 2002;25(2):93–102. doi: 10.1097/00004356-200206000-00003. [DOI] [PubMed] [Google Scholar]
- May LA, Warren S. Measuring quality of life of persons with spinal cord injury: external and structural validity. Spinal Cord. 2002;40(7):341–350. doi: 10.1038/sj.sc.3101311. [DOI] [PubMed] [Google Scholar]
- Calmels P, Bethoux F, Roche G, Fayolle-Minon I, Picano-Gonard C. Evaluation of the handicap and the quality of life in spinal cord injuries: study in a population of 58 patients living at home [in French] Ann Readapt Med Phys. 2003;46(5):233–240. doi: 10.1016/s0168-6054(03)00084-9. [DOI] [PubMed] [Google Scholar]