Abstract
Injectable local anesthetics that would last for many days could have a marked impact on periprocedural care and pain management. Formulations have often been limited in duration of action, or by systemic toxicity, local tissue toxicity from local anesthetics, and inflammation. To address those issues, we developed liposomal formulations of saxitoxin (STX), a compound with ultrapotent local anesthetic properties but little or no cytotoxicity. In vitro, the release of bupivacaine and STX from liposomes depended on the lipid composition and on whether dexamethasone was incorporated. In cell culture, bupivacaine, but not STX, was myotoxic (to C2C12 cells) and neurotoxic (to PC12 cells) in a concentration- and time-dependent manner. Liposomal formulations containing combinations of the above compounds produced sciatic nerve blockade lasting up to 7.5 days (with STX + dexamethasone liposomes) in male Sprague–Dawley rats. Systemic toxicity only occurred where high loadings of dexamethasone increased the release of liposomal STX. Mild myotoxicity was only seen in formulations containing bupivacaine. There was no nerve injury on Epon-embedded sections, and these liposomes did not up-regulate the expression of 4 genes associated with nerve injury in the dorsal root ganglia. These results suggest that controlled release of STX and similar compounds can provide very prolonged nerve blocks with minimal systemic and local toxicity.
Keywords: liposomes, myotoxicity, neurotoxicity, pain, saxitoxin
The development of local anesthetics to provide prolonged analgesia from a single injection has encountered 3 principal challenges: inadequate duration of action, systemic toxicity, and adverse local tissue reaction. The purpose of this research was to produce a local anesthetic lasting many days without those detrimental sequelae.
A wide variety of controlled-release technologies has been used to extend the duration of nerve block, but most such systems result at best in a several-fold extension of duration compared with unencapsulated drugs. Approaches that encapsulate synergistic drug combinations have achieved nerve blocks lasting many days. For example, coencapsulation of bupivacaine and dexamethasone in polymeric microspheres produced nerve blocks lasting >4 days (1). Coencapsulation of site 1 sodium-channel blockers [tetrodotoxin (TTX), saxitoxin (STX), etc., which block the sodium channel at site 1 on the outer surface] with conventional local anesthetics also greatly prolonged sciatic nerve blockade. Addition of dexamethasone prolonged the sciatic nerve blockade to >9 days in the rat when dexamethasone was added (2). However, tissue reaction to such formulations has been problematic. Conventional local anesthetics are intrinsically myotoxic (3, 4). They are also myotoxic when released from a wide range of delivery systems (3, 5), even when the delivery systems themselves are minimally toxic. The myotoxicity of bupivacaine increases dramatically over extended durations of exposure (3), suggesting that myotoxicity may be an inevitable consequence of sustained release of such compounds. Conventional local anesthetics are also neurotoxic (6, 7). The presence of particles themselves enhances local anesthetic myotoxicity in vivo (3), and can cause inflammatory responses at the nerve that may considerably outlast the duration of blockade (2, 3, 8). In contrast, site 1 sodium-channel blockers do not cause myo- or neurotoxicity (9, 10), which would make them desirable for an extended release formulation. However, these extremely potent local anesthetics (11), being very hydrophilic, are difficult to encapsulate effectively in polymeric particles, and the systemic toxicity from their initial rapid release is dose-limiting (12, 13). These considerations make the development of particulate systems based entirely on such compounds (i.e., without inclusion of conventional local anesthetics) very difficult.
Here, we developed prolonged duration local anesthetics based entirely on site 1 sodium-channel blockers, the hypothesis being that there would be less harm to local tissue. To allow increased loading without systemic toxicity, we used liposomes, which are biocompatible microscopic lipid vesicles with a bilayer membrane structure that have been used to deliver hydrophilic, amphiphilic, and hydrophobic drugs. In this report, those are STX, bupivacaine, and dexamethasone, respectively. STX was used as the model site 1 sodium-channel blocker due to its greater availability to us; other site 1 sodium-channel blockers may also have been suitable (11). The resulting formulation produced nerve blocks lasting many days in the rat, with minimal local or systemic toxicity and inflammation.
Results
Liposomal Formulations.
Liposomes were produced with 1,2-dimyristoyl-sn-glycero-3-phosphocholine (DMPC) and 2-dimyristoyl-sn-glycero-3-phosphglycerol (DMPG), or 1,2-distearoyl-sn-glycero-3-phosphocholine (DSPC) and 1,2-distearoyl-sn-glycero-3-phosphatidylglycerol (DSPG). Those made with DMPC are referred to as “fluid” liposomes below; those with DSPC as “solid,” based on their phase transition temperatures (Tm). Particles were loaded with bupivacaine, STX, and/or dexamethasone (Table S1).
The median volume-weighted diameters of both fluid and solid liposomes were ≈4.0 μm, with median zeta potentials of ≈−35 mV, irrespective of drug content (Table S1). The mean encapsulation efficiencies of bupivacaine in solid and fluid liposomes were 64 and 60%, respectively. The liposomal drug loadings, in mg/mL, were 8.7–10.2 for bupivacaine (i.e., ≈1% wt/vol), 0.03–0.018 for STX, and 50–60 for lipids.
In Vitro Drug Release.
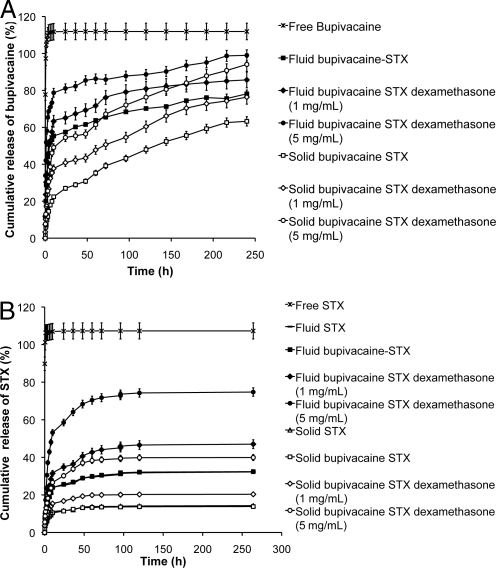
To assess the potential of these liposomes to provide sustained nerve blockade, we performed release kinetic studies at 37 °C. All liposome formulations significantly increased the duration of bupivacaine release, compared with free bupivacaine (e.g., P < 0.001 at 50 h; Fig. 1A). Fluid particles showed faster (e.g., P < 0.05 at 50 h) release than solid ones. Release of bupivacaine was increased in proportion to the amount of dexamethasone incorporated (e.g., P < 0.05 when comparing 0 to 5 mg/mL dexamethasone at 50 h). Dexamethasone release was not affected by lipid type (Fig. S1). However, particles with a higher proportion of dexamethasone (5 mg/mL) showed slower release of dexamethasone on a percentage basis, particularly at later time points (e.g., P < 0.05 when comparing 1 to 5 mg/mL dexamethasone at 50 h). Fluid liposomes showed more rapid release of STX (Fig. 1B) than did solid ones (P < 0.05 at all time points, and <0.001 after 50 h), and dexamethasone accelerated STX release (P < 0.05). These results, which showed sustained release of the compounds of interest for several days, supported their potential to provide prolonged duration local anesthesia.
Fig. 1.
Cumulative release of total encapsulated bupivacaine (A) and STX (B) from liposomes in vitro. Data are means with SDs (n = 4). Statistical significance is discussed in the text.
Stability.
At 4 °C, both solid and fluid liposomes (containing all compounds, singly and in combination) were stable for 2 weeks: drug leakage was <3% over that period, and there was no significant change in liposome size, zeta potential, and drug to lipid ratio. At 21 °C, particles made with both lipid compositions showed >10% release of bupivacaine in 48 h, i.e., they were not stable. Release of STX and dexamethasone were slower than for bupivacaine, but still higher than at 4 °C.
Cytotoxicity.
One of the underlying hypotheses of this work was that prolonged exposure to STX would cause less injury to muscle and nerve than bupivacaine. Before animal studies, we investigated this matter in cell culture.
Myotoxicity.
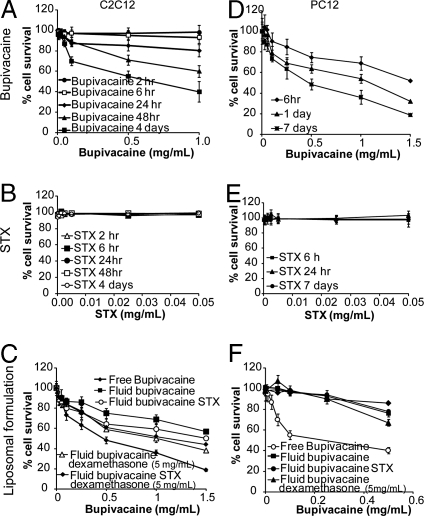
Myotoxicity was assessed by exposing C2C12 cells for up to 4 days to a range of concentrations of free compounds (bupivacaine, dexamethasone, or STX), or liposomes with varying drug contents and lipids compositions. Myotoxicity of bupivacaine solution increased with concentration and duration of exposure (Fig. 2A) (3). In contrast, free STX (0.005–0.05 mg/mL) was not myotoxic at any of the concentrations or any durations of exposure tested (e.g., P < 0.001, 0.01 vs. 0.05 mg/mL at 48 h, and P < 0.001 at 0.1 mg/mL at 6 vs. 24 h; Fig. 2B). This concentration range vastly exceeds that required to achieve effective sciatic nerve blockade (11). Free dexamethasone (0.005–0.5 mg/mL), singly or in combination with the highest STX concentration (0.05 mg/mL), was not myotoxic at up to 2 days (viability >90%). At day 4, survival was reduced to 80 ± 5% (P < 0.05) with 0.5 mg/mL free dexamethasone. This reduction in survival did not occur when the dexamethasone was encapsulated in liposomes.
Fig. 2.
Percentage of C2C12 and PC12 cell survival after exposure to free bupivacaine (A and D), free STX (B and E), and fluid liposomes encapsulating combinations of bupivacaine, dexamethasone and/or STX (C and F). In C and F, data for free bupivacaine are reproduced from A and D for comparison. Data are means with SDs (n = 4). For complete particle compositions, see Table S1.
Blank liposomes were not toxic to cells at concentrations from 0.3 to 6 mg/mL of lipids. Further increasing the lipids reduced cell viability [e.g., viability was 50% at 9 mg/mL (P < 0.001)]. Coadministration of empty liposomes with free drugs did not further reduce cell viability.
Liposomal bupivacaine caused less myotoxicity than the same concentration of free bupivacaine (e.g., P < 0.001 at 0.5 mg/mL at 4 days; Fig. 2C). Myotoxicity increased with concentration and duration of exposure (Fig. 2C). Liposomes containing STX, dexamethasone, or combinations of both were not myotoxic at any concentration (0–1 mg/mL STX), exposure up to 4 days, or lipid composition. Encapsulation of dexamethasone within bupivacaine liposomes increased toxicity (e.g., P < 0.05 at 0.5 mg/mL at 4 days; Fig. 2C), possibly due to the more rapid release of bupivacaine (Fig. 1). Addition of STX did not increase the myotoxicity of any liposome formulation tested (Fig. 2C).
Neurotoxicity.
Similar studies were performed in PC12 cells (a pheochromocytoma cell line frequently used in neurotoxicity studies) (14). Neurotoxicity of bupivacaine solution increased with concentration and duration of exposure (Fig. 2D). Free or encapsulated STX (0.005–0.05 mg/mL) was not neurotoxic at any concentration or duration of exposure (Fig. 2E), nor was free or encapsulated dexamethasone (0.005–0.05 mg/mL) for up to 5 days. Free dexamethasone (0.05 mg/mL) showed a 20% decrease in survival at day 7. Blank solid and fluid liposomes were not toxic at concentrations from 0.3 to 9 mg/mL. Incorporation of STX into fluid bupivacaine liposomes did not increase their cytotoxicity (Fig. 2F), but incorporation of dexamethasone into bupivacaine liposomes did (e.g., P < 0.01 at 0.5 mg/mL Fig. 2F), possibly due to the more rapid release of bupivacaine (Fig. 1). Similar results were obtained with solid liposomes.
These studies showed that extended exposure to STX-based formulations caused little cytotoxicity, and that therefore the liposomes were good candidates for in vivo use.
Duration of Nerve Blockade.
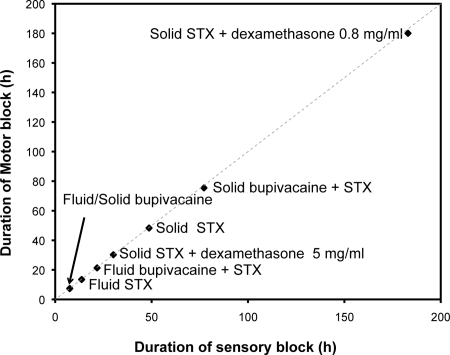
To test the ability of liposomal formulations to produce prolonged nerve blockade and systemic toxicity (increases in latency in the un-injected hindlimb, respiratory distress, and death), rats were injected at the sciatic nerve with 0.6 mL of liposome formulations (8 rats per formulation), containing single compounds or combinations. All liposome formulations containing bupivacaine or STX induced motor and sensory nerve block that subsequently reverted to baseline values. Onset of nerve blockade occurred 10–15 min after injection with fluid liposomes, and 0.5–1.5 h after injection with solid liposomes. The durations of sensory and motor blocks are shown in Fig. 3 and were similar in all cases.
Fig. 3.
Duration of sensory and motor block in animals injected with liposomes containing STX and/or bupivacaine and dexamethasone. Data are means with SDs (n = 8). The dotted line denotes identical durations of sensory and motor block.
A primary goal of this research was to develop injectable formulations that could achieve reliable and prolonged nerve blockade with STX, or at least without bupivacaine. Polymeric microspheres with TTX alone had been ineffective (2). Nerve blockade from fluid liposomes containing STX alone lasted ≈13.5 h. Solid liposomes containing STX alone produced even longer blocks, lasting 48 h, with no signs of systemic toxicity.
We verified that the drug interactions that extended the duration of block in polymeric particles containing TTX (2) also occurred with STX liposomes. The incorporation of some concentrations of dexamethasone into STX liposomes caused marked systemic toxicity and death, presumably because dexamethasone increased liposome permeability to other compounds (Fig. 1). For example, STX-containing fluid liposomes with 5 mg/mL of dexamethasone were uniformly fatal, but liposomes containing the same quantities of STX or dexamethasone alone were not toxic. In solid liposomes, coencapsulation of dexamethasone at 5 mg/mL reduced the duration of block compared with STX (0.031 mg/mL) liposomes (P < 0.01), and 2 of 8 animals died. In contrast, dexamethasone at 0.8 mg/mL led to a marked 3.7-fold increase in the duration of nerve blockade (P < 0.001), to 180 h or 7.5 days, with no signs of systemic toxicity.
Coencapsulation of bupivacaine in fluid STX liposomes extended block by 60% to 21.24 h (P < 0.001), which was approximately the sum of the block durations of the singly encapsulated compounds (block from bupivacaine fluid liposomes was 7.3 h). In solid liposomes, coencapsulation of bupivacaine increased the block duration of STX particles by 56% (P < 0.001), which was more than the sum of the durations of block of the individually encapsulated compounds (block from solid bupivacaine liposomes was 7.4 h.). There were no signs of systemic toxicity from those formulations.
Empty liposomes and dexamethasone liposomes did not produce nerve blockade during serial testing for 24 h. No animals developed autotomy (self-injury) of their hind paws.
Necropsy and Histology.
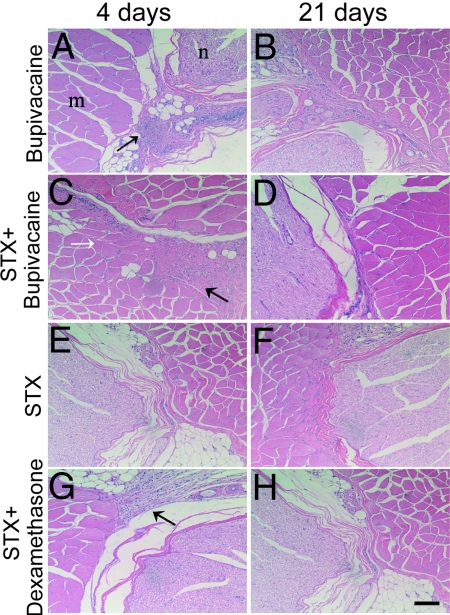
To assess tissue reaction, animals from nerve block experiments were killed 4, 14, and 21 days after injection (n = 3 at each time point), if nerve block had resolved. The sciatic nerve and surrounding tissues were harvested, and processed for histology by hematoxylin-eosin staining.
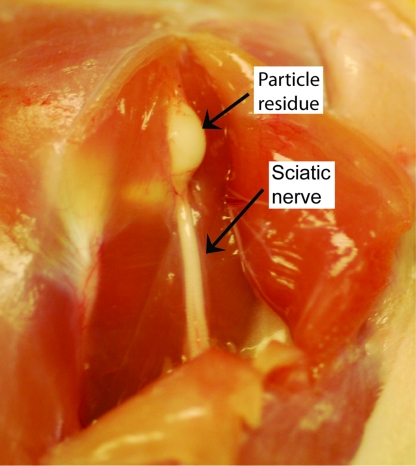
In all cases, liposomes were still seen on gross dissection as a whitish material on the sciatic nerve site at day 4 after injection (Fig. 4). Tissues had a benign appearance, with little matting or apparent inflammation. Microscopic examination of these tissues revealed mild to moderate lymphohistiocytic inflammation along the surface of the tissue at 4 days after injection in all samples (Fig. 5), which dissipated in all cases by 21 days postinjection. Animals injected with bupivacaine liposomes showed a small number of muscle fibers with nuclear centralization (very mild injury); one had a small area of focal fibrosis. In all other cases, the inflammation did not infiltrate muscle and nerve tissue, and there was no evidence of muscle or nerve damage. Individual particles could not be discerned. Because hematoxylin/eosin-stained sections are insensitive for identifying nerve injury, we obtained Epon-embedded sections in 3 animals in each group. Those sections did not reveal nerve injury from any formulation at any time point.
Fig. 4.
Representative photograph of particle residue (here, with solid STX + dexamethasone liposomes) at the site of injection 4 days after injection. Residue appearance was similar in all particle types. Microscopic appearance is shown in Fig. 5.
Fig. 5.
Representative light microscopy of hematoxylin/eosin-stained sections of nerves (n), muscles (m), and surrounding tissues at the site of injection, 4 and 21 days after injection with liposomal formulations: bupivacaine (A and B), bupivacaine plus STX (C and D), STX alone (E and F), or STX plus dexamethasone (G and H). All injected animals showed mild to moderate lymphohistiocytic inflammation (solid arrow) that dissipated by 21 days. An animal injected with bupivacaine showed focal fibrosis of connective tissue surrounding the muscle, and central nucleation in a few muscle fibers (open arrow) 4 days after injection, indicating mild muscle injury. Magnification 200×. (Scale bar, 100 μm.)
Real-Time PCR.
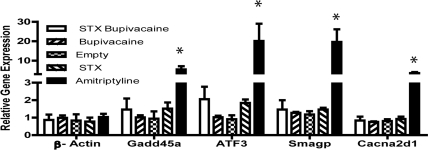
To further assess the presence or absence of nerve injury 4 days after injection, we used real time PCR to study the expression of 4 genes [Gadd45a (15), ATF3 (16, 17), SmagP (18), and Cacna2d1 (19, 20)] whose expression is altered by nerve injury, using RNA from the dorsal root ganglia of animals that received nerve blocks (n = 4 in each group). As a positive control for local anesthetic-associated nerve injury that would be relevant to the formulations used here, 4 animals were given sciatic nerve blocks with 80 mM amitriptyline, a tricyclic antidepressant with local anesthetic properties that resembles bupivacaine in structure and mechanism of action (21), and that causes severe myotoxicity and neurotoxicity (22, 23). Expression was normalized to GAPDH as an internal control; β-actin was chosen as another gene whose expression should not change with nerve injury. All 4 selected genes were dramatically up-regulated in amitriptyline-treated animals 4 days after injection, compared with saline-treated controls (P < 0.001; Fig. 6). In contrast, these genes were not up-regulated by any of the liposomal treatments.
Fig. 6.
Real-time PCR of mRNA from dorsal root ganglia from animals injected with liposomes (empty or containing test compounds), or a toxic concentration of amitriptyline; n = 3 for each treatment. ∗, P < 0.001, in the comparison of amitriptyline treatment with all liposomal treatments.
Discussion
We have developed a set of drug delivery systems containing the site 1 sodium-channel blocker STX, which can produce prolonged nerve blockade without local toxicity, and, in most formulations, without systemic toxicity. They did not require synergistic compounds such as bupivacaine and dexamethasone, although block duration was greatly extended by their use. For example, incorporation of dexamethasone produced blocks lasting >7 days without any systemic toxicity detectable by our neurobehavioral testing methods and clinical examination (2). This prolonged blockade from STX-only liposomes was in contrast to our experience with polymeric microspheres containing TTX, where particles with the highest nontoxic dose of TTX alone produced a median duration of block of 0 min, and addition of dexamethasone prolonged their duration of block to only 8 h. Polymeric microspheres containing TTX also had to be injected with epinephrine to avoid systemic toxicity.
Also, none of the animals developed autotomy (self-injury) of their hindpaws (24), a behavior associated with pain (although that association is controversial), and seen with high prevalence in prolonged blocks from TTX-bupivacaine-dexamethasone polymeric microspheres (2). Importantly for the potential clinical applicability of prolonged duration local anesthetics, the lack of autonomy here suggests that it is not an unavoidable concomitant of prolonged nerve blockade. It is not clear why autotomy was not seen here. Differences between the liposomes and PLGA particles per se would be expected to have effects at the site of injection at the hip, whereas autotomy occurs at the paw (24).
Liposomes have previously been used for controlled release of conventional anesthetics (25–27). Bupivacaine liposomes provide skin analgesia lasting 14–29 h in a mouse model (28), and 42 h in humans (25). Liposomal formulations of various local anesthetics have been used in rat infraorbital nerve blockade, with durations of 65–110 min (29, 30). Block from the bupivacaine liposomes used here lasted 7 h.
Coinjection of solutions containing site 1 sodium-channel blockers and “conventional” local anesthetics prolongs block showed a 6-fold increase, compared with the compounds injected separately (9); this prolongation also occurs when they are coencapsulated in polymeric microspheres (2). Here, we did see this prolongation, but of lesser magnitude. This difference may be because coencapsulation of bupivacaine in STX-containing liposomes reduced the loading of the latter compound (Table S1).
There was mild to moderate focal inflammation 4 days after local injection of liposomes that was completely resolved by 21 days. No myotoxicity or neurotoxicity was seen in any formulations that did not contain bupivacaine (Fig. 5). The finding that there was no nerve injury was supported by the PCR analysis of genes that are known to be related to nerve injury (Fig. 6). These findings are a great improvement over those from polymeric and/or bupivacaine-containing particles in terms of myotoxicity and inflammation.
This improvement in tissue reaction was surprising, given our previous experience that injury results from controlled release of local anesthetics using a wide range of delivery vehicles. Although the reason for this improvement is not clear, it confirms the observation that the presence of particles per se (and by inference their nature) has a large impact on local injury (3).
Aside from the formulations where high dexamethasone contents increased efflux of STX, there was no systemic toxicity from STX-containing liposomes, even with prolonged durations of block, as assessed by the absence of changes in latency in the contralateral extremity. The latter is a validated measure of systemic distribution and toxicity of local anesthetics (13, 31). This lack of systemic toxicity is important, because with polymeric particles, useful blockade could not be achieved without initial signs of systemic toxicity, due to burst release of TTX. This toxicity occurred even in the presence of epinephrine in the injectate, whereas here, there was no systemic toxicity even without epinephrine. It is likely that toxicity would eventually occur were we to further increase the amount of encapsulated STX, or the amount of particles delivered, even were we to add epinephrine to the injectate. However, it is possible that, when used in larger animals, such as humans, prolonged blocks will be achieved with little toxicity. This improvement in safety could occur because the systemic toxicity of a given dose of liposomes would be reduced, because the toxic dose scales linearly with volume of distribution (i.e., the mass of the recipient), whereas local effect (e.g., local anesthesia) has a much weaker relationship to body size (32). Therefore, the same formulation might have a better therapeutic index in larger animals. Also, larger animals can be injected with more particle, which can greatly increase the duration of block (1). These issues will have to be confirmed for these formulations in larger animal models. Nonetheless, it is important to recognize the potential of these particles to be systemically toxic.
Another significant advantage of this formulation over the polymeric systems (2) is the very small coefficient of variation in block duration. For example, STX + dexamethasone liposomes gave a block duration of 180 ± 4 h (coefficient of variation = 2.2%). In contrast, 60-μm polymeric particles gave a median block duraion of 9.25 days, with an interquartile range of 8.3–14.8 days (2). This lower variability may be because the liposomes were a better suspension, without needle-clogging. Reproducibility of block duration is an important clinical performance criterion.
Our data regarding particle stability suggest that these formulations could have storage characteristics suitable for practical use. Obviously, there are many other aspects of formulation and characterization that would have to be addressed before use in humans.
In conclusion, ultralong-acting STX-based liposomal local anesthetics were developed that were biocompatible in terms of myotoxicity, neurotoxicity, inflammation, and systemic toxicity, and did not cause autotomy in an animal model system.
Methods
Liposome Preparation.
Liposomes were prepared by modified thin lipid film hydration (33). Lipids were selected to produce relatively fluid (DMPC-DMPG) or solid (DSPC-DSPG) liposomes at 37 °C (phase transition temperatures, Tm; DSPC = 56 °C and DMPC = 23 °C). DSPC:DSPG:cholesterol or DMPC:DMPG:cholesterol (molar ratio 3:1:2) were dissolved in t-butanol. Dexamethasone was added in some samples before lyophilization. The lyophilized cake was hydrated with 250 mM ammonium sulfate or, in some groups, with 0.1 mg STX, at 55–60 °C. The suspension was homogenized at 10,000 × g with a 3/8“ MiniMicro workhead on a L4RT-A Silverson Laboratory Mixer for 10 min followed by 10 freeze-thaw cycles. Excess free STX was removed by centrifugation (4,000 × g, 4 °C for 20 min), and replaced by 2 mL of 30 mg/mL bupivacaine hydrochloride in 20 mM citrate buffer pH 4.0, or with 0.9% saline if bupivacaine was not desired. Liposome suspensions with bupivacaine added were stirred at 50 °C for 4–6 h. Liposome suspensions were dialyzed against 0.9% saline solution in 50-kDa molecular mass cut-off dialysis bags for 48 h. Drug-free liposomes were prepared by the same procedure, omitting the drug.
Liposome Characterization.
Liposomes were sized with a Beckmann Coulter Counter Multisizer 3. Zeta potentials were measured by using Brookhaven Instruments Corporation ZetaPALS and ZetaPlus software. Liposome drug concentrations were determined after disruption of the liposomes with octyl β-d-glucopyranoside (OGP). Dexamethasone and bupivacaine were quantitated by HPLC (Agilent HPLC 1100 Series system) at 254 and 215 nm, respectively, using methods from the U.S. Pharmacopeia. Determination of STX concentration was based on the method of Bates et al. (34), in which STX is oxidized to fluorescent products. Lipid concentrations were determined by colorimetry by the Bartlett assay (SI Materials and Methods) (35).
In Vitro Drug Release.
One mL of liposomes or compounds in solution were inserted into the lumen of a SpectraPor 1.1 Biotec Dispodialyzer (Spectrum Laboratories) with a 25,000 MW cut-off. The dialysis bag was placed in a test tube with 12 mL PBS and incubated at 37 °C on a tilt-table (Ames Aliquot, Miles). At predetermined intervals, the dialysis bag was transferred to a new test tube with fresh PBS that was prewarmed to 37 °C. Concentrations of compounds were quantitated as above.
Stability.
Stability was determined by examining changes in vesicle size, zeta potential, liposome integrity, and drug and lipid leakage (disruption of the membrane) over time at room temperature (21 °C) and 4 °C. At specific time points, 400 μL of the liposomal formulation was centrifuged with a Centricon separation filter (30,000 MW Millipore) at 3,500 × g, for 30 min, at 4 °C. The liposomes were retained in the upper chamber; 100–150 μL of the filtrate was recovered from the lower chamber, in which drug and lipid concentrations were determined (SI Materials and Methods). Leakage, liposome integrity, size distribution, and zeta potential were evaluated every day for 2 weeks.
Cell Culture.
C2C12 mouse myoblasts [American Type Culture Collection (ATCC) CRL-1772] were cultured to proliferate in DMEM supplemented with 20% FBS and 1% Penicillin Streptomycin. Cell culture supplies were obtained from Invitrogen, unless otherwise noted. Cells were plated at 50,000 cells per mL in DMEM with 2% horse serum and 1% Penn Strep, and left to differentiate into myotubules for 10–14 days. During differentiation, media were exchanged every 2 to 3 days. Cell viability and proliferation were studied after exposures to liposomes, free drugs, and empty liposomes with free drug for up to 96 h (see below).
PC12 cells (ATCC, CRL-1721) originating from rat adrenal gland pheochromocytoma were grown in 24-well tissue culture dishes (CellBind; Corning) with F-12K (ATCC) supplemented with 12.5% horse serum (Gibco), 2.5% FBS (Gibco), and 1% Penn Strep (Sigma). For neuronal induction (PC12), cells were seeded at a relative low density of 5 × 104 cells/cm2 and 50 ng/mL NGF was added 24 h after seeding. Cell viability and proliferation were evaluated as for C2C12 cells. Experiments with PC12 cells were conducted for up to 7 days.
Cell Viability Assay.
Cell viability was assessed after adding drug- or particle- containing media by a colorimetric assay (MTT kit, Promega G4100) at selected time points (SI Materials and Methods).
Sciatic Nerve Block and Neurobehavioral Testing.
Animals were cared for in compliance with protocols approved by the Children's Hospital Animal Care and Use Committee, and the Massachusetts Institute of Technology Committee on Animal Care, which conformed to guidelines of the International Association for the Study of Pain (36). Adult male Sprague–Dawley rats (Charles River Laboratories) weighing 320–420 g were housed in groups, in a 6 AM to 6 PM light–dark cycle. Under brief isoflurane-oxygen anesthesia, a 23G needle was introduced postero-medial to the greater trochanter, until bone was contacted, and 0.6 mL of test solution was injected over the sciatic nerve. Thermal nociception was assessed by a modified hotplate test, and motor function via a weight-bearing test (SI Materials and Methods) (13, 37).
Necropsy and Histological Analysis.
Rats were killed by carbon dioxide at 4, 14, and 21 days. The nerve and surrounding tissues were harvested, and histological hematoxylin-eosin sections were produced with standard techniques. Samples for Epon-embedded sections were fixed for 24 h at 24 °C in Karnovsky's KII Solution [2.5% glutaraldehyde, 2.0% paraformaldehyde, 0.025% calcium chloride in 0.1M sodium cacodylate buffer (Aldrich) pH 7.4]. Samples were postfixed in osmium tetroxide, stained with uranyl acetate, dehydrated in graded ethanol solutions, and infiltrated with propylene oxide/Epon mixtures. Subsequently, 1-μm sections were cut on an ultramicrotome and stained with toluidine blue. Photomicrographs were obtained by using a Nikon Eclipse 50i microscope with SPOT Insight 4 Meg FW Color Mosaic camera and SPOT 4.5.9.1 software from Diagnostic Instruments.
Gene Expression and RNA Isolation.
The L4 and L5 dorsal root ganglia were removed on necrospy and immediately frozen in liquid nitrogen. Tissue samples were stored at −80 °C until use. Total RNA was extracted from homogenized DRG samples by acid phenol extraction (TRIzol reagent; Gibco-BRL), and isolated with a Qiagen RNeasy Mini kit column (QIAGEN). The purity and concentration of RNA samples were determined from the absorbencies at 260 and 280 nm, with a NanoDrop 100 spectrophotometer (NanoDrop Technologies).
Real-Time PCR.
Total DRG RNA samples underwent reverse transcription with SuperScript III (Invitrogen) following the manufacturer's procedure. Real-time PCR for each sample were run in duplicate using 100 ng of cDNA in Taqman gene expression assays (Applied Biosystems) according to the manufacturer's instructions. Real-time PCR was performed using Applied Biosystems Step One equipment and program. The relative amount of specifically amplified cDNA was calculated using the delta-CT method (38, 39). The Applied Biosystems primers used are as follows: GAPDH: Rn99999916_S1, β-actin: Rn00667869_m1; Gadd45 α: Rn00577049_m1; ATF3: Rn00563784_m1; Cacna2d1: Rn01442580_m1; Smagp: Rn00788145_g1.
Statistics.
Data are presented as means ± SDs (n = 4 in release kinetics, cell work, and gene expression; n = 8 in neurobehavioral studies). To take multiple comparisons into account, all statistical comparisons were done with the Tukey–Kramer test, using InStat software (GraphPad). P < 0.05 was considered to denote statistical significance.
Supplementary Material
Acknowledgments.
This work was supported by National Institute of General Medical Sciences Grant GM073626 (to D.S.K.).
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
See Commentary on page 6891.
This article contains supporting information online at www.pnas.org/cgi/content/full/0900598106/DCSupplemental.
References
- 1.Drager C, Benziger D, Gao F, Berde CB. Prolonged intercostal nerve blockade in sheep using controlled-release of bupivacaine and dexamethasone from polymer microspheres. Anesthesiology. 1998;89:969–979. doi: 10.1097/00000542-199810000-00022. [DOI] [PubMed] [Google Scholar]
- 2.Kohane DS, et al. Prolonged duration local anesthesia from tetrodotoxin-enhanced local anesthetic microspheres. Pain. 2003;104:415–421. doi: 10.1016/s0304-3959(03)00049-6. [DOI] [PubMed] [Google Scholar]
- 3.Padera R, Bellas E, Tse JY, Hao D, Kohane DS. Local myotoxicity from sustained release of bupivacaine from microparticles. Anesthesiology. 2008;108:921–928. doi: 10.1097/ALN.0b013e31816c8a48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pere P, Watanabe H, Pitkanen M, Wahlstrom T, Rosenberg PH. Local myotoxicity of bupivacaine in rabbits after continuous supraclavicular brachial plexus block. Reg Anesth. 1993;18:304–307. [PubMed] [Google Scholar]
- 5.Jia X, Colombo G, Padera R, Langer R, Kohane DS. Prolongation of sciatic nerve blockade by in situ cross-linked hyaluronic acid. Biomaterials. 2004;25:4797–4804. doi: 10.1016/j.biomaterials.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Zimmer C, Piepenbrink K, Riest G, Peters J. Cardiotoxic and neurotoxic effects after accidental intravascular bupivacaine administration. Therapy with lidocaine propofol and lipid emulsion. Anaesthesist. 2007;56:449–453. doi: 10.1007/s00101-007-1147-3. [DOI] [PubMed] [Google Scholar]
- 7.Yamashita A, et al. A comparison of the neurotoxic effects on the spinal cord of tetracaine, lidocaine, bupivacaine, and ropivacaine administered intrathecally in rabbits. Anesth Analg. 2003;97:512–519. doi: 10.1213/01.ANE.0000068885.78816.5B. [DOI] [PubMed] [Google Scholar]
- 8.Kohane DS, et al. Biocompatibility of lipid-protein-sugar particles containing bupivacaine in the epineurium. J Biomed Mater Res. 2002;59:450–459. doi: 10.1002/jbm.1261. [DOI] [PubMed] [Google Scholar]
- 9.Barnet CS, Tse JY, Kohane DS. Site 1 sodium channel blockers prolong the duration of sciatic nerve blockade from tricyclic antidepressants. Pain. 2004;110:432–438. doi: 10.1016/j.pain.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 10.Sakura S, Bollen AW, Ciriales R, Drasner K. Local anesthetic neurotoxicity does not result from blockade of voltage-gated sodium channels. Anesth Analg. 1995;81:338–346. doi: 10.1097/00000539-199508000-00023. [DOI] [PubMed] [Google Scholar]
- 11.Kohane DS, et al. The local anesthetic properties and toxicity of saxitonin homologues for rat sciatic nerve block in vivo. Reg Anesth Pain Med. 2000;25:52–59. doi: 10.1016/s1098-7339(00)80011-5. [DOI] [PubMed] [Google Scholar]
- 12.Barnet CS, Louis DN, Kohane DS. Tissue injury from tricyclic antidepressants used as local anesthetics. Anesth Analg. 2005;101:1838–1843. doi: 10.1213/01.ANE.0000184129.50312.C1. [DOI] [PubMed] [Google Scholar]
- 13.Kohane DS, et al. A re-examination of tetrodotoxin for prolonged duration local anesthesia. Anesthesiology. 1998;89:119–131. doi: 10.1097/00000542-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Mearow KM, Dodge ME, Rahimtula M, Yegappan C. Stress-mediated signaling in PC12 cells - the role of the small heat shock protein, Hsp27, and Akt in protecting cells from heat stress and nerve growth factor withdrawal. J Neurochem. 2002;83:452–462. doi: 10.1046/j.1471-4159.2002.01151.x. [DOI] [PubMed] [Google Scholar]
- 15.Befort K, Karchewski L, Lanoue C, Woolf CJ. Selective up-regulation of the growth arrest DNA damage-inducible gene Gadd45 alpha in sensory and motor neurons after peripheral nerve injury. Eur J Neurosci. 2003;18:911–922. doi: 10.1046/j.1460-9568.2003.02827.x. [DOI] [PubMed] [Google Scholar]
- 16.Nakagomi S, Suzuki Y, Namikawa K, Kiryu-Seo S, Kiyama H. Expression of the activating transcription factor 3 prevents c-Jun N-terminal kinase-induced neuronal death by promoting heat shock protein 27 expression and Akt activation. J Neurosci. 2003;23:5187–5196. doi: 10.1523/JNEUROSCI.23-12-05187.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song DY, et al. Axotomy-induced dopaminergic neurodegeneration is accompanied with c-Jun phosphorylation and activation transcription factor 3 expression. Exp Neurol. 2008;209:268–278. doi: 10.1016/j.expneurol.2007.09.033. [DOI] [PubMed] [Google Scholar]
- 18.Soares S, et al. Neuronal and glial expression of the adhesion molecule TAG-1 is regulated after peripheral nerve lesion or central neurodegeneration of adult nervous system. Eur J Neurosci. 2005;21:1169–1180. doi: 10.1111/j.1460-9568.2005.03961.x. [DOI] [PubMed] [Google Scholar]
- 19.Luo ZD, et al. Injury type-specific calcium channel alpha 2 delta-1 subunit up-regulation in rat neuropathic pain models correlates with antiallodynic effects of gabapentin. J Pharmacol Exp Ther. 2002;303:1199–1205. doi: 10.1124/jpet.102.041574. [DOI] [PubMed] [Google Scholar]
- 20.Newton RA, Bingham S, Case PC, Sanger GJ, Lawson SN. Dorsal root ganglion neurons show increased expression of the calcium channel alpha2delta-1 subunit following partial sciatic nerve injury. Brain Res Mol Brain Res. 2001;95:1–8. doi: 10.1016/s0169-328x(01)00188-7. [DOI] [PubMed] [Google Scholar]
- 21.Gerner P, Mujtaba M, Sinnott CJ, Wang GK. Amitriptyline versus bupivacaine in rat sciatic nerve blockade. Anesthesiology. 2001;94:661–667. doi: 10.1097/00000542-200104000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Lirk P, et al. The neurotoxic effects of amitriptyline are mediated by apoptosis and are effectively blocked by inhibition of caspase activity. Anesth Analg. 2006;102:1728–1733. doi: 10.1213/01.ane.0000216018.62549.bb. [DOI] [PubMed] [Google Scholar]
- 23.Haller I, et al. Differential neurotoxicity of tricyclic antidepressants and novel derivatives in vitro in a dorsal root ganglion cell culture model. Eur J Anaesthesiol. 2007;24:702–708. doi: 10.1017/S0265021507000154. [DOI] [PubMed] [Google Scholar]
- 24.Wall PD, et al. Autotomy following peripheral nerve lesions: Experimental anaesthesia dolorosa. Pain. 1979;7:103–111. doi: 10.1016/0304-3959(79)90002-2. [DOI] [PubMed] [Google Scholar]
- 25.Grant GJ, et al. A novel liposomal bupivacaine formulation to produce ultralong-acting analgesia. Anesthesiology. 2004;101:133–137. doi: 10.1097/00000542-200407000-00021. [DOI] [PubMed] [Google Scholar]
- 26.Grant GJ, Piskoun B, Bansinath M. Analgesic duration and kinetics of liposomal bupivacaine after subcutaneous injection in mice. Clin Exp Pharmacol Physiol. 2003;30:966–968. doi: 10.1111/j.1440-1681.2003.03933.x. [DOI] [PubMed] [Google Scholar]
- 27.Malinovsky JM, et al. A dose-response study of epidural liposomal bupivacaine in rabbits. J Control Release. 1999;60:111–119. doi: 10.1016/s0168-3659(99)00062-0. [DOI] [PubMed] [Google Scholar]
- 28.Grant GJ, et al. DRV liposomal bupivacaine: Preparation, characterization, and in vivo evaluation in mice. Pharm Res. 2001;18:336–343. doi: 10.1023/a:1011059131348. [DOI] [PubMed] [Google Scholar]
- 29.Cereda CM, Brunetto GB, de Araujo DR, de Paula E. Liposomal formulations of prilocaine, lidocaine and mepivacaine prolong analgesic duration. Can J Anaesth. 2006;53:1092–1097. [PubMed] [Google Scholar]
- 30.de Araujo DR, et al. Encapsulation of mepivacaine prolongs the analgesia provided by sciatic nerve blockade in mice. Can J Anaesth. 2004;51:566–572. doi: 10.1007/BF03018399. [DOI] [PubMed] [Google Scholar]
- 31.Kohane DS, Lu NT, Cairns BE, Berde CB. Effects of adrenergic agonists and antagonists on tetrodotoxin-induced nerve block. Reg Anesth Pain Med. 2001;26:239–245. doi: 10.1053/rapm.2001.23215. [DOI] [PubMed] [Google Scholar]
- 32.Kohane DS, et al. Sciatic nerve blockade in infant, adolescent, and adult rats: A comparison of ropivacaine with bupivacaine. Anesthesiology. 1998;89:1199–1208. doi: 10.1097/00000542-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 33.Szoka F, Jr, Papahadjopoulos D. Comparative properties and methods of preparation of lipid vesicles (liposomes) Annu Rev Biophys Bio. 1980;9:467–508. doi: 10.1146/annurev.bb.09.060180.002343. [DOI] [PubMed] [Google Scholar]
- 34.Bates HA, Kostriken R, Rapoport H. A chemical assay for saxitoxin. Improvements and modifications. J Agr Food Chem. 1978;26:252–254. doi: 10.1021/jf60215a060. [DOI] [PubMed] [Google Scholar]
- 35.Bartlett GR. Phosphorus assay in column chromatography. J Biol Chem. 1959;234:466–468. [PubMed] [Google Scholar]
- 36.Zimmermann M. Ethical guidelines for investigations of experimental pain in conscious animals. Pain. 1983;16:109–110. doi: 10.1016/0304-3959(83)90201-4. [DOI] [PubMed] [Google Scholar]
- 37.Thalhammer JG, Vladimirova M, Bershadsky B, Strichartz GR. Neurologic evaluation of the rat during sciatic nerve block with lidocaine. Anesthesiology. 1995;82:1013–1025. doi: 10.1097/00000542-199504000-00026. [DOI] [PubMed] [Google Scholar]
- 38.Vandesompele J, et al. Accurate normalization of real-time quantitative RT-PCR data by geometric averaging of multiple internal control genes. Genom Biol. 2002;3 doi: 10.1186/gb-2002-3-7-research0034. RESEARCH0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hoebeeck J, et al. Rapid detection of VHL exon deletions using real-time quantitative PCR. Lab Invest. 2005;85:24–33. doi: 10.1038/labinvest.3700209. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.