Abstract
Purpose
An observational prospective study was conducted to study the effects of hypotonic spa-water baths and narrowband ultraviolet B therapy given alone or in combination for treatment of moderate-severe psoriasis.
Materials and Methods
Two treatments were analysed: 2 weeks of balneotherapy followed by ultraviolet-B (UVB) 311-nm phototherapy (BPT) or 2 weeks of daily bath treatments of Comano water alone (BT). One hundred and eleven adult patients with moderate to severe chronic plaque psoriasis were enrolled. Quality of life (QoL) questionnaires {36-item Short Form of the Medical Outcomes Study questionnaire (SF-36) and Skindex-29} were administered at baseline and 2 months from the end of therapy. The self-administered Psoriasis Area Severity Index (SAPASI), and the General Health Questionnaire (GHQ)-12 (to assess clinical severity and psychological distress, respectively) were also recorded at the same time-periods.
Results
SAPASI was significantly reduced from 15.2 to 8.7 in BPT group and 11.6 to 7.8 in BT. A decrease of greater than 50% after therapy in SAPASI_50 score was reached by 42% and 37% of patients in the BPT and BT groups, respectively. At follow-up, both groups had better scores on all SF-36 scales (with statistically significant improvement in social functioning and mental health in the BPT group) and in all Skindex-29 scales. A statistically significant reduction of GHQ-12 positive cases was observed in the BPT group.
Conclusion
Comano spa-water alone or in combination with phototherapy had beneficial therapeutic effects on patients with psoriasis. Although our observational study design prevents us from making meaningful comparisons between the 2 interventions, the combination of balneo and phototherapy seems to improve QoL and lessen clinical severity, and reduced the proportion of GHQ-12 positive cases.
Keywords: Psoriasis, balneotherapy, phototherapy, Skindex-29, General Health Questionnaire-12, 36-item Short Form of the Medical Outcomes Study questionnaire
INTRODUCTION
Both ultraviolet B (UVB) exposure and bathing have been recognised to have beneficial effects on several chronic skin diseases.1,2 Most types of psoriasis are thought to respond to such interventions. In particular, the combination of baths in an established saline solution and exposure to ultraviolet rays of a wave-length of 311 nm seems to be effective particularly in the treatment of psoriasis.3,4 The efficacy of this method is not completely due to improved effect of phototherapy following hydration of the cornified layer, but also to the ionic mechanism of the elements contained in the baths.5 Several studies have tested different spa water baths, however only a few are randomised controlled trials, nevertheless, the majority of these studies observed the positive effect of saline waters.6,7
Comano, located in Northern Italy, has been known as an important spa water centre since ancient times. The water is oligometallic, has a temperature of 27℃ at the springs, and a pH of 7.5-7.6.8 The Italian National Health System officially recognises the beneficial effects of spa water treatment alone or in conjunction with treatments such as UVB treatment for psoriasis. We designed an observational study as a first step to evaluate the effect of Comano's water baths alone or in association with phototherapy on psoriasis patients, both in terms of clinical severity and patient's quality of life (QoL).
MATERIALS AND METHODS
One-hundred and eleven consecutive patients were observed from September to November 2005. No patient concurrently undergoing any other active treatment for psoriasis was enrolled in the study, and patients who were willing to enter the study protocol voluntarily stopped any treatment before starting the intervention. Only topical emollients for psoriasis treatment were allowed for the 2-month period after the bath sessions.
Other inclusion criteria were: 18 years of age or older, body surface area involved ≥ 10% (i.e., moderate-severe chronic plaque psoriasis), and patients signed a written informed consent form. Patients with erythrodermic and pustular forms of psoriasis, including palmoplantar types, as well as patients who had contraindications to phototherapy or balneotherapy were excluded from the study. The study was approved by the Ethical Committee of IDI-IRCCS.
Patients who agreed to participate in the study underwent 1 of the 2 following treatment programs:
A) Two weeks of daily balneotherapy with Comano water followed by UVB 311-nm phototherapy (BPT)
B) Two weeks of daily bath treatments with Comano water alone (BT).
The choice of treatment was agreed between patient and physician after a briefing.
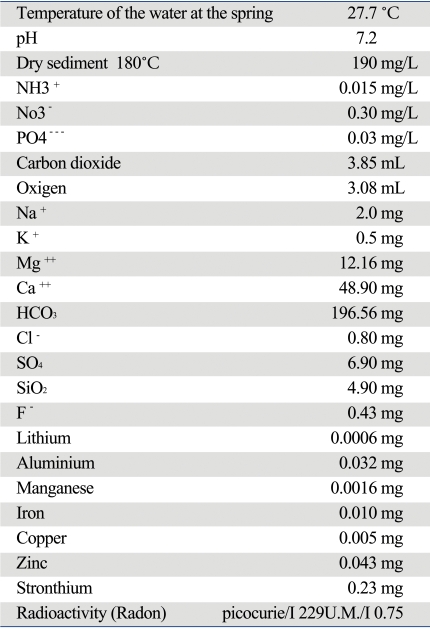
The treatment included 12 to 14 total immersion baths for 20 minutes once a day. The detailed characteristics of Comano water are described in Table 1. Exposure to Narrow Band UVB was determined and monitored according to skin type, and was carried out within 15 minutes from the end of the bath.
Table 1.
Physical and Chemical Features of Comano Spa Water
The severity of disease was assessed by a dermatologist who explained the purposes of the study to patients and gave them questionnaires to complete. The dermatologist monitored patients at the beginning of the study, during therapy, and 2 months later, when the follow-up questionnaires were collected.
The dermatologist also collected information on sociodemographic variables, clinical history, and other factors of clinical interest (e.g. clinical type and location of the disease, personal and family history of psoriasis and other diseases, seasonal changes, symptoms, etc.).
The self-administered Psoriasis Area Severity Index (SAPASI), the Skindex-29, the 36-item Short Form of the Medical Outcomes Study questionnaire (SF-36), and the General Health Questionnaire (GHQ)-12 were administered to patients before any study treatment was started. After 2 months from the end of BT or BPT, a follow up with SAPASI, GHQ-12 and Skindex-29 was requested and obtained by mail.
SAPASI is a structured instrument consisting of a line-drawing silhouette of the front and back of a body for patients to shade-in the affected areas and of 3 visual analog scales for recording the erythema, induration and scaliness of an average lesion. Based on the silhouette shading, 2 of the authors estimated the proportion of involved area for each body district, using the body surface as denominator. Disagreements were discussed until a consensus on the estimated proportion was reached. Finally, the area of psoriatic involvement for each of the 4 regions was assigned a numerical value of 0-6 corresponding to 0-100% involvement: 0, no involvement; 1, < 10%; 2, 10 < 30%; 3, 30 < 50%; 4, 50 < 70%; 5, 70 < 90%; 6, 90-100%. For each region, erythema, desquamation and induration of the plaques were rated according to the classical five-point scale: 0, no involvement; 1, slight; 2, moderate; 3, marked; 4, very marked.
The SAPASI scores were then calculated by investigators using electronic spreadsheets to implement the formulas originally proposed.9 Such scores have the same range of PASI scores and have been shown to have a high correlation with them.10 After 2 months, a SAPASI reduction of at least 50% (SAPASI_50) was considered to be a successful clinical outcome.
The Skindex-29 is a reliable and valid instrument that has been specifically designed for measuring health-related QoL in dermatological patients.11 It is constituted by 3 scales assessing areas considered essential in any instrument purported to assess QoL: burden of symptoms, functioning, and emotional state. The Italian version of this self-administered questionnaire has recently been validated.12,13 Patients answered the 29 questions referring to the previous 4-week period on a 5-point scale from 'never' (= 0) to 'all the time' (= 4). The score of each scale ranges from 0 to 100 (as a percentage of the maximum score obtainable on that scale), and higher scores reflect a worse QoL.
In addition, we also analysed what we called "warnings" in the Skindex-29; i.e. items/symptoms that the patient answered having experienced "all the time" in the four weeks before completing the questionnaire.
The SF-36 questionnaire was designed as a generic indicator of health status for use in population surveys and evaluative studies of health policy.14 As a generic instrument, the SF-36 was designed to be applicable to a wide range of types and severity of conditions. It is a useful instrument for monitoring patients with multiple conditions, for comparing the health status of patients with different conditions, and for comparing patients to the general population. The SF-36 includes 36 items, in a Likert-type or forced-choice format, intended to measure the following 8 dimensions: physical functioning (PF, limitations in performing physical activities such as bathing or dressing), role-physical (RP, limitations with work and other daily activities as a result of physical health), bodily pain (BP, how severe and limiting is pain), general health (GH, how general personal health is evaluated by the patient), vitality (VT, feeling tired and worn out vs. feeling full of energy), social functioning (SF, interference with normal social activities due to physical or emotional problems), role-emotional (RE, limitations with work and other daily activities as a result of emotional problems), mental health (MH, feeling nervous and depressed vs. peaceful, happy and calm). Scores for each domain range from 0 to 100, with high scores indicating a better status. We used the Italian version of the SF-36 cross-culturally validated within the framework of the International Quality of Life Assessment (IQOLA) Project.
The GHQ-12 is a self-administered questionnaire consisting of 12 items, designed to measure psychological distress and to detect current non-psychotic psychiatric disorders, usually depressive or anxiety disorders. The reliability and validity of the Italian version have been documented in many types of patients, including those with dermatological conditions.15,16 Answers are given on a 4-point scale. For instance, the answers to the item "in the last weeks, did you feel under strain?" are "no", "no more than usual", "more than usual", and "much more than usual". When scored with the binary method (0-0-1-1), the GHQ-12 can be used as a screening tool to detect minor non-psychotic psychiatric disorders. For instance, to receive a score of 1 on the previously described item, a subject should answer "more than usual" or "much more than usual". In this way, each subject obtains a score from 0 to 12, based on a previous validation study operationally, patients scoring four or more were considered as "GHQ-12 positive".17
Within-patient comparisons (baseline vs. two months follow-up) were performed using the paired Student's t-test for nonindependent observations. The Student's t-test for independent samples was used to compare the 2 treatment groups in each of questionnaires score/scales/determinants.
Two separate logistic regression models (for BPT and BT, respectively) were created to see whether SAPASI improvement at 2-month follow-up was associated with BPT or BT treatment while simultaneously controlling for other relevant variables such as age, gender, cigarette smoking, alcohol consumption, duration of disease, baseline level of clinical severity, and baseline presence of GHQ-12 positivity.
All statistical analyses were performed using the statistical software Stata 9.0 for Windows.
RESULTS
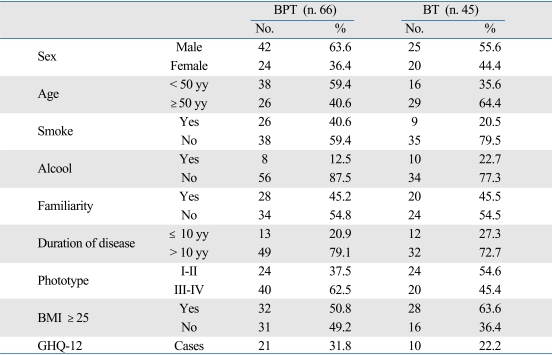
Patient characteristics at baseline are summarized in Table 2. Briefly, there were 66 patients in the BPT group, while there were 45 patients in BT group. Patients in BPT were younger (45 ± 13 years) than in BT (55 ± 15). At baseline, BPT patients had better SF-36 scores on the PF and PR scales, than BT patients. GHQ-12 cases were 32% in the BPT group and 22% in the BT group. SAPASI scores at baseline were significantly lower in BT than BPT. The patients in BPT, depending on the phototype, started UVB treatment with 0.02j and reached a mean cumulative dose of 12.64j.
Table 2.
Characteristic of Patients Treated with Balneophototherapy or Balneotherapy
BMI, body mass index; GHQ-12, General Health Questionnaire-12.
Mean age years ± SD: BPT, balneophototherapy group (45.4 ± 13.4), BT, balneotherapy group (55.4 ± 14.8).
Fifty four patients (82%) in BPT and 38 (84%) in BT sent back the questionnaires by mail 2 months after the end of the Comano treatment. No undesired side effects were described.
The mean SAPASI scores were significantly reduced at 2-month follow-up in both treatment groups (15.2 to 8.7 in group BPT and 11.6 to 7.8 in group BT). The mean value of SAPASI percent reduction was 39.5% in BPT and 37% in BT. SAPASI-50 was reached by 42% and 37% of patients in the BPT and BT groups, respectively.
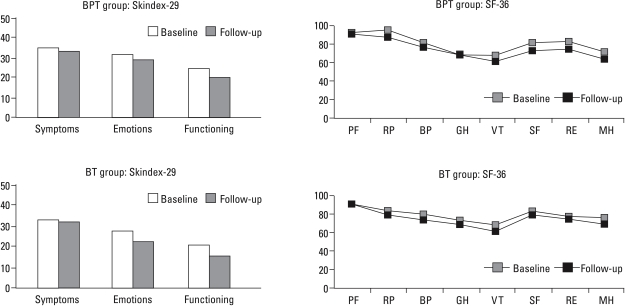
When the 2 separate logistic regression models for BPT and BT were created, none of the simultaneously considered variables (i.e., age, gender, cigarette smoking, alcohol consumption, duration of disease, baseline level of clinical severity, and baseline presence of GHQ-12 positivity) in addition to treatment resulted to be associated with SAPASI reduction. At follow-up, both groups had better scores on all SF-36 scales (with statistically significant improvement in social functioning and mental health in group BPT), and all Skindex-29 scales had lower values than those at baseline (Fig. 1). BPT patients who reached a SAPASI-50 after the intervention had statistically significant improvement in 5 scales of SF-36 health status questionnaire (RP, VT, SF, RE, MH) compared to the baseline; such improvement was not observed in patients treated only with BT (Fig. 2).
Fig. 1.
Skindex-29 test and SF-36 scales before and after BPT or BT therapies. SF-36, 36-item Short Form of the Medical Outcomes Study questionnaire; BTP, balneophototherapy; BT, balneotherapy, PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health.
Fig. 2.
SF-36 scales before and after BPT or BP therapies in patients with reduction of SAPASI > 50%. SF-36, 36-item Short Form of the Medical Outcomes Study questionnaire; BTP, balneophototherapy; BT, balneotherapy, SAPASI, self-administered Psoriasis Area Severity Index; PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health.
Referring to what we defined as "warnings" from the items of the Skindex-29 questionnaire, only one third of patients who answered that she/he experienced that problem "all the time" at baseline, still had the same problem 2 months after the end of treatment. Especially in the symptom scale for items related to "itch", "irritation", "skin sensitive", a dramatic reduction was observed in both groups.
GHQ-12 cases were reduced to 14% in the BPT group and to 18% in the BT group at the 2-month follow-up. The reduction of GHQ-12 cases in BPT was statistically significant, while it was not in BT.
DISCUSSION
In our study, we observed an improvement in clinical severity of psoriasis and QoL in both groups of patients using Narrow-Band UVB plus Comano spa water or Comano spa water alone.
The design of our observational study did not include randomisation, so that patients started one of the treatments on basis of personal preference or indication. Thus, it is not surprising that the 2 groups at baseline were quite different, and that significant differences were observed for some of the most relevant variables. BPT patients were younger with higher mean SAPASI scores before treatment, and a higher proportion of GHQ-12 cases. Such differences, in addition to very likely differences in other unmeasured (or unmeasurable) factors, can scarcely be appropriately taken care of even in a careful statistical analysis, so that relevant residual biases should be expected. Accordingly, it would be inappropriate to compare the 2 treatments and to draw any conclusion about their relative merits. However, it is interesting to describe within-group changes between baseline and follow-up, since the resulting estimates should be unbiased.
It seems that Comano bath treatment per se has a relevant effect on reducing SAPASI scores. In fact, a relevant reduction was observed also in the group not involved with phototherapy, since approximately 40% of reduction was reached in both groups. Such reduction was present 2 months after the end of treatment for both groups, during which period no other treatment was administered except emollients, suggesting that the effects of these interventions are not as ephemeral as they are thought to be, but may persist for a significant lapse of time.
The proportion of GHQ-12 positive patients in the BPT group was statistically significantly reduced 2 months after the intervention. We have recently observed in the prospective section of the IMPROVE study18 that improvement in psychological well being is much more likely in patients with higher percentages of reduction in SAPASI scores, and therefore, the greater clinical improvement in BTP patients, who had worse baseline SAPASI scores, could be a reason for such reduction in psychosocial distress.
Many patients with psoriasis request alternative therapies and BPT or BT seem to be acceptable choices. Narrow-Band ultraviolet B phototherapy is increasingly used as a treatment for psoriasis and the association with balneotherapy was introduced especially with saline bath water.19,20
The beneficial effect of bathing before UVB exposure could be partially explained by the fact that desquamation and reduction of thickness of lesional skin cause a decrease in the barrier function against irradiation.21 Another mechanism for salt water bath is that skin erythemal sensitivity can be increased. Bathing in high-concentration salt solution might enhance the effectiveness of UVB phototherapy, psoriasis lesional skin shows an increase of human leucocites elastasy activity compared with unaffected skin and its increased activity contributes to the persistence of psoriasic lesions. High concentration salt solution can elute this enzyme from psoriasic skin and its reduction can improve psoriasis.22,23 Contradictory data are present in the literature about the use of salt water and UVB. Non randomised comparison studies on patients with psoriasis support the common notion that there is a beneficial effect of salt water bath prior to phototherapy.24,25 Data obtained from comparative studies suggest that any additional benefits of soaking in salt water and tap water in BPT are unlikely to be due to the salinity of the liquids.26
A French group published an observed-blinded, 3-arm randomised control trial (RCT) comparing saline spa water bath alone, spa water bath plus Narrow-Band, UVB and UVB monotherapy in 71 patients with psoriasis, and concluded that spa water bath alone had a minor therapeutic effects on psoriasis, but the beneficial effect of bathing to enhance phototherapy was not demonstrated.6 In a recent randomised study to evaluate the efficacy of Dead Sea salt balneotherapy vs. narrow band ultraviolet B monotherapy for chronic plaque psoriasis, Dawe et al.7 reported that pre-treatment of Dead sea salt soaks before administration of UVB did not result in a clinically important improvement in clearance of psoriasis.
The chemical composition of water used for bathing could catalyse and magnify the effect of phototherapy. BT with Comano spa water is used for psoriasis and other skin disorders, however the mechanism of action of this hypotonic water is still unknown. Studies have demonstrated that Comano water interferes with the expression and secretion of vascular endothelial growth factor-A (VEGF-A) protein isoform in vitro. These effects would reduce all VEGF-A-mediated angiogenic, vessel permeabilising and chemotactic effects, explaining at least in part the beneficial action of balneotherapy in clinical manifestation of psoriasis.27
We observed a reduction of SAPASI scores, an improvement in QoL and overall health status in patients treated in Comano. Even though the reduction of SAPASI scores is larger in the group treated with UVB, the different baseline status in this group should be taken into account, and the greater improvement of skin conditions should not be attributed to the addition of UVB to spa water alone.
The improvement in QoL for psoriasis after BPT or BT treatments was present in all dimensions explored by the Skindex-29, i.e., emotional status, symptoms, and functioning. The difference between before and after treatment did not reach statistical significance, but was clinically relevant in both groups. Especially for symptoms, the percentage of patients experiencing a problem "all the time" was dramatically reduced. The hypotonic Comano water certainly did not increase itch or skin burning, as otherwise reported by Labreze for a study on saline baths.
We wish to further acknowledge and actually warn the readers on the limitations of our observational study: the allocation to the therapeutic interventions was not randomised, and we think that it is a good example of how non-random allocation to different treatment groups often leads to baseline differences that may heavily bias between-treatment comparisons. Furthermore, the use of postal questionnaires in the follow-up did not guarantee feedback from all patients: although percentages of response above 80% are excellent for an observational study of this kind, they would be considered scarce for a clinical trial.
However, in conclusion, our study showed that BT with hypotonic spa water, with or without additional UVB therapy, had a beneficial effect on the clinical improvement of psoriasis. Even considering the limitations of our study design, the association of phototherapy with balneotherapy seems to have effects on psoriasis similar the water bath alone. Information obtained from this observational study might increase interest towards evidence-based evaluation of balneotherapy and balneophototherapy as treatments for psoriasis, and could stimulate randomised controlled trials to test the relative efficacy of the 2 treatments, as well as their possible long-term efficacy.
References
- 1.An appraisal of narrowband (TL-01) UVB phototherapy. British Photodermatology Group workshop Report (April 1996) Br J Dermatol. 1997;137:327–330. [PubMed] [Google Scholar]
- 2.Halevy S, Sukenik S. Different modalities of spa therapy for skin diseases at the Dead Sea area. Arch Dermatol. 1998;134:1416–1420. doi: 10.1001/archderm.134.11.1416. [DOI] [PubMed] [Google Scholar]
- 3.Holló P, Gonzalez R, Kása M, Horváth A. Synchronous balneophototherapy is effective for the different clinical types of psoriasis. J Eur Acad Dermatol Venereol. 2005;19:578–581. doi: 10.1111/j.1468-3083.2005.01257.x. [DOI] [PubMed] [Google Scholar]
- 4.Schiffner R, Shifnner-Rohe J, Wölfl G, Landthaler M, Glässl A, Walther T, et al. Evaluation of a multicentre study of synchronous application of narrowband ultraviolet B phototherapy (TL-01) and bathing in Dead Sea salt solution for psoriasis vulgaris. Br J Dermatol. 2000;142:740–747. doi: 10.1046/j.1365-2133.2000.03420.x. [DOI] [PubMed] [Google Scholar]
- 5.Tsoureli-Nikita E, Menchini G, Ghersetich I, Hercogova J. Alternative treatment of psoriasis with balneotherapy using Leopoldine spa water. J Eur Acad Dermatol Venereol. 2002;16:260–262. doi: 10.1046/j.1468-3083.2002.00452.x. [DOI] [PubMed] [Google Scholar]
- 6.Léauté-Labrèze C, Saillour F, Chêne G, Cazenave C, Luxey-Bellocq ML, Sanciaume C, et al. Saline spa water or combined water and UV-B for psoriasis vs conventional UV-B: lessons from the salies de Béarn randomized study. Arch Dermatol. 2001;137:1035–1039. [PubMed] [Google Scholar]
- 7.Dawe RS, Yule S, Cameron H, Moseley H, Ibbotson SH, Ferguson J. A randomized controlled comparison of the efficacy of Dead Sea salt balneophototherapy vs. narrowband ultraviolet B monotherapy for chronic plaque psoriasis. Br J Dermatol. 2005;153:613–619. doi: 10.1111/j.1365-2133.2005.06663.x. [DOI] [PubMed] [Google Scholar]
- 8.Zumiani G, Zanoni M, Agostini G. Evaluation of the efficacy of Comano thermal baths water versus tap water in the treatment of eczematous dermatitis. G Ital Dermatol Venereol. 2000;135:253–258. [Google Scholar]
- 9.Feldman SR, Fleischer AB, Jr, Reboussin DM, Rapp SR, Exum ML, Clark AR, et al. The self-administered psoriasis area and severity index is valid and reliable. J Invest Dermatol. 1996;106:183–186. doi: 10.1111/1523-1747.ep12329912. [DOI] [PubMed] [Google Scholar]
- 10.Sampogna F, Sera F, Mazzotti E, Pasquini P, Picardi A, Abeni D IDI Multipurpose Psoriasis Research on Vital Experiences (IMPROVE) Study Group. Performance of the self-administered psoriasis area and severity index in evaluating clinical and sociodemographic subgroups of patients with psoriasis. Arch Dermatol. 2003;139:353–358. doi: 10.1001/archderm.139.3.353. [DOI] [PubMed] [Google Scholar]
- 11.Chren MM, Lasek RJ, Flocke SA, Zyzanski SJ. Improved discriminative and evaluative capability of a refined version of Skindex, a quality-of-life instrument for patients with skin diseases. Arch Dermatol. 1997;133:1433–1440. [PubMed] [Google Scholar]
- 12.Abeni D, Picardi A, Puddu P, Pasquini P, Chren MM. Construction and validation of the Italian version of Skindex-29, a new instrument to measure quality of life in dermatology (in Italian, abstract in English) G Ital Dermatol Venereol. 2001;136:73–76. [Google Scholar]
- 13.Abeni D, Picardi A, Pasquini P, Melchi CF, Chren MM. Further evidence of the validity and reliability of the Skindex-29: an Italian study on 2,242 dermatological outpatients. Dermatology. 2002;204:43–49. doi: 10.1159/000051809. [DOI] [PubMed] [Google Scholar]
- 14.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 15.Piccinelli M, Bisoffi G, Bon MG, Cunico L, Tansella M. Validity and test-retest reliability of the Italian version of the 12-item General Health Questionnaire in general practice: a comparison between three scoring methods. Compr Psychiatry. 1993;34:198–205. doi: 10.1016/0010-440x(93)90048-9. [DOI] [PubMed] [Google Scholar]
- 16.Picardi A, Abeni D, Pasquini P. Assessing psychological distress in patients with skin diseases: reliability, validity and factor structure of the GHQ-12. J Eur Acad Dermatol Venereol. 2001;15:410–417. doi: 10.1046/j.1468-3083.2001.00336.x. [DOI] [PubMed] [Google Scholar]
- 17.Picardi A, Abeni D, Mazzotti E, Fassone G, Lega I, Ramieri L, et al. Screening for psychiatric disorders in patients with skin diseases: a performance study of the 12-item General Health Questionnaire. J Psychosom Res. 2004;57:219–223. doi: 10.1016/S0022-3999(03)00619-6. [DOI] [PubMed] [Google Scholar]
- 18.Sampogna F, Tabolli S, Abeni D IDI Multipurpose Psoriasis Research on Vital Experiences (IMPROVE) investigators. The impact of changes in clinical severity on psychiatric morbidity in patients with psoriasis: a follow-up study. Br J Dermatol. 2007;157:508–513. doi: 10.1111/j.1365-2133.2007.08071.x. [DOI] [PubMed] [Google Scholar]
- 19.Montgomery BJ. Bathing for psoriasis in the Dead Sea. JAMA. 1979;241:227–231. doi: 10.1001/jama.241.3.227. [DOI] [PubMed] [Google Scholar]
- 20.Even-Paz Z, Shani J. The Dead Sea and psoriasis. Historical and geographic background. Int J Dermatol. 1989;28:1–9. doi: 10.1111/j.1365-4362.1989.tb01299.x. [DOI] [PubMed] [Google Scholar]
- 21.Abels DJ, Kipnis V. Bioclimatology and balneology in dermatology: a Dead Sea perspective. Clin Dermatol. 1998;16:695–698. doi: 10.1016/s0738-081x(98)00059-5. [DOI] [PubMed] [Google Scholar]
- 22.Boer J. The influence of mineral water solutions in phototherapy. Clin Dermatol. 1996;14:665–673. doi: 10.1016/s0738-081x(96)00102-2. [DOI] [PubMed] [Google Scholar]
- 23.Wiedow O, Wiese F, Streit V, Kalm C, Christophers E. Lesional elastase activity in psoriasis, contact dermatitis, and atopic dermatitis. J Invest Dermatol. 1992;99:306–309. doi: 10.1111/1523-1747.ep12616644. [DOI] [PubMed] [Google Scholar]
- 24.Celerier P, Richard A, Litoux P, Dreno B. Modulatory effects of selenium and strontium salts on keratinocyte-derived inflammatory cytokines. Arch Dermatol Res. 1995;287:680–682. doi: 10.1007/BF00371742. [DOI] [PubMed] [Google Scholar]
- 25.Olafsson JH, Sigurgeirsson B, Pálsdóttir R. Psoriasis treatment: bathing in a thermal lagoon combined with UVB, versus UVB treatment only. Acta Derm Venereol. 1996;76:228–230. doi: 10.2340/0001555576228230. [DOI] [PubMed] [Google Scholar]
- 26.Gambichler T, Tomi NS, Kreuter A. Controlled clinical trials on balneophototherapy in psoriasis. Br J Dermatol. 2006;154:802–803. doi: 10.1111/j.1365-2133.2006.07176.x. [DOI] [PubMed] [Google Scholar]
- 27.Chiarini A, Dal Pra I, Pacchiana R, Menapace L, Zumiani G, Zanoni M, et al. Comano's (Trentino) thermal water interferes with the expression and secretion of vascular endothelial growth factor-A protein isoforms by cultured human psoriatic keratinocytes: a potential mechanism of its anti-psoriatic action. Int J Mol Med. 2006;18:17–25. [PubMed] [Google Scholar]