Abstract
Purpose
To evaluate the diagnosis and treatment of the carpal tunnel syndrome (CTS) due to space occupying lesions (SOL).
Materials and Methods
Eleven patients and 12 cases that underwent surgery for CTS due to SOL were studied retrospectively. We excluded SOL caused by bony lesions, such as malunion of distal radius fracture, volar lunate dislocation, etc. The average age was 51 years. There were 3 men and 8 women. Follow-up period was 12 to 40 months with an average of 18 months. The diagnosis of CTS was made clinically and electrophysiologically. In patients with swelling or tenderness on the area of wrist flexion creases, magnetic resonance imaging (MRI) and/or computed tomogram (CT) were additionally taken as well as the carpal tunnel view. We performed conventional open transverse carpal ligament release and removal of SOL.
Results
The types of lesion confirmed by pathologic examination were; tuberculosis tenosynovitis in 3 cases, nonspecific tenosynovitis in 2 cases, and gout in one case. Other SOLs were tumorous condition in five cases, and abnormal palmaris longus hypertrophy in 1 case. Tumorous conditions were due to calcifying mass in 4 cases and ganglion in 1 case. Following surgery, all cases showed alleviation of symptom without recurrence or complications.
Conclusion
In cases with swelling or tenderness on the area of wrist flexion creases, it is important to obtain a carpal tunnel view, and MRI and/or CT should be supplemented in order to rule out SOLs around the carpal tunnel, if necessary.
Keywords: Carpal tunnel syndrome, space occupying lesion
INTRODUCTION
Carpal tunnel syndrome (CTS) is the most frequently encountered peripheral compression neuropathy. Anatomically, as the median nerve is chronically compressed inside the narrow carpal canal, which consists of the transverse carpal ligament and the carpal bones, pain and paresthesia are exhibited in the median nerve distribution area, and thenar muscle weakness and atrophy occur. Although most cases are idiopathic, CTS is also associated with a number of systemic conditions, including rheumatoid arthritis, hypothyroidism, diabetis mellitus, acromegaly, and pregnancy.
There is a well established link between raised intracarpal pressure and clinical CTS. In mechanical terms, the raised pressure must result from either an increase in content or a decrease in size of the carpal canal, or some combination of the 2. Only in a minority of cases, 1 or both of these circumstances may apply; SOLs in the carpal canal, but such factors are rare in most cases. However, if these SOLs are not discovered or misdiagnosed and treated as idiopathic CTS, the patient's symptoms will not improve. Median nerve compression in the carpal tunnel due to mass effects is very rare, however, there are reports of tumorous conditions, hypertrophy of tenosynoviums, tophaceous gout, malunion after distal radial fractrures, volar lunate dislocation, and posttraumatic osteophytes.1-10 It is possible to detect space occupying bony lesions with plain X-ray before surgery, but it is difficult to detect space occupying soft tissue lesions without special examination. Therefore, the aim of this study was to evaluate the diagnosis and treatment of CTS caused by space occupying lesions (SOLs), especially soft tissue lesions.
MATERIALS AND METHODS
A 10 year retrospective study was carried out on 11 patients with 12 cases that underwent surgery from January 1992 to December 2001 for CTS due to SOL. This study includes not only masses but also the lesions which increase the contents of canal (hypertrophic tenosynovium, tophaceous gout, etc). We excluded SOL caused by bony lesion such as malunion of distal radius fracture, volar lunate dislocation, carpal bone fracture, etc. The average age was 51 years (range, 25 to 78 years). There were 3 men and 8 women. The follow-up period was 12 to 40 months with an average of 18 months. Ten patients had unilateral involvement and only 1 patient had bilateral involvement.
The diagnosis of carpal tunnel syndrome was made clinically and electrophysiologically. Clinical evaluation included presence of typical sensory symptoms, Phalen's and Tinel's tests, sensory testing by two-point discrimination, grip strength (Jamar Dynamometer), pinch strength (Jamar Pinch Gauze), and examination for thenar atrophy. All patients showed distal motor nerve latency of more than 4.2 ms or sensory nerve conduction velocity of less than 45 m per second across the carpal tunnel.
In our hospital, when a patient is clinically suspected of having CTS, we routinely conduct radiological tests and obtain radiographs of posteroanterior, lateral and carpal tunnel views. In patients with swelling or tenderness on the area of wrist flexion creases, computed tomography (CT) and/or magnetic resonance imaging (MRI) along with carpal tunnel view were additionally taken to exclude SOLs. When infection or synovitis was suspected on the volar area of the wrist, bone scan was performed before MRI was taken. We performed conventional open transverse carpal ligament release and removed SOL using the standard long incision.
RESULTS
We performed surgery on 324 patients (568 cases) to treat CTS from January 1992 to December 2001; 244 patients had bilateral CTS and 80 patients unilateral. Ten out of 80 unilateral CTS patients and 1 out of 244 bilateral CTS patients had SOLs. The preoperative physical examination showed definite palpable mass at the volar aspect of the wrist in 1 patient, diffuse swelling in 7 patients, and no definite swelling in 3 patients. Following surgery, all cases showed alleviation of symptom without recurrence or complications. In this study, 10 out of 11 patients exhibited unilateral CTS, and only 1 patient with a calcifying mass exhibited bilateral CTS. Furthermore, 11 cases were due to the lesion inside the carpal canal and only 1 case was due to external compression of the carpal canal (palmaris longus hypertrophy). The types of lesion confirmed by pathologic examination were; tuberculosis tenosynovitis in 3 cases, nonspecific tenosynovitis in 2 cases, and gout in 1 case. Other SOLs were tumorous condition in 5 cases, and abnormal palmaris longus hypertrophy in 1 case.1 Tumorous conditions were due to calcifying mass in 4 cases and ganglion in 1 case (Table 1).3,7
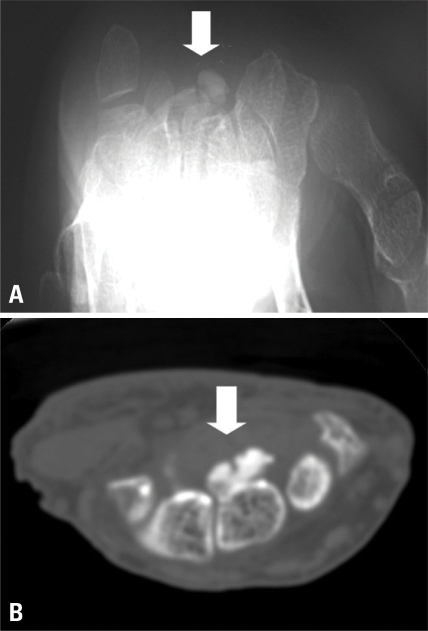
Table 1.
Clinical Features of the Patients
F, female; M, male; MRI, magnetic resonance imaging; CT, computed tomogram; Tbc, tuberculosis; D, dominant hand; N, non-dominant hand; B, both hand.
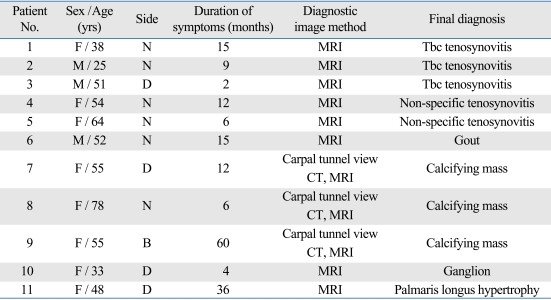
All 3 tuberculous tenosynovitis patients showed clinically proper symptoms of CTS, physical examination of volar wrist crease area showed diffused swelling, and Tinel sign, and Phalen tests appeared to be positive. One of the patients had been diagnosed with pulmonary tuberculosis 2 months before being treated at our hospital and had been prescribed antituberculosis drugs for the past 2 months. Electrophysiologic studies were consistent with CTS, and MRI showed synovial hypertrophy around the flexor tendon (Fig. 1A). Conventional open transverse carpal ligament release was performed, and all the tissue involved was excised and a complete tenosynovectomy was performed. Histologic examination of all the specimens showed caseous necrosis and tuberculous granuloma with Langhans giant cells (Fig. 1B and C). In a culture examination, mycobacterium tuberculosis was cultivated from 2 patients, however, it was not cultivated in a patient who had been undergoing pulmonary tuberculosis. After surgery, patients took anti Tbc drugs (isoniazid + rifampin + ethambutol + pyrazinamide) for 18 months. Postoperative recovery was uneventful with no wound problems and relief of symptoms.
Fig. 1.
(A) Hypertrophied flexor digitorum profundus tenosynovium was noted in carpal tunnel on MRI (black arrow, hypertrophied tenosynovium). (B and C) Caseous necrosis, granuloma with Langerhan's giant cell, and lymphocytic infiltration show tuberculous tenosynovitis (black arrow, Langerhan's multinucleated giant cell).
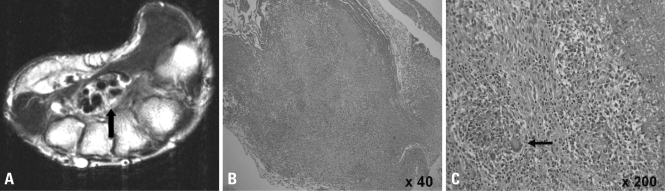
A patient diagnosed as CTS caused by tophaceous gout had a past history of gout 20 years ago, and initial uric acid level was elevated to 8.2 mg/dL. Electrophysilogic study showed CTS, and further MRI examinations indicated infiltration of tophi around carpal bones (Fig. 2A). Conventional open transverse carpal ligament release and removal of goutic tophi were performed. In operative finding, chalky white deposits of urate crystals were seen in synovium of flexor tendon sheaths. Pathologic examinations showed nodular and fibrous materals infiltrated into connective tissues, and histiocytes and giant cells were seen around them, indicating typical findings of gout (Fig. 2B). Under polarized light microscopy, needle-shaped crystals with strong negative birefringence were seen in these surgical specimens (Fig. 2C). After surgery, the patient's gout was treated with allopurinol medication, and uric acid level returned to the normal 5.5 mg/dL in a 14 month follow up examination. The patient was satisfied with the results of the surgery and expressed no discomfort in daily activities.
Fig. 2.
(A) Tophi infiltration was noted between flexor digitorum profundus tenosynovium and carpal bones on MRI (white arrow, tophi infiltration). (B) Urate crystal and lymphocyte infiltration show chronic tophaceous arthritis (H-E stain, ×200). (C) When examined with a polarizing filter, they are yellow when aligned parallel to the axis of the red compensator, but they turn blue when aligned across the direction of polarization (ie, they exhibit negative birefringence).
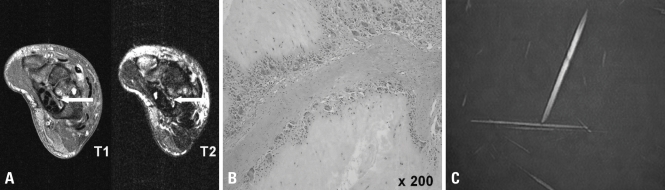
In 3 CTS cases with calcifying mass, 1 patient had both wrists involved and both were operated. There was no palpable mass or diffuse swelling on physical examination, however, tenderness on the volar aspect of wrist existed. Calcified mass was visible in the carpal tunnel view, and CT and MRI were taken in order to identify the exact location, border of lesion, and the involvement of around tissue. In all the cases, the location of the mass was directly above the capitate, and the mass had clear margin (Fig. 3). Conventional open transverse carpal ligament release surgery and mass removal were performed, and the patient's symptoms improved progressively. Histologic examination showed amorphous calcified material encapsulated with fibrous membrane.
Fig. 3.
Calcifying mass was noted on carpal tunnel view and wrist CT. (A) Carpal tunnel view. (B) Wrist axial CT (white arrow, calcifying mass).
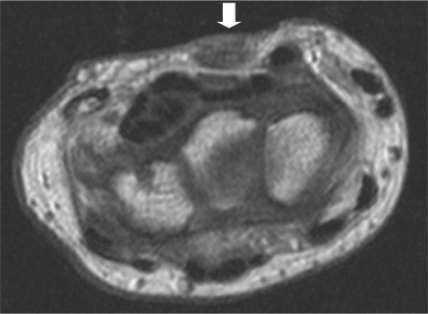
In 1 case, the patient had CTS due to hypertrophy of palmaris longus, and there was diffuse swelling on the volar wrist area. This patient was diagnosed as CTS through electrophysiologic study. An additionally performed MRI examination showed hypertrophy of the palmaris longus muscle and compression of the outer side of the carpal tunnel (Fig. 4). Open transverse carpal ligament release was performed, and hypertrophic palmaris longus was excised. Postoperatively, the pain and paresthesia were completely relieved.
Fig. 4.
Hypertrophied palmaris longus is compressing the carpal tunnel on MRI (white arrow, hypertrophied palmaris longus muscle).
DISCUSSION
CTS is known to be the most common compressive neuropathy in the hand. The carpal tunnel is a very small isolated area consisting of the carpal bones and fibrous tissue, where 9 flexor tendons and 1 median nerve pass through. Although most cases of CTS are idiopathic, the identifiable cause could be the SOL, such as the swelling of tendon sheath, distal radius fracture, rheumatoid arthritis, volar dislocation of lunate, ganglion and gout, etc. Systemic causes of the disease could be DM, hypothyroidism, acromegaly, pregnancy, and amyloidosis .
Idiopathic CTS is generally known to occur bilaterally. According to Bagatur et al.,11 66% of patients with unilateral CTS symptoms exhibit abnormal results in nerve conduction tests on contralateral hand. Therefore, when patient's symptoms and nerve conduction test show unilateral abnormalities, it is necessary to suspect other reasons for CTS besides idiopathic CTS. Nakamichi et al.9 reported that out of 20 patients with abnormal unilateral symptoms and unilateral positive electrophysiologic tests, besides 7 (35%) idiopathic adults, the rest of the patients (65%) showed various causes for median nerve compression, such as occult ganglion, occult calcified mass, tuberculous synovitis, nonspecific synovitis, etc. There are earlier studies on CTS due to SOL such as, lipoma,8 hemangioma,2 synovial sarcoma,12 fibroma of tendon sheath,4 ganglion,13 calcifying mass,3 and tuberculous tenosynovitis.6
In order to rule out SOLs in unilateral CTS patients who exhibit swelling or palpable mass in the volar wrist area during physical examination or patients who exhibit radioopaque lesion discovered during plain X-ray, further special studies (ultrasonogram, CT, MRI) should be performed.13-16 Recently, arthroscope or minimal invasive surgery has been preferred, however, in cases such as this 1 involving SOLs, symptoms does not improve unless open transverse carpal ligament release is performed in conjunction with removal of the SOL. Based on this study, it is important to perform special tests such as CT or MRI to identify the SOL through physical examination when unilateral CTS patients exhibit swelling or tenderness of volar wrist crease area.13-16 The use of MRI scans is an excellent way to examine soft tissue, and also has the advantage to make it possible diagnose exact location and border of lesion and also involvement of surrounding tissue. However, CT scans are superior to MRI with regard to detection of bony lesion. Ultrasonogram has its advantages such as wide availability, lower cost, and shorter examination time, however, accurate characteristics of SOL cannot be identified. Therefore, ultrasonogram was not used in our study.
Although after operative treatment of CTS, there are some cases where proper symptoms of CTS will not alleviated. When a detailed physical examination reveals that a patient exhibits swelling or tenderness on the area of wrist flexion creases, an initial carpal tunnel view test should be administered. Furthermore, if necessary, CT and/or MRI should be conducted to identify the cause of the SOL near the carpal canal so that this information can be used to decide the precise treatment method.
References
- 1.Backhouse KM, Churchill-Davidson D. Anomalous palmaris longus muscle producing carpal tunnel-like compression. Hand. 1975;7:22–24. doi: 10.1016/0072-968x(75)90029-7. [DOI] [PubMed] [Google Scholar]
- 2.Coessens B, De Mey A, Lacotte B, Vandenbroeck D. Carpal tunnel syndrome due to an haemangioma of the median nerve in a 12-year-old child. Ann Chir Main Memb Super. 1991;10:255–257. doi: 10.1016/s0753-9053(05)80292-3. [DOI] [PubMed] [Google Scholar]
- 3.Edwards AJ, Sill BJ, Macfarlane I. Carpal tunnel syndrome due to dystrophic calcification. Aust N Z J Surg. 1984;54:491–492. doi: 10.1111/j.1445-2197.1984.tb05430.x. [DOI] [PubMed] [Google Scholar]
- 4.Evangelisti S, Reale VF. Fibroma of tendon sheath as a cause of carpal tunnel syndrome. J Hand Surg Am. 1992;17:1026–1027. doi: 10.1016/s0363-5023(09)91052-8. [DOI] [PubMed] [Google Scholar]
- 5.Chen WS. Median-nerve neuropathy associated with chronic anterior dislocation of the lunate. J Bone Joint Surg Am. 1995;77:1853–1857. doi: 10.2106/00004623-199512000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Kang HJ, Park SY, Shin SJ, Kang ES, Hahn SB. Tuberculous tenosynovitis presenting as carpal tunnel syndrome. J Korean Soc Surg Hand. 2000;5:137–141. [Google Scholar]
- 7.Kerrigan JJ, Bertoni JM, Jaeger SH. Ganglion cysts and carpal tunnel syndrome. J Hand Surg [Am] 1988;13:763–765. doi: 10.1016/s0363-5023(88)80144-8. [DOI] [PubMed] [Google Scholar]
- 8.Kremchek TE, Kremchek EJ. Carpal tunnel syndrome caused by flexor tendon sheath lipoma. Orthop Rev. 1988;17:1083–1085. [PubMed] [Google Scholar]
- 9.Nakamichi K, Tachibana S. Unilateral carpal tunnel syndrome and space-occupying lesions. J Hand Surg [Br] 1993;18:48–49. doi: 10.1016/0266-7681(93)90236-9. [DOI] [PubMed] [Google Scholar]
- 10.Pai CH, Tseng CH. Acute carpal tunnel syndrome caused by tophaceous gout. J Hand Surg [Am] 1993;18:667–669. doi: 10.1016/0363-5023(93)90315-t. [DOI] [PubMed] [Google Scholar]
- 11.Bagatur AE, Zorer G. The carpal tunnel syndrome is a bilateral disorder. J Bone Joint Surg Br. 2001;83:655–658. doi: 10.1302/0301-620x.83b5.11350. [DOI] [PubMed] [Google Scholar]
- 12.Weiss AP, Steichen JB. Synovial sarcoma causing carpal tunnel syndrome. J Hand Surg [Am] 1992;17:1024–1025. doi: 10.1016/s0363-5023(09)91051-6. [DOI] [PubMed] [Google Scholar]
- 13.Nakamichi K, Tachibana S. Ultrasonography in the diagnosis of carpal tunnel syndrome caused by an occult ganglion. J Hand Surg [Br] 1993;18:174–175. doi: 10.1016/0266-7681(93)90099-2. [DOI] [PubMed] [Google Scholar]
- 14.Horch RE, Allmann KH, Laubenberger J, Langer M, Stark GB. Median nerve compression can be detected by magnetic resonance imaging of the carpal tunnel. Neurosurgery. 1997;41:76–82. doi: 10.1097/00006123-199707000-00016. discussion 82-3. [DOI] [PubMed] [Google Scholar]
- 15.Kamolz LP, Schrögendorfer KF, Rab M, Girsch W, Gruber H, Frey M. The precision of ultrasound imaging and its relevance for carpal tunnel syndrome. Surg Radiol Anat. 2001;23:117–121. doi: 10.1007/s00276-001-0117-8. [DOI] [PubMed] [Google Scholar]
- 16.Yesildag A, Kutluhan S, Sengul N, Koyuncuoglu HR, Oyar O, Guler K, et al. The role of ultrasonographic measurements of the median nerve in the diagnosis of carpal tunnel syndrome. Clin Radiol. 2004;59:910–915. doi: 10.1016/j.crad.2004.03.020. [DOI] [PubMed] [Google Scholar]