Abstract
Background
As childhood obesity has reached epidemic proportions globally, how best to promote active children is undefined. One approach has been through the use of pedometers. In the present study we investigated the accuracy of measuring walking steps with commercially available pedometers and an Accelerometer-based Step-counter in normal and overweight children. Our primary hypothesis was that commercially available pedometers are not an accurate measure of walking steps in normal and overweight children whilst walking. Our secondary hypothesis was that the Accelerometer-based Step-counter provides an accurate measure of walking steps in normal and overweight children.
Methods
Thirteen boys (11 ± 1 year) and fourteen girls (11 ± 1 year) ranging in BMI from 15–27 kg/m2 (sixteen normal and eleven overweight or obese) were recruited. Each child wore four pedometers at the waist and one Accelerometer-based Step-counter on each ankle. Steps were manually counted and energy expenditure measured while the child walked on the treadmill at 0.5, 1, 1.5 and 2 mph, each for 5 minutes. The step-counting devices were also validated whilst children walked on level ground at self-selected pace.
Results
For the commercially available pedometers at the lowest speed of 0.5 mph the percentage error approximated 100% for both the pedometers. At the fastest speed of 2.0 mph the percent approximated 60%. Conversely the Accelerometer-based Step-counter showed a percent error of 24 ± 22% (mean ± SD) at 0.5 mph, however as walking speed increased the error declined to 5 ± 8% at 1.0 mph, 4 ± 5% at 1.5 mph and 2 ± 2% at 2.0 mph. The relationship between steps counted and walking energy expenditure showed good linear correlation (r2≥0.86).
Conclusion
Commercially available pedometers are less accurate for measuring walking and require discretion in their use in children. The accuracy of the Accelerometer-based Step-counter enables it to be used as a tool to assess and potentially promote physical activity in normal and overweight children.
Keywords: pedometers, obesity, energy expenditure, children, walking, physical activity
Background
Childhood obesity has reached epidemic proportions globally.1 Over the last 30 years, 17% of the children population ages 2–19 years in the US have become obese.2 There is supporting evidence that the steady decline in physical activity and our current diet and have a major role in the development of the obesity epidemic.3,4
The question about how best to assess and promote active children remains uncertain. One approach has been through using pedometers.5 These step-counting devices are readily available and inexpensive and can be used to monitor walking or monitoring an exercise treatment.6 Early studies suggest that pedometers may be inaccurate for step counting in children.7 The accuracy of these devices in the normal and obese population has not been studied in detailed, so we should be cautious when recommending them.
In the present study we investigated the accuracy of step counting of commercially available pedometers in normal and overweight children compared to a gold standard of manual step counting. Also we examined an Accelerometer-based Step-counter. Our primary hypothesis was that commercially available pedometers are inaccurate for measuring walking steps in normal and overweight children during low walking speeds. Our secondary hypothesis was that the Accelerometer-based Step-counter is accurate for measuring walking step counts in normal and overweight children. In order to evaluate the relevance of these instruments for energy balance, we also examined the predictive power of the devices with respect to energy expenditure.
Materials and Methods
Subjects
Twenty seven healthy children of varying age (8–12 years), thirteen male (11 ± 1 year) and fourteen girls (11 ± 1 year) ranging in BMI from 15–27 Kg/m2 were recruited through local advertisement (Table 1). Sixteen subjects (6 males and 10 females) were considered normal according to their BMI (5th percentile<BMI<85th percentile for age and sex) and eleven (7 male and 4 female) were considered overweight or obese (BMI ≥ 85th percentile for age and sex).
Table 1.
Characteristics of normal and overweight study participants and Mean Energy Expenditure during different speeds. Values shown are mean ± SD.
| Group (n=27) | Normal (n=16) | Overweight (n=11) | |
|---|---|---|---|
| Age, mean ± SD, y | 11 ± 1 | 10.9 ± 1.4 | 10.8 ± 1.2 |
| Height, mean ± SD, cm | 145 ± 22 | 146.2 ± 11.1 | 142.8 ± 33.3 |
| Gender, male/female, n | 13/14 | 6/10 | 7/4 |
| Weight, mean ± SD, Kg | 47 ± 24 | 36.4 ± 7.6 | 62.9 ± 29.9 |
| BMI, mean ± SD, Kg/m2 | 19 ± 4 | 16.8 ± 1.7 | 22.9 ± 2.8 |
| BMI, percentile, mean ± SD | 61 ± 32 | 41 ± 23 | 92 ± 4 |
| BMI z score, mean ± SD | 0.5 ± 1 | −0.28 ± 0.67 | 1.5 ± 0.34 |
| Fat mass, mean ± SD, Kg | 12.5 ± 8.4 | 7.5 ± 4.2 | 19.8 ± 7.6 |
| Energy expenditure, mean ± SD, Kcal/h | |||
| REE | 60.5 ± 11.3 | 54.7 ± 10.4 | 69 ± 6.2 |
| 0.5mph | 127.8 ± 25.5 | 117.1 ± 21.6 | 143.4 ± 23 |
| 1.0mph | 139.5 ± 28.8 | 128.2 ± 25.5 | 156 ± 25.9 |
| 1.5mph | 155.4 ± 29.9 | 143.1 ± 26.2 | 173.4 ± 26.5 |
| 2.0mph | 171.6 ± 37.8 | 151.7 ± 28.5 | 200.6 ± 30.8 |
Fat mass by Dual Energy X-ray Absorptiometry (DXA), Energy Expenditure by Indirect Calorimeter
Pedometers and Accelerometer-based Step-counter
Two popular pedometers, a piezoelectric (Omron HJ-105, Kyoto, Japan (OM)) and a spring-levered (Yamax Digi-Walker SW-200, Lees Summit, Missouri (YX200)) and a dual-axis accelerometer (Accelerometer-based Step-counter (AS) (Stepwatch, OrthoCare Innovations, Seattle, Washington)) were examined to determine the accuracy of walking steps in normal and overweight children. A total of four pedometers were placed on the waistband, in the midline of the thigh, following manufacturers’ recommendations. Each model was placed on the right and left side of the body. Pedometers were proximal but not touching each other, with the OM on the external and the YX200 on the internal side. One AS unit was placed on the inside of the left ankle and another on the outside of the right ankle. The AS was programmed with the child height using the manufacturers’ software.
Energy Expenditure
Measurements of energy expenditure were performed using an indirect calorimeter (Columbus Instruments, Columbus, OH). Expired air was collected using a dilution face mask that covered the entire face. A primary gas standard (0.5% CO2, 20.5% O2, balanced N2) was used for gas calibrations. Data were collected every thirty seconds and stored on a personal computer. Weekly alcohol burn experiments showed CO2 and O2 recoveries of ≥99%.
Body Composition
Height and weight were measured without shoes and wearing light clothing using a calibrated stadiometer-scale (Seca 644 hand-rail scale, Seca 245 measuring rod, Seca, Hanover, MD). Dual Energy X-ray Absorptiometry (DXA) was performed to assess body composition (GE Medical Systems, Lunar Prodigy, Madison, WI).
Protocol
The child was instructed to fast (water allowed) for at least 6 hrs before arriving at the Clinical Research Unit. All participants wore light clothing and comfortable shoes. The child’s height and weight was measured. After arriving to the laboratory the study personal placed the pedometers and AS on the child as described above. The child rested in a dimly-lit quiet room for 30 minutes. Resting energy expenditure (REE) was then measured for 20 minutes using indirect calorimetry as described above. During the REE measurement, the child was awake, semi-recumbert (10° head bed tilt), lightly clothed and in thermal comfort (68 to 74 °F). The child was asked not to talk or move during the REE measurement. The child was allowed to watch age-appropriate videos during the experiment. After measuring REE, the child was given a small snack (e.g. crackers and juice). After the snack, the indirect calorimetry mask was then replaced and the child then walked on the calibrated treadmill (True 600, St. Louis, Missouri) at 0.5, 1, 1.5 and 2 mph, each for 5 minutes. Steps were manually counted by the same trained investigator and facilitated by an electronic counter (Fisher Scientific, model 07-905-2, Pittsburgh, PA). After all the speeds were completed, the indirect calorimetry mask was removed and the child was allowed to rest for 5 minutes. The child was then asked to walk for 230 meters on level ground at their own pace, followed by the investigator while steps were again counted and the walked timed. Throughout the study, the pedometers were reset at the beginning and read at the end of each walking period. Time-stamped data from the AS was downloaded at the end of the study. The testing protocol was approved by the Mayo Clinic’s Pediatric and Adolescent Medicine Research Committee and the Institutional Review Board. Informed written assent was obtained from the child and informed written consent was obtained from the parent.
Statistical Analyses
Height, weight, age, gender, and BMI, were calculated for each participant. BMI percentiles were calculated by using the BMI calculator for Child and Teen from the Centers for Disease Control and Prevention (CDC) website. The measured height to the nearest 0.1 cm and weight to the nearest 0.1 Kg, together with the sex, date of birth and date of measurement were entered. To address our primary hypothesis that the commercially available pedometers OM and YX200 are not an accurate measure of walking steps in normal and overweight children during low walking speeds, we compared the steps counted manually to the steps counted by the pedometers at the four different speeds. Accuracy was described by the fraction of counts with respect to manual counts. The difference between the pedometers on different sides at each speed was also calculated. The same approach was used to address our secondary hypothesis that the Accelerometer-based Step-counter is an accurate measure of walking steps in normal and overweight children. Bland Altman plots were graphed of the steps reported by the device against the gold standard (manual counts). To address a sub-hypothesis that steps-counted correlated with energy expenditure at the different velocities; regression analysis was used for each subject to examine the relationship between AS counts, weight, and walking energy expenditure at 0 (standing), 0.5, .01, 1.5 and 2.0 mph. The analysis was conducted by randomly sampling the entire data set without replacement in order to generate a data set consisting of 20 elements (five observations at four speeds) with 0 mph speeds included. To address the difference between normal and overweight children, ANOVA and post-hoc unpaired t-test were used. Statistical analyses were conducted with StatView 5.0 (SAS Institute, Cary, NC). Data are expressed as mean ± standard deviation unless otherwise stated. Statistical significance was defined at P<0.05.
Results
The protocol was tolerated well by all the children. For the entire group (Table 1), the children (11 ± 1 years of age; 13 boys and 14 girls) were of mean height (145 ± 22 cm) and mean weight (47 ± 24 Kg); BMI was 19 ± 4 Kg/m2. Sixteen of the children were normal according to their BMI (mean BMI percentile: 41 ± 23; mean BMI z score: −0.28 ± 0.67), and 11 children were obese or overweight (mean BMI percentile: 92 ± 4; mean BMI z score: 1.5 ± 0.34). Twenty six children were white/not of Hispanic origin and 1 child was Asian.
Reproducibility of all the devices (pedometers and AS) was accessed by comparing the steps counted by each device on both sides of the body at all speeds. The mean difference ± SEM for the OM was 10 ± 3%, for the YX200 was 9 ± 3% and for the AS was 3 ± 1%. The total number of steps manually counted in the study was 64011 steps.
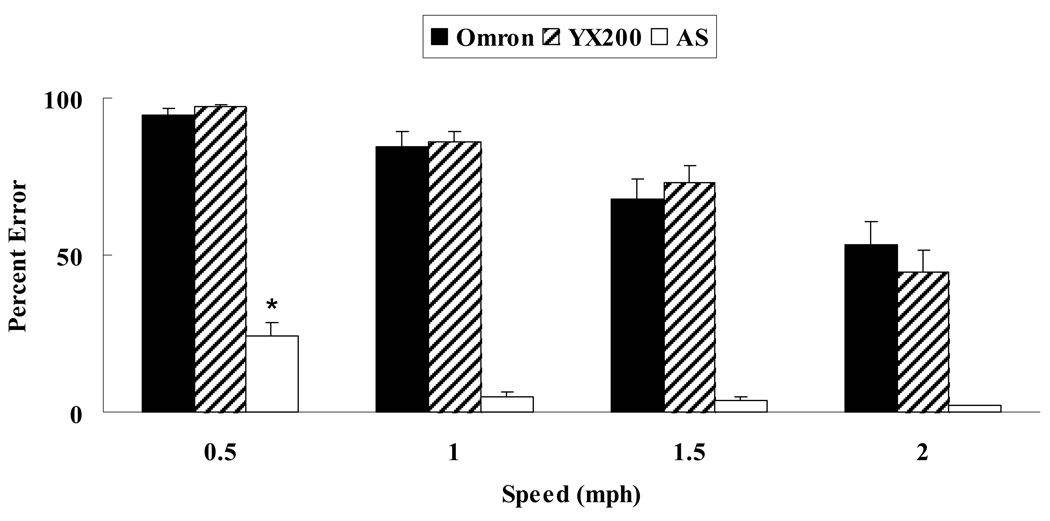
To address our primary hypothesis, that the commercially available pedometers OM and YX200 are not an accurate measure of walking steps in normal and overweight children during low walking speeds, we compared the accuracy of the commercially available pedometers against the gold standard of manual counting. From Figure 1 it is clear that the pedometers were inaccurate. The percent error for both pedometers decreased with each increase in speed. At the lower speed of 0.5 mph the percent error was close to 100% for both the pedometers. However at the fastest speed of 2.0 mph the percent error was approximately 60%. The percent errors were 92% from under-reporting and close to 8 % for over-reporting.
Figure 1.
Pedometer error at the four different walking speeds. Steps were manually counted for all participants (n = 27) while children walked at 0.5, 1.0, 1.5, and 2.0 mph. The manual counts were compared to the steps observed on the pedometers and AS during a 5-minute period. Error is the mean ± SEM at each speed. * Significantly greater error compared to all other speeds, P < 0.0001.
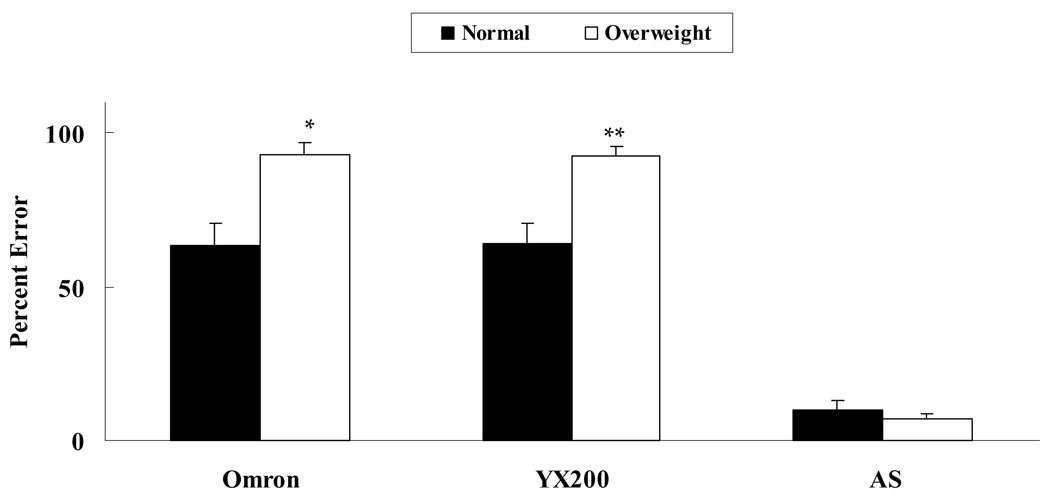
Overall for the normal subjects the pedometers showed a lower percent error compared to the overweight children (OM (p<0.0001), YX200 (p=0.0002)) (Fig 2). This was true for all the speeds we studied. Across all speeds, there were no significant differences in the errors by sex.
Figure 2.
Pedometer error by body category. Steps were manually counted for normal (n = 16) and overweight (n = 11) children. The manual counts were compared to the steps observed on the pedometers and AS during a 5-minute period. Error is the mean ± SEM for all speeds, by weight category. *Significantly greater error in overweight children compared to normal children, P < 0.0001. **Significantly greater error in overweight children compared to lean children, P < 0.0002.
To address our secondary hypothesis, that the AS is an accurate measure of walking steps in normal and overweight children, we compared the accuracy of the AS against our gold standard of manual counting (Fig 1). The percent error was 24 ± 22% at 0.5 mph. As the speed increased the error declined to 5 ± 8% at 1.0 mph, 4 ± 5% at 1.5 mph and 2 ± 2% at 2.0 mph. The difference (ANOVA) between 0.5 mph and the other speeds was significantly greater (p<0.0001).
Overall for the Accelerometer-based Step-counter, the percent error between the normal and overweight was not significantly different (Fig 2). The AS accuracy did not differ by sex.
When children walked at their own pace, the average speed was 2.5 ± 0.3 mph. When this was compared to the 2.0 mph walk on the treadmill (Fig 1), it was seen that the percent error improved somewhat for the commercially available pedometer. For the OM the percent error was 36 ± 8% and for the YX200 was 21 ± 6%. The AS performed well on the treadmill and at the free living walking (5 ± 0.6%).
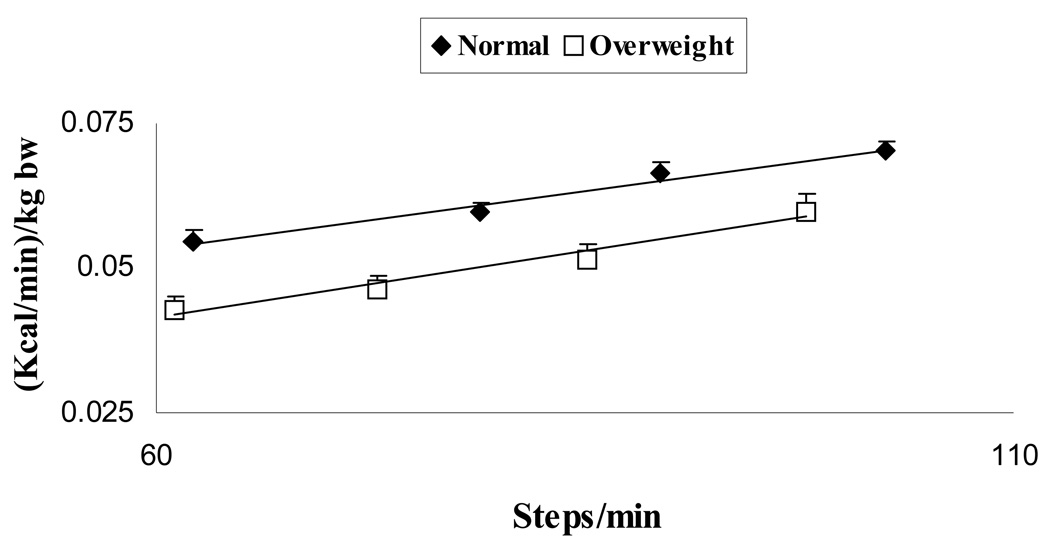
To examine whether walking step rates correlate with walking energy expenditure at the different velocities, linear regression analysis was used. When comparing the relationship between steps counted and walking energy expenditure there were good linear correlation for step counting versus velocity for walking on the treadmill when corrected for weight and fat free mass (Fig 3). With progressive increase in velocity, there was progressive increase in EE (Table 1). There was no significant difference in the in the slope and intercept of these relationships for the normal and overweight children. The iterated multiple linear regressions with 0 mph values included yielded a mean r2 = 0.86 (max r2 = 0.92, min r2 = 0.76) and significant coefficients and regressions in all 50 iterations. A unifying equation for converting steps to energy expenditure is:
| (1) |
Figure 3.
Relationship between manual step counting and energy expenditure. Steps were manually counted (steps/minute) and energy expenditure (kcal/minute) was measured using indirect calorimetry for normal (n = 16) and overweight (n = 11) children. Energy expenditure was adjusted for body weight. Values shown are mean ± SEM.
Discussion
One important factor contributing to the pediatric obesity epidemic is the low levels of physical activity.3, 4 Decreased walking is a major contributing factor.8 Hence pedometers may seem a good option to monitor walking in children. However, many attempts to use them in adults and children have shown that they lack accuracy and precision.7, 9, 10, 11 Commercially available pedometers do not correlate well with walking steps and this may not satisfy expectations, especially when offering them to obese children as tools to assess physical activity. The objective of the present study was to examine the accuracy of two commercially available pedometers and an Accelerometer-based Step-counter. We found that the Accelerometer-based Step-counter was more accurate than the commercially available pedometers we tested, for measuring walking steps in children. Our principal findings are equally true for treadmill and free living walking.
A likely explanation for the decreased accuracy of the commercially available pedometers is two fold. First, at low speeds the acceleration and displacement at the hip, especially in children, is insufficient in magnitude to cause the internal mechanism to count a step.12 Studies have shown that a force of 0.35 × g or more may be needed to register a step.9 Second, the pedometers have to be worn at the waist in a vertical plane to floor in order to count a step; however obese children may wear the pedometer tilted or at an angle due to increased waist circumference. This may explain why pedometers perform so poorly, especially in overweight children.
The Accelerometer-based Step-counter proved to be more accurate. It is accurate for any weight category even at slow walking. This may be because it will respond not only to vertical, but also to horizontal acceleration of the ankle.12. The Accelerometer-based Step-counter, we suggest, could be an excellent tool for researchers interested in monitoring physical activity in high risk populations, where the impact of a particular exercise treatment needs to be evaluated. Prescribing physical activity to our obese population could be easily facilitated using such a device, were it less expensive, more readily available and able to provide direct feedback to the patient.
We recognize the study has limitations. First, the experiment was conducted in a laboratory and not in the free-living state. Second, our study was relatively small; although it was conducted meticulously, so that a larger study would be unlikely to alter the primary findings. Third we did not include children with extremely high BMI and we were limited to a particular pre-pubertal group. Fourth, we examined speeds of 2.0 mph or less. This was done due to safety reasons and because we know from previous studies that children tend to walk 77% of the time at a low level of physical activity intensity. They engage in very short bursts of intense physical activity interspersed with varying intervals of activity of low and moderate intensity.13 Finally the measurements were only done once on each participant. Overall we think that the limitations of our study did not invalidate our results.
Conclusions
Lack of physical activity is a major contributing factor to the obesity epidemic. The solution to how best to assess and promote physical activity in children remains uncertain. Pedometers are readily available and inexpensive and are often used to monitor physical activity or to prescribe exercise. These data however suggest that commercially available pedometers are less accurate for measuring lower levels of activity in normal and overweight children and thus require caution in their use. On the other hand, the accuracy of the Accelerometer-based Step-counter allows it to be considered as an alternative to assess physical activity in children, especially for researchers.
Practitioners taking care of overweight and obese children should be aware of the disadvantages of commercially available pedometers. For the time being while other devices are being evaluated as intervention tools for obesity prevention and treatment, other traditional ways for weight management as lifestyle modifications focused on healthy diet and exercise_14 should be sought in this population.
Acknowledgments
This work was supported by DK 66270, DK 63226, HD 52001 and M01-RR00585.
Abbreviations
- AS
Accelerometer-based Step-counter
- DXA
Dual Energy X-ray Absorptiometry
- REE
Resting Energy Expenditure
- EE
Energy Expenditure
- OM
Omron
- YX200
Yamax Digiwalker
Footnotes
No Conflict of interest or financial disclosures
References
- 1.Jones KL. Role of obesity in complicating and confusing the diagnosis and treatment of diabetes in children. Pediatrics. 2008;121:361–368. doi: 10.1542/peds.2007-1234. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of Overweight and Obesity in the United States 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 3.Lanningham-Foster L, Nysse LJ, Levine JA. Labor saved, calories lost: the energetic impact of domestic labor-saving devices. Obes Res. 2003;11:1178–1181. doi: 10.1038/oby.2003.162. [DOI] [PubMed] [Google Scholar]
- 4.Levine JA, Lanningham-Foster LM, McCrady SK, et al. Interindividual variation in posture allocation: possible role in human obesity. Science. 2005;307:584–586. doi: 10.1126/science.1106561. [DOI] [PubMed] [Google Scholar]
- 5.Stovitz SD, VanWormer JJ, Center BA, Bremer KL. Pedometers as a means to increase ambulatory activity for patients seen at a family medicine clinic. J Am Board Fam Pract. 2005;18:335–343. doi: 10.3122/jabfm.18.5.335. [DOI] [PubMed] [Google Scholar]
- 6.Jakicic JM. Exercise in the treatment of obesity. Endocrinol Metab Clin North Am. 2003;32:967–980. doi: 10.1016/s0889-8529(03)00075-6. [DOI] [PubMed] [Google Scholar]
- 7.Beets MW, Patton MM, Edwards S. The accuracy of pedometer steps and time during walking in children. Med Sci Sports Exerc. 2005;37:513–520. doi: 10.1249/01.mss.0000155395.49960.31. [DOI] [PubMed] [Google Scholar]
- 8.Levine JA, Shelly K, Lanningham-Foster LM, Kane P, Foster R, Manohar C. The Role of Free-Living Daily Walking in Human Weight Gain and Obesity. Diabetes. 2008;57:548–554. doi: 10.2337/db07-0815. [DOI] [PubMed] [Google Scholar]
- 9.Melanson EL, Knoll JR, Bell ML, et al. Commercially available pedometers: considerations for accurate step counting. Prev Med. 2004;39:361–368. doi: 10.1016/j.ypmed.2004.01.032. [DOI] [PubMed] [Google Scholar]
- 10.Schneider PL, Crouter SE, Lukajic O, Bassett DR., Jr Accuracy and reliability of 10 pedometers for measuring steps over a 400-m walk. Med Sci Sports Exerc. 2003;35:1779–1784. doi: 10.1249/01.MSS.0000089342.96098.C4. [DOI] [PubMed] [Google Scholar]
- 11.Crouter SE, Schneider PL, Bassett DR., Jr Spring-levered versus piezo-electric pedometer accuracy in overweight and obese adults. Med Sci Sports Exerc. 2005;37:1673–1679. doi: 10.1249/01.mss.0000181677.36658.a8. [DOI] [PubMed] [Google Scholar]
- 12.Karabulut M, Crouter SE, Bassett DR., Jr Comparison of two wait-mounted and two ankle-mounted electronic pedometers. Eur J Appl Physiol. 2005;95:335–343. doi: 10.1007/s00421-005-0018-3. [DOI] [PubMed] [Google Scholar]
- 13.Bailey RC, Olson J, Pepper SL, Porszasz J, Barstow TJ, Cooper DM. The level and tempo of children's physical activities: an observational study. Med Sci Sports Exerc. 1995;27:1033–1041. doi: 10.1249/00005768-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Barlow SE. Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120 Suppl 4:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]