Abstract
A biopsychosocial perspective was employed to assess associations among situational and psychosocial variables related to health, health care, and HIV/AIDS risk behaviors among 479 homeless men (age 18–64). Poor health was not significantly associated with sexual risk behaviors and was only modestly associated with injection drug use (IDU). Health care was not significantly associated with sexual risk behavior or IDU. HIV/AIDS risk behaviors were highly associated with homelessness severity and post-traumatic stress disorder (PTSD). IDU was significantly associated with greater emotional distress and was more likely among younger men and among white men. Sexual risk behavior was more frequent among those who had particularly poor quality housing such as living on the street or in abandoned buildings. Because interactions with the medical community are limited and not associated with HIV/AIDS risk, outreach in areas in which homeless men congregate, mental health and substance abuse treatment, and permanent supportive housing may help reduce HIV risk among homeless men more effectively.
Keywords: HIV/AIDS risk, homeless men, health utilization, IDU, permanent supportive housing
Homelessness in the United States is a major public health and social service concern. The National Alliance to End Homelessness (NAEH) (2007) estimates that there are over 800,000 homeless persons in the United States and more individuals flow in and out of homelessness at various times. Homeless persons tend to experience a wide range of mental and physical health problems, all of which are exacerbated by poor housing (Burt, Aron, Lee, & Valente, 2001; Schanzer, Dominguez, Shrout, & Caton, 2007). Compared to housed individuals, homeless persons have high rates of chronic disease and are at higher risk for HIV/AIDS. Men, furthermore, are more likely to be homeless, as well as experience longer episodes of homelessness when compared to women (Burt et al., 2001; Kingree, Stephens, Braithwaite, & Griffin, 1999; Phelan & Link, 1999; Williams, 2003). In addition, they are less likely than women to access social services (Calsyn & Morse, 1990).
Health and health care utilization among the entire homeless population is low (Kushel, Vittinghoff, & Haas, 2001). Specific vulnerabilities reported among homeless people such as substance abuse, mental illness, severity of homelessness, and competing needs lead to significant barriers to obtaining health care (e.g., Bhui, Shanahan, & Harding, 2006; Gelberg, Andersen, & Leake, 2000; Kushel, Gupta, Gee & Haas, 2006; Stein, Andersen, Koegel, & Gelberg, 2000). Homeless persons are severely lacking in the financial and non-financial resources necessary to meet their personal and health care needs. Despite their low income, only 28% of homeless persons receive income maintenance. Further, 55% do not have medical insurance, compared to 17% of the general population (U.S. Department of Health and Human Services [USDHHS], 2003).
Homeless men, in particular, have multiple risk factors for poor health as well as HIV/AIDS when compared to women (Williams, 2003). Homeless men have higher rates of alcohol and substance use disorders, injection drug use (IDU), and risky sexual behaviors (Linn, Brown, & Kendrick, 2005; North, Eyrich, Pollio, & Spitznagel, 2004; Zugazaga, 2004). Men are more likely to reside in transient living conditions, and have a higher risk of engaging in risky behaviors that can lead to infection. Single homeless men tend to be older and to have experienced homelessness longer than single homeless women and homeless women with children (Burt et al., 2001; Williams, 2003). Homeless men also are more likely to have been incarcerated (Zugazaga, 2004) which is associated with poorer health outcomes among homeless people (Kushel, Hahn, Evans, Bangsberg, & Moss, 2005). In a sample of homeless persons with co-occurring disorders, homeless men had experienced considerably higher rates of trauma than women (Christensen, Hodgkins, Garces, Estlund, Miller, & Touchton, 2005).
The present study conducted among a large sample of homeless men residing in the Skid Row area of Los Angeles, California, uses an extended biopsychosocial perspective to examine associations among and the impact of situational and psychosocial variables on health and use of services as well as HIV/AIDS risk behaviors (Borrell-Carrió, Suchman, & Epstein, 2004; Engel, 1977; Frankel, Quill, & McDaniel, 2003; Kaslow, Bollini, Druss, Glueckauf, Goldfrank, Kelleher et al., 2007). The model employed in this study includes varied components representing key aspects of domains of the Biopsychosocial Model including biological characteristics (e.g., age and health), psychological factors (e.g., post-traumatic stress, emotional distress), and social factors such as social support. Taking into account the whole person in terms of their biology, psychology, and social environment has been described as optimum in the health care, medical education, and service delivery realm (Frankel & Quill, 2005; Kaslow et al., 2007). However, the Biopsychosocial Model has not been used with great frequency in HIV-related research. Such an approach may hold promise due to the interplay of biological, psychological, and social factors among HIV-risk health behaviors and use of services (Mkanta & Uphold, 2006).
Situational Variables
Social support, poor housing quality, and severity of homelessness are important situational variables to explore in regards to homelessness (Kingree et al., 1999). In general, greater social support is associated with a wide array of positive outcomes and has been shown to be helpful to the homeless and to improve their quality of life (Benda, 2006; Lam & Rosenheck, 2000). Homeless adults receiving greater positive social support, for example, are less likely to report depressive symptoms (Berg, Nyamathi, Christiani, Morisky, & Leake, 2005). Severity of homelessness has been reported to be a critical variable in the prediction of various maladaptive outcomes among homeless persons (e.g., Caton et al., 2005; Stein, Andersen et al., 2000; Stein, Lu, & Gelberg, 2000). Forney, Lombardo, and Toro (2007) reported that an extended time of homelessness is associated with more risky sexual behaviors and a greater risk of contracting HIV. Caton et al. (2005) identified that a shorter duration of homelessness was associated with greater family support and other positive attributes such as better coping skills and absence of a substance abuse or arrest history.
Quality of housing among the homeless varies from residing in supportive housing to living on the streets. Research continues to highlight the effectiveness of permanent supportive housing in ameliorating homelessness (NAEH, 2007). Further, homeless persons who are involved in more stable housing and sheltering programs are more likely to utilize health care (Kushel et al., 2001; O’Toole, Gibbon, Hanusa, & Fine, 1999; Nyamathi, Leake & Gelberg, 2000; Schanzer et al., 2007). Unsheltered homeless persons are more likely to receive acute and episodic care (O’Toole et al., 1999), and experience trauma and victimization (Wenzel, Koegel, & Gelberg, 2000). This study examines whether quality of housing is associated with HIV risk behaviors including IDU and sexual risk behaviors as well as health care utilization, especially among men. Nyamathi et al. (2000) identified that non-sheltered homeless women were more likely to report fair or poor health, and report more use of alcohol or non-injection drugs, to have multiple sexual partners and to have a history of physical assault.
Age and ethnicity are included as situational variables. Older individuals tend to report worse health and the health disadvantage among general minority populations is widely known. Whether this extrapolates within the already-disadvantaged homeless population is open to question but also should be included as an important control. Both age and African-American ethnicity have been identified as risk factors for homelessness itself (Kingree et al., 1999). Regarding ethnicity, Stein, Lu et al. (2000) reported that the health disadvantage among African-Americans was the case for birth outcomes among homeless women. However, Stein, Andersen, and Gelberg (2007) reported a disadvantage among homeless white women in other variables such as more illness, and less preventive care than among African-American women.
Psychosocial & Health-related Variables
Mental disorders are more prevalent among homeless people than among those in the general population (Bhui et al., 2006). In addition to high rates of depression and schizophrenia in this population, posttraumatic stress disorder (PTSD) is prevalent as well. One study exploring violence and the homeless reported that 92% of the homeless men reported one or more PTSD symptoms in their lifetime (North, Smith, & Spitznagel, 1994). Depressive symptoms among the homeless have been associated with risky sexual behaviors, such as multiple partners (Berg et al., 2005). However, relationships between psychiatric disorders and risky behaviors associated with HIV have not been well documented among the homeless (Forney et al., 2007).
Homeless persons have poorer physical health when compared to the general population (Schanzer et al., 2007). Within the homeless population, poorer health has been associated with greater age just as it is in more normative populations (Stein et al., 2007). As described above, men are more likely to be homeless and to engage in a variety of behaviors that put their health at risk (Williams, 2003). The current study examines the relationship of men’s self-reported health to situational, psychosocial, and HIV risk behaviors.
Behavioral outcomes
Health care utilization, injection drug use (IDU), and sexual risk behaviors serve as outcome variables. In general, health care utilization among homeless individuals is low (Kushel et al., 2001) and often consists of exigent care rather than preventive outpatient care that could keep the homeless person from becoming severely ill needing hospitalization or care in an emergency room (Stein et al., 2007). HIV risk behaviors, prevalent among the homeless, include injection drug use, sex with injection drug-using partners, needle-sharing, sex trading, and unprotected sex (Ball, Cobb-Richardson, Connolly, Bujosa, & O’Neall, 2005; Forney et al., 2007;Metraux, Metzger, & Culhane, 2004; Stein, Nyamathi, Ullman & Bentler, 2007).
The model assesses whether pertinent biopsychosocial variables predict (or predict negatively) health care utilization in addition to the HIV risk behaviors of IDU and sexual risk behaviors. Utilization is defined in this current paper as having a regular place to go for care such as a clinic or private office, and outpatient visits. Exigent service utilization so common among the homeless, such as emergency room use and hospitalizations, was not included as appropriate use of services.
Hypothetical model
In addition to assessing the significance of bivariate associations among the variables of interest, a model is tested in which the background situational factors (social support, severity of homelessness, age, ethnicity, and housing quality) predict psychosocial factors of PTSD and emotional distress and health status. In turn, all of these variables predict the behavioral outcomes of IDU, sexual risk behavior, and health care utilization. Because this model is cross-sectional, it is possible that influences go in other directions. However, one goal of the analysis is to observe whether health status is associated with HIV/AIDS risk behaviors. Because poor health drives utilization more in homeless and impoverished populations than in the general population, the explicit association that was included between utilization and poor health served as a control in assessing the associations among health and HIV risk behaviors as well as use of services among those at risk for HIV/AIDS.
Methods
Participants and procedures
This study uses baseline information from an ongoing longitudinal study evaluating the effectiveness of an intervention encouraging completion of a hepatitis A and B vaccine series among homeless adults in the Skid Row area of Los Angeles. Data were collected between September 2003 and June 2006 from 664 participants of whom 479 were heterosexual males (8 men self-identified as homosexual and were deleted from this current sample). Participants were eligible for the intervention if they satisfied the following requirements: 1) age 18–65 residing in one of 16 participating homeless sites; 2) willing to undergo hepatitis A virus, hepatitis B virus (HBV), hepatitis C virus and Human Immunodeficiency Virus (HIV) antibody testing at baseline and at six-month follow-up; 3) willing to participate in the intervention; and 4) no history of HBV vaccination. Positivity for HBV was grounds for exclusion from the study. The UCLA Human Subjects Protection Committee provided oversight of all study activities.
The entire sample was 75% male, 14% White, 70% African-American, 13% Hispanic, 1% other; 2% mixed. The average age was 42 years (S.D. = 9.0; range = 19–65 years). Demographics of the heterosexual male sample were similar to those of the entire sample. The males’ average age was 42 years (S.D. 8.9, range = 20–64). The males were about 71% African-American, 14% White, 13% Hispanic, less than 1% mixed, and 2% other. Twenty-eight percent had not graduated from high school, 44% were high-school graduates, and 27% reported college or other post-high school education. Fifty-five percent had never been married, 7% were married, 36% were separated or divorced, and 2% were widowed. (See Table 1).
Table 1.
Sociodemographic characteristics of the male sample (N = 479).
| Characteristic | % (n) |
|---|---|
| Race/ethnicity | |
| African American | 70.6 (338) |
| Hispanic | 13.1 (63) |
| White | 14.0 (67) |
| Mixed | 0.4 (2) |
| Other | 1.9 (9) |
| Education | |
| = < 11 years | 28.2 (136) |
| 12 years (High school or GED) | 44.1 (212) |
| 13–16 years | 27.2 (131) |
| Marital status | |
| Never married | 54.7 (262) |
| Married | 7.1 (34) |
| Separated | 10.4 (50) |
| Divorced | 25.5 (122) |
| Widowed | 2.3 (11) |
Participating shelters were stratified by type (emergency versus residential recovery) and size and randomized to one of three treatment programs. Flyers were posted at recruitment sites to inform residents of the study and presentations were held at the sites. After written informed consent to screening was obtained, outreach workers administered a brief questionnaire covering basic socio-demographic characteristics and a hepatitis-related health history designed to assess eligibility for the vaccination study. Homeless adults that were HBV negative as assessed by a blood test then provided final written informed consent for the study and were administered the larger baseline survey used in the current study.
Measures
Instruments utilized in the study had been previously tested, modified, and validated for impoverished and/or homeless African-American, Latino, and White adults. Several of the constructs used in the current model are represented as latent variables. They were created from multi-item scales from the baseline questionnaire and are described in more detail below.
Situational Predictors
Social Support
An 18-item scale used in the RAND Medical Outcomes Study (MOS) measured Social Support (Sherbourne & Stewart, 1991). Single items inquired how often various forms of support are available to them if they need it (e.g., “someone you can count on to listen to you when you need to talk”). Items were rated from 1 (none of the time) to 5 (all of the time). Coefficient alpha was high among the items (Coefficient α =.97). To avoid too many indicators, the 18 scores were randomly combined into parcels of 6 to obtain 3 mean indicators for Social Support. Parceling is acceptable in structural modeling especially when alpha coefficients are high (Yuan, Bentler, & Kano, 1997).
Severity of Homelessness was indicated by 2 items
The number of times they had been homeless and the number of years (percent of life) they had been homeless in their lifetimes. This variable representing homelessness severity has been used in prior research (e.g., Stein, Lu, et al., 2000; Stein & Nyamathi, 2004). To avoid a spuriously high correlation between age and years of homelessness, percent of lifetime homeless was calculated and used in the analysis rather than years.
Although the entire sample is classified as homeless and considered to be poorly housed, Poor quality housing was indicated by their reporting that their usual place to spend the night in the last 30 days was an abandoned building, a car or other vehicle, on the street or other outdoor place (1 = poor housing, 0 = not one of the above categories). Twenty-nine percent of the sample reported poor quality housing.
Demographics include single items representing ethnicity (African-American = 1, all others = 0; White = 1, all others = 0) and age in years. Hispanics and others were used as the reference groups for ethnicity.
Intervening Psychosocial and Health-related Variables
Post-traumatic Stress Disorder (PTSD) was indicated by responses to the PTSD Symptoms Checklist. There were 7 items that were combined into 3 indicators (Coefficient α =.98). Items were scaled from 1 (not at all or only 1 time) to 4 (5 or more times a week/almost always) and were based on the most upsetting physical or sexual event that they had experienced. For example, “having upsetting thoughts or pictures about the event that come into your head when you don’t want them to.”
Poor Health Status was indicated by 4 indicators including 1) an assessment of their health on a 1–5 scale ranging from excellent (1) to poor (5); 2) a rating of their bodily pain in the past 6 months ranging from none (1) to very severe (6); 3) an average score from the 10-item MOS physical functioning scale (Stewart, Hays, & Ware, 1988; Stewart & Ware, 1993). Items range from 1 (no trouble) to 3(a lot of trouble) and assess whether, for example, they have trouble with lifting, climbing, bending, or walking various distances; 4) the mean response to an eleven-item scale (yes =1)/no =0) assessing specific illness symptoms or illnesses in the past 6 months, e.g., repeated indigestion or upset stomach, cardiac pain, skin infections, pneumonia.
Emotional Distress was measured by responses to the 5-item Mental Health Index (MHI) subscale from the RAND Health Survey SF-36 (Ware & Sherbourne, 1992) that assesses mood in the previous 4 weeks. Scores range from 1 (all of the time) to 6 (none of the time) and were reverse scored where appropriate so that higher scores indicate more distress. Sample items include: “I was downhearted and blue,” “I was a happy person.” All 5 items were used as a separate indicator. Another emotional distress variable consisted of a total-item score from the 16-item Center for Epidemiological Studies Depression (CES-D) scale (Radloff, 1997) that assesses the frequency of depressive symptoms in the previous week on a 4-point response scale ranging from 1 (rarely or none of the time) to 4 (most of the time). The items were reverse-scored as appropriate, and summed.
Health-related Behavioral Outcomes
Injection Drug Use (IDU) risk behavior in the past 6 months was indicated by yes/no responses to injection of cocaine, heroin, heroin mixed with cocaine (speedballs), speed, needle-sharing, and having a sex partner who injects drugs.
Sexual Risk Behavior in the past 6 months was indicated by responses to 3 items. These items were the average number of times per week they had sex without a condom for 1) sexual intercourse, 2) oral sex, and 3) anal sex.
Health Care Utilization was indicated by 1) whether they are currently able to receive care at a regular place for care such as a clinic or from a private doctor, 2) whether they had visited a clinic or private doctor in the past 6 months.
Analysis
The analyses were performed using the EQS structural equations program (Bentler, 2006). Latent variable analysis allows one to evaluate causal hypotheses with correlational, non-experimental data. Goodness-of-fit of the models was assessed with the maximum-likelihood χ2 statistic, the Comparative Fit Index (CFI), the Satorra-Bentler χ2 (S-B χ2), the Robust Comparative Fit Index (RCFI), and the root mean squared error of approximation (RMSEA) (Bentler, 2006). The Robust S-B χ2 was used in addition to the maximum likelihood χ2 because it is more appropriate when data depart from multivariate normality. The CFI and RCFI range from 0 to 1 and reflect the improvement in fit of a hypothesized model over a model of complete independence among the measured variables. CFI and RCFI values at .95 or greater are desirable, indicating that the hypothesized model reproduces 95% or more of the covariation in the data. The RMSEA is a measure of lack of fit per degrees of freedom; values less than .06 indicate a good fit between the hypothesized model and the observed data.
An initial confirmatory factor analysis (CFA) assessed the adequacy of the hypothesized measurement model and the associations among the latent and single-item variables. Then a latent variable path model positioned the situational (Social Support, Chronic Homelessness, and Poor Housing) and demographic variables (age, ethnicity) as predictors of the psychosocial and health-related variables of PTSD, Poor Health Status, and Emotional Distress which served as intervening variables. All variables then predicted the health-related behavioral outcomes of IDU, Sexual Risk Behaviors, and Health Care Utilization.
Results
Confirmatory Factor Analysis
Table 2 reports summary statistics of the measured variables and the factor loadings of the hypothesized factor structure. All factor loadings were significant (p ≤.001). Fit indexes for the CFA model were all excellent: ML χ2 = 723.32, 430 df; CFI =.96, RMSEA =.038, 90% confidence interval for RMSEA (CI) =.033 to .042; S-B χ2 = 570.33, 430 df; RCFI =.97; RMSEA =.026, CI =.020 to .032. Although the initial fit of the model was outstanding, two supplemental covariances were added between error residuals: one between the two reverse scored items from the RAND MHI and one between injection of speedballs and injecting cocaine. These supplementary relationships appear reasonable in light of their high associations with each other and their addition improved the fit further.
Table 2.
Summary statistics and factor loadings in the CFA model.
| Variables | Mean (SD) | Factor Loading |
|---|---|---|
| Situational Variables | ||
| Social Support | ||
| Support 1 | 3.26 (1.20) | .91 |
| Support 2 | 3.13 (1.25) | .98 |
| Support 3 | 3.07 (1.29) | .93 |
| Severity of Homelessness | ||
| Number of Times | 3.22 (4.48) | .68 |
| % life homeless | 8.50 (9.90) | .56 |
| Age (years) | 42.28 (8.95) | — |
| African-American (Yes/No) | 0.71 (.46) | — |
| Caucasian/White (Yes/No) | 0.14 (.35) | — |
| Poor Housing Quality (Yes/No) | 0.29 (.45) | — |
| Psychosocial and Health-related Variables | ||
| PTSD | ||
| Post 1 | 0.50 (0.84) | .94 |
| Post 2 | 0.52 (0.86) | .99 |
| Post 3 | 0.51 (0.85) | .96 |
| Poor Health Status | ||
| Health rating | 2.54 (1.11) | .54 |
| Pain rating | 2.16 (1.44) | .67 |
| Low physical function | 0.53 (0.44) | .59 |
| Mean number of illnesses | 0.53 (1.31) | .59 |
| Emotional Distress | ||
| Very nervous | 2.55 (1.55) | .62 |
| Calm & peaceful (R) | 3.11 (1.48) | .57 |
| Downhearted | 2.56 (1.39) | .75 |
| Happy (R) | 3.08 (1.45) | .59 |
| In the dumps | 2.07 (1.38) | .61 |
| CES-D Composite | 16.56 (11.19) | .75 |
| Health-related Behavioral Outcomes | ||
| IDU | ||
| Cocaine | 0.02 (0.13) | .49 |
| Heroin | 0.05 (0.21) | .81 |
| Heroin-Cocaine (speedballs) | 0.02 (0.14) | .80 |
| Speed | 0.02 (0.15) | .37 |
| Share needles | 0.06 (0.23) | .78 |
| IDU sex partner | 0.040.21) | .65 |
| Sexual Risk Behavior | ||
| One week freq. intercourse, no condom | 1.18 (2.36) | .78 |
| One week freq. oral sex, no condom | 1.08 (2.21) | .91 |
| One week freq. anal sex, no condom | 0.17 (0.78) | .37 |
| Health Care Utilization | ||
| Place to get health care | 0.15 (0.36) | .51 |
| Number of visits (last 6 months) | 0.27 (0.45) | .54 |
All factor loadings significant, p ≤.001. (R) = reverse-scored.
Table 3 reports the correlations among the variables in the model. Examining significant associations within Table 3 from top to bottom, Greater Social Support was significantly associated with being younger, better health, less emotional distress, less IDU, and better housing quality. Older homeless men reported worse health, were less likely to report IDU, were more likely to utilize health care, were more likely to be African-American, were less likely to be White, and were more likely to have poor housing quality (e.g., streets, cars, abandoned buildings). Chronic Homelessness was most associated with PTSD, Poor Health, Emotional Distress, IDU, Sexual Risk Behavior, not being African-American, and being white. It was modestly but significantly associated with healthcare utilization and poor quality housing. PTSD was most highly associated with Poor Health, Emotional Distress, IDU, Sexual Risk Behavior (modestly), more Healthcare Utilization, and was more associated with white men. African-Americans were less likely to report PTSD. Poor Health was significantly associated with Emotional Distress, modestly with IDU, and, not surprisingly, quite a bit with Healthcare Utilization (.64). Emotional Distress was significantly associated with greater IDU, poor housing quality, and was more prevalent among the white males. IDU was associated only modestly with Sexual Risk Behavior (.11) and was more prevalent among white males (.25) and less prevalent among the African-American males (−.33). More Sexual Risk Behavior was associated with poor housing quality.
Table 3.
Correlations among latent and measured variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Social Support | — | ||||||||||
| 2. Age | −.15*** | — | |||||||||
| 3. Severity of Homelessness | −.13* | .05 | — | ||||||||
| 4. PTSD | −.10* | −.07 | .20*** | — | |||||||
| 5. Poor Health | −.18*** | .28*** | .22*** | .20*** | — | ||||||
| 6. Emotional Distress | −.33*** | −.06 | .26*** | .30*** | .39*** | — | |||||
| 7. IDU | −.13** | −.13** | .19*** | .15** | .11* | .25*** | — | ||||
| 8. Sexual Risk Behavior | −.03 | −.01 | .23*** | .12* | .00 | .10 | .11* | — | |||
| 9. Healthcare utilization | .03 | .32*** | .20* | .19** | .64*** | .05 | −.07 | .03 | — | ||
| 10. African-American | .05 | .32*** | −.17** | −.12** | −.01 | −.12* | −.33*** | .01 | .01 | — | |
| 11. Caucasian/white | −.03 | −.20*** | .19** | .18*** | .05 | .17** | .25*** | −.03 | −.05 | NA | — |
| 12. Poor housing quality | −.18*** | .18*** | .11* | −.05 | .09 | .12** | .06 | .16*** | .10 | .10* | −.08 |
= p <.05,
p <.01;
p <.001
Predictive Path Model
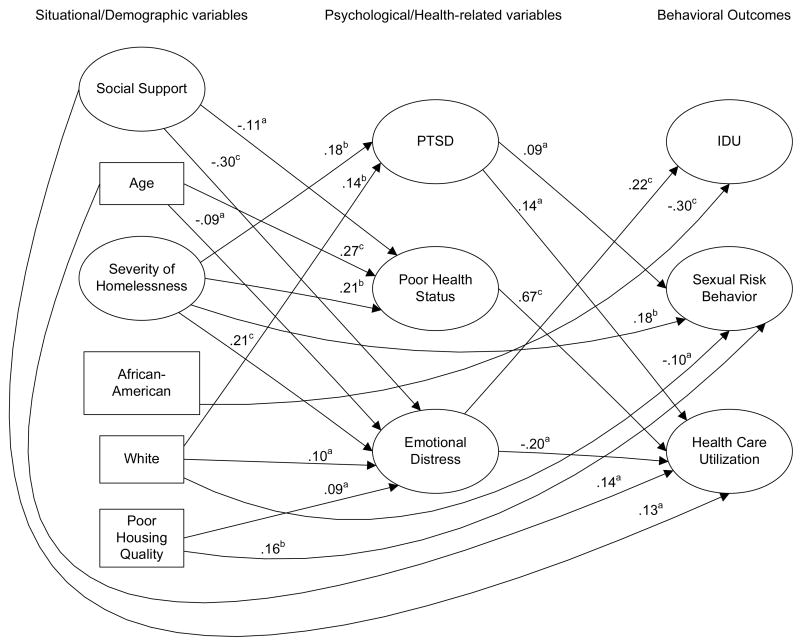
The final predictive structural equation model is presented in Figure 1 after non-significant paths and covariances were gradually deleted. The figure indicates the logical flow of influences from the background demographic and situational factors to the intervening psychosocial and health status factors which in turn predicted the outcome behaviors. Associations among the predictors are not depicted for readability but are similar to those reported in Table 3. No paths or correlations were added to this model. Fit indexes for the final path model were very good: ML χ2 = 759.45, 463 df; CFI =.96, RMSEA =.037, CI =.032 to .041; S-B χ2 = 600.68, 463 df; RCFI =.97; RMSEA =.025, CI =.019 to .030.
Figure 1.
Final structural path model depicting influences of situational, demographic, psychosocial, and health status variables on HIV risk behaviors and health care utilization among 479 homeless men. Arrows represent regression paths. All regression coefficients are standardized. The large circles designate latent variables; the rectangles represent measured variables. a p <.05; b p <.01; c p <.001.
Direct Effects
PTSD was predicted by Chronic Homelessness and white ethnicity. Poor Health Status was predicted by Chronic Homelessness, less Social Support, and greater age. Emotional Distress was predicted significantly by less Social Support, younger age, Chronic Homelessness, and Poor Quality Housing. IDU was predicted by Emotional Distress, and was less likely among African-Americans. Sexual Risk Behavior was predicted by PTSD, Chronic Homelessness, Poor Quality Housing, and was less likely among the white males. Health Care Utilization was predicted by more PTSD, Poor Health Status, less Emotional Distress, more Social Support, and greater age.
Indirect Effects mediated through the intervening variables were assessed for their significance. Social Support negatively impacted and Severity of Homelessness positively impacted IDU. These indirect influences would have flowed through Emotional Distress. Greater age and Severity of Homelessness had significant and positive indirect effects on Health Care Utilization which were probably mainly mediated through Poor Health Status.
Discussion
The outstanding fit of the model confirms the high degree of interconnectedness and relatedness of the variables within the model. These results highlight the usefulness of components of the biopsychosocial model in assessing relations among variables related to health and health risk among homeless men (e.g., Mkanta & Uphold, 2006). The structural equation model consists of cross-sectional variables so influences may be flowing in directions other than those pictured or in a bi-directional fashion. However, this model depicted one way that one can conceptualize the flow of behaviors among a group of highly interconnected variables that are pertinent to health and health risk behaviors.
This population is considered to be at high risk for HIV/AIDS and the psychosocial and situational correlates of their health and health-risk behaviors provide important areas in which meaningful interventions can occur to encourage better health and fewer risk behaviors. The health-related variables indicating poor health and health care use were minimally associated with HIV risk behaviors. Neither good health nor bad health impacted their high risk behaviors to any appreciable extent. There was only a very small relationship between sexual risk behaviors and IDU. Metraux et al. (2004) reported that there was limited support for positing homelessness among IDUs as independently associated with sharing needles but also did not discover other high HIV/AIDS risk behaviors highly associated with IDU among the homeless, especially sexual behaviors. Furthermore, within this vulnerable population, minority ethnicity did not signal a worse situation. Rather, the white men were the most likely to report severity of homelessness, use injection drugs, and report more PTSD and greater emotional distress.
Infrequent interactions with the medical community cannot be depended upon to decrease HIV/AIDS risk behavior among homeless men. Healthcare utilization among men who are homeless is driven by poor health as the very large association between poor health status and utilization indicates. Alternatives for decreasing HIV risk behaviors among homeless men are through other venues and through recognition of associations among other variables that are pertinent to HIV risk behaviors. This would include better housing, substance abuse treatment, and treatment for mental illness. Susser, Valencia, and Conover (1993) observed that male psychiatric patients in homeless shelters are relatively inaccessible to preventive interventions but they may be reached during the course of their treatment in shelter programs.
The predictive model points out the centrality of severity of homelessness even within a sample that by definition is all homeless. This finding shows that homeless males are not a homogeneous group but are very heterogeneous with a need to be evaluated individually, with their life histories given consideration, especially in their health-related variables and susceptibility to HIV/AIDS. Furthermore, poor housing quality was an independent predictor of distress (which predicted more IDU) and more sexual risk behavior. Thus, leverage points for change may arise out of housing considerations. Similar results among homeless women of reproductive age have been found as well (Stein et al., 2007). Women reporting the most homelessness severity also reported other threats to health and more drug use and alcohol problems, greater psychological distress, and a lack of appropriate health care.
Social support was an important part of the model. It was associated with better housing quality, less severity of homelessness, and was more prevalent among younger homeless men. In addition, it predicted considerably less emotional distress and better health status. Benda (2006) identified social support as more important among homeless women than among homeless men. However, there is a role for greater social support in improving both physical and mental health outcomes for homeless men, especially the long-term homeless.
Because homeless persons are in transient living conditions, and thus at a higher risk for engaging in risky behaviors that can lead to infection, housing is a vital piece of HIV prevention. Permanent supportive housing offers homeless individuals the assurance of long-term housing and appropriate services (Martinez & Burt, 2006; Schanzer et al., 2007; U.S. Department of Housing and Urban Development, [USDHUD] 2006). Permanent supportive housing programs operate under the assumption that the combination of permanent housing and ongoing supportive services will foster independence and self-sufficiency among homeless persons (USDHUD, 2006). Residents in permanent supportive housing units receive a rent subsidy, which enables the residents to access resources that will improve their quality of life (USDHUD, 2006).
Stable housing increases the likelihood for a homeless person to seek medical care (Burt et al., 2001; NAEH, 2006; Schanzer et al., 2007). Relying on the emergency room is detrimental not only to the homeless individual, but also to society as a whole because of costs. One month’s stay in a mental hospital would be equivalent to the cost of about 20 months in supportive housing (Bring L.A. Home, 2006). Hospitalization of homeless persons costs 49 times more than supportive housing (Bring L.A. Home, 2006).
Limitations
The predictive model that was tested could have been formulated with a different ordering. However, it has a logical flow in terms of positing a chain of events leading to more HIV/AIDS risk behaviors as well as health care utilization. Also, self-reports of sexual behaviors, substance abuse and health were used. In general, such reports have been found to be reasonably reliable among homeless people, especially for shorter time periods (Klinkenberg, Calsyn, Morse, McCudden, Richmond, & Burger, 2002). A 6-month or shorter recall time was used for most of the variables in the model.
Conclusion
Among the men including in this study, greater sexual risk behavior was predicted most strongly by poor quality housing and severity of homeless. IDU was associated with greater emotional distress and was much less prevalent among African-Americans. Self-reported poor health was not associated highly with either HIV/AIDS risk behavior and poor health was the major impetus for use of healthcare services. HIV/AIDS risk behaviors were not associated with health care utilization at all. The HIV/AIDS prevention needs of homeless men must be addressed outside of the fragile health care system available to the homeless.
Acknowledgments
The authors thank Gisele Pham for secretarial and production assistance. Support for this research was provided by grants 1R01 DA016147 and P01-DA01070-34 from the National Institute on Drug Abuse.
Contributor Information
Judith A. Stein, Department of Psychology, University of California, Los Angeles
Adeline Nyamathi, School of Nursing, University of California, Los Angeles.
Jazmin I. Zane, Department of Social Welfare, University of California, Los Angeles
References
- Ball SA, Cobb-Richardson P, Connolly AJ, Bujosa CT, O’Neall TW. Substance abuse and personality disorders in homeless drop-in center clients: Symptom severity and psychotherapy retention in a randomized clinical trail. Comprehensive Psychiatry. 2005;46:371–379. doi: 10.1016/j.comppsych.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Benda BB. Survival analyses of social support and trauma among homeless male and female veterans who abuse substances. American Journal of Orthopsychiatry. 2006;76:70–79. doi: 10.1037/0002-9432.76.1.70. [DOI] [PubMed] [Google Scholar]
- Bentler PM. EQS 6 structural equations program manual. Encino, CA: Multivariate Software, Inc; 2006. [Google Scholar]
- Berg J, Nyamathi A, Christiani A, Morisky D, Leake B. Predictors of screening results for depressive symptoms among homeless adults in Los Angeles with latent tuberculosis. Research in Nursing & Health. 2005;28:220–229. doi: 10.1002/nur.20074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhui K, Shanahan L, Harding G. Homelessness and mental illness: A literature review and a qualitative study of perceptions of the adequacy of care. International Journal of Social Psychiatry. 2006;52:152–165. doi: 10.1177/0020764006062096. [DOI] [PubMed] [Google Scholar]
- Borrell-Carrio F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: Principles, practice, and scientific inquiry. Annals of Family Medicine. 2004;2:576–582. doi: 10.1370/afm.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt M, Aron LY, Lee E, Valente J. Helping America’s Homeless. Washington, D.C: The Urban Institute Press; 2001. [Google Scholar]
- Calsyn RJ, Morse G. Homeless men and women: Commonalities and a service gender gap. American Journal of Community Psychology. 1990;18:597–608. doi: 10.1007/BF00938062. [DOI] [PubMed] [Google Scholar]
- Caton CLM, Dominguez B, Schanzer B, Hasin DS, Shrout PE, Felix A, et al. Risk factors for long-term homelessness: Findings from a longitudinal study of first-time homeless single adults. American Journal of Public Health. 2005;95:1753–1759. doi: 10.2105/AJPH.2005.063321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen RC, Hodgkins CC, Garces LK, Estlund KL, Miller MD, Touchton R. Homeless, mentally ill and addicted: The need for abuse and trauma services. Journal of Health Care for the Poor and Underserved. 2005;16:615–621. doi: 10.1353/hpu.2005.0091. [DOI] [PubMed] [Google Scholar]
- Engel G. The need for a new medical model: A challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- Forney JC, Lombardo S, Toro PA. Diagnostic and other correlates of HIV risk behaviors in a probability sample of homeless adults. Psychiatric Services. 2007;58:92–99. doi: 10.1176/ps.2007.58.1.92. [DOI] [PubMed] [Google Scholar]
- Frankel RM, Quill TE. Integrating biopsychosocial and relationship-centered care into mainstream medical practice: A challenge that continues to produce positive results. Families, Systems, & Health. 2005;23:413–421. [Google Scholar]
- Frankel RM, Quill TE, McDaniel SH. The biopsychosocial approach: Past, present, future. Rochester: NY: University of Rochester Press; 2003. [Google Scholar]
- Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: Application to medical care use and outcomes for homeless people. Health Services Research. 2000;34:1273–1302. [PMC free article] [PubMed] [Google Scholar]
- Kaslow NJ, Bollini AM, Druss B, Glueckauf RL, Goldfrank LR, Kelleher KJ, et al. Health care for the whole person: Research update. Professional Psychology: Research and Practice. 2007;38:278–289. [Google Scholar]
- Kingree JB, Stephens T, Braithwaite R, Griffin J. Predictors of homelessness among participants in a substance abuse treatment program. American Journal of Orthopsychiatry. 1999;69:261–266. doi: 10.1037/h0080428. [DOI] [PubMed] [Google Scholar]
- Klinkenberg WD, Calsyn RJ, Morse GA, McCudden S, Richmond TL, Burger G. Consistency of recall of sexual and drug-using behaviors for homeless persons with dual diagnosis. AIDS and Behavior. 2002;6:295–307. [Google Scholar]
- Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. Journal of General Internal Medicine. 2006;21:71–77. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushel MB, Hahn JA, Evans JL, Bangsberg DR, Moss AR. Revolving doors: Imprisonment among the homeless and marginally housed population. American Journal of Public Health. 2005;95:1747–1752. doi: 10.2105/AJPH.2005.065094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285:200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- Lam JA, Rosenheck RA. Correlates of improvement in quality of life among homeless persons with serious mental illness. Psychiatric Services. 2000;51:116–118. doi: 10.1176/ps.51.1.116. [DOI] [PubMed] [Google Scholar]
- Linn JG, Brown M, Kendrick L. Injection drug use among homeless adults in the southeast with severe mental illness. Journal of Health Care for the Poor and Undeserved. 2005;16:83–90. doi: 10.1353/hpu.2005.0126. [DOI] [PubMed] [Google Scholar]
- Martinez TE, Burt MR. Impact of permanent supportive housing on the use of acute care health services by homeless adults. Psychiatric Services. 2006;57:992–999. doi: 10.1176/ps.2006.57.7.992. [DOI] [PubMed] [Google Scholar]
- Metraux S, Metzger DS, Culhlane DP. Homelessness and HIV risk behaviors among injection drug users. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2004;81:618–629. doi: 10.1093/jurban/jth145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mkanta WN, Uphold CR. Theoretical and methodological issues in conducting research related to health care utilization among individuals with HIV infection. AIDS Patient Care and STDs. 2006;20:293–303. doi: 10.1089/apc.2006.20.293. [DOI] [PubMed] [Google Scholar]
- National Alliance to End Homelessness (NAEH) Research Reports on Homelessness. Washington, DC: author; 2007. Homelessness Counts. [Google Scholar]
- North CS, Eyrich KM, Pollio DE, Spitznagel EL. Are rates of psychiatric disorders in the homeless population changing? American Journal of Public Health. 2005;94:103–108. doi: 10.2105/ajph.94.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North CS, Smith EM, Spitznagel EL. Violence and the homeless: An epidemiologic study of victimization and aggression. Journal of Traumatic Stress. 1994;7:95–110. doi: 10.1007/BF02111915. [DOI] [PubMed] [Google Scholar]
- Nyamathi AM, Christiani A, Windokun F, Jones T, Strehlow A, Shoptaw S. Hepatitis C virus infection, substance use and mental illness among homeless youth: A review. AIDS, 19, Supplement. 2005;3:S34–S40. doi: 10.1097/01.aids.0000192068.88195.27. [DOI] [PubMed] [Google Scholar]
- Nyamathi AM, Leake B, Gelberg L. Sheltered versus nonsheltered homeless women differences in health, behavior, victimization, and utilization of care. Journal of General Internal Medicine. 2000;15:565–572. doi: 10.1046/j.1525-1497.2000.07007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Toole TP, Gibbon JL, Hanusa BH, Fine MJ. Utilization of health care services among subgroups of urban homeless and housed poor. Journal of Health Politics, Policy and Law. 1999;24:91–114. doi: 10.1215/03616878-24-1-91. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG. Who are the “homeless”? Reconsidering the stability and composition of the homeless population. American Journal of Public Health. 1999;89:1334–1338. doi: 10.2105/ajph.89.9.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Schanzer B, Dominguez B, Shrout PE, Caton CLM. Homelessness, health status, and health care use. American Journal of Public Health. 2007;97:464–469. doi: 10.2105/AJPH.2005.076190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Stein JA, Andersen R, Gelberg L. Applying the Gelberg-Andersen Behavioral Model for Vulnerable Populations to health services utilization in homeless women. Journal of Health Psychology. 2007;12:791–804. doi: 10.1177/1359105307080612. [DOI] [PubMed] [Google Scholar]
- Stein JA, Andersen RM, Koegel P, Gelberg L. Predicting health services utilization among homeless adults: A prospective analysis. Journal of Health Care for the Poor and Underserved. 2000;11:212–230. doi: 10.1353/hpu.2010.0675. [DOI] [PubMed] [Google Scholar]
- Stein JA, Lu M, Gelberg L. Severity of homelessness and adverse birth outcomes. Health Psychology. 2000;19:524–534. [PubMed] [Google Scholar]
- Stein JA, Nyamathi A. Correlates of Hepatitis C infection in homeless men: A latent variable approach. Drug & Alcohol Dependence. 2004;75:89–95. doi: 10.1016/j.drugalcdep.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Stein JA, Nyamathi AM, Ullman J, Bentler PM. Impact of marriage on HIV/AIDS risk behaviors among impoverished high risk couples: A multilevel latent variable approach. AIDS & Behavior. 2007;11:87–98. doi: 10.1007/s10461-005-9058-2. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Hays RD, Ware JE., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Medical Care. 1988;26:724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Ware J. Measuring function and well-being: the medical outcomes study approach. Durham, NC: Duke University Press; 1993. [Google Scholar]
- Susser E, Valencia E, Conover S. Prevalence of HIV infection among psychiatric patients in a New York City men’s shelter. American Journal of Public Health. 1993;83:568–570. doi: 10.2105/ajph.83.4.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) Ending Chronic Homelessness: Strategies for Action. Washington, DC: author; 2003. [Google Scholar]
- U.S. Department of Housing and Urban Development. (USDHUD) Predicting staying in or leaving permanent supportive housing that serves the homeless people with serious mental illness. Washington, DC: author; 2006. [Google Scholar]
- Ware J, Sherbourne C. The MOS 36-item Short-Form Health Survey (SF-36) Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Wenzel SL, Koegel P, Gelberg L. Antecedents of physical and sexual victimization among homeless women: a comparison to homeless men. American Journal of Community Psychology. 2000;28:367–390. doi: 10.1023/A:1005157405618. [DOI] [PubMed] [Google Scholar]
- Williams DR. The health of men: Structured inequalities and opportunities. American Journal of Public Health. 2003;93:724–731. doi: 10.2105/ajph.93.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K-H, Bentler PM, Kano Y. On averaging variables in a confirmatory factor analysis model. Behaviormetrika. 1997;24:71–83. [Google Scholar]
- Zugazaga C. Stressful life event experiences of homeless adults: A comparison of single men, single women, and women with children. Journal of Community Psychology. 2004;32:643–654. [Google Scholar]