Abstract
This study tested the effect of a structured aerobic exercise program on anger expression in healthy overweight children. Overweight, sedentary children were randomly assigned to an aerobic exercise program or a no-exercise control condition. All children completed the Pediatric Anger Expression Scale at baseline and posttest. Anger Out and Anger Expression scores were lower for the exercise condition at posttest. Fitness improvements contributed significantly to final models, and points earned for adherence correlated negatively with posttest Anger Out. An aerobic exercise program might be an effective strategy to reduce anger expression, including reduction of aggressive behavior, in overweight children.
The number of overweight children in the U.S. is at a record high (29) and these children are more likely than their non-overweight peers to have behavior problems (25). Overweight adolescents are also more likely to be bullies and to be bullied (20), and a handful of studies suggest a positive relationship between overweight status and anger expression (21, 26).
Psychological states such as anger and hostility have the potential to adversely affect physical health in childhood and adulthood. Anger, defined as the emotional aspect of hostility, has been shown to increase the risk of cardiovascular disease in adults (12). Adolescents who were more hostile were more likely to have metabolic syndrome 3 years later (32). Behaviorally, anger emotionality in 5 year old children has been shown to be predictive of externalizing problem behaviors at home at age 6 1/2, and at school at age 8 (33). In adolescents, high levels of anger and impulsivity were associated with high levels of delinquency (7). Thus, anger has been linked with both health outcomes and behavioral competence.
There is some literature suggesting a link between anger, physical exercise, and fitness. Physical activity has been shown to improve anxiety and depression in adults (10), adolescents (4), and children (31). Exercise is a component of some anger management treatments (23). An intervention study in adolescents suggested a possible benefit of vigorous exercise on hostility (28). Two studies have reported a relationship of anger with physical fitness level. Stewart et al. highlighted a significant correlation between higher levels of aerobic fitness and desirable scores on an anger survey in adults (35). In a sample of healthy middle aged women, anger scores predicted adverse laboratory values (high cholesterol, triglyceride, and glucose levels), but only for those who were physically unfit (34). Thus, it is possible that exercise can reduce anger and buffer its physical consequences.
We examined whether an exercise intervention designed to decrease cardiovascular risk would reduce anger expression. Given the association of obesity with behavior problems, interventions that effectively address both issues may be particularly useful during the current childhood obesity epidemic. No published studies report effects of an exercise intervention on children's anger expression. This experiment tested the effects of such a program on anger expression in overweight, sedentary children. We hypothesized that children assigned to the exercise group would show improved scores on an anger self-report measure in comparison to a non-exercise control group.
Method
Participants
Two hundred and eight overweight, sedentary children (aged 7-11; mean age = 9.7; SD= 1.1; 57% female; 59% African American) who completed the Pediatric Anger Expression Scale (PAES) (19) at baseline and after an exercise intervention were included in the study. Children were recruited from public elementary schools (2003 - 2006). Healthy black or white children were eligible if they were 7-11 yrs old, overweight (≥85th percentile body mass index, BMI), were not currently participating in a regular physical activity program for more than one hour per week, had no medical condition that would affect study results or limit physical activity (e.g. orthopedic conditions), and attended a school that was included in the study. This study was conducted as part of a larger project examining the effect of exercise on metabolism. Children from whom we were unable to collect blood samples were excluded from the parent study. Study subjects were recruited and intervened upon in 6 cohorts to provide a larger sample size than could be evaluated at one time. Two to three subjects per day completed baseline and posttest measures. Intervention cycles took place from November 2003 through December 2006, for 10-15 weeks each.
Procedure
All children and parents completed the informed consent/assent process. The study was reviewed and approved by the Human Assurance Committee (Institutional Review Board). Children were offered incentives of a savings bond worth $50 (face value at maturity $100) for baseline and a savings bond worth $200 (face value at maturity $400) at posttest for completing an 8-hour day of testing procedures including those reported here.
After baseline testing was complete, a statistician assigned the experimental condition via a computer-generated randomization sequence balanced by race and gender. The study coordinator enrolled participants and shared their randomization status with them. Children were randomly assigned to one of three groups: a no-exercise control condition (n = 69), low dose exercise condition (20 min/d, n = 69) or high dose exercise condition (40 min/d, n = 70). The low and high dose exercise groups were transported daily to and from the gymnasium together, and spent an equal amount of time in the program each day. Children assigned to the control condition were not provided any after-school program or transportation but were asked to continue their usual activities.
Measures
Parents provided information on the child's ethnicity, gender, birth date, medical history, and whether the child was enrolled in any regular physical activity program. Parents also provided information regarding their education level and marital status. Body weight (in shorts and t-shirt) and height (without shoes) were measured with an electronic scale (Detecto, Web City, MO) and stadiometer (Tanita, Arlington Heights, IL) and converted to a BMI z-score (SAS code available from Centers for Disease Control). BMI z-score reflects the number of standard deviations above or below the average value for a child's age and sex based on the current childhood norms (30). Pediatricians conducted physical examinations on all subjects at baseline and assessed pubertal development using Tanner scales.
Anger Expression
The Pediatric Anger Expression Scale (PAES) (19) was completed by all children at baseline and posttest. The construct of anger is considered to be multidimensional, and is usually separated into independent components such as overtly expressed anger, anger turned inward, and anger controlled (13). The PAES is a 15-item self-report inventory, which yields 3 factor analytically derived scales (Anger In, Anger Out, Anger Control; score range 5 - 15 for each scale) and an overall Anger Expression score. Cronbach's alpha coefficients were reported: Anger In = 0.77; Anger Out = 0.77; Anger Control = 0.67; and Anger Expression = 0.60 (19). An independent study showed acceptable psychometric properties of the PAES (internal consistency and temporal stability) and principal component structures that were comparable to the scale authors' findings (27). The Anger In style (e.g. I'm afraid to show my anger, I hide my anger) is indicative of holding in and possibly denying anger. The Anger Out style is anger openly expressed (e.g. I show my anger, lose my temper, slam doors, hit someone), potentially including hostile and aggressive behavior. Anger Control is a more cognitive and less impulsive approach to dealing with anger (e.g. I keep my cool, I control my temper), where an attempt is made to resolve the conflict or frustration. The overall Anger Expression score is calculated with the following formula: (Anger In + Anger Out) - Anger Control.
Aerobic Fitness
Fitness was measured with a graded treadmill test at baseline and posttest (Modified Balke Protocol for Poorly Fit Children; American College of Sports Medicine, 2000) preceded by a warm-up (2 min at 2.5 mph, 0% grade; 2 min at 3.0 mph, 3.0% grade). The test was done on a Monark treadmill. Children were encouraged to walk as long as they could. Instructors stopped the test when children signaled they could not continue, when children had reached maximum according to the standard criteria, or for safety reasons. The indicator of aerobic fitness was the duration of each child's treadmill test (treadmill time, sec) (11).
Percent Body Fat
To measure body fat, dual energy x-ray absorptiometry (QDR 4500W, Hologic Inc., Bedford, MA) segments the body into fat, bone, and fat free soft tissue. Children were scanned at baseline and again at posttest. Percent body fat adjusts for body mass.
Intervention
After-school exercise program
The children assigned to the intervention were provided free transportation via school bus to our research gymnasium, and then home or to a neighborhood school after the exercise classes ended each day. The exercise sessions were held on school day afternoons in the research gymnasium and were instructed by trained research staff. The emphasis was on intensity, enjoyment and safety, not competition nor the enhancement of skills; therefore, activities were selected based on ease of comprehension, fun, and ability to elicit a heart rate (HR) greater than 150 bpm. Examples of these activities include running games, jump rope, basketball, and soccer (16). Children remained at our laboratories for approximately 75 min each day due to time required for changing, water breaks, etc. In the high dose group, two 20 min bouts of intermittent vigorous exercise were done in a fashion consistent with guidelines for children, in short bursts of intense physical activity interspersed with lower intensity activity (recovery) (2, 8). The two exercise groups exercised in the same gymnasium. After the first 20 min bout, the low dose group was escorted to a separate room where they engaged in supervised sedentary activities, while the high dose group completed a second 20 min bout. The children assigned to the exercise programs received 12.8 ± 1.6 weeks of the exercise intervention between baseline and posttest. Children's average attendance was 85% ± 13% of available days between baseline and posttest. Average HR during the classes was 165 ± 8 bpm. There was one serious adverse event (a fracture). Intervention duration, attendance, and HR were similar in low and high dose conditions (p > .05).
Behavioral Structure
Polar HR monitors (S610i; Polar Electro, Oy, Finaland) were used to monitor intensity and incentivize adherence to the exercise dose. Participants who demonstrated good behavior, attended at least 4 days/week, and had an average HR ≥ 150 earned points and chose weekly from prize boxes. The first day of the after-school exercise program was spent reviewing the handbook. Expectations included courtesy, following directions, participation in all activities, and proper use of equipment. Foul language, bullying and fighting were not permitted. If participants misbehaved, consequences ranged from a loss of points for the day, to suspension from exercise sessions or expulsion from the program. Progress reports for each child were provided to parents monthly.
Statistical methods
All data were screened for violations of normality. Because no dose-response effects were found for any of the anger sub-scales, the 20 and 40 minute exercise groups were collapsed. T-tests were used to check baseline group differences on demographic makeup (age, race, gender, parental marital status, and parental education), and also on pubertal stage, body composition and fitness measures, and PAES scales. Correlations were computed between these baseline characteristics, intervention duration, fitness and fatness measures, and PAES scales. To test contributions of group assignment, body fat and physical fitness to posttest anger scores in intent-to-treat analyses, hierarchical multiple regression models were utilized. The same model was used for each of the four scales of the PAES (Anger In, Anger Out, Anger Control, and Anger Expression), with predictor variables entered as follows: demographics, cohort and pubertal stage in step 1, baseline anger scores in step 2, group and interactions with group (race, race × gender, marital status, educational level, age, pubertal stage, baseline percent body fat, and baseline fitness) in step 3, percent body fat change (from baseline to posttest) in step 4, and treadmill time change in step 5. Non-significant interactions were dropped from the final models. To explore possible contributions of the behavioral protocol of the intervention to changes in anger, partial correlations between intervention points and anger scores at posttest, adjusting for all covariates, were examined. Statistical analyses were performed using SPSS 15.0, and statistical significance was assessed using an alpha level of .05.
Results
Baseline and posttest PAES data were obtained from 208 children (mean age 9.4; 59% black; 58% female), and were similar to available normative means (19, 27). At baseline, no significant differences were detected between experimental conditions for demographics, pubertal stage, body composition, fitness, or anger scales. Race, gender, socioeconomic status, age, and pubertal stage of the sample may be viewed in Table 1, along with baseline, posttest, and change scores for the body composition, fitness, and anger measures. There were two significant correlations with pubertal stage, Anger Expression (r = -.19) and BMI z-score (r = .14). Remaining comparisons yielded no significant associations (each |r| < 0.12). T-tests revealed a significant gender difference for the Anger Expression scale at baseline, with boys having higher values than girls (m ± SD; 7.9 ± 3.2 vs. 6.9 ± 3.5; t(219) = 2.15, p = .03).
Table 1.
Characteristics of the sample
| Control (n = 69) | Exercise (n = 139) | |||||
|---|---|---|---|---|---|---|
| Pre | Post | Change | Pre | Post | Change | |
| n or Mean (SD) | Mean (SD) | Mean (SD) | n or Mean (SD) | Mean (SD) | Mean (SD) | |
| Race | ||||||
| White | 30 | 55 | ||||
| Black | 39 | 84 | ||||
| Gender | ||||||
| Male | 26 | 63 | ||||
| Parental marital status a | ||||||
| Married | 21 | 44 | ||||
| Not married | 45 | 82 | ||||
| Parental education b | ||||||
| Partial high school | 2 | 8 | ||||
| High school | 14 | 23 | ||||
| Partial college | 28 | 58 | ||||
| College graduate | 21 | 34 | ||||
| Age (yrs) | 9.8 (1.1) | 9.7 (1.1) | ||||
| Tanner stage | 1.5 (0.9) | 1.4 (0.8) | ||||
| BMI z-score | 2.1 (0.4) | 2.1 (0.4) | -0.01 (0.1) | 2.1 (0.4) | 2.0 (0.5) | -0.08 (0.1) |
| Percent body fat | 40.9 (6.7) | 40.6 (6.3) | -0.32 (2.0) | 40.3 (5.8) | 38.8 (6.1) | -1.46 (2.4) |
| Treadmill time (sec) | 444 (175) | 437 (184) | -6.0 (143) | 485 (198) c | 551 (212) d | 66.0 (198) |
| Pediatric Anger Expression Scale | ||||||
| Anger In | 9.6 (2.2) | 9.7 (2.2) | 0.1 (2.5) | 10.1 (2.4) | 9.8 (2.4) | -0.3 (2.5) |
| Anger Out* | 7.9 (2.2) | 8.5 (2.3) | 0.6 (2.8) | 8.4 (2.5) | 7.9 (2.2) | -0.4 (2.3) |
| Anger Control | 10.8 (2.2) | 10.6 (2.2) | -0.2 (2.1) | 11.0 (2.3) | 11.1 (2.4) | 0.1 (2.5) |
| Anger Expression* | 6.7 (3.8) | 7.6 (3.3) | 0.9 (4.4) | 7.5 (3.2) | 6.7 (3.2) | -0.8 (3.5) |
n = 187
n = 188
n = 138
n = 137
p = .01 for adjusted posttest group differences at step 3
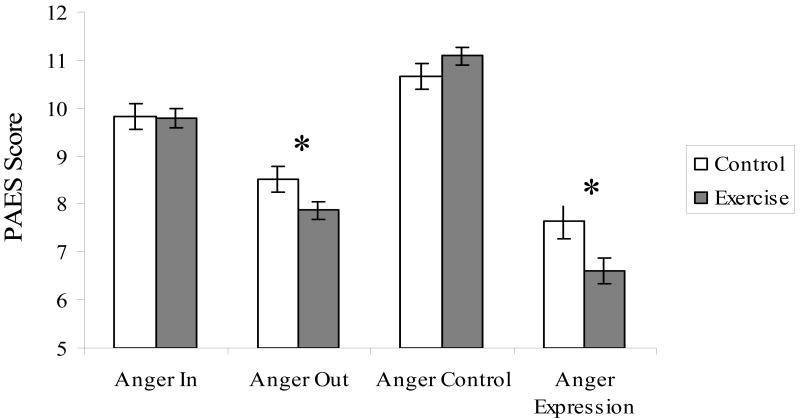
A significant effect of exercise on the Anger Out and Anger Expression scales was detected, with children in the exercise group having lower posttest scores than those in the control condition (adjusted posttest means presented in Figure 1). Regression analyses revealed that along with group and baseline anger score, fitness (i.e., treadmill time) change was also a significant predictor of posttest Anger Out, such that greater improvements in fitness were associated with greater reductions in Anger Out. The effect of group remained significant at steps 4 and 5. Race, gender, marital status, education level, cohort, age, pubertal stage, and change in body fat did not make significant contributions to either model. There were no significant interaction effects in any of the 4 anger scale models. Hierarchical regression models for the Anger Out and Anger Expression scales can be viewed in Table 2. Aside from baseline anger scores, no significant predictors were found for Anger In or Anger Control models.
Figure 1.
Posttest means (SE) by condition for Pediatric Anger Expression Scale, adjusted for race, gender, cohort, parental education, parental marital status, age, pubertal development, baseline anger, and changes in fitness and body fat.
*Exercise condition significantly lower than control condition (p < .05)
Table 2.
Model Fit and Beta-Weights on Hierarchical Regression Analyses Predicting Posttest Anger Out and Anger Expression Scores
| Variable | b | β | p | R2 change | F change |
|---|---|---|---|---|---|
| Dependent Variable: Anger Out | |||||
| Step 1 | |||||
| Age | -.15 | -.07 | .40 | ||
| Race | .13 | -.03 | .72 | ||
| Gender | -.37 | -.08 | .36 | ||
| Cohort | -.07 | -.05 | .49 | ||
| Education | .08 | .04 | .64 | ||
| Marital | .23 | .09 | .23 | ||
| Puberty | .15 | .05 | .60 | .02 | .46 |
| Step 2 | |||||
| Baseline Anger | .43 | .44 | < .001 | .19 | 40.7* |
| Step 3 | |||||
| Group | -.42 | -.18 | .01 | .03 | 6.7* |
| Step 4 | |||||
| Group | -.40 | -.17 | .02 | .001 | .16 |
| Percent Fat Change | .03 | .03 | .69 | ||
| Step 5 | |||||
| Group | -.35 | -.15 | .04 | .03 | 6.1* |
| Treadmill Time Change | -.002 | -.17 | .005 | ||
| Dependent Variable: Anger Expression | |||||
| Step 1 | |||||
| Age | -.21 | -.07 | .40 | ||
| Race | -.30 | -.05 | .57 | ||
| Gender | -.81 | -.13 | .14 | ||
| Cohort | -.02 | -.01 | .90 | ||
| Education | -.18 | -.06 | .47 | ||
| Marital | .35 | .10 | .19 | ||
| Puberty | .07 | .02 | .87 | .03 | 0.9 |
| Step 2 | |||||
| Baseline Anger | .28 | .30 | < .001 | .09 | 17.5* |
| Step 3 | |||||
| Group | -.76 | -.22 | .002 | .05 | 10.0* |
| Step 4 | |||||
| Group | -.72 | -.21 | .004 | ||
| Percent Fat Change | .07 | .05 | .51 | .00 | 0.43 |
| Step 5 | |||||
| Group | -.66 | -.20 | .01 | ||
| Treadmill Time Change | -.002 | -.12 | .09 | .01 | 2.9* |
p < .05
Correlations between intervention points and posttest anger scores were calculated with all covariates partialled out. A significant negative partial correlation was found for the Anger Out scale, r(128) = -.21, p = .016.
Discussion
The results of this study suggest that an after-school aerobic exercise program may reduce or prevent the increase in anger expression among overweight, sedentary children. This is the first study testing the effect of an exercise program on anger in school-aged children. Children assigned to the exercise classes showed decreases at posttest for the Anger Out scale compared to controls, who increased. There was a significant finding on the summary Anger Expression scale, which is attributable to the Anger Out effect. There were no significant changes on the two remaining scales, Anger In and Anger Control. No moderation by race, gender, socioeconomic status, age, pubertal stage, fatness or fitness was observed, indicating generalizability of these results to overweight children. These experimental results extend the growing body of literature showing the beneficial effects of exercise on emotional states in adults, adolescents, and children (4, 10, 31). Effectively reducing anger could be valuable given the extensive literature highlighting the association of anger with cardiovascular events (12). Thus, anger reduction due to exercise may be partly responsible for the cardiovascular benefits of a healthy lifestyle.
Improved fitness, a direct result of the exercise program, was significantly related to lower posttest Anger Out scores. Anger is associated with increased prefrontal lobe activity (17), and previous cross-sectional work has related fitness to improved executive function in children and adults (6, 18), and reduced anger in adults (35). The prefrontal cortex is the locus of executive function, including inhibition and self-control (24). Emotions are generated, integrated with other information, and restrained by the prefrontal cortex (22). Exercise training has been shown to improve executive function in older adults (6), and an improvement in executive function due to exercise has been observed in this sample of overweight children (9). Thus, improvement in executive functioning due to exercise may explain these findings.
While not measured in this study, serotonin has a known association with both exercise and anger expression. In human adults, aggression has been shown to correlate negatively with central nervous system serotonergic activity (5). In rats, exercise has been shown to buffer stress by altering serotonin and norepinephrine brain systems (14). The human prefrontal cortex has a high density of serotonin receptors (3), so this may account for the reduced anger scores observed in the exercise condition.
The reduction in percent body fat, a direct result of the exercise intervention, did not make a significant contribution in explaining reductions in anger scores. The lack of an association may partly be explained by the restriction of range in the sample, which was limited to overweight children. Although children assigned to the exercise condition did lose a statistically significant amount of body fat in comparison to controls (-1.5% vs. -0.3%), all subjects remained overweight at the completion of the intervention. Cross-sectional association of anger with fatness in other studies (21, 26) may be due to fatness acting as an easily measurable marker for inactivity, which may be the underlying cause of mood disturbance.
The significant correlation between points children earned in the intervention and posttest Anger Out scores indicates the contribution of the behavioral protocol to the present finding. Behavioral interventions, most notably cognitive-behavioral therapy, have been successful in reducing anger and aggression in children (36). The present intervention was based on the operant principles of a token economy, which can improve behavior in children (1). Aggressive behaviors such as hitting and pushing were punished if demonstrated in the exercise class, so the intervention was intentionally reinforcing a healthier mode of anger expression, as well as vigorous activity. Therefore, the observed changes in self-reported anger expression may be a result of the structured behavioral protocol used in the exercise classes. Future studies comparing an exercise program to a non-exercise attention control condition are needed to isolate the effects of exercise in children.
Demand characteristics are a possible confound in the present study. First, children were not blinded to experimental condition. The children in the exercise classes had more contact with investigators, and they may have been more eager than controls to please the staff. Attention from staff every day and other aspects of an after-school program could have resulted in a behavior change. Inclusion of an attention control condition could rule out these explanations. Also, anger data was collected using a self -report questionnaire, and some investigators suggest that collecting data about mood in children may best be accomplished by observer ratings in naturalistic settings such as in school or at play (15). Finally, the PAES was normed with a 9-13 year old sample (19) and despite observing similar scores with the present study sample, our age range is slightly lower (7-11 yrs.). It is possible that younger children may not be cognizant of their usual mood state and may be reporting current mood or responding in a desirable fashion. These possible effects were handled statistically by partialing out age in the regression model.
While the anger scores at post were significantly lower in the exercise condition than control condition, the posttest scores in the control condition were similar to the baseline scores in the exercise condition. Therefore, these results must be interpreted cautiously. These findings in a healthy, community sample may not generalize to children with clinically significant behavior problems. However, the small but statistically significant reduction in anger scores observed in this study might accumulate over a longer period of regular exercise activity to make a meaningful difference in a child's likelihood of developing serious behavior problems. Such a small improvement realized across a population of more active children could deliver social benefits. If replicated, these findings may have important implications for children's health and psychosocial adjustment.
The deleterious effects of outward hostility and aggression on cardiovascular health and psychosocial adjustment, along with the value of current anger reduction strategies in children, make the results of the present study appealing. These results are also important in light of the current childhood obesity epidemic. Exercise is inexpensive, simple, and promotes general good health. Including a healthy dose of organized, vigorous physical activity in children's daily lives may be beneficial not only for maintenance of appropriate weight and cardiovascular health, but also for the development of appropriate social behavior.
Acknowledgments
Supported by NIH R01 DK60692 and R01 DK70922. Catrina Creech designed the behavioral contingencies for the exercise program. Kashala Carter, Shena Givens, Sara Groves, Abby Messick, Stephanie Moore, Jennifer Murphy, Ankur Pogula, Laura Power, and Deena Walker are acknowledged for data collection, entry and management.
Footnotes
A preliminary version of this work was presented at the 10th National Conference on Child Health Psychology in Gainesville, Florida, April 20, 2006.
Contributor Information
Joseph Tkacz, Department of Pediatrics, Georgia Prevention Institute, Medical College of Georgia, 1499 Walton Way, HS-1714, Augusta, GA 30912 phone: 706-721-4534, fax: 706-721-7150, email: jtkacz@mcg.edu
Deborah Young-Hyman, Department of Pediatrics, Georgia Prevention Institute, Medical College of Georgia, 1499 Walton Way, HS-1705, Augusta, GA 30912 phone: 706-721-4534, fax: 706-721-7150, email: dounghyman@mcg.edu
Colleen A. Boyle, currently: Department of Nutrition, Syracuse University, 302 Lyman Hall, Syracuse, NY 13244 phone: 315-443-2386, fax: 315-443-2735, email: cboyle@syr.edu
Catherine L. Davis, Department of Pediatrics, Georgia Prevention Institute, Medical College of Georgia, 1499 Walton Way, HS-1711, Augusta, GA 30912 phone: 706-721-4534, fax: 706-721-7150, email: cadavis@mcg.edu
References
- 1.Adams CD, Girolami PA, Joseph KE, Sauvageot SA, Slater H. Use of a token reinforcement system to promote appropriate behavior at a pediatric burn summer camp. J Burn Care Rehabil. 2002;23:297–305. doi: 10.1097/00004630-200207000-00015. discussion 294-296. [DOI] [PubMed] [Google Scholar]
- 2.Bailey RC, Olson J, Pepper SL, Porszasz J, Barstow TJ, Cooper DM. The level and tempo of children's physical activities: an observational study. Med Sci Sports Exerc. 1995;27:1033–1041. doi: 10.1249/00005768-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Biver F, Lotstra F, Monclus M, Wikler D, Damhaut P, Mendlewicz J, Goldman S. Sex difference in 5HT2 receptor in the living human brain. Neurosci Lett. 1996;204:25–28. doi: 10.1016/0304-3940(96)12307-7. [DOI] [PubMed] [Google Scholar]
- 4.Calfas KJ, Taylor WC. Effects of physical activity on psychological variables in adolescents. Pediatric Exercise Science. 1994;6:406–423. [Google Scholar]
- 5.Coccaro EF. Central serotonin and impulsive aggression. Br J Psychiatry Suppl. 1989:52–62. [PubMed] [Google Scholar]
- 6.Colcombe SJ, Kramer AF, Erickson KI, Scalf P, McAuley E, Cohen NJ, Webb A, Jerome GJ, Marquez DX, Elavsky S. Cardiovascular fitness, cortical plasticity, and aging. Proc Natl Acad Sci U S A. 2004;101:3316–3321. doi: 10.1073/pnas.0400266101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colder CR, Stice E. A longitudinal study of interacive effects of imulsivity and anger on adolescent behavvior. Journal of Youth and Adolescence. 1998;27:255–274. [Google Scholar]
- 8.Corbin CB, Pangrazi RP. Pangrazi Physical activity for children: A statement of guidelines. National Association for Sport and Physical Education; Reston, VA: 1998. [Google Scholar]
- 9.Davis CL, Tomporowski PD, Boyle CA, Waller JL, Miller PH, Naglieri J, Gregoski M. Effects of aerobic exercise on overweight children's cognitive functioning: A randomized controlled trial. Research Quarterly for Exercise & Sport. 2007;78:510–19. doi: 10.1080/02701367.2007.10599450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dunn AL, Trivedi MH, O'Neal HA. Physical activity dose-response effects on outcomes of depression and anxiety. Med Sci Sports Exerc. 2001;33:S587–597. doi: 10.1097/00005768-200106001-00027. discussion 609-10. [DOI] [PubMed] [Google Scholar]
- 11.Eisenmann JC, Wickel EE, Welk GJ, Blair SN. Relationship between adolescent fitness and fatness and cardiovascular disease risk factors in adulthood: the Aerobics Center Longitudinal Study (ACLS) Am Heart J. 2005;149:46–53. doi: 10.1016/j.ahj.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 13.Forgays DG, Forgays DK, Spielberger CD. Factor structure of the State-Trait Anger Expression Inventory. J Pers Assess. 1997;69:497–507. doi: 10.1207/s15327752jpa6903_5. [DOI] [PubMed] [Google Scholar]
- 14.Greenwood BN, Foley TE, Day HE, Campisi J, Hammack SH, Campeau S, Maier SF, Fleshner M. Freewheel running prevents learned helplessness/behavioral depression: role of dorsal raphe serotonergic neurons. J Neurosci. 2003;23:2889–2898. doi: 10.1523/JNEUROSCI.23-07-02889.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grunbaum JA, Vernon SW, Clasen CM. The association between anger and hostility and risk factors for coronary heart disease in children and adolescents: a review. Ann Behav Med. 1997;19:179–189. doi: 10.1007/BF02883335. [DOI] [PubMed] [Google Scholar]
- 16.Gutin B, Riggs S, Ferguson M, Owens S. Description and process evaluation of a physical training program for obese children. Research Quarterly for Exercise and Sport. 1999;70:65–69. doi: 10.1080/02701367.1999.10607731. [DOI] [PubMed] [Google Scholar]
- 17.Harmon-Jones E, Sigelman J. State anger and prefrontal brain activity: evidence that insult-related relative left-prefrontal activation is associated with experienced anger and aggression. J Pers Soc Psychol. 2001;80:797–803. [PubMed] [Google Scholar]
- 18.Hillman CH, Castelli DM, Buck SM. Aerobic fitness and neurocognitive function in healthy preadolescent children. Med Sci Sports Exerc. 2005;37:1967–1974. doi: 10.1249/01.mss.0000176680.79702.ce. [DOI] [PubMed] [Google Scholar]
- 19.Jacobs GA, Phelps M, Rohrs B. Assessment of anger expression in children: The pediatric anger expression scale. Personality and Individual Differences. 1989;10:59–65. [Google Scholar]
- 20.Janssen I, Craig WM, Boyce WF, Pickett W. Associations between overweight and obesity with bullying behaviors in school-aged children. Pediatrics. 2004;113:1187–1194. doi: 10.1542/peds.113.5.1187. [DOI] [PubMed] [Google Scholar]
- 21.Johnson EH. Interrelationships between psychological factors, overweight, and blood pressure in adolescents. J Adolesc Health Care. 1990;11:310–318. doi: 10.1016/0197-0070(90)90041-y. [DOI] [PubMed] [Google Scholar]
- 22.Koenigs M, Young L, Adolphs R, Tranel D, Cushman F, Hauser M, Damasio A. Damage to the prefrontal cortex increases utilitarian moral judgements. Nature. 2007;446:908–911. doi: 10.1038/nature05631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Larkin KT, Zayfert C. Anger management training with mild essential hypertensive patients. J Behav Med. 1996;19:415–433. doi: 10.1007/BF01857676. [DOI] [PubMed] [Google Scholar]
- 24.Lezak MD, Howieson DB, Loring DW. Neuropsychological assessment. Oxford University Press; New York: 2004. [Google Scholar]
- 25.Lumeng JC, Gannon K, Cabral HJ, Frank DA, Zuckerman B. Association between clinically meaningful behavior problems and overweight in children. Pediatrics. 2003;112:1138–1145. doi: 10.1542/peds.112.5.1138. [DOI] [PubMed] [Google Scholar]
- 26.Mueller WH, Meininger JC, Liehr P, Chandler PS, Chan W. Adolescent blood pressure, anger expression and hostility: possible links with body fat. Ann Hum Biol. 1998;25:295–307. doi: 10.1080/03014469800005652. [DOI] [PubMed] [Google Scholar]
- 27.Musante L, Treiber FA, Davis HC, Waller JL, Thompson WO. Assessment of self-reported anger expression in youth. Assessment. 1999;6:225–233. doi: 10.1177/107319119900600303. [DOI] [PubMed] [Google Scholar]
- 28.Norris R, Carroll D, Cochrane R. The effects of physical activity and exercise training on psychological stress and well-being in an adolescent population. J Psychosom Res. 1992;36:55–65. doi: 10.1016/0022-3999(92)90114-h. [DOI] [PubMed] [Google Scholar]
- 29.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA: the journal of the American Medical Association. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 30.Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, Grummer-Strawn LM, Curtin LR, Roche AF, Johnson CL. Centers for Disease Control and Prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109:45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 31.Hammack K, Davis CL, Tkacz JP, Young-Hyman D. Exercise effects on self-worth and depression symptoms in overweight children: A randomized controlled trial. Journal of Pediatric Psychology, Revised manuscript under review. 2008 doi: 10.1093/jpepsy/jsp007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raikkonen K, Matthews KA, Salomon K. Hostility predicts metabolic syndrome risk factors in children and adolescents. Health Psychol. 2003;22:279–286. doi: 10.1037/0278-6133.22.3.279. [DOI] [PubMed] [Google Scholar]
- 33.Rydell AM, Berlin L, Bohlin G. Emotionality, emotion regulation, and adaptation among 5- to 8-year-old children. Emotion. 2003;3:30–47. doi: 10.1037/1528-3542.3.1.30. [DOI] [PubMed] [Google Scholar]
- 34.Siegman AW, Malkin AR, Boyle S, Vaitkus M, Barko W, Franco E. Anger, and plasma lipid, lipoprotein, and glucose levels in healthy women: the mediating role of physical fitness. J Behav Med. 2002;25:1–16. doi: 10.1023/a:1013558000465. [DOI] [PubMed] [Google Scholar]
- 35.Stewart KJ, Turner KL, Bacher AC, DeRegis JR, Sung J, Tayback M, Ouyang P. Are fitness, activity, and fatness associated with health-related quality of life and mood in older persons? J Cardiopulm Rehabil. 2003;23:115–121. doi: 10.1097/00008483-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Williams S, Waymouth M, Lipman E, Mills B, Evans P. Evaluation of a children's temper-taming program. Can J Psychiatry. 2004;49:607–612. doi: 10.1177/070674370404900906. [DOI] [PubMed] [Google Scholar]