Abstract
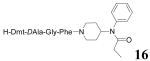
Enkephalin analogues with an 4-anilidopiperidine scaffold have been designed and synthesized to achieve therapeutic benefit for the treatment of pain due to mixed μ and δ opioid agonist activities. Ligand 16, in which a Dmt-substituted enkephalin-like structure was linked to the N-phenyl-N-piperidin-4-yl propionamide moiety showed very high binding affinities (0.4 nM) at μ and δ receptors with an increased hydrophobicity (aLogP = 2.96). This novel lead compound was found to have very potent agonist activities in MVD (1.8 nM) and GPI (8.5 nM) assays.
Introduction
Neuropathic pain, which is associated with disease or injury of the nervous system and characterized by the presence of spontaneous ongoing types of pain, is particularly difficult to treat.1-2 Morphine is a very potent μ opioid agonist and one of the most commonly used drugs in the treatment of pain, even though it has serious side effects such as constipation, tolerance, and dependence for long term usage.2-3 Recent studies have shown that the tolerance to morphine can be reduced by co-administration of a small amount of DPDPE, a well known δ opioid receptor agonist, and that modulation of both μ and the δ opioid receptors may be beneficial based on the pharmacological and functional interactions between them.4-5 We herein set out to design and discover novel, nonselective bivalent opioid ligands with a potential therapeutic advantage by reducing adverse side effects in the treatment of pain.
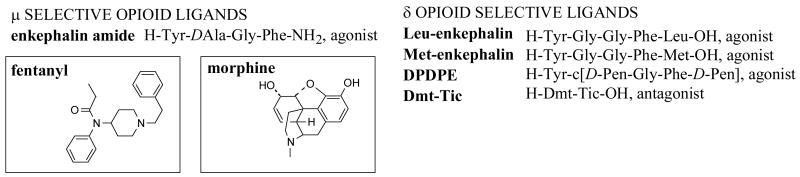
Enkephalins are highly flexible pentapeptides which can exist in numerous conformations (Figure 1).6 The SAR study of enkephalins has shown that i) an additional aromatic group strongly enhanced receptor affinity; and ii) the COOH group at the C-terminus played an important role in δ opioid receptor selectivity.7-10
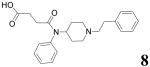
Figure 1.
Chemical structure of opioid analogues
Natural opioid peptides show in general poor bioavailability, mainly due to their inability to penetrate the blood-brain barrier, and rapid degradation in vivo by several peptidases. To overcome these problems, diverse strategies such as insertion of unnatural amino acids, introduction of conformational constraints, and cyclization of linear peptides have been adopted.11-13 In several cases, peptide analogues or peptidomimetics have been found to possess much higher biological activity than that expected on the basis of simple binding affinity studies.
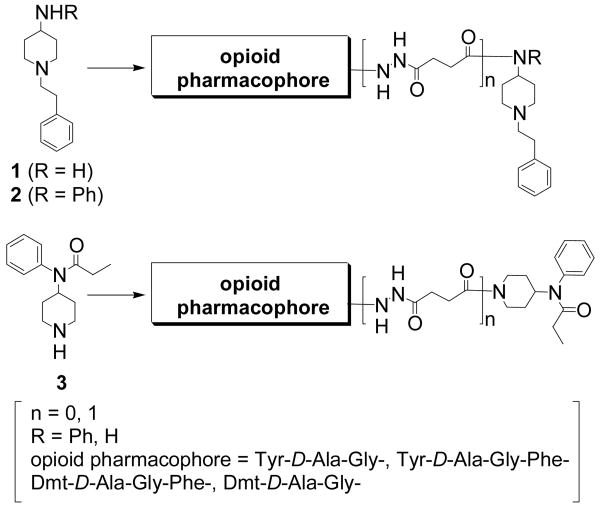
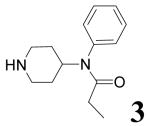
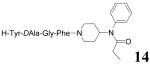
On the basis of these facts, we sought additional opportunities to increase the potency at both opioid receptors and change the overall physicochemical properties by modifying the C-terminus of enkephalin. Previously our group developed several fentanyl derived moieties which can be ligated with various kinds of amino acids (or peptide pharmacophores) to create a new class of opioid analogues.14, 15 We found that the propionyl moiety along with the phenethyl part of fentanyl plays an important role in opioid receptor binding and activation. Among them a ligand which carries a Tyr-D-Ala-Gly-Phe opioid message sequence showed good opioid affinity and bioactivity suggesting that a novel class of analgesics can be further developed by this approach. Pursuing enhanced bioactivity at both opioid receptors, a series of enkephalin analogues were designed and synthesized in which three different structural moieties of fentanyl (1-3) were attached to the C-terminus with or without a linker and tyrosine moiety was replaced by Dmt (Figure 2, Scheme 1). These analogues were designed to have a mixed μ and δ agonist profile with a potential for increased cell permeability due to the lipophilic character of the 4-anilido piperidine moiety (Table 1).16-17
Figure 2.
Design of opioid ligands.
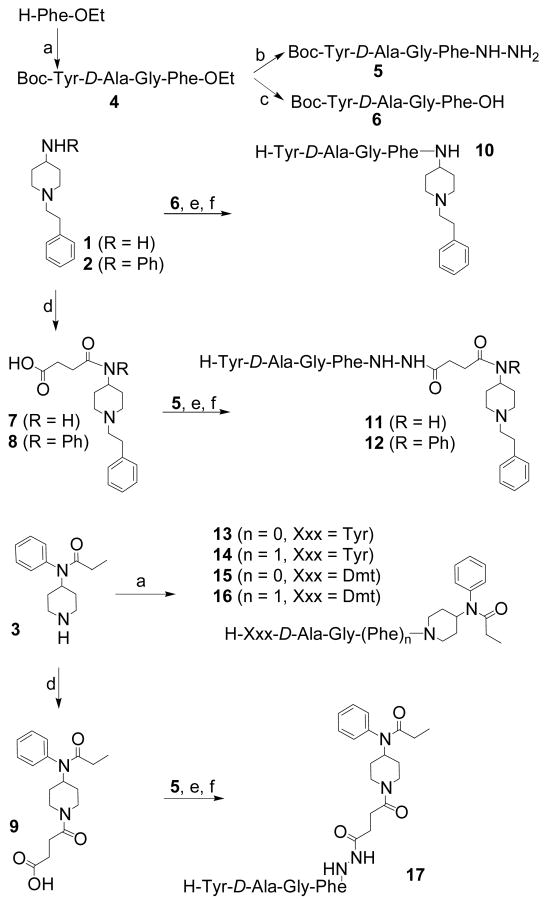
Scheme 1a.
a (a) stepwise coupling (BOP/HOBt/NMM, DMF, rt, 2-4 h) and deprotection (TFA, 0 °C, 20 min); (b) 1N KOH, EtOH; (c) NH2-NH2, DMF, 1 day; (d) succinic anhydride, EtOAc, 1 day; (e) BOP/HOBt/NMM, DMF, 4 h; (f) TFA, 0 °C, 20 min
Table 1.
| structure | aLogP | structure | aLogP |
|---|---|---|---|
|
1.54 |
|
2.93 |
|
3.19 |
|
4.04 |
|
2.00 |
|
2.80 |
| Tyr-DAla-Gly-Phe-OH | -0.54 |
|
2.96 |
| Tyr-DAla-Gly-Phe-NH2 | 0.32 | ||
| Tyr-DAla-Gly-Phe-NH-NH2 | 0.81 |
Results and Discussion
There is evidence that nonselective μ/δ ligands with different combinations of agonist and (or) antagonist activities at each of the opioid receptors can act as potent analgesics.18, 19 These bifunctional ligands bind to more than one opioid receptor while producing the desired physiological effects with enhanced efficacy and without many of the undesirable side effects of selective μ opioid receptor ligands.19 Rational design of opioid ligands that have mixed agonist activities for both μ and δ opioid receptors was accomplished in these studies by the combination of enkephalin-like structures (e.g., H-Tyr-D-Ala-Gly-Phe-) and parts of the fentanyl moiety {(1-phenethyl-piperidin-4-yl)-phenyl-amine or 1-phenethyl-piperidin-4-ylamine}. Taking into account our experience in the development of μ opioid selective 4-anilidopiperidine analogues, we also introduced the N-phenyl-N-piperidin-4-yl-propionamide to the enkephalin-like structures. In this regard, we modified the enkephalin-like structure along with the insertion of a linker (Figure 2).
The designed ligands were prepared by stepwise (for 10-12, 17) or fragment (for 13-16) solution-phase peptide syntheses using Nα-Boc chemistry, and the products were purified by preparative RP-HPLC to afford > 98% pure compounds in 40-50% overall yields (Scheme 1). During the chain elongation, the peptide intermediates were isolated by precipitation from appropriate organic solvents, usually diethyl ether, with high purity.
Opioid binding affinities of these ligands for the human δ opioid receptor (hDOR) or the rat μ opioid receptor (rMOR) were determined by radioligand competition analysis using [3H]DPDPE for the δ opioid receptor and [3H]DAMGO for the μ opioid receptor in cell membrane preparations from transfected cells that stably express the respective receptor type. Opioid agonist efficacy was examined by monitoring [35S]GTP-γ-S binding. For functional characterization of the ligands at the δ and μ opioid receptors, classical assays were performed to evaluate their opioid agonist activities in the GPI and MVD. These results generally were comparable with the results from the [35S]GTP-γ-S binding assay.
The new opioid ligands showed a very broad range of bioactivities at the δ and μ opioid receptors depending on their respective structures (Table 2).20-21 Comparing with the tetrapeptide amide, most ligands increased their binding affinities at the δ opioid receptor with the ligation of the fentanyl moieties. The most distinct observation was that the parts of the fentanyl moiety attached to the C-terminus of the enkephalin like structure played an important role in determining selectivity for the opioid receptors. Derivatization of peptides at the N- or C-terminus has frequently been carried out in attempts to improve the activity, bioavailability, and physicochemical properties of potential drug candidates. In our case, these modifications seemed to have the greatest effect on opioid selectivity as measured by in vitro binding and functional assays. Ligand 10, in which 1-phenethyl-piperidin-4-ylamine is attached to the C-terminus of the enkephalin showed μ opioid receptor selectivity in the functional (δ/μ = 2.4) and GTP-γ-S binding (δ/μ = 4.2) assays, whereas ligand 14 with a N-phenyl-N-piperidin-4-yl propionamide moiety gave highly δ opioid receptor selective binding affinity (Ki = 0.69 nM, δ/μ = 0.03) and agonist activity (IC50 = 24 nM, δ/μ = 0.12) in the MVD. This trend of selectivity for the δ and μ opioid receptors was observed in the whole series of ligands except for 17 which has a linker inserted between the two moieties. In the case of ligand 17, its μ opioid receptor selectivity over the δ receptor in GTP-γ-S binding (δ/μ = 6.3) and functional assays (δ/μ = 2.0) is more likely to be caused by the linker, 3-hydrazinocarbonyl-propionyl, rather than by the N-phenyl-N-piperidin-4-yl propionamide moiety. Compared to 10, ligands 11 and 12 showed an increased selectivity for the μ opioid receptor as evidenced by their enhanced biological activities (Ki = 1.2 nM, EC50 = 16 nM at rMOR; IC50 = 47 nM at GPI for 11, Ki = 1.1 nM, EC50 = 11 nM at rMOR; IC50 = 95 nM at GPI for 12). There were subtle differences in the biological activities of 11 and 12. The additional aromatic group on the piperidin-4-ylamine moiety in ligand 12 did not enhance biological activities at either receptor. Ligand 11 which has a less hindered and more flexible structure at the C-terminus of the enkephalin, can bind better to the opioid receptors. This is especially noted in the μ opioid receptor.
Table 2.
Bioactivities of the Opioid Ligands
| no | hDORa [3H]DPDPE b | rMORa [3H]DAMGOc | [35S]GTP-γ-S binding | IC50 (nM)e | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| hDORd | rMORd | |||||||||||
| LogIC50f,g | Kih (nM) | LogIC50f,g | Kih (nM) | LogEC50f | EC50 (nM)i | Emaxj (%) | LogEC50f | EC50 (nM)i | Emaxj (%) | MVD(δ) | GPI(μ) | |
| 8 | -4.70±0.17 | 9400 | -4.93±0.20 | 5400 | ns | ns | ns | ns | ns | ns | 1% | 0% |
| 10 | -7.51±0.12 | 14 | -7.52±0.26 | 14 | -6.29±0.15 | 510 | 92 | -6.90±0.31 | 125 | 53 | 380±80 | 160±50 |
| 11 | -8.12±0.11 | 3.7 | -8.60±0.08 | 1.2 | -7.54±0.09 | 29 | 78 | -7.79±0.09 | 16 | 52 | 250±50 | 47±12 |
| 12 | -7.88±0.12 | 6.1 | -8.63±0.16 | 1.1 | -6.95±0.10 | 110 | 32 | -7.96±0.14 | 11 | 52 | 290±70 | 95±6 |
| 13 | -4.87±0.23 | 7000 | -4.96±0.31 | 5700 | Ns | ns | ns | Ns | ns | ns | 3% | 3% |
| 14 | -8.75±0.08 | 0.69 | -7.24±0.24 | 23 | -7.43±0.39 | 37 | 72 | -7.39±0.41 | 41 | 63 | 24±2 | 200±60 |
| 15 | -6.40±0.19 | 180 | -7.05±0.07 | 40 | -6.78±0.20 | 170 | 15 | -7.08±0.29 | 82 | 32 | 10% | 15% |
| 16 | -9.10±0.10 | 0.36 | -9.08±0.22 | 0.38 | -9.12±0.17 | 0.77 | 24 | -9.05±0.18 | 0.88 | 50 | 1.8±0.2 | 8.5±3.3 |
| 17 | -8.18±0.08 | 3.2 | -7.92±0.06 | 5.7 | -6.82±0.20 | 150 | 71 | -7.63±0.25 | 24 | 43 | 250±70 | 120±50 |
| DAMGO | - | - | - | - | - | - | - | -7.44±0.19 | 37 | 150 | - | - |
| DPDPE | - | - | - | - | 8.80±0.25 | 1.6 | 69 | |||||
| YDAGF-NH2 | -6.14±0.16 | 300 | -8.24±0.13 | 2.8 | -6.72±0.17 | 190 | 44 | -7.98±0.22 | 13 | 99 | 120±10 | 47±10 |
| DALEA20-21 | - | 2.4 | - | 7.7 | - | - | - | - | - | - | 7.6 | 8.3 |
Competition analyses were carried out using membrane preparations from transfected HN9.10 cells that constitutively expressed the respective receptor types.
Kd = 0.50 ± 0.1 nM.
Kd = 0.85 ± 0.2 nM.
Expressed from CHO cell.
Concentration at 50% inhibition of muscle contraction at electrically stimulated isolated tissues.
Logarithmic values determined from the non-linear regression analysis of data collected from at least two independent experiments.
Competition against radiolabeled ligand.
Antilogarithmic value of the respective IC50.
Antilogarithmic value of the respective EC50.
Net total bound/basal binding × 100 ± SEM.
ns: not saturated
Ligand 14 in which N-phenyl-N-piperidin-4-yl propionamide was attached to the C-terminus of enkephalin showed highly selective biological activities for the δ opioid receptor in binding (Ki = 0.69 nM) and functional (IC50 = 24 nM at MVD) assays. It is worthwhile to note that the moiety at the C-terminal reversed the μ selectivity (δ/μ = 107 and 2.5 in the binding and functional assays, respectively) of tetrapeptide amide (H-Tyr-DAla-Gly-Phe-NH2) to the δ selectivity (δ/μ = 0.03 and 0.12 in the binding and functional assays, respectively) in ligand 14 and the insertion of the flexible linker inverted again its selectivity in the GTP-γ-S binding and the functional assays from favoring the δ opioid to the μ opioid receptor as evidenced by the 4.1- to 10-fold decreased δ opioid and 1.6- to 4.0-fold increased μ opioid biological activities in ligand 17. As described earlier, the insertion of the flexible linker to ligand 10 amplified its μ opioid receptor selectivity in 11 and 12 by increasing biological activities at the μ receptor much more than at the δ opioid receptor. This observation suggests that there is a distinct topographical difference between the δ and μ opioid receptors, despite the high biological activities observed. The more flexible structure seems to better fit the μ opioid receptor binding pocket. Thus, our modifications at the C-terminus seem to primarily determine the selectivity between the δ and μ opioid receptors.
In general, for the opioid receptors, the key pharmacophore elements in a peptide structure are the phenylalanine and tyrosine residues, and the free amine group of the N-terminus tyrosine. In ligands 13 and 15, phenylalanine was truncated to investigate the possible role of the phenyl group on the N-phenyl-N-piperidin-4-yl propionamide moiety as a replacement. In this case, both ligands lost their agonist activities in the MVD and GPI assays. Moderate binding affinities of ligand 15 (Ki = 180 nM and 40 nM at hDOR and rMOR, respectively) at both receptors are more likely to be caused by the 2,6-dimethyltyrosine (Dmt) substitution to facilitate opioid receptor recognition.18, 22 These results demonstrated that phenylalanine is an important key residue and the piperidine linked aromatic group of fentanyl moiety cannot be used as its substitute. This may be due to the lack of topographical similarity that cannot be maintained by the longer distance and different orientation of the alternate aromatic group. Ligand 14 was a lead compound showing good binding affinities at both δ and μ receptors, good biological efficacies, and agonist functions even though its substantial selectivity for the δ receptor. Since it has been known that substitution of Dmt for tyrosine in opioid peptides results in a more pronounced increase in μ receptor affinity than in δ receptor affinity,22-24 further modification on the ligand was performed to balance its bioactivities at both receptors by replacing the tyrosine with Dmt. The replacement dramatically increased biological activities for both δ and μ opioid receptors, especially much more for the μ receptor. In binding assay, 16 showed a 2 fold increase in affinity at the δ receptor (Ki = 0.36 nM) and a 60 fold increased in affinity at the μ receptor (Ki = 0.38 nM) as compared to 14, thus resulting in balanced binding affinities at both receptors. In addition, 16 was on the order of 13 fold more potent than 14 in the MVD (IC50 = 1.83 nM) and 24 fold in the GPI (IC50 = 8.51 nM) assays. These results demonstrate that the Dmt substitution for tyrosine in opioid peptides results in a higher increase in μ receptor affinity than in δ receptor affinity. In summary, The well-known effect of Dmt substitution for the tyrosine residue increased the biological activities dramatically yielding the most potent opioid ligand 16 for both δ and μ opioid receptors. Binding affinities and EC50 values (0.77 nM and 0.88 nM at hDOR and rMOR, respectively) were in the subnanomolar range. The best IC50 values also were obtained for this analogue.
Conclusion
Novel enkephalin analogues in which different parts of the fentanyl moiety were attached at the C-terminus of the tetrapeptide structure (Tyr-D-Ala-Gly-Phe-) have been designed and synthesized. The mixed μ and δ opioid agonist activities of these ligands were sought in order to enhance their analgesic effects while reducing the undesired side effects and increasing bioavailability. These analogues showed a broad range of biological activities depending on their respective structures. While all the analogues containing the tetrapeptide structure retained their potencies for both μ and δ opioid receptors, their selectivities for the receptors were highly dependent on the topographical structure of the C-terminus. It is likely that the more flexible and longer length of ligands 11 and 12 possess a better fit for the μ opioid receptor binding pocket than that for the δ opioid receptor. Furthermore, a reverse trend has been noticed for the more constrained structures of ligands 14 and 16. The best result in all three assays (binding, GTP-γ-S, functional) occurred when Tyr was replaced with Dmt, and N-phenyl-N-piperidin-4-yl propionamide was attached to the C-terminus of the tetrapeptide structure as in ligand 16. This ligand may have a greater potential to penetrate the blood-brain barrier due to the lipophilic character of the N-phenyl-N-piperidin-4-yl-propionamide moiety.
Experimental Section
Boc-Tyr-D-Ala-Gly-Phe-OEt (4)
TFA.H-D-Ala-Gly-Phe-OEt was prepared as previously described.18 The tripeptide ester (1.13 g, 2.6 mmol) and Nα-Boc-Tyr (0.79 g, 2.8 mmol) were dissolved in DMF (10 mL) and cooled in an ice-bath for 10 min. BOP (0.79 g, 2.8 mmol), HOBt (0.38 g, 2.8 mmol), and NMM (0.56 mL, 5.2 mmol) were added to the reaction mixture and stirred for 3 h at rt. After checking for disappearance of the starting amine by TLC, the mixture was concentrated under reduced pressure, followed by dilution with EtOAc (50 mL). The organic layer was washed with 5% NaHCO3 (3 × 50 mL), 5% citric acid (2 × 50 mL), brine (1 × 50 mL), and water consecutively and dried over anhydrous Na2SO4. After filtering, the solution was concentrated under reduced pressure to give a solid. The residue was washed with diethylether (2 × 50 mL) and dried in vacuo to afford 1.46 g (96% yield) of 4 as a white powder. MS m/z 607.2 [M+Na]+
Boc-Tyr-D-Ala-Gly-Phe-NH-NH2 (5)
Compound 4 (467 mg, 0.8 mmol) in 8 mL of EtOH was treated with 55% hydrazine (0.8 mL) for 1 day and solidified with water to give pure 5 as a white power in 89% yield: analytical RP-HPLC tR 16.9 min, purity >98%; MS m/z 571.0 [M+H]+
Boc-Tyr-D-Ala-Gly-Phe-OH (6)
Compound 4 (584 mg, 1 mmol) in 8 mL of MeOH was treated with 2 mL of 1 M KOH for 2 h at rt. and neutralized with 2 mL of 1N HCl. The mixture was concentrated under reduced pressure and extracted with EtOAc. After concentration, a white solid was formed to give pure 6 (422 mg) in 76% yield: analytical RP-HPLC tR 14.3 min, purity >99%; MS m/z 556.9 [M+H]+
N-(1-Phenethyl-piperidin-4-yl)-succinamic acid (7), N-(1-phenethyl-piperidin-4-yl)-N-phenyl-succinamic acid (8), 4-oxo-4-[4-(phenyl-propionyl-amino)-piperidin-1-yl]-butyric acid (9)
Compound 1 (or 2, 3)9 (408 mg, 2 mmol) was dissolved in 10 mL of EtOAc and succinic anhydride (300 mg, 3 mmol) was added to the mixture. The reaction mixture was stirred for 3 h (3 days for 2, 1 h for 3) at rt and formed solid was filtered and washed with EtOAc to give 7 (or 8, 12) in quantitative yield. 7 MS m/z 305.3 [M+H]+ 8 MS m/z 381.2 [M+H]+ 12 MS m/z 333.1 [M+H]+
Ligands 10-12 and 17
Nα-Boc-protected intermediates were prepared by the same coupling method described above and deprotected by TFA at 0 °C for 20 min. The mixtures were evaporated and co-evaporated with toluene. The concentrated solids were triturated with diethyl ether. The crude powders were purified by preparative RP-HPLC (10 – 40 % of acetonitrile within 20 min) to give pure 10-12, and 17 as white powders in 70%, 52%, 48%, and 55% yields, respectively. For analytical data, see Supporting Information.
Ligands 13-16
These ligands were prepared by stepwise synthesis using the same coupling and deprotection methods starting from 3. The crude peptide ligands were purified by preparative RP-HPLC (10 – 50 % of acetonitrile within 20 min) to give pure 13, 14, 15, and 16 as white powders in overall 35-42%. For analytical data, see Supporting Information.
Radioligand Labeled Binding Assay, [35S]GTP-γ-S binding Assay, GPI and MVD in Vitro Bioassay
The methods were carried out according to that previously described.25
Supplementary Material
1H NMR, MS, HRMS, TLC, HPLC, and purity data of the ligands 8-17. This material is available free of charge via the Internet at http://pubs/acs/org.
Acknowledgments
The work was supported by grants from the USDHS, National Institute on Drug Abuse(DA-12394 and DA-06284). We thank Margie Colie for assistance with the manuscript.
Abbreviations
- Boc
tert-butyloxycarbonyl
- BOP
(benzotriazole-1-yloxy)-tris(dimethylamino)-phosphonium hexafluorophosphate
- CHO
Chinese hamster ovary
- DALEA
[D-Ala2, Leu5]enkephalin amide
- DMF
N,N-dimethylformamide
- hDOR
human δ opioid receptor
- DPDPE
c[D-Pen2,D-Pen5]enkephalin
- DAMGO
[D-Ala2,NMePhe4,Gly5-ol]enkephalin
- Dmt
2,6-dimethyltyrosine
- GPI
guinea pig isolated ileum
- HOBt
1-hydroxybenzotriazole
- rMOR
rat μ opioid receptor
- MVD
mouse vas deferens
- NMM
N-methylmorpholine
- RP-HPLC
reverse phase high performance liquid chromatography
- SAR
structure-activity relationships
- TFA
trifluoroacetic acid
- TLC
thin layer chromatography
References
- 1.Wiesenfeld-Hallin Z, Xu SJ, Hokfelt T. The role of spinal cholecystokinin in chronic pain states. Pharmacol Toxicol. 2002;91:398–403. doi: 10.1034/j.1600-0773.2002.910619.x. [DOI] [PubMed] [Google Scholar]
- 2.Ossipov MH, Lai J, King T, Vanderah TW, Porreca F. Underlying mechanisms of pronociceptive consequences of prolonged morphine exposure. Biopolymers. 2005;80:319–324. doi: 10.1002/bip.20254. [DOI] [PubMed] [Google Scholar]
- 3.Ossipov MH, Lai J, King T, Vanderah TW, Malan TP, Hruby VJ, Porreca F. Antinociceptive and nociceptive actions of opioids. J Neurobiology. 2004;61:126–148. doi: 10.1002/neu.20091. [DOI] [PubMed] [Google Scholar]
- 4.Zhao GM, Wu D, Soong Y, Shimoyama M, Berezowska I, Schiller PW, Szeto HH. Profound spinal tolerance after repeated exposure to a highly selective μ-opioid peptide agonist: role of δ-opioid receptors. J Pharmacol Exp Ther. 2002;302:188–196. doi: 10.1124/jpet.302.1.188. [DOI] [PubMed] [Google Scholar]
- 5.Jiang Q, Mosberg HI, Porreca F. Modulation of the potency and efficacy of mu-mediated antinociception by delta agonists in the mouse. J Pharmacol Exp Ther. 1990;254:683–689. [PubMed] [Google Scholar]
- 6.Schiller PW. Role of the conformational element in peptide-receptor interactions. Studies with cyclic opioid peptide analogs. Biophys Chem. 1988;31:63–39. doi: 10.1016/0301-4622(88)80009-7. [DOI] [PubMed] [Google Scholar]
- 7.Hruby VJ, Gehrig CA. Recent developments in the design of receptor specific opioid peptides. Med Res Rev. 1989;9:343–401. doi: 10.1002/med.2610090306. [DOI] [PubMed] [Google Scholar]
- 8.DiMaio J, Nguyen TMD, Lemieux C, Schiller PW. Synthesis and pharmacological characterization in vitro of cyclic enkephalin analogs: effect of conformational constraints on opiate receptor selectivity. J Med Chem. 1982;25:1432–1438. doi: 10.1021/jm00354a008. [DOI] [PubMed] [Google Scholar]
- 9.Ronai AZ, Szekely JI, Berzetei I, Miglecz E, Bajusz S. Tetrapeptide-amide analogues of enkephalin: The role of C-terminus in determining the character of opioid activity. Biochem Biophys Res Commun. 1979;91:1239–1249. doi: 10.1016/0006-291x(79)91200-2. [DOI] [PubMed] [Google Scholar]
- 10.Kodama H, Uchida H, Yasunaga T, Kondo M, Costa T, Shimohigashi Y. Effect of modification of enkephalin C-terminal functions on affinity selection of opioid receptors. J Molecular Recognition. 1990;3:197–203. doi: 10.1002/jmr.300030505. [DOI] [PubMed] [Google Scholar]
- 11.Hruby VJ. Conformational restrictions of biologically active peptides via amino acid side chain groups. Life Sci. 1982;31:189–199. doi: 10.1016/0024-3205(82)90578-1. [DOI] [PubMed] [Google Scholar]
- 12.Hruby VJ, Agnes RS. Conformation-activity relationships of opioid peptides with selective activities at opioid receptors. Biopolymers. 1999;51:391–410. doi: 10.1002/(SICI)1097-0282(1999)51:6<391::AID-BIP3>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 13.Hruby VJ, Balse PM. Conformational and topographical considerations in designing agonist peptidomimetics from peptide leads. Curr Med Chem. 2000;7:945–970. doi: 10.2174/0929867003374499. [DOI] [PubMed] [Google Scholar]
- 14.Lee YS, Nyberg J, Moye S, Agnes R, Davis P, Ma S, Lai J, Porreca F, Vardanyan R, Hruby VJ. Understanding the structural requirements of 4-anilidopiperidine analogues for biological activities at μ and δ opioid receptors. Bioorg Med Chem Lett. 2007;17:2161–2165. doi: 10.1016/j.bmcl.2007.01.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Petrov RR, Vardanyan RS, Lee YS, Ma SW, Davis P, Begay LJ, Lai J, Porreca F, Hruby VJ. Synthesis and evaluation of 3-aminopropionyl substituted fentanyl analogs for opioid activity. Bioorg Med Chem Lett. 2006;16:4946–4950. doi: 10.1016/j.bmcl.2006.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tetko IV, Tanchuk VY, Villa EP. Prediction of n-Octanol/Water Partition Coefficients from PHYSPROP Database Using Artificial Neural Networks and E-State Indices. J Chem Inf Comput Sci. 2001;41:1407–1421. doi: 10.1021/ci010368v. [DOI] [PubMed] [Google Scholar]
- 17.Tetko IV, Gasteiger J, Todeschini R, Mauri A, Livingstone D, Ertl P, Palyulin VA, Radchenko EV, Zefirov NS, Makarenko AS, Tanchuk VY, Prokopenko VV. Virtual computational chemistry laboratory - design and description. J Comput Aid Mol Des. 2005;19:453–63. doi: 10.1007/s10822-005-8694-y. [DOI] [PubMed] [Google Scholar]
- 18.Schiller PW, Fundytus ME, Merovitz L, Weltrowska G, Nguyen TMD, Lemieux C, Chung NN, Coderre TJ. The opioid μ agonist/δ antagonist DIPP-NH2 [ψ] produces a potent analgesic effect, no physical dependence, and less tolerance than morphine in rats. J Med Chem. 1999;42:3520–3526. doi: 10.1021/jm980724+. [DOI] [PubMed] [Google Scholar]
- 19.Horan PJ, Mattia A, Bilsky EJ, Weber S, Davis TP, Yamamura HI, Malatynska E, Appleyard SM, Slaninova J, Misicka A, Lipkowski AW, Hruby VJ, Porreca F. Antinociceptive profile of biphalin, a dimeric enkephalin analog. J Pharmacol Exp Ther. 1993;265:1446–1454. [PubMed] [Google Scholar]
- 20.Rigaudy P, Garbav-laureguiberry C, Jacquemin-Sablon S, Le Pecq JB, Roques BP. Synthesis and binding properties to DNA and to opioid receptors of enkephalin-ellipticinium conjugates. Int J Pept Prot Res. 1987;30:347–355. doi: 10.1111/j.1399-3011.1987.tb03341.x. [DOI] [PubMed] [Google Scholar]
- 21.DiMaio J, Nguyen TMD, Lemieux C, Schiller PW. Synthesis and pharmacological characterization in vitro of cyclic enkephalin analogs: effect of conformational constraints on opiate receptor selectivity. J Med Chem. 1982;25:1432–1438. doi: 10.1021/jm00354a008. [DOI] [PubMed] [Google Scholar]
- 22.Bryant SD, Jinsmaa Y, Salvadori S, Okada Y, Lazarus LH. Dmt and opioid peptides: a potent alliance. Biopolymers. 2003;71:86–102. doi: 10.1002/bip.10399. [DOI] [PubMed] [Google Scholar]
- 23.Schiller PW, Nguyen TMD, Berezowska I, Dupuis S, Weltrowska G, Chung NN, Lemieux C. Synthesis and in vitro opioid activity profiles of DALDA analogs. Eur J Med Chem. 2000;35:895–901. doi: 10.1016/s0223-5234(00)01171-5. [DOI] [PubMed] [Google Scholar]
- 24.Hasnsen DW, Stapelfeld A, Savage MA, Reichman M, Hammond DL, Haaseth RC, Mosberg HI. Systemic analgesic activity and δ–opioid selectivity in [2,6-dimethyl-Tyr1, D-Pen2, D-Pen5]enkephalin. J Med Chem. 1992;35:684–687. doi: 10.1021/jm00082a008. [DOI] [PubMed] [Google Scholar]
- 25.Lee YS, Agnes RS, Badghisi H, Davis P, Ma SW, Lai J, Porreca F, Hruby VJ. Design and synthesis of novel hydrazide linked bifunctional peptides as δ/μ opioid receptor agonists and CCK-1/CCK-2 receptor antagonists. J Med Chem. 2006;49:1773–1780. doi: 10.1021/jm05085. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1H NMR, MS, HRMS, TLC, HPLC, and purity data of the ligands 8-17. This material is available free of charge via the Internet at http://pubs/acs/org.