Abstract
Background
Pyronaridine, a Mannich base anti-malarial with high efficacy against drug resistant Plasmodium falciparum, is currently evaluated as a fixed dose combination with artesunate for the treatment of uncomplicated malaria. In this study, the in vitro activity of pyronaridine against clinical isolates of P. falciparum from Lambaréné, Gabon, was assessed in order to obtain baseline data on its activity prior to its future use in routine therapy. Moreover, follow-up assessment on the in vitro activity of chloroquine, artesunate and quinine was performed.
Methods
In vitro response of field isolates of P. falciparum to pyronaridine, chloroquine, artesunate and quinine was assessed using the traditional WHO microtest. In addition, the histidine-rich protein 2 (HRP-2) assay was performed and evaluated for its future implementation for follow-up of drug susceptibility testing.
Results
Pyronaridine exhibited a high in vitro activity against P. falciparum, with a geometric mean cut-off concentration of 9.3 nmol/l. Fifty percent effective concentrations were 1.9 nmol/l and 2.0 nmol/l in the WHO microtest and HRP-2 assay, respectively. Results matched closely in vivo findings from a recent clinical trial on pyronaridine-artesunate treatment. One isolate showed diminished sensitivity to artesunate. For chloroquine and quinine resistance levels were comparable to prior studies from Lambaréné. Results from the novel HRP-2 assay corresponded well to those obtained by the WHO microtest.
Conclusion
Pyronaridine is highly active in chloroquine-resistant parasites and seems a promising partner drug for artemisinin-based combination therapy in Africa.
Background
Malaria continues to be a major cause of morbidity and mortality in sub-Saharan Africa, particularly in young children. Early detection and effective chemotherapy remain the cornerstones in its control [1]. The rapid development and spread of anti-malarial drug resistance has made surveillance of drug sensitivity a high priority issue. In addition to assessing the activity of common anti-malarials against Plasmodium falciparum in routine surveys, the evaluation of new compounds against field isolates is of major importance for drug development.
In Lambaréné, Gabon, routine anti-malarial drug susceptibility monitoring has been performed since 1992 [2-5]. So far the WHO microtest – one of the longest used and best validated assays for the assessment of in vitro drug sensitivity under field conditions – has been used for this purpose [6]. Meanwhile, novel methods in drug susceptibility testing have been developed, such as the histidine-rich protein II (HRP-2) assay [7]. This method, based on HRP-2 measurement in an enzyme-linked immunosorbent assay (ELISA), is equally simple to implement, but considerably less labour intensive compared with the WHO microtest. Due to these advantages, the WHO microtest will be replaced for standard drug susceptibility monitoring in Lambaréné in the future by the novel HRP-2 assay. Previous findings from laboratory adapted clones and from different geographical regions suggest that results obtained by the HRP-2 assay be comparable with those obtained by the WHO microtest [7].
The anti-malarial agent pyronaridine is a Mannich base derivative of mepacrine, one of the earliest synthetic anti-malarials [8]. It is currently evaluated as a fixed dose combination with artesunate for the treatment of uncomplicated falciparum and vivax malaria in adult and paediatric patients [9]. Its anti-plasmodial activity involves interference with the glutathione-dependent detoxification of haem and targeting of β-haematin formation [10]. Reports from paediatric patients in Africa showed that pyronaridine is effective against chloroquine resistant strains of P. falciparum in vivo [9,11], yet data from South-East Asia indicate the potential for rapid development of resistance against pyronaridine, when used as monotherapy [12].
The present study aimed to assess the susceptibility of clinical P. falciparum field isolates from Lambaréné to pyronaridine in order to obtain baseline data on the activity of this for Africa yet novel anti-malarial drug prior to its widespread use in routine therapy. In addition the study was designed to assess the potential for the novel HRP-2 assay to replace the standard WHO microtest.
Methods
Study area and patients
The study was carried out at the Medical Research Unit of the Albert Schweitzer Hospital in Lambaréné, Gabon, in a region of stable, hyperendemic P. falciparum malaria transmission [13,14]. Patients attending the outpatient clinic between March and October 2006 were asked to participate in the study if they met the following inclusion criteria: P. falciparum monoinfection with 1,000–100,000 asexual parasites per μl blood, no schizontaemia, no signs or symptoms of severe malaria, and no history of intake of anti-malarial drugs in the preceding month. Information about age, sex, and duration of fever was collected on a questionnaire. Informed consent was obtained from participants or their legal representatives. The study was approved by the Ethics Committee of the International Foundation for the Albert Schweitzer Hospital in Lambaréné.
In vitro drug sensitivity assays
Two different methods of drug sensitivity testing were deployed in order to assess the susceptibility of fresh field isolates of P. falciparum to pyronaridine, artesunate, chloroquine and quinine. First, the standard World Health Organization in vitro microtest was used similar to previous reports, measuring drug-dependent inhibition of schizont maturation (SMI) within 24 hours by microscopic assessment [2-5]. Briefly, two millilitres of venous blood were mixed with complete parasite culture medium (RPMI 1640, 200 μM hypoxanthine, 25 mM Hepes, 0.5% albumax, 2 mM l-glutamine) to a final concentration of 5% blood medium mixture (BMM). Ninety-six-well test plates were pre-dosed in ascending quantities of drugs, dosing each plate with all respective drugs for one isolate. Final drug concentrations were 0.5–365.9 nmol/l BMM for pyronaridine (Mr: 910.04), 0.1–85.8 nmol/l BMM for artesunate (Mr: 384.425), 0.8–51.2 μmol/l blood for chloroquine (Mr: 515.867) and 55–3567 nmol/l BMM for quinine (Mr: 785.06). Artesunate, chloroquine and quinine were dissolved in 70% ethanol, pyronaridine was resuspended in distilled water. In accordance to the protocols distributed by the World Health Organization drug concentrations for chloroquine are expressed as related to blood due to their considerable accumulation in erythrocytes [6].
Fifty μl BMM were transferred into scheduled wells and incubated at 37.5°C in candle jars. After 24 hours parasites were harvested and Giemsa-stained thick blood films were prepared. The number of mature schizonts was microscopically counted against 200 asexual parasites in each well. Tests were considered successful if at least 10% schizont maturation was observed in the drug-free control-well.
In addition, the HRP-2 assay was performed according to the published standard operational procedures [7]. Two ml of venous blood were mixed with parasite medium to a concentration of 3% BMM. Test plates were pre-dosed to the same final concentrations as in the WHO test and incubated for 72 hours at 37°C in candle jars. To test for successful in vitro parasite-growth, a thick blood smear of one control-well was performed after 26 h. One non-treated 26 h sample was frozen to calculate background HRP-2 production. Parasite culture was judged successful if at least 10% parasites matured to schizonts at the 26-hour time point. After 72 h plates were freeze-thawed twice. Parasite growth, calculated from HRP-2 levels, was measured with an enzyme linked immunosorbent assay at an absorbent maximum of 450 nm.
Statistical analysis
Non-linear regression analysis with 4-parameter fits of log-concentration/response curves was used to determine individual inhibitory concentrations of the respective isolates. All regressions were checked manually. Cut off concentrations were calculated as geometric mean of the lowest individual concentrations with no mature schizont among 200 parasites in the WHO microtest. Nonparametric analysis was used for concentration data that was not normally distributed. A two-tailed Mann-Whitney-U-Test was performed in order to test for difference between the two drug sensitivity assays. All tests were performed at a two sided significance level of α = 0.05.
Results
Ninety-five outpatients attending the Albert Schweitzer Hospital were included in this study. The patients' median age was three years, ranging from three month to 18 years, and 55% were female. Median asexual parasitaemia at presentation was 36,500 per μl blood. In the schizont maturation microtest 32, 36, 34, and 32 out of 95 isolates yielded valid results for pyronaridine, chloroquine, artesunate and quinine, respectively. Twenty-five isolates fulfilled the criteria for successful parasite-culture in the HRP-2 assay and 15, 16, 12 and 14 were successfully employed for drug sensitivity testing, respectively. Post-hoc analysis of the unexpected low success rate of cultivation, especially in the HRP-2 assay, revealed that poor growth was associated with one lot of the commercially acquired medium. Those isolates were identified and excluded from the analysis. Table 1 shows 50 percent, 99 percent and cut-off concentrations of the tested drugs as obtained by the WHO microtest and HRP-2 assay.
Table 1.
EC50, EC99 and cut-off concentrations of pyronaridine, chloroquine, artesunate and quinine in WHO microtest and HRP-2 assay
| WHO Microtest | HRP-2 assay | |||||
| N | EC50 (95%CI) | Cut-off concentration (95%CI) | N | EC50 (95% CI) | EC99 (95%CI) | |
| Pyronaridine | 32 | 1.87 (1.40–2.48) |
9.32 (5.2–13.9) |
15 | 2.03 (1.57–2.63) |
9.03 (6.42–12.69) |
| Chloroquine | 36 | 7.1 (5.2–9.6) |
21.7 (15.4–30.6) |
16 | 5.5 (4.4–6.9) |
19.2 (15.3–24.2) |
| Artesunate | 34 | 2.08 (1.48–2.92) |
9.24 (6.53–13.06) |
12 | 2.25 (1.70–2.99) |
15.24 (10.45–22.24) |
| Quinine | 32 | 272 (210–353) |
873 (723–1053) |
14 | 204 (167–250) |
662 (561–781) |
All values are in nmol/l BMM except for chloroquine (μmol/l blood),
Means and 95% confidence intervals are depicted as antilog of arithmetic mean of log-transformed data
Pyronaridine
Pyronaridine inhibited in vitro growth and schizont maturation in the WHO assay at a geometric mean cut-off concentration of 9.3 nmol/l BMM. The respective geometric mean EC99 concentration in the HRP-2 assay was 9.0 nmol/l. In one isolate schizont maturation was observed at a pyronaridine concentration of 122 nmol/l BMM, resulting in a cut-off concentration of 366 nmol/l BMM. Further two isolates showed cut-off concentrations of 122 nmol/l. Geometric mean EC50 values were 1.9 and 2.0 nmol/l BMM for the WHO microtest and the HRP-2 assay, respectively.
Chloroquine
The geometric mean cut-off concentration for chloroquine was 21.7 μmol/l blood in the WHO assay, 19.2 μmol/l blood was the respective EC99 value in the HRP-2 assay. The most sensitive isolate showed a cut-off concentration of 3.2 μmol/l blood, all other isolated exhibited cut-off concentrations of 6.4 μmol/l blood or higher. In four parasite cultures, microscopic assessment revealed schizont maturation up to the highest concentration of 51.3 μmol/l blood. The 50 percent effective concentrations were 7.1 μmol/l blood in the WHO microtest and 5.5 μmol/l in the HRP-2 assay, respectively.
Artesunate
Fifty percent effective concentrations were 2.1 nmol/l BMM in the microtest and 2.3 nmol/l BMM in the HRP-2 assay for artesunate. Two isolates exhibited schizont maturation at 28.6 nmol/l BMM, yielding cut-off concentrations of 85 nmol/l BMM. In one isolate in vitro schizont maturation was not inhibited by the highest artesunate concentration of 85 nmol/l BMM. The same isolate exhibited good sensitivity to pyronaridine and to quinine. The geometric mean cut-off concentration was 9.2 nmol/l BMM. The HRP-2 assay showed a mean EC99 level of 15.2 nmol/l BMM.
Quinine
All isolates were susceptible to quinine. Highest cut-off concentrations were at 1783 nmol/l BMM, thus well below the threshold of resistance (5120 nmol/l BMM). The geometric mean cut-off concentration was 873 nmol/l, the EC99 in the HRP-2 assay was 662 nmol/l BMM. The EC50 values in the WHO microtest and in the HRP-2 assay were 272 and 204 nmol/l BMM, respectively.
Activity correlation of the tested drugs
Correlation analysis of EC50 values of the individual isolates was performed in order to assess the relationship between sensitivity of parasites to pyronaridine, chloroquine, artesunate and quinine (Table 2). Significant correlation was found between in vitro activities of the anti-malarials quinine and chloroquine (r = 0.50, p < 0.005). Interestingly, the activity of pyronaridine was correlated with artesunate (r = 0.84 p < 0.0001), but not with chloroquine or quinine.
Table 2.
Activity correlation between pyronaridine, chloroquine, artesunate and quinine in fresh Plasmodium falciparum isolates
| Pyronaridine | Chloroquine | Artesunate | ||
| Chloroquine | R2 | 0.13 | - | - |
| P | 0.52 | |||
| N | 30 | |||
| Artesunate | R2 | 0.84 | -0.07 | - |
| P | <.0001* | 0.69 | ||
| N | 29 | 30 | ||
| Quinine | R2 | 0.06 | 0.50 | 0.02 |
| P | 0.74 | 0.0037* | 0.93 | |
| N | 30 | 31 | 30 |
R2: correlation coefficient in pairwise correlation analysis
* statistically significant
Comparison of HRP-2 assay and WHO microtest
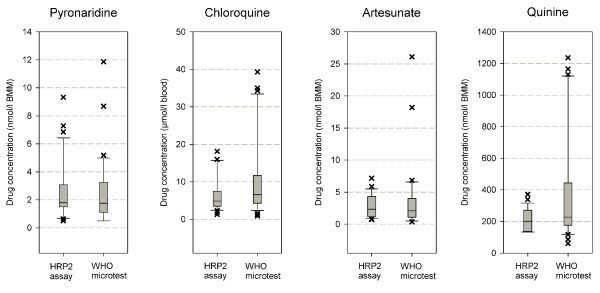
No statistically significant differences between the EC50 values from the two drug sensitivity assays were found in U-test of pooled data of the individual drugs (p = 0.82 for pyronaridine, 0.72 for artesunate, 0.11 for chloroquine and 0.20 for quinine). Differences in geometric means of EC50 values were largest for chloroquine (7.1 μmol/l, 95% CI 5.2–9.6 in the WHO microtest versus 5.5 μmol/l 95% CI: 4.4–6.9 in the HRP-2 assay, p = 0.11) and quinine (272 nmol/l 95% CI: 210–353 versus 204 nmol/l 95%CI 167–250, respectively. p = 0.20). Figure 1 shows the distribution of EC50 values for the respective drugs.
Figure 1.
Box plots of pyronaridine, chloroquine, artesunate and quinine EC50 in HRP-2 assay and WHO microtest.
Cut-off concentrations as determined by the WHO microtest correlate closely to the equivalent EC99 values of the HRP-2 assay (Table 1). Significantly more isolates yielded valid results in the microtest (36%) than in the HRP-2 based assay (15%) (p < 0.001).
Discussion
Pyronaridine exhibited a high level of in vitro activity against isolates of P. falciparum from infected Gabonese subjects in this study. Fifty percent effective concentrations were 2.0 and 1.9 nmol/l, which is consistent with previously published data from studies with laboratory strains and field isolates obtained by a different drug sensitivity assay (isotopic hypoxanthine assay) [15,16].
Median pyronaridine concentrations of 9.3 nmol/l (EC99 in HRP-2 assay) and 9.0 nmol/l (cut-off concentration in WHO microtest) inhibited growth of P. falciparum in vitro. In a recent pharmacokinetic assessment of a fixed-dose pyronaridine artesunate combination in African children, the mean maximal plasma concentrations of pyronaridine were 115 nmol/l in patients [9]. Earliest reappearances of parasites in peripheral blood in this study were observed on day 21 (one patient) and day 28 (three patients) after treatment. Interestingly, the patient with parasite reappearance on day 21 exhibited a pyronaridine plasma level of 9.9 nmol/l at that time. In polynomial regression analysis of pooled plasma levels of all patients, mean pyronaridine blood concentrations fell below levels of 9 nmol/l on day 22. First reappearances in vivo therefore occurred only after plasma levels fell below concentrations similar to cut-off concentrations obtained in this in vitro study.
Although the extrapolation of in vitro drug sensitivity assessments to in vivo data should always be cautious [17], in vitro results of the present study matched closely clinical findings of this clinical trial on pyronaridine-artesunate combination therapy.
The relationship between in vitro activity of pyronaridine and chloroquine against P. falciparum has been discussed controversially in previous reports and contradictory conclusions concerning cross-resistance have been drawn from studies, which found a significant correlation between pyronaridine and chloroquine in vitro activity and differences in activity of pyronaridine against chloroquine resistant and sensitive strains [15,16,18,19]. In the present study, in vitro response to chloroquine was poor in all tested isolates, yet parasites proved to be highly susceptible to pyronaridine. There was no statistically significant correlation of the in vitro activities of the two drugs against P. falciparum. These in vitro findings and the recently reported high cure rates of three days pyronaridine-artesunate combination therapy provide convincing evidence against a clinically significant cross resistance of pyronaridine and chloroquine in vivo. The results underline the usefulness of pyronaridine for the treatment of patients in regions affected by P. falciparum resistant to chloroquine [9,11].
Since the first in vitro drug susceptibility assessment in Lambaréné in 1992 [2], high levels of resistance against chloroquine have been observed in vitro and in vivo [3-5]. Similar to previous studies in vitro response to chloroquine was poor in this study. EC50 levels were comparable to the last assessment in 2002 [5], despite a decrease in drug pressure due to a change of national treatment policies to artemisinin-based combination therapy in 2003. Artesunate was highly active against P. falciparum in the present assessment. EC50 levels were similar to recent in vitro and in vivo findings at the study site and in neighbouring countries [20-22]. One isolate showed a diminished sensitivity to artesunate with schizont maturation up to the highest concentration of 85.8 nmol/l and a corresponding EC50 level of 19.9 nmol/l. Another isolate had a comparably high EC50 value of 10.1 nmol/l and a respective cut-off concentration in the WHO microtest of 85.8 nmol/l. These findings support recent in vitro susceptibility assessments by Cojean et al [23], reporting on 6 out of 397 African P. falciparum isolates with dihydroartemisinin EC50 levels above 10 nmol/l and a maximum EC50 of 31.8 nmol/l in one isolate. Especially in the light of increasing availability and use of artemisinins in many parts of Africa, the importance of close surveillance for susceptibility as well as strict deployment of artemisinins exclusively in combination therapy with effective partner drugs cannot be overemphasized.
As in previous reports from Lambaréné, susceptibility to quinine was high in this study. Mean EC50 (204 and 272 nmol/l in HRP-2 assay and WHO microtest, respectively) were comparable to results obtained in 2002 (286 nmol/l) [5]. Despite its widespread use, quinine remains a highly effective anti-malarial in Gabon, especially as drug of choice for parenteral treatment of hospitalized patients.
Comparative assessment of the HRP-2 assay and WHO microtest was performed in order to establish baseline data for the use of the ELISA based assay in Lambaréné in the future. Results obtained by the HRP-2 assay closely paralleled those obtained by the WHO microtest despite methodological problems in this study due to a deficient batch of culture medium. Considering its reduced labour-intensity and good reproducibility the HRP-2 assay can, therefore, be recommended for follow up of anti-malarial drug susceptibility testing and will replace the WHO microtest in future assessments at our study site.
Conclusion
Artesunate, chloroquine and quinine in vitro drug activity was similar, compared to data from earlier in vitro assessments, and results of the HRP-2 assay were comparable to those obtained by the traditional WHO microtest.
The study demonstrated high anti-malarial activity of pyronaridine against fresh field isolates of P. falciparum and corresponded well to recent findings of pyronaridine anti-malarial activity in vivo. Pyronaridine is recommended for further clinical development in combination therapy and continued in vitro drug activity monitoring.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
FK contributed to the conception and design of the study, performed parasite cultivation and microscopic assessment, analysed the data and wrote the manuscript. PP performed parasite cultivation and HRP-2 immunoassay. SB gathered field isolates from patients and performed parasite cultivation. BM contributed to performance of immunoassay and analysis of data, PGK revised the manuscript and supervised the research group, MR conceived and designed the study, contributed to analysis of data, performed second reading for microscopic assessments in WHO microtest and drafted and revised the manuscript. All authors read and approved the final version of the manuscript.
Acknowledgments
Acknowledgements
We thankfully acknowledge the participations of our patients in the Albert Schweitzer Hospital in Lambaréné. This study was supported by a grant of the independent Karl Landsteiner Gesellschaft, Austria.
Contributor Information
Florian Kurth, Email: florian.kurth@uniklinikum-dresden.de.
Peter Pongratz, Email: PPongratz@gmx.at.
Sabine Bélard, Email: sabinebelard@yahoo.de.
Benjamin Mordmüller, Email: benjamin.mordmueller@uni-tuebingen.de.
Peter G Kremsner, Email: peter.kremsner@uni-tuebingen.de.
Michael Ramharter, Email: michael.ramharter@meduniwien.ac.at.
References
- Kremsner PG, Krishna S. Antimalarial combinations. Lancet. 2004;364:285–294. doi: 10.1016/S0140-6736(04)16680-4. [DOI] [PubMed] [Google Scholar]
- Winkler S, Brandts C, Wernsdorfer WH, Graninger W, Bienzle U, Kremsner PG. Drug sensitivity of Plasmodium falciparum in Gabon. Activity correlations between various antimalarials. Trop Med Parasitol. 1994;45:214–218. [PubMed] [Google Scholar]
- Philipps J, Radloff PD, Wernsdorfer W, Kremsner PG. Follow-up of the susceptibility of Plasmodium falciparum to antimalarials in Gabon. Am J Trop Med Hyg. 1998;58:612–618. doi: 10.4269/ajtmh.1998.58.612. [DOI] [PubMed] [Google Scholar]
- Borrmann S, Binder RK, Adegnika AA, Missinou MA, Issifou S, Ramharter M, Wernsdorfer WH, Kremsner PG. Reassessment of the resistance of Plasmodium falciparum to chloroquine in Gabon: implications for the validity of tests in vitro vs. in vivo. Trans R Soc Trop Med Hyg. 2002;96:660–663. doi: 10.1016/S0035-9203(02)90345-7. [DOI] [PubMed] [Google Scholar]
- Ramharter M, Wernsdorfer WH, Kremsner PG. In vitro activity of quinolines against Plasmodium falciparum in Gabon. Acta Trop. 2004;90:55–60. doi: 10.1016/j.actatropica.2003.11.001. [DOI] [PubMed] [Google Scholar]
- In vitro test (mark II) for the assessment of the response of Plasmodium falciparum to chloroquine, mefloquine, quinine, sulfadoxine/pyrimethamine and amodiaquine. WHO document CTD/MAL/97.20 Rev 2 2001 http://www.who.int/drugresistance/malaria/en/markiii.pdf
- Noedl H, Wernsdorfer WH, Miller RS, Wongsrichanalai C. Histidine-rich protein II: a novel approach to malaria drug sensitivity testing. Antimicrob Agents Chemother. 2002;46:1658–1664. doi: 10.1128/AAC.46.6.1658-1664.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang C, Lin-Hua T, Jantanavivat C. Studies on a new antimalarial compound: pyronaridine. Trans R Soc Trop Med Hyg. 1992;86:7–10. doi: 10.1016/0035-9203(92)90414-8. [DOI] [PubMed] [Google Scholar]
- Ramharter M, Kurth F, Schreier AC, Nemeth J, Glasenapp IV, Belard S, Schlie M, Kammer J, Koumba PK, Cisse B, Mordmuller B, Lell B, Issifou S, Oeuvray C, Fleckenstein L, Kremsner PG. Fixed-dose pyronaridine-artesunate combination for treatment of uncomplicated falciparum malaria in pediatric patients in Gabon. J Infect Dis. 2008;198:911–919. doi: 10.1086/591096. [DOI] [PubMed] [Google Scholar]
- Auparakkitanon S, Chapoomram S, Kuaha K, Chirachariyavej T, Wilairat P. Targeting of hematin by the antimalarial pyronaridine. Antimicrob Agents Chemother. 2006;50:2197–2200. doi: 10.1128/AAC.00119-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ringwald P, Bickii J, Basco LK. Efficacy of oral pyronaridine for the treatment of acute uncomplicated falciparum malaria in African children. Clin Infect Dis. 1998;26:946–953. doi: 10.1086/513942. [DOI] [PubMed] [Google Scholar]
- Yang HL, Liu DQ, Yang YM, Huang KG, Dong Y, Yang PF, Liao MZ, Zhang CY. In vitro sensitivity of Plasmodium falciparum to eight antimalarials in China-Myanmar and China-Lao PDR border areas. Southeast Asian J Trop Med Public Health. 1997;28:460–464. [PubMed] [Google Scholar]
- Ramharter M, Adegnika AA, Agnandji ST, Matsiegui PB, Grobusch MP, Winkler S, Graninger W, Krishna S, Yazdanbakhsh M, Mordmüller B, Lell B, Missinou MA, Mavoungou E, Issifou S, Kremsner PG. History and perspectives of medical research at the Albert Schweitzer Hospital in Lambaréné, Gabon. Wien Klin Wochenschr. 2007;119:8–12. doi: 10.1007/s00508-007-0857-5. [DOI] [PubMed] [Google Scholar]
- Wildling E, Winkler S, Kremsner PG, Brandts C, Jenne L, Wernsdorfer WH. Malaria epidemiology in the province of Moyen Ogoov, Gabon. Trop Med Parasitol. 1995;46:77–82. [PubMed] [Google Scholar]
- Pradines B, Mabika Mamfoumbi M, Parzy D, Owono Medang M, Lebeau C, Mourou Mbina JR, Doury JC, Kombila M. In vitro susceptibility of African isolates of Plasmodium falciparum from Gabon to pyronaridine. Am J Trop Med Hyg. 1999;60:105–108. doi: 10.4269/ajtmh.1999.60.105. [DOI] [PubMed] [Google Scholar]
- Vivas L, Rattray L, Stewart L, Bongard E, Robinson BL, Peters W, Croft SL. Anti-malarial efficacy of pyronaridine and artesunate in combination in vitro and in vivo. Acta Trop. 2008;105:222–228. doi: 10.1016/j.actatropica.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Ekland EH, Fidock DA. In vitro evaluations of antimalarial drugs and their relevance to clinical outcomes. Int J Parasitol. 2008;38:743–747. doi: 10.1016/j.ijpara.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pradines B, Tall A, Parzy D, Spiegel A, Fusai T, Hienne R, Trape JF, Doury JC. In-vitro activity of pyronaridine and amodiaquine against African isolates (Senegal) of Plasmodium falciparum in comparison with standard antimalarial agents. J Antimicrob Chemother. 1998;42:333–339. doi: 10.1093/jac/42.3.333. [DOI] [PubMed] [Google Scholar]
- Elueze EI, Croft SL, Warhurst DC. Activity of pyronaridine and mepacrine against twelve strains of Plasmodium falciparum in vitro. J Antimicrob Chemother. 1996;37:511–518. doi: 10.1093/jac/37.3.511. [DOI] [PubMed] [Google Scholar]
- Pradines B, Hovette P, Fusai T, Atanda HL, Baret E, Cheval P, Mosnier J, Callec A, Cren J, Amalvict R, Gardair JP, Rogier C. Prevalence of in vitro resistance to eleven standard or new antimalarial drugs among Plasmodium falciparum isolates from Pointe-Noire, Republic of the Congo. J Clin Microbiol. 2006;44:2404–2408. doi: 10.1128/JCM.00623-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramharter M, Kurth FM, Belard S, Bouyou-Akotet MK, Mamfoumbi MM, Agnandji ST, Missinou MA, Adegnika AA, Issifou S, Cambon N, Heidecker JL, Kombila M, Kremsner PG. Pharmacokinetics of two paediatric artesunate mefloquine drug formulations in the treatment of uncomplicated falciparum malaria in Gabon. J Antimicrob Chemother. 2007;60:1091–1096. doi: 10.1093/jac/dkm355. [DOI] [PubMed] [Google Scholar]
- Ramharter M, Noedl H, Thimasarn K, Wiedermann G, Wernsdorfer G, Wernsdorfer WH. In vitro activity of tafenoquine alone and in combination with artemisinin against Plasmodium falciparum. Am J Trop Med Hyg. 2002;67:39–43. doi: 10.4269/ajtmh.2002.67.39. [DOI] [PubMed] [Google Scholar]
- Cojean S, Hubert V, Le Bras J, Durand R. Resistance to dihydroartemisinin. Emerg Infect Dis. 2006;12:1798–1799. doi: 10.3201/eid1211.060903. [DOI] [PMC free article] [PubMed] [Google Scholar]