Abstract
AIM
To describe the use of psycho-stimulants in the Netherlands between 1996 and 2006 in children and adolescents, and in relation to age and sex.
METHODS
With the pharmacy prescription database the IADB.nl, yearly prevalences of psycho-stimulants per 1000 children were calculated, as was the length of psycho-stimulant use with Kaplan–Meier method in SPSS 12.0.
RESULTS
Psycho-stimulant use increased in boys (0–19) from 4.5‰ in 1996 to 31.1‰ in 2006 and for girls from 0.7 to 8.1‰, respectively. The largest increase was among boys aged 10–19 years. There is a trend towards prescribing the sustained release preparation of methylphenidate (Concerta).
CONCLUSIONS
In the Netherlands a large increase in psycho-stimulants use is observed. However, in the Netherlands the prevalence ratio male/female declined from 6.4 in 1996 to 3.8 in 2006.
Keywords: children and adolescents, mental health, pharmacoepidemiology, stimulants
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT?
In the USA psycho-stimulant use has increased rapidly in the 1990s and stabilized around 2000.
This study describes the prevalence of psycho-stimulant use between1996 and 2006 in the Netherlands.
WHAT THIS STUDY ADDS
The prevalence of psycho-stimulant use among youth in the Netherlands has increased more than eightfold in the period 1996–2006, but in 2006 it is still below the prevalence in the USA.
Introduction
The high increase in psycho-stimulant use in the 1990s has led to widespread discussion about the frequent use of psycho-stimulants in children and adolescents in the USA and Europe. In 2002 the use of psycho-stimulants among US children aged 0–19 years ranged between 3 and 4.3%. [1, 2] There were concerns about side-effects, risks and long term outcome, but also about under-recognition of treatment needs and underdiagnosis of hyperactivity disorders. Despite this, the use of psycho-stimulants increased, as in the Netherlands [3]. Since physicians in the Netherlands are known to be more restrictive in prescribing drugs [3, 4], one might question if this increase in psycho-stimulant use as seen in the USA is also noticeable in the Netherlands.
This study describes the prevalence and duration of use of psycho-stimulants in children and adolescents in the Netherlands from 1996 to 2006, in relation to age and sex.
Methods
For this study the IADB.nl (http://www.iadb.nl) was used, which contains prescription drug-dispensing data from the Netherlands. The estimated population size covered by the IADB.nl increased from 62 000 aged 0–19 years in 1996 to approximately 120 000 aged 0–19 years in 1999 and has remained stable since. The database includes all prescriptions, regardless of prescriber, insurance or reimbursement status, except over-the-counter drugs and drugs dispensed during a hospital stay. Each prescription record comprises information about the drug, date of dispensing, amount dispensed, dose regimen and the prescribing physician. All drugs are coded according to the Anatomical Therapeutic Chemical (ATC) classification [5]. Each patient has a unique, although anonymous, identifier. Due to a high patient pharmacy commitment in the Netherlands and sophisticated pharmacy software, the medication records for each patient are virtually complete [6].
During the study period 1996–2006 we selected all children and adolescents (0–19 years) with at least one psycho-stimulant prescription (ATC code N06BA). Attention deficit hyperactivity disorder (ADHD) medications prescribed were methylphenidate, methylphenidate sustained release and, less frequently, atomoxetine.
The yearly prevalence (1996–2006) of stimulant use was calculated per 1000 with 95% confidence intervals (CIs) for all children and adolescents 0–19 years old and per age category (0–4, 5–9, 10–14 and 15–19 years) and sex.
To test whether the duration of psycho-stimulant use changed over this period, children and adolescents who started to use medication in the period 1996–1999 were compared with those who started between 2001 and 2004. Children and adolescents were regarded starters if they had not had any stimulant prescription before, despite being registered for ≥6 months in the database. Duration of stimulant use was estimated for all incident users using the Kaplan–Meier survival estimator. Stimulant treatment was considered stopped when a child had not received prescribed stimulants for ≥100 consecutive days after the theoretical end date of the final prescription. Cox proportional hazard ratio (HR) with 95% CIs was used to calculate the difference between two cohorts. Statistical analyses were performed in SPSS 12.0 for Windows (SPSS Inc., Chicago, IL, USA). Analogously, duration of use is described for male and female users for the whole period 1996–2006.
Results and discussion
Use of psycho-stimulants had increased among children and adolescents (0–19 years) between 1996 and 2006 from 2.6/1000 to 19.5/1000. The use among boys (0–19 years) increased from 4.5 (3.8–5.3) to 31.1 (29.8–32.5) per 1000 and among girls (0–19 years) from 0.7 (0.5–1.1) to 8.1 (7.4–8.8) per 1000. In 2006 the use of psycho-stimulants among preschoolers (0–4-year-olds) was very low (1/1000 in boys and 0.2/1000 in girls). In 2006, 6.1% (95% CI 5.7, 6.5) of the boys aged 10–14 years and 1.5% (95% CI 1.3, 1.7) of the girls in the same age category received at least one prescription per year for a stimulant. There are significantly more male than female psycho-stimulant users, although the prevalence ratio male/female fell from 6.4 in 1996 to 3.8 in 2006. (See Table 1 for the other age categories.) However, this prevalence ratio male/female is smaller compared with studies from other countries (range 8–10). This suggests more awareness of and attention to ADHD in girls among physicians and parents in the Netherlands.
Table 1.
Psycho-stimulant use among Dutch 0–19-year-olds between the years 1996 and 2006. Prevalence per 1000, related to age and sex
| Age, years | 1996 | 1999 | 2003 | 2006 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0–4 | Pop. male/female | 7 355/7 139 | 13 421/12 868 | 15 512/15 035 | 15 839/14 769 | |||||
| prev. male/1000 | 0.8 (0.3, 1.8) | 1.54 (0.9, 2.3) | 1.2 (0.7, 1.8) | 1.0 (0.5, 1.5) | ||||||
| prev. female/1000 | 0.1 (0.0, 0.8) | 0.5 (0.2, 1.1) | 0.1 (0.0, 0.5) | 0.2 (0.0, 0.6) | ||||||
| Pop. male/female | 7 600/7 628 | 13 367/13 086 | 13 795/13 203 | 14 966/14 309 | ||||||
| 5–9 | prev. male/1000 | 8.8 (6.8, 11.2) | 29.0 (26.2, 32.0) | 23.6 (21.1, 26.3) | 35.5 (32.6, 38.6) | |||||
| prev. female/1000 | 1.2 (0.5, 2.2) | 5.3 (4.1, 6.7) | 6.8 (5.5, 8.4) | 8.5 (7.1, 10.2) | ||||||
| Pop. male/female | 7 961/7 686 | 13 167/13 068 | 13 520/13 571 | 14 306/14 921 | ||||||
| 10–14 | prev. male/1000 | 6.7 (5.0, 8.7) | 28.7 (25.9, 31.7) | 46.4 (43.0, 50.1) | 60.7 (56.8, 64.7) | |||||
| prev. female/1000 | 1.2 (0.5, 2.2) | 5.1 (3.9, 6.4) | 10.7 (9.0, 12.6) | 14.5 (12.6, 16.5) | ||||||
| Pop. male/female | 8 666/8 494 | 15 641/15 612 | 15 898/16 116 | 16 608/17 736 | ||||||
| 15–19 | prev. male/1000 | 2.0 (1.1, 3.1) | 9.3 (7.8, 10.9) | 21.0 (18.8, 23.4) | 30.4 (27.8, 33.1) | |||||
| prev. female/1000 | 0.4 (0.1, 1.0) | 1.9 (1.2, 2.7) | 4.8 (3.8, 6.0) | 8.9 (7.6, 10.4) | ||||||
| All ages: | ||||||||||
| 0–19 | Pop. male/female | 31 582/30 947 | 55 596/54 634 | 58 725/57 925 | 61 719/61 735 | |||||
| prev. male/1000 | 4.5 (3.8, 5.3) | 16.7 (15.7, 17.9) | 22.2 (21.1, 23.5) | 31.1 (29.8, 32.5) | ||||||
| prev. female/1000 | 0.7 (0.5, 1.1) | 3.1 (2.7, 3.6) | 5.4 (4.8, 6.1) | 8.1 (7.4, 8.8) | ||||||
Prevalences per 1000. 95% confidence intervals in parentheses.
Noteworthy was a shift of highest use in 5–9-year-olds in 1996 to highest use in 10–14-year-olds in 2006. A shift in prevalence towards higher use in older age groups could be related to an increased duration of use in recent years. We observed a shorter duration of use in children and adolescents who started in the period 1996–1999 with stimulants compared with those who started between 2001 and 2004 (HR 0.84, 95% CI 0.75, 0.93). We also found a significant difference in duration of use between boys and girls presented in Figure 1 (HR 1.30, 95% CI 1.14, 1.48, adjusted for calendar year).
Figure 1.
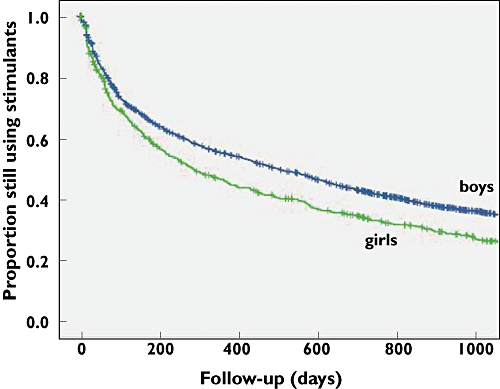
Duration of stimulants drug use for boys (blue) and girls (green) who started therapy between 1996 and 2003. (Kaplan–Meier survival curve, + are censored data)
In recent years, there was a trend towards prescribing the extended-release psycho-stimulants that were introduced in 2003, instead of the immediate-release methylphenidate among all ages in more recent years. In 2006 approximately 30% of all stimulant prescriptions were sustained-release methylphenidate. Atomoxetine, which was introduced in 2002, accounted for <5% of prescriptions. The observed changes indicate that more children and also older children and girls receive treatment with medication for ADHD. A possible explanation may be more awareness of ADHD among physicians and parents. A limitation is that information about diagnoses is lacking. However, previous studies have shown that in 92% of stimulant users it was prescribed for ADHD [3].
Conclusions
Among Dutch children and adolescents aged 0–19 years we found a significant increase in the use of psycho-stimulants from 2.6 per 1000 in 1996 to 19.5 per 1000 in 2006. Use in boys increased from 0.45 to 3.1% (a sixfold increase), but less markedly so in girls from 0.07 to 0.8% (a 12-fold increase). These increases can be attributed to new use, the use of recently introduced preparations and use in older children. The use of stimulants among preschoolers is nil. Compared with the USA, the prevalence of use in Dutch children and adolescents in 2006 is below that among US children aged 0–19 years even when compared with 2002, when it ranged between 3 and 4.3% [1, 2]. These lower prescribing rates might reflect under-recognition of ADHD in the Netherlands. Safety studies on long-term use of stimulants are strongly recommended.
Competing interests
None declared.
REFERENCES
- 1.Zuvekas SH, Vitiello B, Norquist GS. Recent trends in stimulant medication use among U.S. children. Am J Psychiatry. 2006;163:579–85. doi: 10.1176/ajp.2006.163.4.579. Erratum in Am J Psychiatry 2006; 163: 942. [DOI] [PubMed] [Google Scholar]
- 2.Zito JM, Safer DJ, de Jong-van den Berg LTW, Janhsen K, Fegert JM, Gardner JF, Glaeske G, Valluri SC. A three-country comparison of psychtropic medication prevalence in youth. Child and Adolescent Psychiatry and Mental Health. DOI: 10.1186/1753-2000-2-26. [DOI] [PMC free article] [PubMed]
- 3.Faber A. Stimulant Treatment in children: a Dutch Perspective. Enschede, the Netherlands: Gildeprint B.V; 2006. [Google Scholar]
- 4.Cars O, Molstad S, Melander E. Variation in antibiotic use in the European Union. Lancet. 2007;357:1851–3. doi: 10.1016/S0140-6736(00)04972-2. [DOI] [PubMed] [Google Scholar]
- 5.WHO Collaborating Centre for Drugs Statistics Methodology. [last accessed 8 July 2008]. Available at http://www.whoccno/atcddd/
- 6.Tobi H, van den Berg PB, de Jong-van den Berg LTW. The Interaction Database: synergy of science and practice in pharmacy. Lect Notes Comput Sci. 2000;1933:206–21. [Google Scholar]


