Abstract
Primary sclerosing cholangitis (PSC) is a chronic progressive disorder of unknown aetiology characterised by chronic inflammation and stricture formation of the biliary tree. Symptoms include itch and lethargy and in advanced cases cholangitis and end-stage liver disease, however increasing numbers of asymptomatic individuals are being identified. The disease is rare in the general population but is strongly associated with inflammatory bowel disease (IBD) affecting up to 5% of patients with Ulcerative Colitis, with a slightly lower prevalence (up to 3.6%) in Crohn's disease. The strength of this association means that the vast majority (> 90%) of patients with PSC also have IBD, although many may have only mild gastro-intestinal symptoms. Usually IBD presents before PSC, although vice-versa can occur and the onset of both conditions can be separated in some cases by many years. Mean age of diagnosis of PSC is in the fifth decade of life with a strong male predominance. Risk is increased in those with a family history of PSC, suggesting a genetic predisposition and the disease is almost exclusive to non-smokers. The ulcerative colitis associated with PSC is characteristically mild, runs a quiescent course, is associated with rectal sparing, more severe right sided disease, backwash ileitis and has a high risk of pouchitis post-colectomy. Most worrisome is the high risk of colorectal malignancy which necessitates routine colonoscopic surveillance. Cholangiocarcinoma is also a frequent complication of PSC with a 10%-15% lifetime risk of developing this condition. Treatment with high dose ursodeoxycholic acid offers some chemoprotective effects against colorectal malignancy and may decrease symptoms, biochemical and histological progression of liver disease. Small duct PSC patients characteristically have normal cholangiography, and liver biopsy is required for diagnosis, it appears to have a more favourable prognosis. Autoimmune Hepatitis (AIH) is also more prevalent in patients with IBD, with up to 16% of patients with AIH also having ulcerative colitis. A small subgroup of patients have a AIH-PSC overlap syndrome and the management of these patients depends on liver histology, serum IgM levels, autoantibodies, degree of biochemical cholestasis and cholangiography as some of these patients may respond to immunosupression.
Keywords: Primary sclerosing cholangitis, Autoimmune hepatitis, Liver disease, Inflammatory bowel disease, Crohn's disease, Ulcerative colitis
INTRODUCTION
The first association between colonic ulceration and liver disease was made in 1874 by Thomas CH, who described a young man who died of a ‘much enlarged, fatty liver in the presence of ulceration of the colon’[1]. The association was confirmed by James Lister in 1899, who reported a patient with ulcerative colitis and secondary diffuse hepatitis[2]. Over the next 100 years it has become well established that there is a close relationship between inflammatory bowel disease and various hepatobiliary disorders. These disorders are listed in Table 1.
Table 1.
Hepatobiliary disorders associated with inflammatory bowel disease
| Hepatobiliary disorders |
Associated with |
|
| Ulcerative colitis | Crohn’s disease | |
| Primary sclerosing cholangitis (PSC) | ||
| Large duct PSC | + | + |
| Small duct PSC (‘pericholangitis’) | + | + |
| Cirrhosis | + | + |
| Hepatoma | + | + |
| Cholangiocarcinoma | + | + |
| Miscellaneous disorders | ||
| Fatty liver | + | + |
| Granulomas | + | |
| Amyloidosis | + | |
| Hepatic abscess | + | |
| Gallstones | + | |
| Autoimmune hepatitis | + | |
| Primary biliary cirrhosis | (+) | |
| Budd-Chiari syndrome | (+) | (+) |
+: Definite association; (+): Possible association.
PRIMARY SCLEROSING CHOLANGITIS
First described by Smith and Loe in 1965[3] Primary sclerosing cholangitis (PSC) is a chronic progressive disorder of unknown aetiology characterised by inflam-mation, fibrosis and stricture formation in medium and large sized ducts in the biliary tree[4,5]. Common symptoms include itch and lethargy although many patients (up to 45%) are asymptomatic, even with advanced disease[5]. The disease is strongly associated with Inflammatory Bowel Disease and may be detected as an incidental finding of a raised serum alkaline phosphatase. Magnetic resonance cholangography (MRCP) and endoscopic cholangiography (ERCP) are diagnostic, demonstrating the diffuse multifocal strictures and dilatation giving rise to a characteristic ‘beaded’ appearance (Figure 1).
Figure 1.
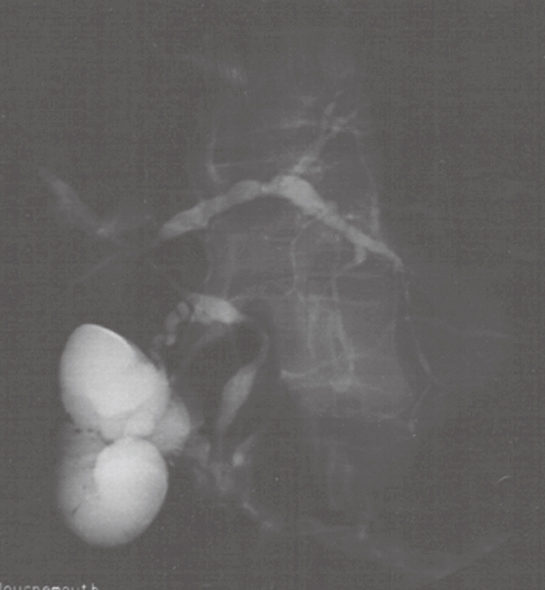
Endoscopic Retrograde Cholangiogram showing the classic ‘beaded’ appearance of bile ducts in Primary Sclerosing Cholangitis.
Prevalence
PSC is rare in the general population. Data from Olmsted County (USA) in the year 2000 identified 20.9 cases of PSC per 100 000 of the population in men and 6.3 per 100 000 in women[6], which is similar to that seen in the UK[7]. There has been a suggestion that the incidence may be rising. In Spain the prevalence in 1988 was 2.24 per million having been 0.78 cases per million in 1984[8]. It is however unclear if this represents a true increase in the disease or improved case recognition due to improved diagnostics particularly in asymptomatic individuals.
PSC in IBD
Because of its strong association with inflammatory bowel disease (IBD) PSC is far more common in patients with ulcerative colitis (UC). The prevalence quoted in different case series varies widely, largely due to differences in the number of patients included with severe, active, or extensive inflammatory bowel disease studied and also in the method used to investigate liver dysfunction. Studies on unselected patients provide the most accurate data but are ethically difficult as both liver biopsy and ERCP are associated with significant morbidity. In an early study of unselected adult patients from Oxford, 5%-6% of the 300 patients with ulcerative colitis had significant histological abnormalities on hepatic histology compared with 10% of 100 unselected patients with Crohn’s disease; none of these patients underwent cholangiography[9,10]. Studies (Table 2) using selected patients include a large Swedish study of 1500 patients with UC where it was found that 5% of patients had increased serum Alkaline Phosphatase and, of those who underwent ERCP, 85% had evidence of PSC, being more common in men and those with pancolitis[11]. Other reports have found similar results. In a study from Oslo, 14% of patients had evidence of hepatobiliary pathology with 4% of patients with UC having PSC[12]. Thus it is generally accepted that approximately 5% of patients with UC will have associated PSC.
Table 2.
Prevalence of primary sclerosing cholangitis in patients with ulcerative colitis
The percentage of Crohn's disease patients affected by PSC is much smaller[13]. In one study of 262 patients, 38 (15%) had abnormal liver function tests and underwent ERCP and liver biopsy, 9 of these (3.4% of the total) had PSC[14]. Crohn's disease associated with PSC is generally seen in patients who have extensive colonic or ileocolonic disease, or in paediatric populations.
IBD in PSC
Vice versa the great majority of patients with PSC have underlying IBD. The frequency with which it is recognised again varies widely depending on the intensity with which it is sought, varying from a minimum 25% of all PSC patients having IBD if identified by clinical history alone to 90% of patients if biopsies of rectum and sigmoid are taken at the time of flexible Sigmoidoscopy[15]. There are also large geographical variations in the prevalence of IBD in PSC (Table 3). Since the recognition of inflammatory bowel disease has important implications in terms of risk of colorectal cancer (PSC patients without IBD are not at increased risk of colorectal cancer and do not require colonoscopic surveillance[16]) it is the authors practice to perform colonoscopy and serial biopsies in all patients with newly diagnosed PSC.
Table 3.
Prevalence of inflammatory bowel disease in patients with primary sclerosing cholangitis (PSC)
Aetiology
The aetiology of PSC itself is unknown. The 2:1 male to female gender ratio of patients and the relatively poor response of the disease to immunosuppression suggest that PSC is not a classic autoimmune disease. However the association of PSC with IBD, autoimmune diseases, and a host of other humoral and cellular immune abnormalities (Table 4) make an immunopathogenic mechanism likely. Particularly common serological abnormalities are raised IgM levels in up to 50% and positive anti-smooth muscle antibodies and antinuclear antibodies in up to 75%[21]. Anti Neutrophil Cytoplasmic Antibodies with a pericellular pattern (pANCA) are also a common finding, being present in 80% of patients being and unrelated to the presence or absence of UC. Cellular immunity anomalies include portal tract infiltration of functional T cells, restricted T cell receptor repertoire, and aberrant expression of HLA and costimulatory molecules on biliary epithelial cells.
Table 4.
Evidence for the influence of immune mechanisms on the aetiology of PSC
| Humoral immunity | Increased circulating immune complexes |
| Elevated immunoglobulin levels (IgG and IgM) | |
| Low titres of non-organ specific autoantibodies (ANA and SMA) | |
| High titres of antineutrophil antibodies | |
| Autoantibodies to BEC surface antigens | |
| Cell mediated immunity | Decreased levels of circulating peripheral CD8+ve Tcells |
| Portal T cell and NK cell infiltrate | |
| Increased activated and memory T cells | |
| Restricted T cell receptor repertoire (Vβ3) | |
| Aberrant expression of HLA-DR on BEC | |
| Coexpression of costimulatory molecules and HLA-DR on BECs | |
| Increased circulating and tissue bound adhesion molecules | |
| Immune effector mechanisms | Enhanced cytokine expression in the liver |
| Immunogenetic mechanisms | HLA associations |
Immunogenetic studies have identified a number of key HLA haplotypes (Table 5) associated with PSC, HLA-B8/DR3 haplotype being particularly common in patients with PSC and UC and infrequent in patients with PSC alone[22]. This haplotype is also associated with other organ-specific autoimmune disease including coeliac disease, thyrotoxicosis, lupoid autoimmune hepatitis, myasthenia gravis, and type 1 diabetes mellitus. However PSC, independent of HLA type, is also associated with a range of autoimmune diseases, diabetes mellitus and Graves disease being the most common. Saarinen et al found that 25% of patients with PSC had one or more autoimmune disease, compared to 9% of patients with inflammatory bowel disease alone[23].
Table 5.
Key HLA haplotypes associated with primary sclerosing cholangitis
| Haplotype | Significance in PSC |
| B8-TNF*2-DRB3*0101-DRB1*0301-DQA1*0501-DQB1*0201 | Strong association with disease susceptibility |
| DRB3*0101-DRB1*1301-DQA1*0103-DQB1*0603 | Strong association with disease susceptibility |
| DRB5*0101-DRB1*1501-DQA1*0102-DQB1*0602 | Weak association with disease susceptibility |
| DRB4*0103-DRB1*0401-DQA1*03-DQB1*0302 | Strong association with protection against disease |
| MICA*008 | Strong association with disease susceptibility |
Possible explanations for the PSC association with IBD include the development of autoantibodies to an unknown antigen in an immunogenetically susceptible host which cross reacts with biliary and colonic epithelium and is capable of inducing complement activation[24]. Alternatively, the initiation of the immune response may be the ingress of bacteria or other toxic metabolites through the diseased bowel wall.
CLINICAL COURSE
Onset
PSC is a disease of middle age with a mean age of diagnosis is 40 years in men and 45 years in women. Bowel symptoms have usually developed before those of PSC and UC is therefore usually diagnosed several years before PSC. However occassionally symptoms of PSC may precede IBD by up to 4 years[25]. The age of onset of the symptoms also has important implications as there is evidence to suggest patients with Colitis in childhood have a high prevalence of liver abnormalities than adults, with up to 60% children having abnormal liver function tests[26].
Risk factors
Unlike other immune mediated diseases PSC is far more common in men with 70% of all PSC patients being male. This male preponderance is absent in PSC patients without associated IBD, being equally common in both males and females[27]. In addition to IBD and male sex, another recognised risk factor is a family history of the disease, There is a 0.7% risk in first degree relatives of patients with PSC rising to 1.5% in siblings of affected individuals[28].
Smoking is a well recognized protective factor against the development of ulcerative colitis, and three studies have suggested that cigarette smoking may also additionally protect against the development of PSC. Moreover, this protective effect was more marked in patients with primary sclerosing cholangitis than ulcerative colitis and was seen in patients with and without inflammatory bowel disease[29–31]. The mechanism of protection in both disorders remains unknown.
Clinical characteristics of IBD associated with PSC
There are a number of unique features of Ulcerative Colitis associated with PSC (Table 6). The colitis is often mild, asymptomatic and runs a quiescent course[32]. It is associated with rectal sparing[33]; and therefore not seen on rigid sigmoidoscopy; is often more severe proximally and associated with backwash ileitis. It may be visible microscopically with a relatively normal macroscopic appearance and pouchitis is far more common after colectomy and ileo-anal pouch formation, occurring in up to 60% of PSC patients compared to 15% in patients with UC alone[34].
Table 6.
Clinical, Endoscopic, and Histological findings that characterize IBD-PSC
| Male predominance |
| Quiescent colitis |
| Pancolitis |
| Rectal sparing |
| Backwash ileitis |
| Pouchitis |
| Colorectal dysplasia/carcinoma |
| Different extracolonic manifestations |
Most importantly PSC is a significant risk factor for the development of carcinoma of the colon in patients with inflammatory bowel disease[35–37]. A meta-analysis demonstrated a four fold increase in colon cancer in UC patients with PSC when compared to UC alone (RR 4.26 95% CI 2.8-6.48)[38]. The risk of proximal cancer is particularly increased[37,39]. Additional risk factors are duration and extent of disease and a family history of colorectal cancer[40]. Current U.K. guidelines therefore recommend annual screening colonoscopy in IBD patients with PSC[41].
Treatment of PSC with ursodeoxycholic acid appears to have a chemopreventative effect decreasing the incidence of carcinoma of the colon and is therefore recommended[42]. Treatment with 5-aminosalicylic acid (5-ASA) compounds have also been shown to reduce the risk of colorectal cancer in general patients with UC[43]. There are no studies specific for PSC/IBD patients in this context but it is reasonable to infer that it will be protective and is also therefore recommended.
Prognosis
Despite treatment however PSC is generally progressive and prognosis poor. Median survival without liver transplantation after diagnosis is approximately 12 years[44] with survival worse for those who are symptomatic at presentation[45].
The major cause of mortality is the occurrence of cholangiocarcinoma, which is significantly increased in patients with PSC who display a 10%-15% lifetime risk of developing the disease. This risk is higher in patients with associated inflammatory bowel disease than those with PSC alone, with an estimated annual incidence of 0.5%-1%[46–48]. Unfortunately there remains no validated screening tool for cholangiocarcinoma and therefore tumours often present at an advanced stage and have a poor prognosis. Other complications of PSC include osteoporosis, this is a frequent finding the mechanism of which remains unclear[49]. Bone density measurement should therefore be considered in these patients.
PSC treatment
Treatments which have been tried in an attempt to pre-vent progression of the liver disease to cirrhosis and to decrease the risk of complications especially malignancy include tacrolimus[50], methotrexate[51], corticoteroids[52], D-penillamine[53], etanercept[54], cyclosporin[55], azathioprine, 6-mercaptopurine[56] and pentoxifylline[57]. None of these agents have demonstrated any consistent benefit.
Ursodeoxycholic acid (UDCA) is the only drug which has been demonstrated to have a positive effect. It is also the most extensively studied[58] with some, but not all, studies showing improvements in biochemistry, symptoms and histology[59–64]. The most promising data is for long term UDCA used at high dose, 20-30 mg/kg per day (in divided doses), as this may increase clinical benefit and decrease histological progression of disease[65,66]. In view of its chemopreventative effect against colon cancer and its low incidence of side effects, high-dose UDCA is currently the best available treatment for PSC.
The concurrence of both conditions also requires that the impact of treatment of either disease on the other must be considered. Proctocolectomy appears to have no effect on liver biochemistry, histology or survival of patients with PSC and chronic UC[67]. However the natural history of UC following liver transplantation is variable[68–72]. One study showed approximately a third had improvement in colitis, a third remained unchanged and a third suffered increased activity of colonic disease[73]. Several series report increased rates of colon cancer and colectomy after liver transplantation[74–76]. It remains unclear if this is due to longstanding immunosuppressant use or confounding variables such as long duration of disease.
SMALL DUCT PSC
A variant of the disease called ‘small duct PSC’ is applied to the small percentage of patients with characteristic clinical findings but who have a normal cholangiogram. The absence of macroscopic abnormalities necessitates liver biopsy for the diagnosis of small-duct PSC. Characteristic features of PSC on liver biopsy are concentric rings of connective tissue around bile ducts, the so-called ‘onion ring’ appearance[77]. Other features which are less specific include enlargement of the portal triads, periportal inflammation with mononuclear and polymorphonuclear cells, oedema and bile duct proliferation. Extension into the hepatic parenchyma with bridging fibrosis and ultimately cirrhosis represents advanced disease.
Small duct PSC appears to have a more favourable prognosis with a median survival 29.5 years compared to 17 years for classical PSC[78–81], although occasionally patients with small duct PSC progress to large duct disease.
AUTOIMMUNE HEPATITIS AND OVERLAP SYNDROMES IN IBD
Patients with IBD are also at increased risk of other of immune mediated liver disease including autoimmune hepatitis (AIH). In one study, UC was present in 16% of patients with AIH[82]. AIH and PSC may also occur within the same individual and it remains unclear if this represents the independent occurrence of both diseases, either sequentially or concurrently, the presence of a distinct overlap syndrome or different stages in the evolution of a single disease entity.
Difficulties with definitions and thus classification of these patients has led to widely varying estimates as to the frequency of the coexistence of the two conditions with studies ranging from 7.6% to 53.8%. of patients with PSC have features of AIH[83–89]. and conversely an abnormal cholangiogram being present in 42% of patients with AIH and UC. The association between AIH and PSC appears more common in the paediatric population.
Patients with PSC should be suspected of having associated AIH or AIH-PSC overlap if they have interface hepatitis on biopsy, high serum IgG levels, lower ALP and the presence of autoantibodies (ANA or SMA titre > 1:40). It is important to identify these patients as they maybe responsive to treatment with steroids[85].
Patients with AIH should be suspected of having associated PSC or AIH-PSC overlap[90] if they have pruritis, UC, bile duct abnormalities on histology, cholestatic liver biochemistry (ALP × 2 ULN) and abnormal cho-langiography. These patients tend to be unresponsive to steroids[87,91–93].
CONCLUSION
From the original descriptions of liver disease associated with disease of the bowel over a century ago much progress has been made. The association of inflammatory bowel disease with PSC, AIH and overlap syndromes is now well established and much is known on the epidemiology and course of the conditions. Although there remain many more questions than answers, an increasingly developed concept of hepatobiliary disorder in inflammatory bowel disease has emerged. It is suggested that the major hepatobiliary diseases seen in association with both UC and Crohn’s disease, namely PSC, cirrhosis, cholangiocarcinoma, and most cases of autoimmune hepatitis, represent different aspects of the same spectrum of hepatobiliary disease. However what is cause, what is consequence and what is coincidence remains to be seen.
Footnotes
S- Editor Liu Y E- Editor Liu Y
References
- 1.Thomas CH. Ulceration of the colon with a much enlarged fatty liver. Trans Pathol Soc Phil. 1873;4:87–88. [Google Scholar]
- 2.Lister JD. A specimen of diffuse ulcerative colitis with secondary diffuse hepatitis. Trans Pathol Soc Lon. 1899;50:130–134. [Google Scholar]
- 3.Smith MP, Loe RH. Sclerosing cholangitis; review of recent case reports and associated diseases and four new cases. Am J Surg. 1965;110:239–246. doi: 10.1016/0002-9610(65)90018-8. [DOI] [PubMed] [Google Scholar]
- 4.Lee YM, Kaplan MM. Primary sclerosing cholangitis. N Engl J Med. 1995;332:924–933. doi: 10.1056/NEJM199504063321406. [DOI] [PubMed] [Google Scholar]
- 5.Angulo P, Lindor KD. Primary sclerosing cholangitis. Hepatology. 1999;30:325–332. doi: 10.1002/hep.510300101. [DOI] [PubMed] [Google Scholar]
- 6.Bambha K, Kim WR, Talwalkar J, Torgerson H, Benson JT, Therneau TM, Loftus EV Jr, Yawn BP, Dickson ER, Melton LJ 3rd. Incidence, clinical spectrum, and outcomes of primary sclerosing cholangitis in a United States community. Gastroenterology. 2003;125:1364–1369. doi: 10.1016/j.gastro.2003.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Kingham JG, Kochar N, Gravenor MB. Incidence, clinical patterns, and outcomes of primary sclerosing cholangitis in South Wales, United Kingdom. Gastroenterology. 2004;126:1929–1930. doi: 10.1053/j.gastro.2004.04.052. [DOI] [PubMed] [Google Scholar]
- 8.Escorsell A, Pares A, Rodes J, Solis-Herruzo JA, Miras M, de la Morena E. Epidemiology of primary sclerosing cholangitis in Spain. Spanish Association for the Study of the Liver. J Hepatol. 1994;21:787–791. doi: 10.1016/s0168-8278(94)80240-8. [DOI] [PubMed] [Google Scholar]
- 9.Perrett AD, Higgins G, Johnston HH, Massarella GR, Truelove SC, Wright R. The liver in ulcerative colitis. Q J Med. 1971;40:211–238. doi: 10.1093/oxfordjournals.qjmed.a067266. [DOI] [PubMed] [Google Scholar]
- 10.Perrett AD, Higgins G, Johnston HH, Massarella GR, Truelove SC, Wrigth R. The liver in Crohn's disease. Q J Med. 1971;40:187–209. doi: 10.1093/oxfordjournals.qjmed.a067265. [DOI] [PubMed] [Google Scholar]
- 11.Olsson R, Danielsson A, Jarnerot G, Lindstrom E, Loof L, Rolny P Rydén BO, Tysk C, Wallerstedt S. Prevalence of primary sclerosing cholangitis in patients with ulcerative colitis. Gastroenterology. 1991;100:1319–1323. [PubMed] [Google Scholar]
- 12.Schrumpf E, Elgjo K, Fausa O, Gjone E, Kolmannskog F, Ritland S. Sclerosing cholangitis in ulcerative colitis. Scand J Gastroenterol. 1980;15:689–697. doi: 10.3109/00365528009181516. [DOI] [PubMed] [Google Scholar]
- 13.Atkinson AJ, Carroll WW. Sclerosing cholangitis. association with regional enteritis. JAMA. 1964;188:183–184. [PubMed] [Google Scholar]
- 14.Rasmussen HH, Fallingborg JF, Mortensen PB, Vyberg M, Tage-Jensen U, Rasmussen SN. Hepatobiliary dysfunction and primary sclerosing cholangitis in patients with Crohn's disease. Scand J Gastroenterol. 1997;32:604–610. doi: 10.3109/00365529709025107. [DOI] [PubMed] [Google Scholar]
- 15.Tung BY, Bretnall T, Kowdley KV. Diagnosis and prevelence of ulcerative colitis in patients with sclerosing cholangitis (abstract) Hepatology. 1996;24:169A. [Google Scholar]
- 16.Rutter MD, Saunders BP, Wilkinson KH, Kamm MA, Williams CB, Forbes A. Most dysplasia in ulcerative colitis is visible at colonoscopy. Gastrointest Endosc. 2004;60:334–339. doi: 10.1016/s0016-5107(04)01710-9. [DOI] [PubMed] [Google Scholar]
- 17.Broome U, Glaumann H, Hultcrantz R. Liver histology and follow up of 68 patients with ulcerative colitis and normal liver function tests. Gut. 1990;31:468–472. doi: 10.1136/gut.31.4.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiesner RH, LaRusso NF. Clinicopathologic features of the syndrome of primary sclerosing cholangitis. Gastroenterology. 1980;79:200–206. [PubMed] [Google Scholar]
- 19.Okolicsanyi L, Fabris L, Viaggi S, Carulli N, Podda M, Ricci G. Primary sclerosing cholangitis: clinical presentation, natural history and prognostic variables: an Italian multicentre study. The Italian PSC Study Group. Eur J Gastroenterol Hepatol. 1996;8:685–691. [PubMed] [Google Scholar]
- 20.Okada H, Mizuno M, Yamamoto K, Tsuji T. Primary sclerosing cholangitis in Japanese patients: association with inflammatory bowel disease. Acta Med Okayama. 1996;50:227–235. doi: 10.18926/AMO/30499. [DOI] [PubMed] [Google Scholar]
- 21.Woolf GM, Vierling JM. Disappearing intrahepatic bile ducts: the syndromes and their mechanisms. Semin Liver Dis. 1993;13:261–275. doi: 10.1055/s-2007-1007354. [DOI] [PubMed] [Google Scholar]
- 22.van Milligen de Wit AW, van Deventer SJ, Tytgat GN. Immunogenetic aspects of primary sclerosing cholangitis: implications for therapeutic strategies. Am J Gastroenterol. 1995;90:893–900. [PubMed] [Google Scholar]
- 23.Saarinen S, Olerup O, Broome U. Increased frequency of autoimmune diseases in patients with primary sclerosing cholangitis. Am J Gastroenterol. 2000;95:3195–3199. doi: 10.1111/j.1572-0241.2000.03292.x. [DOI] [PubMed] [Google Scholar]
- 24.Chapman RW, Cottone M, Selby WS, Shepherd HA, Sherlock S, Jewell DP. Serum autoantibodies, ulcerative colitis and primary sclerosing cholangitis. Gut. 1986;27:86–91. doi: 10.1136/gut.27.1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fausa O, Schrumpf E, Elgjo K. Relationship of inflammatory bowel disease and primary sclerosing cholangitis. Semin Liver Dis. 1991;11:31–39. doi: 10.1055/s-2008-1040420. [DOI] [PubMed] [Google Scholar]
- 26.Nemeth A, Ejderhamn J, Glaumann H, Strandvik B. Liver damage in juvenile inflammatory bowel disease. Liver. 1990;10:239–248. doi: 10.1111/j.1600-0676.1990.tb00465.x. [DOI] [PubMed] [Google Scholar]
- 27.Rabinovitz M, Gavaler JS, Schade RR, Dindzans VJ, Chien MC, Van Thiel DH. Does primary sclerosing cholangitis occurring in association with inflammatory bowel disease differ from that occurring in the absence of inflammatory bowel disease? A study of sixty-six subjects. Hepatology. 1990;11:7–11. doi: 10.1002/hep.1840110103. [DOI] [PubMed] [Google Scholar]
- 28.Bergquist A, Lindberg G, Saarinen S, Broome U. Increased prevalence of primary sclerosing cholangitis among first-degree relatives. J Hepatol. 2005;42:252–256. doi: 10.1016/j.jhep.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 29.Loftus EV Jr, Sandborn WJ, Tremaine WJ, Mahoney DW, Zinsmeister AR, Offord KP, Melton LJ 3rd. Primary sclerosing cholangitis is associated with nonsmoking: a case-control study. Gastroenterology. 1996;110:1496–1502. doi: 10.1053/gast.1996.v110.pm8613055. [DOI] [PubMed] [Google Scholar]
- 30.van Erpecum KJ, Smits SJ, van de Meeberg PC, Linn FH, Wolfhagen FH, vanBerge-Henegouwen GP, Algra A. Risk of primary sclerosing cholangitis is associated with nonsmoking behavior. Gastroenterology. 1996;110:1503–1506. doi: 10.1053/gast.1996.v110.pm8613056. [DOI] [PubMed] [Google Scholar]
- 31.Mitchell SA, Thyssen M, Orchard TR, Jewell DP, Fleming KA, Chapman RW. Cigarette smoking, appendectomy, and tonsillectomy as risk factors for the development of primary sclerosing cholangitis: a case control study. Gut. 2002;51:567–573. doi: 10.1136/gut.51.4.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lundqvist K, Broome U. Differences in colonic disease activity in patients with ulcerative colitis with and without primary sclerosing cholangitis: a case control study. Dis Colon Rectum. 1997;40:451–456. doi: 10.1007/BF02258391. [DOI] [PubMed] [Google Scholar]
- 33.Loftus EV Jr, Harewood GC, Loftus CG, Tremaine WJ, Harmsen WS, Zinsmeister AR, Jewell DA, Sandborn WJ. PSC-IBD: a unique form of inflammatory bowel disease associated with primary sclerosing cholangitis. Gut. 2005;54:91–96. doi: 10.1136/gut.2004.046615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Penna C, Dozois R, Tremaine W, Sandborn W, LaRusso N, Schleck C, Ilstrup D. Pouchitis after ileal pouch-anal anastomosis for ulcerative colitis occurs with increased frequency in patients with associated primary sclerosing cholangitis. Gut. 1996;38:234–239. doi: 10.1136/gut.38.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brentnall TA, Haggitt RC, Rabinovitch PS, Kimmey MB, Bronner MP, Levine DS, Kowdley KV, Stevens AC, Crispin DA, Emond M, et al. Risk and natural history of colonic neoplasia in patients with primary sclerosing cholangitis and ulcerative colitis. Gastroenterology. 1996;110:331–338. doi: 10.1053/gast.1996.v110.pm8566577. [DOI] [PubMed] [Google Scholar]
- 36.Broome U, Lofberg R, Veress B, Eriksson LS. Primary sclerosing cholangitis and ulcerative colitis: evidence for increased neoplastic potential. Hepatology. 1995;22:1404–1408. doi: 10.1002/hep.1840220511. [DOI] [PubMed] [Google Scholar]
- 37.Shetty K, Rybicki L, Brzezinski A, Carey WD, Lashner BA. Shetty K, Rybicki L, Brzezinski A, Carey WD, Lashner BA. The risk for cancer or dysplasia in ulcerative colitis patients with primary sclerosing cholangitis. Am J Gastroenterol. 1999;94:1643–1649. doi: 10.1111/j.1572-0241.1999.01156.x. [DOI] [PubMed] [Google Scholar]
- 38.Soetikno RM, Lin OS, Heidenreich PA, Young HS, Blackstone MO. Increased risk of colorectal neoplasia in patients with primary sclerosing cholangitis and ulcerative colitis: a meta-analysis. Gastrointest Endosc. 2002;56:48–54. doi: 10.1067/mge.2002.125367. [DOI] [PubMed] [Google Scholar]
- 39.Marchesa P, Lashner BA, Lavery IC, Milsom J, Hull TL, Strong SA, Church JM, Navarro G, Fazio VW. The risk of cancer and dysplasia among ulcerative colitis patients with primary sclerosing cholangitis. Am J Gastroenterol. 1997;92:1285–1288. [PubMed] [Google Scholar]
- 40.Eaden J. Review article: colorectal carcinoma and inflammatory bowel disease. Aliment Pharmacol Ther. 2004;20 Suppl 4:24–30. doi: 10.1111/j.1365-2036.2004.02046.x. [DOI] [PubMed] [Google Scholar]
- 41.Eaden JA, Mayberry JF. Guidelines for screening and surveillance of asymptomatic colorectal cancer in patients with inflammatory bowel disease. Gut. 2002;51 Suppl 5:V10–V12. doi: 10.1136/gut.51.suppl_5.v10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pardi DS, Loftus EV Jr, Kremers WK, Keach J, Lindor KD. Ursodeoxycholic acid as a chemopreventive agent in patients with ulcerative colitis and primary sclerosing cholangitis. Gastroenterology. 2003;124:889–893. doi: 10.1053/gast.2003.50156. [DOI] [PubMed] [Google Scholar]
- 43.Eaden J. Review article: the data supporting a role for aminosalicylates in the chemoprevention of colorectal cancer in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18 Suppl 2:15–21. doi: 10.1046/j.1365-2036.18.s2.3.x. [DOI] [PubMed] [Google Scholar]
- 44.Farrant JM, Hayllar KM, Wilkinson ML, Karani J, Portmann BC, Westaby D, Williams R. Natural history and prognostic variables in primary sclerosing cholangitis. Gastroenterology. 1991;100:1710–1717. doi: 10.1016/0016-5085(91)90673-9. [DOI] [PubMed] [Google Scholar]
- 45.Broome U, Olsson R, Loof L, Bodemar G, Hultcrantz R, Danielsson A, Prytz H, Sandberg-Gertzen H, Wallerstedt S, Lindberg G. Natural history and prognostic factors in 305 Swedish patients with primary sclerosing cholangitis. Gut. 1996;38:610–615. doi: 10.1136/gut.38.4.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Burak K, Angulo P, Pasha TM, Egan K, Petz J, Lindor KD. Incidence and risk factors for cholangiocarcinoma in primary sclerosing cholangitis. Am J Gastroenterol. 2004;99:523–526. doi: 10.1111/j.1572-0241.2004.04067.x. [DOI] [PubMed] [Google Scholar]
- 47.Levy C, Lymp J, Angulo P, Gores GJ, Larusso N, Lindor KD. The value of serum CA 19-9 in predicting cholangiocarcinomas in patients with primary sclerosing cholangitis. Dig Dis Sci. 2005;50:1734–1740. doi: 10.1007/s10620-005-2927-8. [DOI] [PubMed] [Google Scholar]
- 48.Bjornsson E, Kilander A, Olsson R. CA 19-9 and CEA are unreliable markers for cholangiocarcinoma in patients with primary sclerosing cholangitis. Liver. 1999;19:501–508. doi: 10.1111/j.1478-3231.1999.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 49.Hay JE, Lindor KD, Wiesner RH, Dickson ER, Krom RA, LaRusso NF. The metabolic bone disease of primary sclerosing cholangitis. Hepatology. 1991;14:257–261. [PubMed] [Google Scholar]
- 50.Van Thiel DH, Carroll P, Abu-Elmagd K, Rodriguez-Rilo H, Irish W, McMichael J, Starzl TE. Tacrolimus (FK 506), a treatment for primary sclerosing cholangitis: results of an open-label preliminary trial. Am J Gastroenterol. 1995;90:455–459. [PMC free article] [PubMed] [Google Scholar]
- 51.Kaplan MM, Arora S, Pincus SH. Primary sclerosing cholangitis and low-dose oral pulse methotrexate therapy. Clinical and histologic response. Ann Intern Med. 1987;106:231–235. doi: 10.7326/0003-4819-106-2-231. [DOI] [PubMed] [Google Scholar]
- 52.Kochhar R, Goenka MK, Das K, Nagi B, Bhasin DK, Chawla YK, Vaiphei K, Singh K, Dilawari JB. Primary sclerosing cholangitis: an experience from India. J Gastroenterol Hepatol. 1996;11:429–433. doi: 10.1111/j.1440-1746.1996.tb00286.x. [DOI] [PubMed] [Google Scholar]
- 53.Klingenberg SL, Chen W. D-penicillamine for primary sclerosing cholangitis. Cochrane Database Syst Rev. 2006;11:CD004182. doi: 10.1002/14651858.CD004182.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Epstein MP, Kaplan MM. A pilot study of etanercept in the treatment of primary sclerosing cholangitis. Dig Dis Sci. 2004;49:1–4. doi: 10.1023/b:ddas.0000011827.87103.2e. [DOI] [PubMed] [Google Scholar]
- 55.Wiesner RH, Steiner B, LaRusso NF, Lindor KD, Baldus WP. A controlled trial evaluating cyclosporine in the treatment of primary sclerosing cholangitis (abstract) Hepatology. 1991;14:63A. [Google Scholar]
- 56.Wagner A. Azathioprine treatment in primary sclerosing cholangitis. Lancet. 1971;2:663–664. doi: 10.1016/s0140-6736(71)80107-1. [DOI] [PubMed] [Google Scholar]
- 57.Bharucha AE, Jorgensen R, Lichtman SN, LaRusso NF, Lindor KD. A pilot study of pentoxifylline for the treatment of primary sclerosing cholangitis. Am J Gastroenterol. 2000;95:2338–2342. doi: 10.1111/j.1572-0241.2000.02324.x. [DOI] [PubMed] [Google Scholar]
- 58.Liu J, Kjaergard LL, Als-Nielsen B, Gluud C. Artificial and bioartificial support systems for liver failure: a Cochrane Hepato-Biliary Group Protocol. Liver. 2002;22:433–438. doi: 10.1034/j.1600-0676.2002.01554.x. [DOI] [PubMed] [Google Scholar]
- 59.Beuers U, Spengler U, Kruis W, Aydemir U, Wiebecke B, Heldwein W, Weinzierl M, Pape GR, Sauerbruch T, Paumgartner G. Ursodeoxycholic acid for treatment of primary sclerosing cholangitis: a placebo-controlled trial. Hepatology. 1992;16:707–714. doi: 10.1002/hep.1840160315. [DOI] [PubMed] [Google Scholar]
- 60.Chazouilleres O, Poupon R, Capron JP, Metman EH, Dhumeaux D, Amouretti M, Couzigou P, Labayle D, Trinchet JC. Ursodeoxycholic acid for primary sclerosing cholangitis. J Hepatol. 1990;11:120–123. doi: 10.1016/0168-8278(90)90281-u. [DOI] [PubMed] [Google Scholar]
- 61.Stiehl A, Walker S, Stiehl L, Rudolph G, Hofmann WJ, Theilmann L. Effect of ursodeoxycholic acid on liver and bile duct disease in primary sclerosing cholangitis. A 3-year pilot study with a placebo-controlled study period. J Hepatol. 1994;20:57–64. doi: 10.1016/s0168-8278(05)80467-2. [DOI] [PubMed] [Google Scholar]
- 62.De Maria N, Colantoni A, Rosenbloom E, Van Thiel DH. Ursodeoxycholic acid does not improve the clinical course of primary sclerosing cholangitis over a 2-year period. Hepatogastroenterology. 1996;43:1472–1479. [PubMed] [Google Scholar]
- 63.Lindor KD. Ursodiol for primary sclerosing cholangitis. Mayo Primary Sclerosing Cholangitis-Ursodeoxycholic Acid Study Group. N Engl J Med. 1997;336:691–695. doi: 10.1056/NEJM199703063361003. [DOI] [PubMed] [Google Scholar]
- 64.van Hoogstraten HJ, Wolfhagen FH, van de Meeberg PC, Kuiper H, Nix GA, Becx MC, Hoek AC, van Houte DP, Rijk MC, Salemans JM, et al. Ursodeoxycholic acid therapy for primary sclerosing cholangitis: results of a 2-year randomized controlled trial to evaluate single versus multiple daily doses. J Hepatol. 1998;29:417–423. doi: 10.1016/s0168-8278(98)80059-7. [DOI] [PubMed] [Google Scholar]
- 65.Harnois DM, Angulo P, Jorgensen RA, Larusso NF, Lindor KD. High-dose ursodeoxycholic acid as a therapy for patients with primary sclerosing cholangitis. Am J Gastroenterol. 2001;96:1558–1562. doi: 10.1111/j.1572-0241.2001.03777.x. [DOI] [PubMed] [Google Scholar]
- 66.Mitchell SA, Bansi DS, Hunt N, Von Bergmann K, Fleming KA, Chapman RW. A preliminary trial of high-dose ursodeoxycholic acid in primary sclerosing cholangitis. Gastroenterology. 2001;121:900–907. doi: 10.1053/gast.2001.27965. [DOI] [PubMed] [Google Scholar]
- 67.Cangemi JR, Wiesner RH, Beaver SJ, Ludwig J, MacCarty RL, Dozois RR, Zinsmeister AR, LaRusso NF. Effect of proctocolectomy for chronic ulcerative colitis on the natural history of primary sclerosing cholangitis. Gastroenterology. 1989;96:790–794. [PubMed] [Google Scholar]
- 68.Gavaler JS, Delemos B, Belle SH, Heyl AE, Tarter RE, Starzl TE, Gavaler C, van Thiel DH. Ulcerative colitis disease activity as subjectively assessed by patient-completed questionnaires following orthotopic liver transplantation for sclerosing cholangitis. Dig Dis Sci. 1991;36:321–328. doi: 10.1007/BF01318204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Carr LJ, Harrison LM, Evans AL, Stephens JA. Patterns of central motor reorganization in hemiplegic cerebral palsy. Brain. 1993;116:1223–1247. doi: 10.1093/brain/116.5.1223. [DOI] [PubMed] [Google Scholar]
- 70.Papatheodoridis GV, Hamilton M, Mistry PK, Davidson B, Rolles K, Burroughs AK. Ulcerative colitis has an aggressive course after orthotopic liver transplantation for primary sclerosing cholangitis. Gut. 1998;43:639–644. doi: 10.1136/gut.43.5.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dvorchik I, Subotin M, Demetris AJ, Fung JJ, Starzl TE, Wieand S, Abu-Elmagd KM. Effect of liver transplantation on inflammatory bowel disease in patients with primary sclerosing cholangitis. Hepatology. 2002;35:380–384. doi: 10.1053/jhep.2002.30695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Miki C, Harrison JD, Gunson BK, Buckels JA, McMaster P, Mayer AD. Inflammatory bowel disease in primary sclerosing cholangitis: an analysis of patients undergoing liver transplantation. Br J Surg. 1995;82:1114–1117. doi: 10.1002/bjs.1800820836. [DOI] [PubMed] [Google Scholar]
- 73.MacLean AR, Lilly L, Cohen Z, O’Connor B, McLeod RS. Outcome of patients undergoing liver transplantation for primary sclerosing cholangitis. Dis Colon Rectum. 2003;46:1124–1128. doi: 10.1007/s10350-004-7291-9. [DOI] [PubMed] [Google Scholar]
- 74.Narumi S, Roberts JP, Emond JC, Lake J, Ascher NL. Liver transplantation for sclerosing cholangitis. Hepatology. 1995;22:451–457. [PubMed] [Google Scholar]
- 75.Bleday R, Lee E, Jessurun J, Heine J, Wong WD. Increased risk of early colorectal neoplasms after hepatic transplant in patients with inflammatory bowel disease. Dis Colon Rectum. 1993;36:908–912. doi: 10.1007/BF02050624. [DOI] [PubMed] [Google Scholar]
- 76.Vera A, Gunson BK, Ussatoff V, Nightingale P, Candinas D, Radley S, Mayer AD, Buckels JA, McMaster P, Neuberger J, et al. Colorectal cancer in patients with inflammatory bowel disease after liver transplantation for primary sclerosing cholangitis. Transplantation. 2003;75:1983–1988. doi: 10.1097/01.TP.0000058744.34965.38. [DOI] [PubMed] [Google Scholar]
- 77.Ludwig J, Barham SS, LaRusso NF, Elveback LR, Wiesner RH, McCall JT. Morphologic features of chronic hepatitis associated with primary sclerosing cholangitis and chronic ulcerative colitis. Hepatology. 1981;1:632–640. doi: 10.1002/hep.1840010612. [DOI] [PubMed] [Google Scholar]
- 78.Wee A, Ludwig J. Pericholangitis in chronic ulcerative colitis: primary sclerosing cholangitis of the small bile ducts? Ann Intern Med. 1985;102:581–587. doi: 10.7326/0003-4819-102-5-581. [DOI] [PubMed] [Google Scholar]
- 79.Broome U, Glaumann H, Lindstom E, Loof L, Almer S, Prytz H, Sandberg-Gertzen H, Lindgren S, Fork FT, Jarnerot G, et al. Natural history and outcome in 32 Swedish patients with small duct primary sclerosing cholangitis (PSC) J Hepatol. 2002;36:586–589. doi: 10.1016/s0168-8278(02)00036-3. [DOI] [PubMed] [Google Scholar]
- 80.Angulo P, Maor-Kendler Y, Lindor KD. Small-duct primary sclerosing cholangitis: a long-term follow-up study. Hepatology. 2002;35:1494–1500. doi: 10.1053/jhep.2002.33202. [DOI] [PubMed] [Google Scholar]
- 81.Bjornsson E, Boberg KM, Cullen S, Fleming K, Clausen OP, Fausa O, Schrumpf E, Chapman RW. Patients with small duct primary sclerosing cholangitis have a favourable long term prognosis. Gut. 2002;51:731–735. doi: 10.1136/gut.51.5.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Perdigoto R, Carpenter HA, Czaja AJ. Frequency and significance of chronic ulcerative colitis in severe corticosteroid-treated autoimmune hepatitis. J Hepatol. 1992;14:325–331. doi: 10.1016/0168-8278(92)90178-r. [DOI] [PubMed] [Google Scholar]
- 83.el-Shabrawi M, Wilkinson ML, Portmann B, Mieli-Vergani G, Chong SK, Williams R, Mowat AP. Primary sclerosing cholangitis in childhood. Gastroenterology. 1987;92:1226–1235. doi: 10.1016/s0016-5085(87)91082-1. [DOI] [PubMed] [Google Scholar]
- 84.Gohlke F, Lohse AW, Dienes HP, Lohr H, Marker-Hermann E, Gerken G, Meyer zum Buschenfelde KH. Evidence for an overlap syndrome of autoimmune hepatitis and primary sclerosing cholangitis. J Hepatol. 1996;24:699–705. doi: 10.1016/s0168-8278(96)80266-2. [DOI] [PubMed] [Google Scholar]
- 85.McNair AN, Moloney M, Portmann BC, Williams R, McFarlane IG. Autoimmune hepatitis overlapping with primary sclerosing cholangitis in five cases. Am J Gastroenterol. 1998;93:777–784. doi: 10.1111/j.1572-0241.1998.224_a.x. [DOI] [PubMed] [Google Scholar]
- 86.Gregorio GV, Portmann B, Karani J, Harrison P, Donaldson PT, Vergani D, Mieli-Vergani G. Autoimmune hepatitis/sclerosing cholangitis overlap syndrome in childhood: a 16-year prospective study. Hepatology. 2001;33:544–553. doi: 10.1053/jhep.2001.22131. [DOI] [PubMed] [Google Scholar]
- 87.Boberg KM, Fausa O, Haaland T, Holter E, Mellbye OJ, Spurkland A, Schrumpf E. Features of autoimmune hepatitis in primary sclerosing cholangitis: an evaluation of 114 primary sclerosing cholangitis patients according to a scoring system for the diagnosis of autoimmune hepatitis. Hepatology. 1996;23:1369–1376. doi: 10.1002/hep.510230612. [DOI] [PubMed] [Google Scholar]
- 88.van Buuren HR, van Hoogstraten HJE, Terkivatan T, Schalm SW, Vleggaar FP. High prevalence of autoimmune hepatitis among patients with primary sclerosing cholangitis. J Hepatol. 2000;33:543–548. doi: 10.1034/j.1600-0641.2000.033004543.x. [DOI] [PubMed] [Google Scholar]
- 89.Floreani A, Rizzotto ER, Ferrara F, Carderi I, Caroli D, Blasone L, Baldo V. Clinical course and outcome of autoimmune hepatitis/primary sclerosing cholangitis overlap syndrome. Am J Gastroenterol. 2005;100:1516–1522. doi: 10.1111/j.1572-0241.2005.41841.x. [DOI] [PubMed] [Google Scholar]
- 90.Czaja AJ. The variant forms of autoimmune hepatitis. Ann Intern Med. 1996;125:588–598. doi: 10.7326/0003-4819-125-7-199610010-00009. [DOI] [PubMed] [Google Scholar]
- 91.Czaja AJ, Carpenter HA, Santrach PJ, Moore SB. Autoimmune cholangitis within the spectrum of autoimmune liver disease. Hepatology. 2000;31:1231–1238. doi: 10.1053/jhep.2000.7878. [DOI] [PubMed] [Google Scholar]
- 92.Kaya M, Angulo P, Lindor KD. Overlap of autoimmune hepatitis and primary sclerosing cholangitis: an evaluation of a modified scoring system. J Hepatol. 2000;33:537–542. doi: 10.1034/j.1600-0641.2000.033004537.x. [DOI] [PubMed] [Google Scholar]
- 93.Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, Chapman RW, Cooksley WG, Czaja AJ, Desmet VJ, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;31:929–938. doi: 10.1016/s0168-8278(99)80297-9. [DOI] [PubMed] [Google Scholar]


