Abstract
Prostanoid metabolites are key mediators in inflammatory responses, and accumulating evidence suggests that mesenchymal stem cells (MSCs) can be recruited to injured or inflamed tissues. In the present study, we investigated whether prostanoid metabolites can regulate migration, proliferation, and differentiation potentials of MSCs. We demonstrated herein that the stable thromboxane A2 (TxA2) mimetic U46619 strongly stimulated migration and proliferation of human adipose tissue-derived MSCs (hADSCs). Furthermore, U46619 treatment increased expression of α-smooth muscle actin (α-SMA), a smooth muscle marker, in hADSCs, suggesting differentiation of hADSCs into smooth muscle-like cells. U46619 activated ERK and p38 MAPK, and pretreatment of the cells with the MEK inhibitor U0126 or the p38 MAPK inhibitor SB202190 abrogated the U46619-induced migration, proliferation, and α-SMA expression. These results suggest that TxA2 plays a key role in the migration, proliferation, and differentiation of hADSCs into smooth muscle-like cells through signaling mechanisms involving ERK and p38 MAPK.
Keywords: cell movement; cell proliferation; 15-hydroxy-11α, 9α-(epoxymethano)prosta-5, 13-dienoic acid; mesenchymal stem cells; mitogen-activated protein kinase 1; mitogen-activated protein kinase 14; thromboxane A2
Introduction
Mesenchymal stem cells or multipotent stromal cells (MSCs) can be isolated from a variety of tissues, including bone marrow and adipose tissues, and they possess self-renewal capacity, long-term viability, and differentiation potential toward diverse cell types, such as adipogenic, osteogenic, chondrogenic, and myogenic lineages (Prockop, 1997; Pittenger et al., 1999; Short et al., 2003; Barry and Murphy, 2004). In addition to their stem cell-like properties, MSCs exhibit homing ability to injured and inflamed sites in animal models of myocardial infarction and cerebral ischemia (Chamberlain et al., 2007). Transplanted MSCs have been reported to differentiate into smooth muscle cells (SMCs) in vivo and contribute to the remodeling of vasculature (Davani et al., 2003; Gojo et al., 2003; Yoon et al., 2005). We have previously demonstrated that lysophospholipids, such as sphingosylphosphorylcholine and lysophosphatidic acid, increased α-smooth muscle actin (α-SMA) expression in human adipose tissue-derived MSCs (hADSCs) (Jeon et al., 2006, 2008), suggesting a potential role of MSCs as progenitor cells for SMCs.
Prostanoids, including prostaglandin D2, prostaglandin E2, prostaglandin F2α, prostaglandin I2, and thromboxane A2 (TxA2), are produced from arachidonic acid by cyclooxygenase enzymes (Tilley et al., 2001). TxA2, a major prostanoid metabolite of arachidonic acid, is produced through isomerization of prostaglandin H2 by TxA2 synthase, predominantly in platelets and in response to a variety of physiological and pathological stimuli (Halushka et al., 1989; Dogne et al., 2005). TxA2 mediates a broad range of cellular responses, including cell proliferation, migration, platelet aggregation, and smooth muscle contraction (Bos et al., 2004; Huang et al., 2004b), and it plays a pivotal role in atherosclerotic vascular diseases, myocardial infarction, and bronchial asthma (Negishi et al., 1995). Its actions are primarily mediated by the TP receptor (TxA2 receptor), a G-protein-coupled receptor that triggers activation of MAPKs, including ERK and p38 MAPK (Bos et al., 2004; Huang et al., 2004b). However, functional involvement of prostanoid metabolites on migration, proliferation, and smooth muscle differentiation of hADSCs has not been clarified.
In the present study, we sought to elucidate the role of TxA2 and other prostanoids in the migration, proliferation, and smooth muscle differentiation of hADSCs. We demonstrate for the first time that TxA2 stimulates migration, proliferation, and α-SMA expression in hADSCs through molecular mechanisms involving ERK and p38 MAPK.
Results
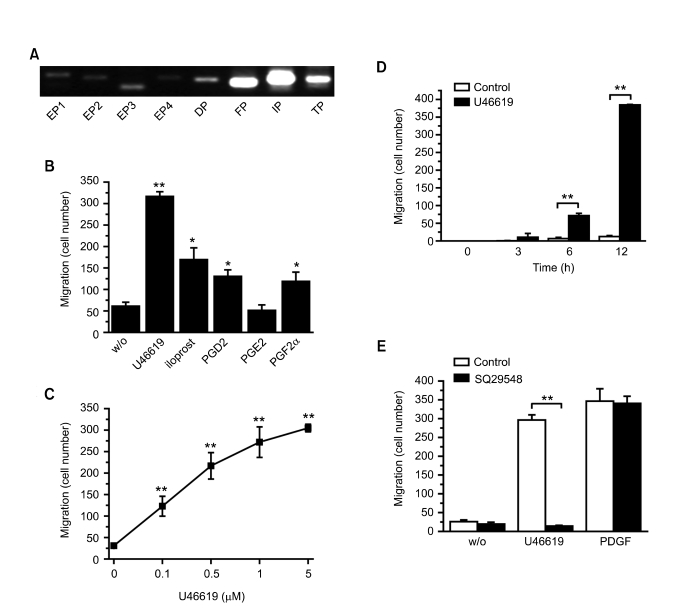
U46619 stimulated migration of hADSCs through a TP receptor-dependent mechanism
In order to determine whether hADSCs express prostanoid receptors, we extracted total RNAs from hADSCs and performed RT-PCR with primers specific to each prostanoid receptor. As shown in Figure 1A, three prostanoid receptors, including FP, IP, and TP, were highly expressed in hADSCs. Compared to the expression levels of these prostanoid receptors, however, the DP and the EP receptors (EP1, EP2, EP3, and EP4) were expressed at relatively low levels. To explore the effects of prostanoid metabolites on hADSC migration, we measured the migration of the hADSCs toward prostanoid metabolites by using a Boyden apparatus. As shown in Figure 1B, the stable TxA2 analogue U46619 greatly stimulated hADSC migration. Iloprost (a stable analog of prostacyclin, an IP receptor agonist), prostaglandin D2 (a DP receptor agonist), and prostaglandin F2α (a FP receptor agonist) also increased migration of hADSCs, but their effects were less potent than those of U46619. In contrast, prostaglandin E2 (an EP receptor agonist) had no significant impact on hADSC migration. U46619 dose-dependently stimulated hADSC migration with a maximal stimulation at 5 µM (Figure 1C), and the U46619-induced migration greatly increased after a 12 h exposure (Figure 1D). These results indicate that prostanoid metabolites derived from arachidonic acid stimulate migration of hADSCs, and that among these metabolites, TxA2 is the most potent in stimulating hADSC migration.
Figure 1.
Effects of U44619 and prostanoid metabolites on the migration of hADSCs. (A) The mRNA levels of prostanoid receptors (EP1, EP2, EP3, EP4, DP, FP, IP, TP) in hADSCs were determined by RT-PCR analysis. Representative data from three independent experiments are shown. (B) Serum-free media containing 5 µM U46619, iloprost, PGF2α, PGD2, PGE2, or LTB4 were placed in the lower chambers of the Boyden apparatus, and the numbers of migratory hADSCs were determined after 12 h. (C) Indicated concentrations of U46619 were placed in the lower chambers, and the numbers of migratory hADSCs were determined after 12 h. (D) Serum-free media containing vehicles or 5 µM U46619 were placed in the lower chambers, and the number of migrated hADSCs were determined after the indicated time periods. (E) Serum-free media containing 5 µM U46619, 10 ng/ml PDGF-BB, and/or 10 µM SQ29548 were placed into the lower chambers, and the numbers of migrating hADSCs were determined after 12 h. Data represent mean ± SD (n = 4). *, P < 0.05; **, P < 0.01 versus control.
In order to clarify whether the TP receptor mediated the U46619-induced migration, we examined the effects of SQ29548, a TP receptorspecific antagonist, on the U46619-induced migration of hADSCs. As shown in Figure 1E, pretreatment of hADSCs with SQ29548 completely abrogated the migration of the cells stimulated by U46619, in contrast to the result that SQ29548 did not significantly impact PDGF-induced migration of hADSCs, suggesting that the TP receptor plays a specific role in U46619-induced migration of hADSC.
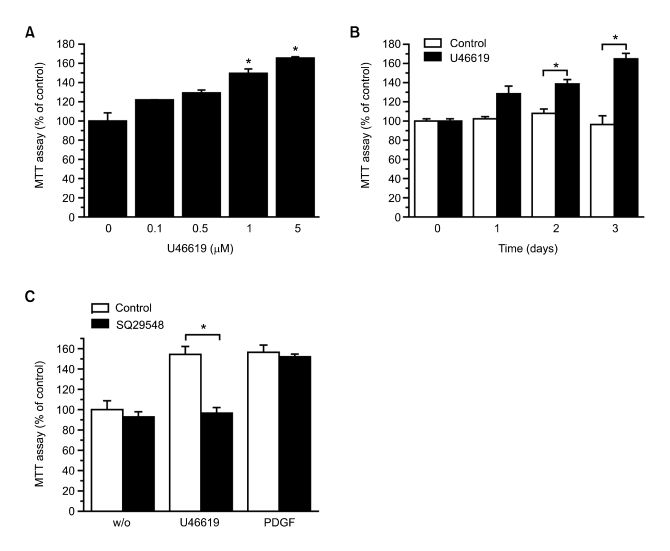
Activation of TP receptor induced proliferation of hADSCs
To investigate whether TxA2 affected the proliferation of hADSCs, we examined the effect of U46619 on the proliferation of hADSCs using an MTT assay. U46619 treatment markedly stimulated hADSC proliferation in a dose-dependent (Figure 2A) and time-dependent (Figure 2B) manner. Pretreating the cells with SQ29548 completely abrogated the proliferation of hADSCs stimulated by U46619 but not PDGF-BB (Figure 2C), suggesting that TxA2 stimulated not only migration but also proliferation of hADSCs through TP receptor-dependent mechanism.
Figure 2.
Effect of U46619 on proliferation of hADSCs. (A) hADSCs were treated with the indicated concentrations of U46619 for three days. (B) hADSCs were exposed to vehicles or 5 µM U46619 for the indicated time periods. (C) hADSCs were treated with 5 µM U46619 or 10 ng/ml PDGF-BB in the absence or presence of 10 µM SQ29548 for three days. Proliferation was determined with an MTT assay. Data represent means ± SD (n = 4). *indicates P < 0.05.
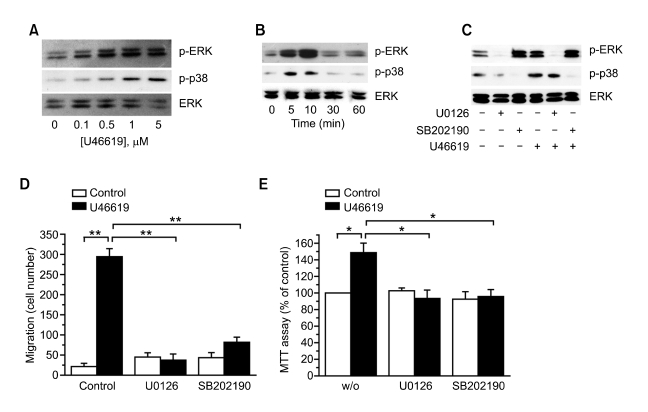
U46619 induced migration and proliferation of hADSCs through ERK- and p38 MAPK-dependent pathways
U46619 reportedly activates MAPKs, including ERK and p38 MAPK (Bos et al., 2004; Huang et al., 2004b). To explore whether U46619 activated ERK and p38 MAPK as part of the mechanism underlying hADSC stimulation, we examined the effects of U46619 on the phosphorylation levels of ERK and p38 MAPK in these cells. As shown in Figure 3A, U46619 treatment dose-dependently increased phosphorylation levels of ERK and p38 MAPK. The phosphorylation levels of ERK and p38 MAPK observed after 5 min of U46619 stimulation (Figure 3B). Moreover, pretreating the cells with the MEK1/2 inhibitor U0126 or the p38 MAPK inhibitor SB202190 specifically inhibited the U46619-induced phosphorylation of ERK or p38 MAPK, respectively (Figure 3C). Pretreating the cells with either U0126 or SB202190 completely attenuated U46619-induced migration and proliferation of hADSCs (Figure 3D and E), suggesting that both ERK and p38 MAPK are involved in the U46619-stimulated migration and proliferation of hADSCs.
Figure 3.
Roles of ERK and p38 MAPK in the U46619-induced migration and proliferation of hADSCs. (A) hADSCs were treated with the indicated concentrations of U46619 for 10 min. (B) hADSCs were treated with 5 µM U46619 for the indicated time periods. (C) hADSCs were pretreated with vehicles, 10 µM U0126, or 10 µM SB202190 for 15 min and treated with vehicles or 5 µM U46619 for 10 min. Phosphorylation levels of ERK and p38 MAPK and the expression levels of total ERK were determined by Western blotting. (D) Serum-free media containing vehicles or 5 µM U46619 in the absence or presence of 10 µM U0126 or 10 µM SB202190 were placed into the lower chambers, and the numbers of migrating hADSCs were determined after 12 h. (E) Serum-starved hADSCs were treated with 5 µM U46619 or vehicles (control) in the absence or presence of 10 µM U0126 or 10 µM SB202190 for three days, and proliferation was determined with an MTT assay. Data represent means ± SD (n = 4). *, P < 0.05; **, P < 0.01.
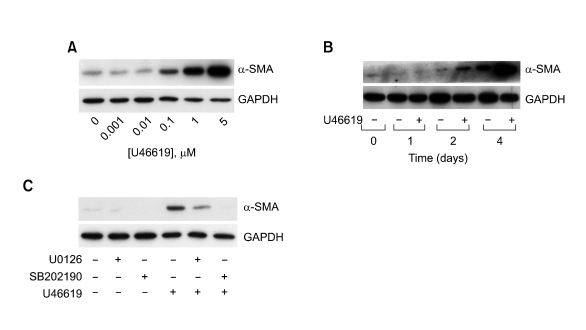
U46619 induced differentiation of hADSCs into smooth muscle-like cells through ERK- and p38 MAPK-dependent pathways
To explore whether TxA2 can induce differentiation of hADSCs to SMCs, hADSCs were treated with indicated concentrations of U46619 for four days, and then the expression levels of α-SMA, a SMC marker, were determined by Western blotting. As shown in Figure 4A, U46619 dose-dependently increased the expression of α-SMA. The expression of α-SMA was drastically increased after exposure of the cells to 5 µM U46619 for four days (Figure 4B), suggesting U46619-induced differentiation of hADSCs to smooth muscle-like cells. The U46619-induced α-SMA expression was markedly abrogated by pretreating the cells with U0126 or SB202190 (Figure 4C), suggesting that ERK and p38 MAPK are involved in the U46619-stimulated differentiation of hADSCs into smooth muscle-like cells.
Figure 4.
Effect of U46619 on the expression levels of α-SMA in hADSCs. (A) hADSCs were treated with indicated concentrations of U46619 for four days. (B) hADSCs were treated with vehicle or 1 µM U46619 for indicated time periods. (C) hADSCs were treated with 5 µM U46619 or vehicle in the absence or presence of 10 µM U0126 or 10 µM SB202190 for four days. The expression levels of α-SMA were determined by Western blotting with anti-α-SMA antibody. To ensure equal loading in each lane, the levels of GAPDH were determined by Western blotting. Representatives of three independent experiments are shown.
Discussion
In the present study, we demonstrated for the first time that TxA2-induced activation of the TP receptor ultimately led to migration, proliferation, and smooth muscle differentiation of hADSCs through mechanisms involving ERK and p38 MAPK. In support of these results, ERK and p38 MAPK reportedly play a key role in the migration of diverse cell types (Huang et al., 2004a). Overexpression of a constitutively-active MEK1 mutant promoted the migration of FG carcinoma cells, whereas depletion of endogenous ERK by antisense oligonucleotides inhibited cell migration (Klemke et al., 1997). In coronary artery smooth muscle cells, U46619 stimulated proliferation through an ERK-dependent mechanism (Morinelli et al., 1994). Furthermore, p38 MAPK is involved in smooth muscle cell migration induced by PDGF, TGF-β, and IL-1β (Hedges et al., 1999), as well as PDGF-induced migration of endothelial cells (Matsumoto et al., 1999). Furthermore, we have reported that sphingosylphosphorylcholine and lysophosphatidic acid induced α-SMA expression in hADSCs through ERK-dependent mechanism (Jeon et al., 2006, 2008). Taken together, these results support the notion that ERK and p38 MAPK play a central part in the TxA2-induced migration, proliferation, and smooth muscle differentiation of hADSCs.
TxA2 is produced mainly in platelets, but it can also be synthesized by other cell types, including monocytes and vascular smooth muscle (Tilley et al., 2001; Reiss and Edelman, 2006). While the levels of prostanoids like TxA2 are generally very low in uninflamed tissues, they markedly increase as a part of the inflammatory response in injured tissues (Tilley et al., 2001). The current study provides an unprecedented demonstration that TxA2 potently activates migration and proliferation of MSCs and stimulates differentiation of the cells into smooth muscle-like cells. Taken together with the previous reports suggesting that MSCs can be recruited into injured and inflamed tissues (Wang et al., 2002; Chamberlain et al., 2007; Fox et al., 2007; Ponte et al., 2007), the results herein suggest that TxA2 may participate in MSC-mediated tissue repair by stimulating homing of MSCs into injured tissues and inducing proliferation and differentiation of MSCs into smooth muscle-like cells. The implication of TxA2-induced functional modulation of MSCs in the regeneration of injured tissues should be determined further.
Methods
Materials
PBS, α-minimum essential medium, trypsin, and FBS were purchased from Invitrogen (Carlsbad, CA). U46619, iloprost, prostaglandin F2α, prostaglandin D2, prostaglandin E2, and SQ29548 were purchased from Cayman Chemicals (Ann Arbor, MI). Human platelet-derived growth factor-BB (PDGF-BB) was purchased from R&D Systems, Inc. (Minneapolis, MN). U0126, and SB202190 were purchased from EMD Biosciences (San Diego, CA). Anti-phospho-ERK, anti-ERK, and anti-phospho-p38 MAPK were from Cell Signaling Technology (Beverly, MA). Anti-GAPDH antibody was purchased from Chemicon International Inc. (Temecula, CA). HRP-labeled secondary antibodies and the enhanced chemiluminescence Western blotting system were from Amersham Biosciences (Pittsburgh, PA). MTT, anti-α-SMA antibody, and all other reagents were obtained from Sigma-Aldrich (St. Louis, MO).
Cell culture
Subcutaneous adipose tissue was obtained from elective surgeries with the patients' consent, as approved by Institution Review Board of Busan National University Hospital. To isolate hADSCs, adipose tissues were washed at least three times with sterile PBS and treated with an equal volume of collagenase type I solution (0.1% collagenase type I and 1% BSA, buffered with Hank's balanced salt solution) for 60 min at 37℃ with intermittent shaking. Floating adipocytes were separated from the stromal-vascular fraction by centrifugation at 300 g for 5 min. The cell pellet was resuspended in α-minimum essential medium supplemented with 10% FBS, 100 U/ml penicillin, and 100 µg/ml streptomycin, and cells were plated in tissue culture dishes at 3,500 cells/cm2. Primary hADSCs were cultured for 4-5 days until they reached confluence, at which point they were defined as passage "0". For experiments, hADSCs were used at passage 3-10.
Cell migration assay
hADSC migration was assayed using a Boyden chamber apparatus, as previously described (Law et al., 1996). Briefly, hADSCs were harvested with 0.05% trypsin containing 0.02% EDTA, washed once, and suspended in α-minimum essential medium at a concentration of 2 × 105 cells/ml. Membrane filters (8-µm pore size) in disposable 96-well chemotaxis chambers (Neuro Probe, Inc.; Gaithersburg, MD) were precoated overnight with 20 µg/ml rat-tail collagen at 4℃. Aliquots (100 µl per well) of the hADSC suspension were loaded into the upper chambers, and test reagents were placed in the lower chamber. After incubation for the indicated time periods, the filters were disassembled, and the upper surface of each filter was scraped free of cells by wiping it with a cotton swab. The numbers of cells that had migrated to the lower surfaces of each filter were determined by microscopically counting the cells in four places (× 100 magnification) after staining with hematoxylin and eosin.
MTT assay
Proliferation was determined with a colorimetric MTT assay: MTT is metabolized by NAD-dependent dehydrogenase to form a colored reaction product (formazan), and the amount of dye formed directly correlates with the number of cells. To determine cell numbers, hADSCs were seeded in a 24-well culture plate at a density of 2 × 104 cells/well, cultured for 48 h in normal growth medium, serum-starved for 24 h, and treated with various reagents (or a vehicle control) for the indicated times. The cells were washed twice with PBS and incubated with 100 µl of MTT (0.5 mg/ml) for 2 h at 37℃. The formazan granules generated by the cells were dissolved in 100 µl of DMSO, and the absorbance of the solution at 562 nm was determined by using a PowerWavex microplate spectrophotometer (Bio-Tek Instruments, Inc.; Winooski, VT) after dilution to a linear range.
Western blot analysis
Confluent, serum-starved hADSCs were treated with the indicated conditions, washed with ice-cold PBS, and lysed in lysis buffer (20 mM Tris-HCl, 1 mM ethylene glycol tetraacetic acid, 1 mM EDTA, 10 mM NaCl, 0.1 mM PMSF, 1 mM Na3VO4, 30 mM sodium pyrophosphate, 25 mM β-glycerophosphate, 1% Triton X-100, pH 7.4). Lysates were resolved by SDS-PAGE, transferred onto nitrocellulose membranes, and stained with 0.1% Ponceau S solution. After blocking with 5% nonfat milk, the membranes were immunoblotted with appropriate primary antibodies, and the bound antibodies were visualized with HRP-conjugated secondary antibodies and an enhanced chemiluminescence system.
RT-PCR analysis
Cells were treated as indicated, and total cellular RNA was extracted by the Trizol method (Invitrogen). For RT-PCR analysis, 2 µg aliquots of RNA were subjected to cDNA synthesis with 200 U of M-MLV reverse transcriptase (Invitrogen) and 0.5 µg of oligo (dT) 15 primer (Promega; Madison, WI). The cDNA in 2 µl of the reaction mixture was amplified with 0.5 U of GoTaq DNA polymerase (Promega) and 10 pmol each of sense and antisense primers, as follows: EP1 5'-GCTATGAGCTGCAGTACCC-3', 5'-CACGACACCACCATGATAC-3'; EP2 5'-CTCCTGAGAAAGACAGTGCT-3', 5'-CTGATATTCGCAAAGTCCTC-3'; EP3 5'-AGCAGAAAGAATGCAACTTC-3', 5'-AGCTGGATGCATAGTTGTTT-3'; EP4 5'-CTCCTGAGAAAGACAGTGCT-3', 5'-CTGATATTCGCAAAGTCCTC-3'; DP 5'-TTCTTCATGTCCTTCTTTGG-3', 5'-GCTGGAGTAGAGCACAGAGT-3'; FP 5'-CTTCATGACAGTGGGAATCT-3', 5'-CCAAAAATACTGCAAAGGAC-3'; IP 5'-GTGCAGGAACCTCACCTAC-3', 5'-AAAGAGGATGAGCATGGAC-3'; TP 5'-AACATTACCCTGGAGGAGAG-3', 5'-CGAAGAAGATCATGACGAC-3'. The thermal cycle profile was as follows: denaturation at 95℃ for 30 s, annealing at 47-55℃ for 45 s (depending on the primers used), and extension at 72℃ for 45 s. Each PCR was carried out for 30 cycles, and PCR products were size-fractionated on 1.2% ethidium bromide/agarose gels and quantified under UV transillumination.
Statistical analysis
The results of multiple observations are presented as mean ± SD. For multivariate data analysis, group differences were assessed with two-way ANOVA, followed by post hoc comparisons tested with Scheffe's method.
Acknowledgements
This study was financially supported by Pusan National University in program Post-Doc. 2006 and the Korea Research Foundation grants (KRF-2007-521-C00225).
Abbreviations
- α-SMA
α-smooth muscle actin
- hADSCs
human adipose tissue-derived mesenchymal stem cells
- MSCs
mesenchymal stem cells
- SMCs
smooth muscle cells
- TxA2
thromboxane A2
References
- 1.Barry FP, Murphy JM. Mesenchymal stem cells: clinical applications and biological characterization. Int J Biochem Cell Biol. 2004;36:568–584. doi: 10.1016/j.biocel.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Bos CL, Richel DJ, Ritsema T, Peppelenbosch MP, Versteeg HH. Prostanoids and prostanoid receptors in signal transduction. Int J Biochem Cell Biol. 2004;36:1187–1205. doi: 10.1016/j.biocel.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 3.Chamberlain G, Fox J, Ashton B, Middleton J. Concise review: mesenchymal stem cells: their phenotype, differentiation capacity, immunological features, and potential for homing. Stem Cells. 2007;25:2739–2749. doi: 10.1634/stemcells.2007-0197. [DOI] [PubMed] [Google Scholar]
- 4.Davani S, Marandin A, Mersin N, Royer B, Kantelip B, Herve P, Etievent JP, Kantelip JP. Mesenchymal progenitor cells differentiate into an endothelial phenotype, enhance vascular density, and improve heart function in a rat cellular cardiomyoplasty model. Circulation. 2003;108(Suppl 1):II253–II258. doi: 10.1161/01.cir.0000089186.09692.fa. [DOI] [PubMed] [Google Scholar]
- 5.Dogne JM, Hanson J, Pratico D. Thromboxane, prostacyclin and isoprostanes: therapeutic targets in atherogenesis. Trends Pharmacol Sci. 2005;26:639–644. doi: 10.1016/j.tips.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Fox JM, Chamberlain G, Ashton BA, Middleton J. Recent advances into the understanding of mesenchymal stem cell trafficking. Br J Haematol. 2007;137:491–502. doi: 10.1111/j.1365-2141.2007.06610.x. [DOI] [PubMed] [Google Scholar]
- 7.Gojo S, Gojo N, Takeda Y, Mori T, Abe H, Kyo S, Hata J, Umezawa A. In vivo cardiovasculogenesis by direct injection of isolated adult mesenchymal stem cells. Exp Cell Res. 2003;288:51–59. doi: 10.1016/s0014-4827(03)00132-0. [DOI] [PubMed] [Google Scholar]
- 8.Halushka PV, Mais DE, Mayeux PR, Morinelli TA. Thromboxane, prostaglandin and leukotriene receptors. Annu Rev Pharmacol Toxicol. 1989;29:213–239. doi: 10.1146/annurev.pa.29.040189.001241. [DOI] [PubMed] [Google Scholar]
- 9.Hedges JC, Dechert MA, Yamboliev IA, Martin JL, Hickey E, Weber LA, Gerthoffer WT. A role for p38(MAPK)/HSP27 pathway in smooth muscle cell migration. J Biol Chem. 1999;274:24211–24219. doi: 10.1074/jbc.274.34.24211. [DOI] [PubMed] [Google Scholar]
- 10.Huang C, Jacobson K, Schaller MD. MAP kinases and cell migration. J Cell Sci. 2004a;117:4619–4628. doi: 10.1242/jcs.01481. [DOI] [PubMed] [Google Scholar]
- 11.Huang JS, Ramamurthy SK, Lin X, Le Breton GC. Cell signalling through thromboxane A2 receptors. Cell Signal. 2004b;16:521–533. doi: 10.1016/j.cellsig.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Jeon ES, Moon HJ, Lee MJ, Song HY, Kim YM, Bae YC, Jung JS, Kim JH. Sphingosylphosphorylcholine induces differentiation of human mesenchymal stem cells into smooth-muscle-like cells through a TGF-{beta}-dependent mechanism. J Cell Sci. 2006;119:4994–5005. doi: 10.1242/jcs.03281. [DOI] [PubMed] [Google Scholar]
- 13.Jeon ES, Moon HJ, Lee MJ, Song HY, Kim YM, Cho M, Suh DS, Yoon MS, Chang CL, Jung JS, Kim JH. Cancer-derived lysophosphatidic acid stimulates differentiation of human mesenchymal stem cells to myofibroblast-like cells. Stem Cells. 2008;26:789–797. doi: 10.1634/stemcells.2007-0742. [DOI] [PubMed] [Google Scholar]
- 14.Klemke RL, Cai S, Giannini AL, Gallagher PJ, de Lanerolle P, Cheresh DA. Regulation of cell motility by mitogen-activated protein kinase. J Cell Biol. 1997;137:481–492. doi: 10.1083/jcb.137.2.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Law RE, Meehan WP, Xi XP, Graf K, Wuthrich DA, Coats W, Faxon D, Hsueh WA. Troglitazone inhibits vascular smooth muscle cell growth and intimal hyperplasia. J Clin Invest. 1996;98:1897–1905. doi: 10.1172/JCI118991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matsumoto T, Yokote K, Tamura K, Takemoto M, Ueno H, Saito Y, Mori S. Platelet-derived growth factor activates p38 mitogen-activated protein kinase through a Ras-dependent pathway that is important for actin reorganization and cell migration. J Biol Chem. 1999;274:13954–13960. doi: 10.1074/jbc.274.20.13954. [DOI] [PubMed] [Google Scholar]
- 17.Morinelli TA, Zhang LM, Newman WH, Meier KE. Thromboxane A2/prostaglandin H2-stimulated mitogenesis of coronary artery smooth muscle cells involves activation of mitogen-activated protein kinase and S6 kinase. J Biol Chem. 1994;269:5693–5698. [PubMed] [Google Scholar]
- 18.Negishi M, Sugimoto Y, Ichikawa A. Molecular mechanisms of diverse actions of prostanoid receptors. Biochim Biophys Acta. 1995;1259:109–119. doi: 10.1016/0005-2760(95)00146-4. [DOI] [PubMed] [Google Scholar]
- 19.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 20.Ponte AL, Marais E, Gallay N, Langonne A, Delorme B, Herault O, Charbord P, Domenech J. The in vitro migration capacity of human bone marrow mesenchymal stem cells: comparison of chemokine and growth factor chemotactic activities. Stem Cells. 2007;25:1737–1745. doi: 10.1634/stemcells.2007-0054. [DOI] [PubMed] [Google Scholar]
- 21.Prockop DJ. Marrow stromal cells as stem cells for nonhematopoietic tissues. Science. 1997;276:71–74. doi: 10.1126/science.276.5309.71. [DOI] [PubMed] [Google Scholar]
- 22.Reiss AB, Edelman SD. Recent insights into the role of prostanoids in atherosclerotic vascular disease. Curr Vasc Pharmacol. 2006;4:395–408. doi: 10.2174/157016106778521652. [DOI] [PubMed] [Google Scholar]
- 23.Short B, Brouard N, Occhiodoro-Scott T, Ramakrishnan A, Simmons PJ. Mesenchymal stem cells. Arch Med Res. 2003;34:565–571. doi: 10.1016/j.arcmed.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 24.Tilley SL, Coffman TM, Koller BH. Mixed messages: modulation of inflammation and immune responses by prostaglandins and thromboxanes. J Clin Invest. 2001;108:15–23. doi: 10.1172/JCI13416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang L, Li Y, Chen X, Chen J, Gautam SC, Xu Y, Chopp M. MCP-1, MIP-1, IL-8 and ischemic cerebral tissue enhance human bone marrow stromal cell migration in interface culture. Hematology. 2002;7:113–117. doi: 10.1080/10245330290028588. [DOI] [PubMed] [Google Scholar]
- 26.Yoon YS, Wecker A, Heyd L, Park JS, Tkebuchava T, Kusano K, Hanley A, Scadova H, Qin G, Cha DH, Johnson KL, Aikawa R, Asahara T, Losordo DW. Clonally expanded novel multipotent stem cells from human bone marrow regenerate myocardium after myocardial infarction. J Clin Invest. 2005;115:326–338. doi: 10.1172/JCI22326. [DOI] [PMC free article] [PubMed] [Google Scholar]