Abstract
Elevated heart rate has been proposed as an independent risk factor for cardiovascular diseases, but their interrelationships are not well understood. In this study, we performed a genome-wide linkage scan in 1,026 individuals (mean age 30.6 years, 54.5% women) from 73 extended families of Mongolia and determined quantitative trait loci that influence heart rate. The DNA samples were genotyped using deCODE 1,039 microsatellite markers for 3 cM density genome-wide linkage scan. Correlation analysis was carried out to evaluate the correlation of the covariates and the heart rate. T-tests of the heart rate were also performed on sex, smoking and alcohol intake. Consequently, this model was used in a nonparametric genome-wide linkage analysis using variance component model to create a multipoint logarithm of odds (LOD) score and a corresponding P value. In the adjusted model, the heritability of heart rate was estimated as 0.32 (P < .0001) and a maximum multipoint LOD score of 2.03 was observed in 77 cM region at chromosome 18. The second largest LOD score of 1.52 was seen on chromosome 5 at 216 cM. Genes located on the specified locations in chromosomes 5 and 18 may be involved in the regulation of heart rate.
Keywords: cardiovascular diseases, chromosome mapping, genomics, heart rate, Mongolia
Introduction
Epidemiological and clinical studies suggest that elevated heart rate is a potential risk factor for a variety of cardiovascular diseases (CVD) including atherosclerosis, coronary artery disease (CAD), myocardial infarction, arterial hypertension and heart failure (Greenland et al., 1999; Colhoun et al., 2001; King et al., 2006; Palatini et al., 2006; Brasel et al., 2007; Fox et al., 2007; Rogowski et al., 2007). The elevated heart rate is closely associated with age, high blood pressure, body mass index (BMI), smoking, alcohol consumption, high cholesterol level, and physical inactivity. But, even after adjusting for other potential risk factors, elevated heart rate remains significantly associated with CVD, mortality and all cause mortality in patients with CVD as well as general population (Kannel WB et al., 1987; Gillman et al., 1993; Palatini 1999; Kristal-Boneh et al., 2000; Fujiura et al., 2001; Kovar et al., 2004; Diaz et al., 2005; Fox et al., 2007; Reil and Bohm 2007; Theobald et al., 2007). The mechanism for elevated heart rate and its association with such diseases and death is still not well understood. A number of twin and family studies have reported that genetic factors influence the regulation of heart rate (Singh et al., 1999; Woodman et al., 2002; Wilk et al., 2002; Martin et al., 2004; Neumann et al., 2005; Laramie et al., 2006; Larson et al., 2007; Newton-Cheh et al., 2007; O'Donnell et al., 2007). Voss et al. (1996) reported that there is a genetic component in heart rate generation and heart rate variability in monozygotic and dizygotic twin pairs. Singh et al., (2002) identified significant genetic regions contributing to heart rate variability on chromosome 15 at 62 cM and chromosome 2 at 153 cM. In the recent meta-analysis of genome-wide scans for study networks that enrolled Caucasians and African-Americans, Laramie et al. (2006) concluded in the replication between various ethnic groups as well as the study networks with low heterogeneity on chromosome 5p13-14. Wilk et al. (2002) also identified that 195.06 cM region of chromosome 4 is seemingly related to the variability in resting heart rate.
Most published studies on genetic influences on the variation of heart rate focused on Caucasian and not on Asian populations. The genetic background and environmental factors to which a subject group is exposed differ in every human population. In this study, we assessed genetic components involved in heart rate variation using data from gene discovery for complex traits in isolated large families of Asians of Northeast (GENDISCAN) study. Large extended families enable the full utilization of family design for linkage study. GENDISCAN study is committed to incorporating most of methodological issues of complex diseases using genetically homogeneous population and emphasizing the quantitative phenotypes.
Materials and Methods
Subjects
One thousand and twenty six Mongolian individuals (54.5% women) from 73 extended families from Dornod, Mongolia were genotyped. Informed consents to participate in the study were obtained from all subjects. The protocol for GENDISCAN study was approved by the institutional review board (IRB) of Seoul National University of Korea (approval number, H-0307-105-002).
Heart rate and covariates
Four consecutive measurements of the heart rate and blood pressure were made on both arms of each participant while seated, employing a standard electronic sphygmomanometer. When the four blood pressure measurements differed by more than 10 mmHg, a fifth measurement was made and the lowest four were used in the analyses. The larger means of each set of measurements were accepted as heart rate and the blood pressure respectively. Measurements in children from age 10 to 16 were made using appropriate cuffs and a mercury sphygmomanometer. Data on potentially confounding factors for heart rate such as age, sex, smoking, and alcohol consumption were collected through interviews performed by trained interviewers. The standing height in centimeter (cm) and weight in kilograms (kg) were measured, and BMI was calculated in kg/m2.
Genotyping
For those who agreed to be genotyped, genomic DNA was extracted from peripheral venous blood leukocytes using standard procedure and genotyped using deCODE 1,039 microsatellite marker platform. Whole genome analyses have been performed. For 1,039 deCODE marker sets, optimized multiplex PCR reactions were set up on Zymark ALH 400, run on MJR Tetrad and pooled on Gilson Cyberlab C200 robots. The reaction volume was 5 µl, and for each PCR 20 ng of genomic DNA was amplified in the presence of 2 pmol of each primer, 0.25 U AmpliTaq Gold, 0.2 mM dNTPs and 2.5 mM MgCl2 (buffer was supplied by the manufacturer, Applera). Cycling conditions were as follows: 95℃ for 10 min, followed by 37 cycles of 94℃ for 15 s, annealing for 30 s at 55℃, and 1 min extension at 72℃. The PCR products were supplemented with the internal size standard GS500-LIZ, and the pools were separated and detected on 3730 Sequencers. Alleles were automatically called using DAC, an allele-calling program developed at deCODE genetics Inc. and the program deCODE GT was used to fractionate called genotypes, according to quality, and to edit when necessary.
Statistical analysis
Correlation analysis
We carried out a correlation analysis to evaluate the correlation of covariates (age, sex, smoking, alcohol intake, brachial systolic pressure, brachial diastolic pressure, brachial mean arterial pressure and body mass index) and heart rate, and Pearson correlation coefficients were identified. T-tests of heart rate were also performed on the three categories, which are sex, smoking and alcohol intake, by using SAS statistical software version 9.1.
Pedigree and genotype data cleaning, single- and multi-point identity by descent (IBD) calculation
For the family relationship, nonpaternity was examined using PEDCHECK. Relationships other than paternity were checked using average identity by descent (IBD)-based method by PREST. After correcting pedigree error and mendelian errors, non-mendelian errors were examined and corrected using SimWalk. After pedigree and genotype errors were corrected, IBD matrices between every relationship pair were calculated. IBD matrix for single marker was calculated by SOLAR, and multipoint IBD (MIBD) matrices were computed on every 1 cM distance using Markov chain Monte Carlo method by LOKI. We used Haldane's mapping function to convert map distances into recombination fractions.
Heritability estimation
Genetic components of selected phenotypes were estimated in terms of heritability. Narrow sense heritability, defined as the proportion of total phenotypic variation due to additive genetic effects, was calculated. Age-sex adjusted phenotype (adjusted for age, sex, age-square, product of age and sex, product of age-square and sex) was estimated by SOLAR for quantitative traits.
Multipoint variance component-based linkage analysis for heart rate
To reduce the type I error from deviated distribution, original values were normalized using Z-transformation. The genetic variance of heart rate was decomposed into specific additive genetic effects from specific markers (Quantitative trait loci, QTL) and non-QTL given by:
Ωij = Π σ2QTL + 2Φijσ2N-QTL + I e2
Where Ω is the covariance matrix of the entire family, π is a matrix of the proportions of the specific QTL that the relative pairs share as IBD, Φ is a kinship matrix, I is an identity matrix, σ2QTL is specific QTL effects of the genetic markers, σ2N-QTL is residual genetic effect, and e2 is random environmental effects and errors. The likelihood that QTL effects can be estimated were compared with the likelihood of null hypothesis that specific QTL effect equals zero. The logarithm of odds (LOD) score between likelihood of null and alternative hypothesis was used to test the significance of linkage results. The multipoint linkage analyses were performed using SOLAR. In the genome-wide scans, age, sex, age2 and the interactions between them retained in the models as covariates at P < 0.10. Because variance composition method is sensitive to outliers, multivariate residual kurtosis in each analysis retained less than 0.8 thereby avoiding type 1 error.
Results
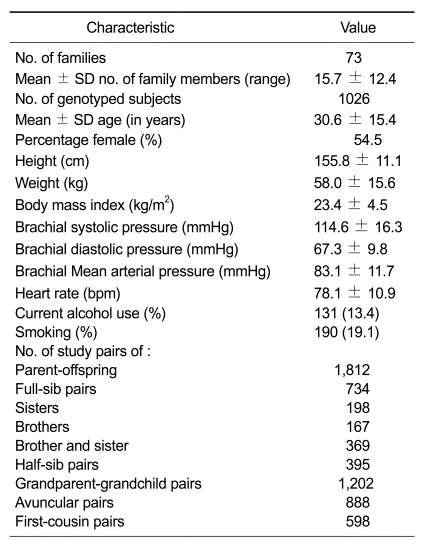
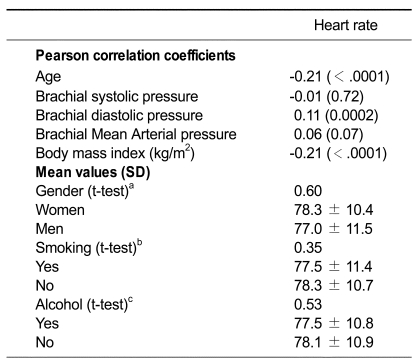
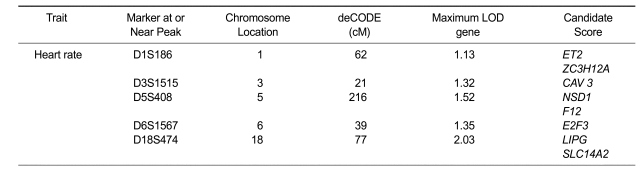
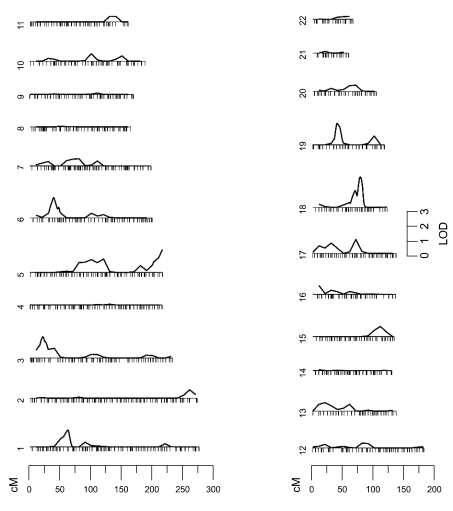
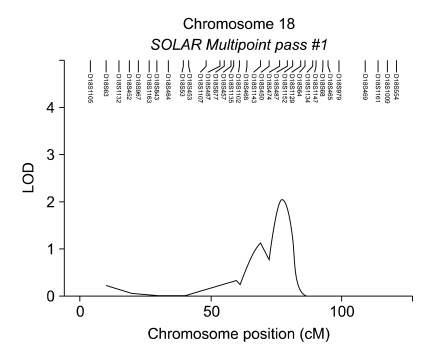
Demographic and pedigree characteristics of the data set and the covariates are presented in Table 1. The data set of examined individuals included a large number of relative pair types as we have recruited extended families. The data set included information on 2,546 pairs of first-degree relatives (1,812 parent-offspring pairs and 734 full-sib pairs), and 2,485 pairs of their second-degree relatives (395 half-sibling pairs, 1,202 grandparent-grandchild pairs). The other 888 and 598 pairs were avuncular and first-cousins, respectively. Current alcohol use and smoking was reported by 13.4% and 19.1%, of the subjects, respectively. Mean age of the subjects was 30.6 yrs. Mean resting heart rate was 78.1 and the mean number of family members was 15.7. The mean BMI was 23.4 and the mean brachial systolic, diastolic, and arterial blood pressure was 114.6, 67.3, and 83.1, respectively. Table 2 shows the relationships between baseline characteristics and heart rate. Age, brachial diastolic pressure, and BMI were significantly associated with mean heart rate. The adjusted heritability model includes age, gender, BMI, smoking and alcohol consumption. In the adjusted model, the heritability of heart rate was estimated to be 0.32 (P < .0001). In Table 3 are presented LOD scores greater than 1.0, nearest markers, chromosomal locations and candidate genes. In the adjusted model a maximum LOD score of 2.03 was seen on chromosome 18 at 77 cM. The second largest LOD score of 1.52 was seen on chromosome 5 at 216 cM. Figure 1 shows the chromosomal regions linked to heart rate genome-wide linkage analysis. As shown in Figure 2, there is suggestive evidence of linkage (LOD score = 2.03) of a quantitative trait locus (QTL) for heart rate on chromosome 18 at 77 cM.
Table 1.
Demographic and pedigree characteristics of the dataset.
Table 2.
Relationships between baseline characteristic data and heart rate.
aP values reflect test of subgroup differences (women versus men). bP value of smoking yes, no; cP value of alcohol yes, no
Table 3.
LOD scores, chromosomal locations, and nearest marker data for all LOD scores > 1.00a.
aIncludes adjustment for age, gender, BMI, smoking and alcohol.
Figure 1.
Genome-wide linkage analysis of chromosomal regions linked to heart rate.
Figure 2.
Evidence of linkage (LOD score = 2.03) of a quantitative trait locus (QTL) for heart rate on chromosomes 18 at 77 cM.
Discussion
It has long been known that heart rate is under the control of the parasympatic and sympathetic nervous system, and that heightened sympathetic tone increases the heart rate (Bonaa and Arnesen, 1992; Palatini and Julius, 1997; Rahn et al., 1999; Fujiura et al., 2001). In more recent studies, they pointed out that genetic components may play an essential role in the regulation of heart rate variability. The Framingham heart study (Singh et al., 1999) also demonstrated that genetic factors are involved in heart rate variability. The degree of heritability of heart rate was 0.32 in GENDISCAN study. This value is somewhat higher than the figure (0.21) reported for Framingham Heart Study participants (Singh et al., 1999), but is lower than the figure (0.41) reported for participants of Netherlands Twin Register (Kupper et al., 2004). All the three studies provide evidence for a strong genetic component in heart rate variability.
We showed a peak with a maximum LOD of 2.03 on chromosome 18 at 77 cM. As described by Duchesne et al. (2001), SLC14A2 (solute carrier family 14 urea transporter) gene which lies near this loci, encodes UT-A protein expressed in the heart. The expression of this protein in failing left ventricle is 1.4-4.3 fold to that in normal nonfailing ventricle. Further, LIPG (endothelial lipase precursor) gene also lies on chromosome 18 at 77cM. This gene encodes the protein that process substantial phospholipase activity and plays an important role in lipid metabolism. More recently, Shimizu et al. (2007) reported that the significant association between 584C/T SNP of LIPG gene and an acute myocardial infarction (AMI) independent of HDL-C levels in a Japanese population. It is also of interest that chromosome 5 yielded the second largest linkage peak which corresponds to its 216 cM region. An analysis of the database indicated that the chromosomal region 216 cM on chromosome 5 contains NSD1 (nuclear receptor SET domain containing gene1) gene. The protein encoded by NSD1 gene enhances transactivation of androgen receptor (AR). It has been reported that the intragenic mutation of this gene is associated with the high frequency of congenital heart defects or heart conduction (Cecconi et al., 2005). F12 (coagulation factor XII) gene also located at 216 cM on chromosome 5 encodes coagulation factor XII, which circulates in blood as a zymogen. Roldan et al., (2005) reported that the C46T polymorphism of F12 is associated with a reduction of plasma FXII levels and a development of myocardial infarction (MI), particularly in hypercholesterolemic patients. Santamaria et al. (2004) also reported that the homozygosity for the C46T polymorphism of the F12 gene is significantly associated with high risk of coronary artery disease (CAD) in the Spanish population. Moreover, the ZC3H12A (zinc finger CCCH type containing 12A) gene was located at 62cM on chromosome 1, which is an MCP1 (monocyte chemotactic protein-1) induced protein. Recent study of Zhou et al., (2006) reported that MCP-1 causes cell death of cardiomyocytes and plays an important role in the development of ischemic heart disease (IHD). Also, the ET2 (endothelin 2) gene at 62 cM on chromosome 1 was founded. Sharma et al. (1999) reported that polymorphism in the ET2 gene influences the hypertension when blood pressure is assessed as a quantitative trait. Moreover, E2F3 gene at 39 cM on chromosome 6 encodes a transcription factor of the E2F family. This family protein has an important role of controlling tumor suppressor proteins and cell cycle. The region at 21 cM on chromosome 3 includes CAV 3 gene, which encodes caveolin-3 muscle-specific protein. This finding is interesting in the background of evidence that cav-3 null mice show perivascular fibrosis, cellular infiltration in cardiac tissue and cardiac myocyte hypertrophy, which exhibits inter- and intrafamilial variations ranging from benign to malignant forms with high risk of cardiac failure and sudden cardiac death (Cribbs et al., 2001; Woodman et al., 2002; Chen et al., 2003; Ha et al., 2005).
In conclusion, we identified susceptible loci for heart rate variability in an Asian population. This study strongly indicates that heart rate is controlled by genes mapped to several loci. We believe characterization of genes that affects heart rate variability can lead to unraveling of the pathogenetic mechanisms underlying heart rate variability and its association with CVD and to rational therapeutic interventions.
Acknowledgements
We would like to thank all the individuals and their families for participation in this study. Korean government approved and has supported the pilot study, and phase I study (Ministry of Education & Science Technology, Grant # M10305030001-08N0503-00110).
Abbreviations
- ADRB1
adrenergic receptor gene
- AMI
acute myocardial infarction
- AR
androgen receptor
- CAV3
caveolin 3 gene
- CVD
cardiovascular disease
- F12
coagulation factor XII gene
- ET2
endothelin 2 gene
- LIPG
Endothelial lipase precursor gene
- EL
endothelial lipase
- GENDISCAN
gene discovery for complex traits in isolated large families of Asians of Northeast
- HDL-C
high density lipoprotein cholesterol
- MCP1
monocyte chemoattractant protein 1
- ZC3H12A
zinc finger CCCH type containing 12A gene
- NSD1
nuclear receptor SET domain containing gene 1
- IBD
identity by descent
- IHD
ischemic heart disease
- SOLAR
sequential oligogenic linkage analysis routines
- SNP
single nucleotide polymorphism
- SLC14A2
solute carrier family 14 gene
- TG
triglyceride
- E2F3
E2F transcription factor 1 gene
- UT-A protein
urea transporter protein
- VC
variance component
References
- 1.Bonaa KH, Arnesen E. Association between heart-rate and atherogenic blood lipid fractions in a population - the Tromso Study. Circulation. 1992;86:394–405. doi: 10.1161/01.cir.86.2.394. [DOI] [PubMed] [Google Scholar]
- 2.Brasel KJ, Guse C, Gentilello LM, Nirula R. Heart rate: Is it truly a vital sign? J Trauma. 2007;62:812–817. doi: 10.1097/TA.0b013e31803245a1. [DOI] [PubMed] [Google Scholar]
- 3.Cecconi M, Forzano F, Milani D, Cavani S, Baldo C, Selicorni A, Pantaleoni C, Silengo M, Ferrero GB, Scarano G, Della Monica M, Fischetto R, Grammatico P, Majore S, Zampino G, Memo L, Cordisco EL, Neri G, Pierluigi M, Bricarelli FD, Grasso M, Faravelli F. Mutation analysis of the NSD1 gene in a group of 59 patients with congenital overgrowth. American Journal of Medical Genetics Part A. 2005;134A:247–253. doi: 10.1002/ajmg.a.30492. [DOI] [PubMed] [Google Scholar]
- 4.Chen CC, Lamping KG, Nuno DW, Barresi R, Prouty SJ, Lavoie JL, Cribbs LL, England SK, Sigmund CD, Weiss RM, Williamson RA, Hill JA, Campbell KP. Abnormal coronary function in mice deficient in alpha(1H) T-type Ca2+ channels. Science. 2003;302:1416–1418. doi: 10.1126/science.1089268. [DOI] [PubMed] [Google Scholar]
- 5.Colhoun HM, Francis DP, Rubens MB, Underwood SR, Fuller JH. The association of heart-rate variability with cardiovascular risk factors and coronary artery calcification - A study in type 1 diabetic patients and the general population. Diabetes Care. 2001;24:1108–1114. doi: 10.2337/diacare.24.6.1108. [DOI] [PubMed] [Google Scholar]
- 6.Cribbs LL, Martin BL, Schroder EA, Keller BB, Delisle BP, Satin J. Identification of the T-type calcium channel (Ca(V)3.1d) in developing mouse heart. Circulation Research. 2001;88:403–407. doi: 10.1161/01.res.88.4.403. [DOI] [PubMed] [Google Scholar]
- 7.Diaz A. Long-term prognostic value of resting heart rate in patients with suspected or proven coronary artery disease. European Heart Journal. 2005;26:967–974. doi: 10.1093/eurheartj/ehi190. [DOI] [PubMed] [Google Scholar]
- 8.Duchesne R, Klein JD, Velotta JB, Doran JJ, Rouillard P, Roberts BR, McDonough AA, Sands JM. UT-A Urea Transporter Protein in Heart Increased Abundance During Uremia, Hypertension, and Heart Failure. Circulation Research. 2001;89:139–145. doi: 10.1161/hh1401.093293. [DOI] [PubMed] [Google Scholar]
- 9.Fox K, Borer JS, Camm AJ, Danchin N, Ferrari R, Lopez Sendon JL, Steg PG, Tardif JC, Tavazzi L, Tendera M. Resting heart rate in cardiovascular disease. Journal of the American College of Cardiology. 2007;50:823–830. doi: 10.1016/j.jacc.2007.04.079. [DOI] [PubMed] [Google Scholar]
- 10.Fujiura Y, Adachi H, Tsuruta M, Jacobs DR, Jr, Hirai Y, Imaizumi T. Heart rate and mortality in a Japanese general population: An 18-year follow-up study. Journal of Clinical Epidemiology. 2001;54:495–500. doi: 10.1016/s0895-4356(00)00323-1. [DOI] [PubMed] [Google Scholar]
- 11.Gillman MW, Kannel WB, Belanger A, D'Agostino RB. Influence of Heart-Rate on Mortality Among Persons with Hypertension - the Framingham-Study. American Heart Journal. 1993;125:1148–1154. doi: 10.1016/0002-8703(93)90128-v. [DOI] [PubMed] [Google Scholar]
- 12.Greenland P, Daviglus ML, Dyer AR, Liu K, Huang CF, Goldberger JJ, Stamler J. Resting heart rate is a risk factor for cardiovascular and noncardiovascular mortality - The Chicago Heart Association Detection Project in Industry. American Journal of Epidemiology. 1999;149:853–862. doi: 10.1093/oxfordjournals.aje.a009901. [DOI] [PubMed] [Google Scholar]
- 13.Hyunil Ha, Yunbae Pak. Modulation of the caveolin-3 and Akt status in caveolae by insulin resistance in H9c2 cardiomyoblasts. Exp Mol Med. 2005;37:169–178. doi: 10.1038/emm.2005.23. [DOI] [PubMed] [Google Scholar]
- 14.Kannel WB, Kannel C, Paffenbarger RS, Jr, Cupples LA. Heart-Rate and Cardiovascular Mortality - the Framingham-Study. American Heart Journal. 1987;113:1489–1494. doi: 10.1016/0002-8703(87)90666-1. [DOI] [PubMed] [Google Scholar]
- 15.King DE, Everett CJ, Mainous AG, Liszka HA. Long-term prognostic value of resting heart rate in subjects with prehypertension. American Journal of Hypertension. 2006;19:796–800. doi: 10.1016/j.amjhyper.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 16.Kovar D, Cannon CP, Bentley JH, Charlesworth A, Rogers WJ. Does initial and delayed heart rate predict mortality in patients with acute coronary syndromes? Clinical Cardiology. 2004;27:80–86. doi: 10.1002/clc.4960270207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kristal-Boneh E, Silber H, Harari G, Froom P. The association of resting heart rate with cardiovascular, cancer and all-cause mortality - Eight year follow-up of 3527 male Israeli employees (the CORDIS Study) European Heart Journal. 2000;21:116–124. doi: 10.1053/euhj.1999.1741. [DOI] [PubMed] [Google Scholar]
- 18.Kupper NH, Willemsen G, van den Berg M, de Boer D, Posthuma D, Boomsma DI, de Geus EJ. Heritability of ambulatory heart rate variability. Circulation. 2004;110:2792–2796. doi: 10.1161/01.CIR.0000146334.96820.6E. [DOI] [PubMed] [Google Scholar]
- 19.Laramie JM, Wilk JB, Hunt SC, Ellison RC, Chakravarti A, Boerwinkle E, Myers RH. Evidence for a gene influencing heart rate on chromosome 5p13-14 in a meta-analysis of genome-wide scans from the NHLBI Family Blood Pressure Program. Bmc Medical Genetics. 2006;7:17. doi: 10.1186/1471-2350-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Larson MG, Atwood LD, Benjamin EJ, Cupples LA, D'Agostino RB, Sr, Fox CS, Govindaraju DR, Guo CY, Heard-Costa NL, Hwang SJ, Murabito JM, Newton-Cheh C, O'Donnell CJ, Seshadri S, Vasan RS, Wang TJ, Wolf PA, Levy D. Framingham Heart Study 100K project: genome-wide associations for cardiovascular disease outcomes. Bmc Medical Genetics. 2007;8:s5. doi: 10.1186/1471-2350-8-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin LJ, Comuzzie AG, Sonnenberg GE, Myklebust J, James R, Marks J, Blangero J, Kissebah AH. Major quantitative trait locus for resting heart rate maps to a region on chromosome 4. Hypertension. 2004;43:1146–1151. doi: 10.1161/01.HYP.0000122873.42047.17. [DOI] [PubMed] [Google Scholar]
- 22.Neumann SA, Lawrence EC, Jennings JR, Ferrell RE, Manuck SB. Heart rate variability is associated with polymorphic variation in the choline transporter gene. Psychosomatic Medicine. 2005;67:168–171. doi: 10.1097/01.psy.0000155671.90861.c2. [DOI] [PubMed] [Google Scholar]
- 23.Newton-Cheh, Guo CY, Wang TJ, O'donnell CJ, Levy D, Larson MG. Genome-wide association study of electrocardiographic and heart rate variability traits: the Framingham Heart Study. Bmc Medical Genetics. 2007;8:s7. doi: 10.1186/1471-2350-8-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O'Donnell CJ, Cupples LA, D'Agostino RB, Fox CS, Hoffmann U, Hwang SJ, Ingellson E, Liu C, Murabito JM, Polak JF, Wolf PA, Demissie S. Genome-wide association study for subclinical atherosclerosis in major arterial territories in the NHLBI's Framingham Heart Study. Bmc Medical Genetics. 2007;8:s4. doi: 10.1186/1471-2350-8-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palatini P, Julius S. Association of tachycardia with morbidity and mortality: pathophysiological considerations. Journal of Human Hypertension. 1997;11:S19–S27. [PubMed] [Google Scholar]
- 26.Palatini P. Heart rate as a risk factor for atherosclerosis and cardiovascular mortality - The effect of antihypertensive drugs. Drugs. 1999;57:713–724. doi: 10.2165/00003495-199957050-00004. [DOI] [PubMed] [Google Scholar]
- 27.Palatini P, Benetos A, Julius S. Impact of increased heart rate on clinical outcomes in hypertension - Implications for antihypertensive drug therapy. Drugs. 2006;66:133–144. doi: 10.2165/00003495-200666020-00001. [DOI] [PubMed] [Google Scholar]
- 28.Rahn KH, Barenbrock M, Hausberg M. The sympathetic nervous system in the pathogenesis of hypertension. J Hypertens Suppl. 1999;17:S11–S14. [PubMed] [Google Scholar]
- 29.Reil JC, Bohm M. The role of heart rate in the development of cardiovascular disease. Clinical Research in Cardiology. 2007;96:585–592. doi: 10.1007/s00392-007-0537-5. [DOI] [PubMed] [Google Scholar]
- 30.Rogowski O, Shapira I, Shirom A, Melamed S, Toker S, Berliner S. Heart rate and microinflammation in men: a relevant atherothrombotic link. Heart. 2007;93:940–944. doi: 10.1136/hrt.2006.101949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roldán V, Corral J, Marín F, Pineda J, Vicente V, González-Conejero R. Synergistic association between hypercholesterolemia and the C46T factor XII polymorphism for developing premature myocardial infarction. Thrombosis and Haemostasis. 2005;94:1294–1299. doi: 10.1160/TH05-06-0453. [DOI] [PubMed] [Google Scholar]
- 32.Santamaría A, Martínez-Rubio A, Mateo J, Tirado I, Soria JM, Fontcuberta J. Homozygosity of the T allele of the 46 C - T polymorphism in the F12 gene is a risk factor for acute coronary artery disease in the Spanish population. Haematologica. 2004;89:878–879. [PubMed] [Google Scholar]
- 33.Sharma P, Hingorani A, Jia H, Hopper R, Brown MJ. Quantitative association between a newly identified molecular variant in the endothelin-2 gene and human essential hypertension. Journal of Hypertension. 1999;17:1281–1287. doi: 10.1097/00004872-199917090-00007. [DOI] [PubMed] [Google Scholar]
- 34.Shimizu M, Kanazawa K, Hirata K, Ishida T, Hiraoka E, Matsuda Y, Iwai C, Miyamoto Y, Hashimoto M, Kajiya T, Akita H, Yokoyama M. Endothelial lipase gene polymorphism is associated with acute myocardial infarction, independently of high-density lipoprotein-cholesterol levels. Circ J. 2007;71:842–846. doi: 10.1253/circj.71.842. [DOI] [PubMed] [Google Scholar]
- 35.Singh JP, Larson MG, O'Donnell CJ, Tsuji H, Evans JC, Levy D. Heritability of heart rate variability - The Framingham Heart Study. Circulation. 1999;99:2251–2254. doi: 10.1161/01.cir.99.17.2251. [DOI] [PubMed] [Google Scholar]
- 36.Singh JP, Larson MG, O'Donnell CJ, Tsuji H, Corey D, Levy D. Genome scan linkage results for heart rate variability (the Framingham Heart Study) Am J Cardiol. 2002;12:1290–1293. doi: 10.1016/s0002-9149(02)02865-5. [DOI] [PubMed] [Google Scholar]
- 37.Theobald H, Wandell PE. Effect of heart rate on long-term mortality among men and women. Acta Cardiologica. 2007;62:275–279. doi: 10.2143/ac.62.3.2020817. [DOI] [PubMed] [Google Scholar]
- 38.Voss A, Busjahn A, Wessel N, Schurath R, Faulhaber HD, Luft FC, Dietz R. Familial and genetic influences on heart rate variability. J Electrocardiol. 1996;29:154–160. doi: 10.1016/s0022-0736(96)80045-8. [DOI] [PubMed] [Google Scholar]
- 39.Wilk JB, Myers RH, Zhang Y, Lewis CE, Atwood L, Hopkins PN, Ellison RC. Evidence for a gene influencing heart rate on chromosome 4 among hypertensives. Human Genetics. 2002;111:207–213. doi: 10.1007/s00439-002-0780-9. [DOI] [PubMed] [Google Scholar]
- 40.Wilk JB, Myers RH, Pankow JS, Hunt SC, Leppert MF, Freedman BI, Province MA, Ellison RC. Adrenergic receptor polymorphisms associated with resting heart rate: The HyperGEN study. Annals of Human Genetics. 2006;70:566–573. doi: 10.1111/j.1469-1809.2005.00258.x. [DOI] [PubMed] [Google Scholar]
- 41.Woodman SE, Park DS, Cohen AW, Cheung MW, Chandra M, Shirani J, Tang B, Jelicks LA, Kitsis RN, Christ GJ, Factor SM, Tanowitz HB, Lisanti MP. Caveolin-3 knock-out mice develop a progressive cardiomyopathy and show hyperactivation of the p42/44 MAPK cascade. Journal of Biological Chemistry. 2002;277:38988–38997. doi: 10.1074/jbc.M205511200. [DOI] [PubMed] [Google Scholar]
- 42.Zhou L, Azfer A, Niu J, Graham S, Choudhury M, Adamski Frances M., Younce C, Binkley Phillip F., Kolattukudy Pappachan E. Monocyte Chemoattractant Protein-1 Induces a Novel Transcription Factor That Causes Cardiac Myocyte Apoptosis and Ventricular Dysfunction. Circ Res. 2006;98:1177–1185. doi: 10.1161/01.RES.0000220106.64661.71. [DOI] [PMC free article] [PubMed] [Google Scholar]