Abstract
The etiology and pathogenesis of type 2 diabetes mellitus (T2DM) are not completely understood although it is often associated with other conditions such as obesity, hypertension, and dyslipidemia. Lipoprotein lipase (LPL) is a key enzyme in human lipid metabolism that facilitates the removal of triglyceride-rich lipoproteins from the bloodstream. LPL hydrolyzes the core of triglyceride-rich lipoproteins (chylomicrons and very low density lipoprotein) into free fatty acids and monoacylglycerol. To gain insight into the possible role of LPL in T2DM, nine single nucleotide polymorphisms (SNPs) of LPL were analyzed for the association with T2DM using 944 unrelated Koreans, including 474 T2DM subjects and 470 normal healthy controls. Of the nine LPL SNPs we analyzed, a significant association with multiple tests by the false discovery rate (FDR) was observed between T2DM and SNP rs343 (+13836C>A in intron 3). SNP rs343 was also marginally associated with some of T2DM-related phenotypes including total cholesterol, high density lipoprotein cholesterol (HDLc), and log transformed glycosylated hemoglobin in 470 normal controls, although no significant association was detected by multiple tests. In total, our results suggest that the control of lipid level by LPL in the bloodstream might be an important factor in T2DM pathogenesis in the Korean population.
Keywords: Asian continental ancestry group; diabetes mellitus, type 2; haplotypes; lipoprotein lipase; polymorphism, single nucleotide
Introduction
The normal glucose level in the blood is coordinately maintained by a complex interplay between the insulin responsiveness of key insulin target tissues (skeletal muscle, liver, adipose tissue, kidney, and brain) and glucose-stimulated insulin secretion by pancreatic β cells (Lowell and Shulman, 2005). In type 2 diabetes mellitus (T2DM), a failure in this coordination causes insulin resistance or insufficient insulin secretion by the pancreas, ultimately leading to high blood glucose levels (Alberti and Zimmet, 1998). Although genetic and environmental factors are believed to be closely related to T2DM, the exact mechanisms that underlie dysfunction of insulin uptake or secretion in T2DM are not clear.
Deviations from normal levels of fats in the blood (dyslipidemia) are consistently associated with T2DM. Dyslipidemia associated with T2DM is characterized by high levels of both plasma triglycerides (TGs) and very low density lipoprotein (VLDL) and low levels of high density lipoprotein (HDL) (Taskinen, 2003). Several lines of evidence indicate that high TGs play a role in insulin resistance and T2DM (Mingrone et al., 1999; Yang et al., 2003a). TGs are present in circulating chylomicrons and VLDL particles and hydrolyzed by lipoprotein lipase (LPL) into nonesterified fatty acids and 2-monoacylglycerol for tissue utilization and HDL formation (Mead et al., 2002; de Vries et al., 2003; Kalmar et al., 2005). Thus, LPL has a central role in both VLDL and HDL metabolism. Deficiency or dysfunction of LPL has been associated with various diseases including atherosclerosis, chylomicronemia, obesity, Alzheimer's disease, and the dyslipidemia related to diabetes and insulin resistance (Mead et al., 2002). In T2DM, LPL activity is commonly deficient and contributes to the increased level of serum TGs and the decreased level of HDL (Taskinen, 1987; Klannemark et al., 2000; Kalmar et al., 2005).
Several studies have shown an association between genetic variations in LPL and lipid metabolism in T2DM patients (Marcais et al., 2000; Ma et al., 2003; Socquard et al., 2006). For example, an association between higher plasma TGs and lower HDL cholesterol levels and the H+ allele of LPL HindIII polymorphism has been reported in Chinese patients with early-onset T2DM (Ma et al., 2003). Several studies have also shown associations between polymorphisms in LPL and T2DM-related complications (Ukkola et al., 1995; Mattu et al., 2002; Solini et al., 2004; Ng et al., 2006; Javorsky et al., 2006). For instance, the LPL S447X polymorphism is associated with nephropathy in T2DM patients (Ng et al., 2006). However, to our knowledge, few studies have identified genetic variations in LPL that are directly associated with T2DM, although a recent study reported that a polymorphism in the promoter region (-G53C) of the LPL gene is protective against T2DM (Radha et al., 2007).
To identify LPL polymorphisms, we sequenced the LPL genomic region from 24 unrelated Koreans and detected 31 genetic variants. In an attempt to reveal the genetic variations in the LPL gene associated with T2DM, we analyzed nine selected single nucleotide polymorphisms (SNPs) in 944 unrelated Koreans (474 T2DM subjects and 470 normal controls). Using the SNP genotyping data from these nine SNPs, we also analyzed the association of LPL SNPs with T2DM-related phenotypes such as obesity, blood pressure, dyslipidemia, blood glucose, and blood insulin in normal healthy controls. Our data demonstrated a significant association between one SNP in LPL intron 3 (+13836C>A) and T2DM. In addition, this polymorphism was also marginally associated with total cholesterol (TCHOL), high density lipoprotein cholesterol (HDLc), and log transformed glycosylated hemoglobin (log-HbA1C), when the false discovery rate (FDR) estimation to account for the multiple comparisons was not considered in the analysis.
Materials and Methods
Sequencing analysis for LPL SNP identification
Genetic variants of the LPL gene were identified by sequencing analysis of DNA from 24 unrelated Koreans. We sequenced the entire exons, 5' untranslated region (UTR), 3' UTR, up to several hundred base pairs of exon-intron boundary regions (including the splice junctions), and the promoter region (approximately 1.0 kb upstream from the transcriptional start site). The information for the gene and genomic DNA sequence of LPL was obtained from GenBank (http://www.ncbi/nlm.nih.gov/). Genomic regions targeted for sequencing were amplified by PCR from genomic DNA of 24 immortalized cell lines generated from unrelated Koreans. Primers for PCR were designed using the Primer3 program (http://www-genome.wi.mit.edu/cgi-bin/primer/primer3_www.cgi) (Rozen and Skaletsky, 2000) (Supplemental Table 1). PCR-amplified fragments were sequenced on both strands using an ABI Prism 3730 sequencer (Applied Biosystems, Foster City, CA) according to the manufacturer's protocol. The PolyPhred program (http://www.droog.gs.wasington.edu/PolyPhred.html) was used to assemble the sequences and identify SNPs (Nickerson et al., 1997).
Subjects
Two community cohorts (Ansung and Ansan) in South Korea were initiated from 2001 as major projects for the Korean Health and Genome Study (KHGS). The Ansan cohort primarily represents an urban community, whereas the Ansung cohort represents a rural community. All participants in either cohort were 40-69 years old, had resided within the boarders of the survey area for at least 6 months, and were mentally and physically healthy to participate. Cohort examinations with participants' consent were accomplished biennially for the prospective studies. To date, 2,239 men and 2,779 women in Ansung, and 2,523 men and 2,497 women in Ansan have participated in the cohorts.
In this study, 474 unrelated individuals were recruited from 10,038 individuals in the Ansung-Ansan prospective community cohort as T2DM subjects according to World Health Organization criteria. A total of 470 unrelated individuals who had no history of diabetes, no first-degree relatives with diabetes, fasting plasma glucose level less than 126 mg/dl, plasma glucose level 120 min after glucose ingestion (glucose 120) less than 140 mg/dl, and HbA1C level less than 5.8% were recruited as normal control subjects from the cohort. To be eligible, normal control subjects also had to be free of medications for diabetes, hypertension, and dyslipidemia. Both T2DM and normal control subjects were ≥ 60 years of age. The clinical profiles of the study subjects are summarized in Table 1. The study was approved by the institutional review board of the Korean National Institute of Health. All subjects gave written informed consent.
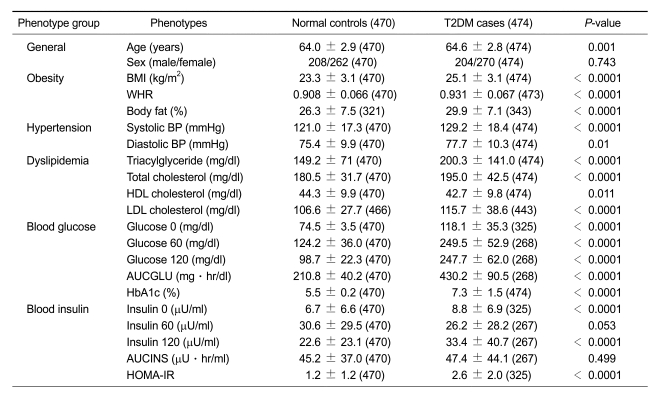
Table 1.
Clinical profile of study subjects.
Values are mean ± standard deviation (SD). Values in parentheses are the number of subjects assessed for each clinical profile. P values: T2DM cases versus normal controls. (BMI, body mass index; WHR, waist hip ratio; BP, blood pressure; Glucose 0, fasting plasma glucose level; Glucose 60 and 120, plasma glucose level 60 and 120 min after glucose ingestion, respectively; Insulin 0, fasting plasma insulin level; Insulin 60 and insulin 120, plasma insulin level 60 and 120 min after glucose ingestion, respectively; AUCGLU, glucose area under the curve; AUCINS, insulin area under the curve; HbA1C, glycosylated hemoglobin; HOMA-IR, homeostasis model assessment-insulin resistance; HDL, high density lipoprotein; LDL, low density lipoprotein).
Genotyping
Among 31 LPL SNPs identified from 24 unrelated Korean subjects, 11 SNPs (rs343, +13836C>A; rs249, +14055T>C; rs254, +14946C>G; rs316, +21485C>A; rs328, +22773C>G; rs4922115, +25879G>A; rs3208305, +26697A>T; rs3200218, +27120A>G; rs13702, +27541T>C; rs3866471, +27718C>A; rs9644636, +27945T>G) were selected for subsequent large scale genotyping. Selection was based on their tagging status. Minor allele frequencies of 31 LPL SNPs obtained from sequencing results of 24 unrelated Korean subjects were used to calculate the pair-wise r2 coefficient (Hao et al., 2007). SNPs were chosen as tagging SNPs if they were common SNPs (minor allele frequency ≥ 0.02) and were predicted by r2 value ≥ 0.8. SNPs in exons or promoter regions were preferred in SNP selection (Supplemental Figure 1 and Supplemental Table 1) (Stram et al., 2003).
Genotyping of total 944 subjects was performed for 11 SNPs selected in LPL by an allelic discrimination assay using the TaqMan (Aplied Bio systems) reaction as described (Hurd et al., 2000). Duplicate genotyping for about 10% of samples was performed as a quality control. Only SNP genotyping results that satisfied the concordance rate in duplicates > 99% and the genotype success rate > 97% were allowed for subsequent association analyses.
Statistics
Deviation from the expected Hardy-Weinberg frequency was examined with the chi-square (χ2) test. Minor allele frequencies and heterozygosities in terms of functional location were calculated from each SNP genotyping result of study subjects. A haplotype block was generated by a linkage disequilibrium (D') plot of LPL in study subjects using HaploView v3.2 (http://www.broad.mit.edu/mpg/haploview/)(Barrett et al., 2005). Haplotypes were also inferred by HaploView analysis for given SNPs of the LPL gene. The associations of SNPs or haplotypes with T2DM between controls and T2DM patients were determined by logistic regression analysis while controlling for age, sex, and body mass index (BMI). The associations between SNPs or haplotypes and T2DM-related subphenotypes were determined by linear regression analysis while controlling for age, sex, and BMI. Only 470 normal control subjects were used for linear regression analyses of T2DM-related subphenotypes in order to exclude possible influences of T2DM treatment on the phenotypic values in the T2DM patients. Among several phenotypes (Table 1), the levels of TG and all blood glucose and insulin related phenotypes were transformed with logarithm to normalize their skewed distribution. Several clinical parameters of T2DM related phenotypes were compared between T2DM cases and control subjects, showing a statistically significant difference between the two groups except with respect to parameters such as age, insulin level 60 min after glucose ingestion (Insulin 60), and insulin area under the curve (AUCINS) (Table 1). The SAS statistical software package (SAS Institute Inc., Cary, NC) was used to perform general statistical analyses. Statistical significance was determined at a two-tailed value of P < 0.05. For the multiple comparisons, the FDR estimation method was applied to the association analyses (Pounds and Cheng, 2006; Forner et al., 2008).
Korean SNP database
The information for most SNPs described in this study is available in the Korean SNP database (http://www.ksnp.ngri.re.kr/SNP/index.jsp) that was constructed at the Center for Genome Sciences (Korean National Institute of Health).
Results
We identified a total of 31 genetic variants of the LPL gene from 24 unrelated Korean subjects by sequencing (Supplemental Figure 1 and http://www.ngri.re.kr/SNP/index.jsp). Among them, 11 SNPs selected as tagging SNPs based on the criterion of pair-wise correlation coefficient, r2 ≥ 0.8 were genotyped from a total of 474 patient and 470 control subjects to discover genetic polymorphisms implicated in T2DM. The average genotyping success rate was 99.3% and a minimum was 97.1% for SNP rs328. Duplicate genotyping for 10% of the samples as a quality control showed no mismatches among duplicates, indicating highgenotyping reproducibility.
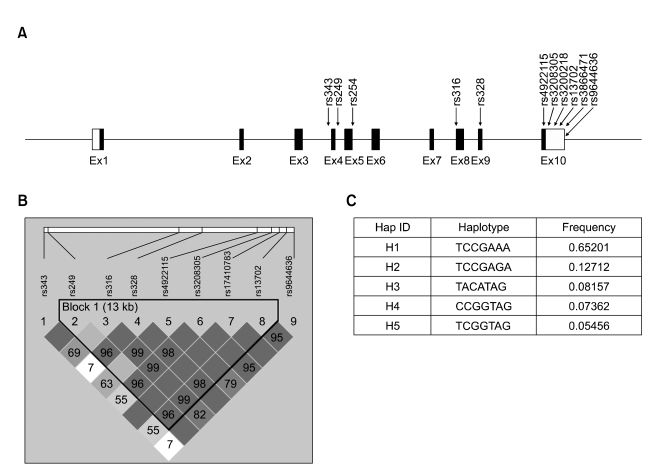
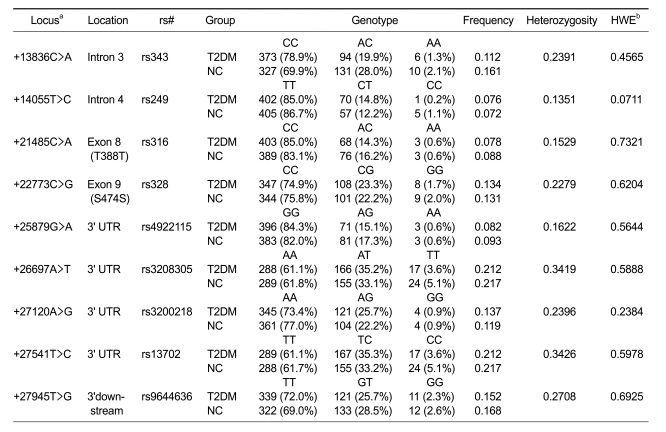
Eleven SNPs of the LPL gene analyzed in this study were localized in introns (rs343, rs249, and rs254), the coding region (rs316 and rs328), 3'UTR (rs4922115, rs3208305, rs3200218, rs13702, and rs3866471) and 3' downstream region (rs9644636) on chromosome 8p22 (Figure 1A). In the normal control subjects, the genotype distributions of nine SNPs were in Hardy-Weinberg equilibrium (P > 0.05) (Table 2) but two (rs254 and rs3866471) were not. Thus, in subsequent association studies we further analyzed the nine SNPs that were in Hardy-Weinberg equilibrium. The minor allele frequencies of these nine SNPs were 0.137, 0.074, 0.083, 0.132, 0.088, 0.215, 0.128, 0.215, and 0.16 at positions +13836C>A (rs343), +14055T>C (rs249), +21485C>A (rs316), +22773C>G (rs328), +25879G>A (rs4922115), +26697A>T (rs3208305), +27120A>G (rs3200218), +27541T>C (rs13702), and +27945T>G (rs9644636), respectively. The observed heterozygosity of each polymorphic locus in the population is indicated in Table 2.
Figure 1.
Gene map and haplotypes in LPL. (A) Gene map and SNPs in the LPL gene on chromosome 8p22. Black boxes denote coding exons, and white boxes denote 5' and 3' UTRs. The locations of the SNPs within the gene are shown by arrows. (B) Haplotype block generated by a linkage disequilibrium (D') plot of the LPL gene in subjects from the Ansung-Ansan cohort in Korea. All numbers in squares represent the D' value expressed as a percentile. All squares without numbers represent D' = 1. Plots were generated using HaploView v3.2. (C) Haplotypes of the LPL gene. Haplotypes with frequency > 0.05 are presented.
Table 2.
Genotype distribution of LPL polymorphisms in type 2 diabetes mellitus (T2DM) cases (n = 474) and normal control (NC) subjects (n = 470) in the Korean population.
aThe number and + sign in the locus indicate the nucleotide number downstream from translational start site; bP values of deviation from HWE among all subjects
One haplotype block comprising seven SNPs (rs249, rs316, rs328, rs4922115, rs3208305, rs3200218, and rs13702) could be constructed due to very strong linkage disequilibrium (LD) among nine SNPs in the LPL gene (Figure 1B). We used HaploView v3.2 to generate the haplotype block (Barrett et al., 2005). Among all possible haplotypes from seven SNPs, five common haplotypes with frequencies greater than 5% were used for further analyses (Figure 1C).
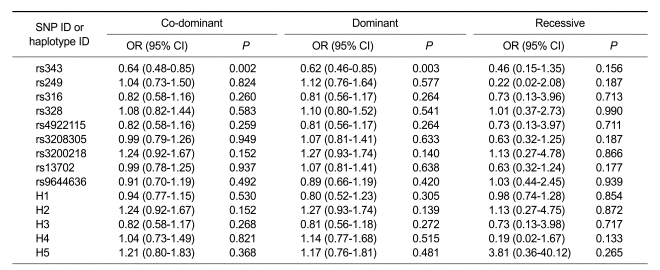
To identify genetic variants of the LPL gene that are associated with T2DM, we performed logistic regression analysis for nine SNPs and five haplotypes. Logistic analyses controlling for age, sex, and BMI indicated a significant association (protective effect) of one SNP (rs343, +13826C>A) with T2DM (P = 0.002, OR = 0.64, co-dominant model; P = 0.003, OR = 0.62, dominant model). The association of SNP rs314 was still retained even after the multiple comparisons with FDR estimation (P = 0.038 in the codominant model). The other eight SNPs and all five haplotypes were not associated with T2DM (Table 3). It is noteworthy that rs343 was not in a haplotype block generated in this study due to weak LD with other SNPs (Figure 1B). The frequency of the +13836A genotype was higher in normal control subjects (30.1%) than in T2DM subjects (21.2%) (Table 2).
Table 3.
Logistic analysis of LPL SNPs and haplotypes in T2DM and normal control subjects while controlling for age, sex, and BMI as covariates.
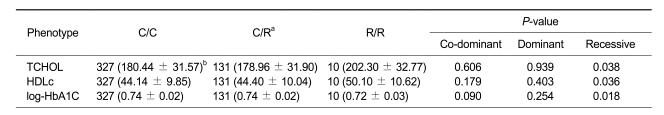
To gain insight into the genetic relevance of LPL polymorphisms to T2DM risk factors (such phenotypes related to obesity, hypertension, dyslipidemia, blood glucose, and blood insulin), linear regression analyses between LPL polymorphisms (including nine SNPs and five haplotypes) and risk factors were performed in normal control subjects (Supplemental Tables 2 and 3). For these linear regression analyses, we only used 470 normal control subjects since treatment for T2DM may affect on the phenotypic values. Without considering multiple tests, significant associations were detected between rs343 (+13826C>A) and T2DM-related subphenotypes such as total cholesterol (TCHOL; P = 0.038, recessive model), high density lipoprotein cholesterol (HDLc; P = 0.036, recessive model), and log-transformed glycosylated hemoglobin (log-HbA1C; P = 0.018, recessive model) (Table 4). The relevance of HDLc and HbA1C to rs343 agrees with T2DM association of this polymorphism, whereas TCHOL is not consistent (see Discussion).
Table 4.
Regression analyses of rs343 with total cholesterol (TCHOL), high density lipoprotein cholesterol (HDLc), and natural log transformed glycosylated hemoglobin (ln-HbA1C) while controlling for age, sex, and BMI as covariates in 470 normal controls.
aC and R indicate common allele and rare allele, respectively; bNumbers in parentheses indicate mean ± standard deviation. Unit for both TCHOL and HDLc is mg/dl, and unit for log-HbA1C is %.
Three LPL SNPs, rs3208305, rs13702, and rs9644636, were not associated with any T2DM-related risk factors, whereas other LPL SNPs primarily had significant associations with blood glucose-related phenotypes (rs316 with log-glucose 0, and log-HbA1C; rs328 with log-glucose 60, and log-AUCGLU; rs4922115 with log-glucose 0, and log-HbA1C). In addition, rs316 was associated with BODY_FAT (obesity-related phenotype), and rs3200218 was associated with WHR (obesity-related phenotype) and TCHOL and LDLc (dyslipidemia-related phenotype) (Supplemental Table 2). Five haplotypes also showed significant associations with at least one T2DM-related risk factor (Supplemental Table 3).
When LPL SNPs were examined with the FDR estimation for the association with T2DM-related phenotypes, most P values corrected for the multiple comparisons were not in the statistically significant levels. However, it is noteworthy that our results still suggest the possible involvement of LPL SNPs in the pathogenesis of T2DM via T2DM-related phenotypes.
Discussion
LPL is one of the candidate genes of dyslipidemia (Hoffer et al., 1998; Julien et al., 1998; Pillarisetti and Saxena, 2003; Pruneta-Deloche et al., 2005) and hypertension (Williams et al., 1994; Yang et al., 2003b; Li et al., 2004; Chen et al., 2005) because its gene product is a major regulator of triglyceride clearance in the blood. LPL catalyzes the hydrolysis of triglycerides of circulating chylomicrons and VLDL, excesses of which are the potent causes of both disorders. T2DM is a common metabolic disorder for which the etiology is not yet clearly understood. About one-third of T2DM patients have hypertension and/or dyslipidemia, indicating the relationship between these disorders and T2DM (Tkac, 2005). High triglyceride levels in the blood (hypertriglyceridemia) are also seen in 20~60% of T2DM patients, and these levels are two to three times higher than in non-diabetic subjects (Taskinen, 1992; Klannemark et al., 2000). Furthermore, insulin resistance is associated with increased cholesterol synthesis and decreased cholesterol absorption in normoglycemic men (McPherson and Jones, 2003). Thus, we hypothesized that there may be a genetic link between the LPL gene and T2DM. Interestingly, LPL has been predicted to be one of nine potent T2DM genes by the application of seven independent computational disease gene prioritization methods to the analysis of 9,556 positional candidate genes for T2DM and the related trait, obesity (Tiffin et al., 2006).
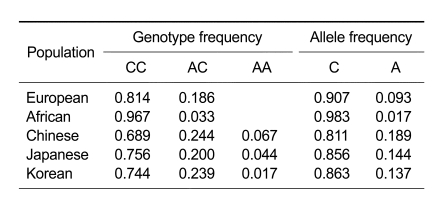
As one way to address our hypothesis, we studied possible associations between T2DM and LPL polymorphisms. Our findings in this study demonstrate that individuals who have the A allele at LPL +13836 (rs343 on chromosome 8p22) appear to be protected against T2DM (Tables 2 and 3). Allele and genotype frequencies of LPL +13836C>A in the Korean population observed in this study were compared with those in other populations obtained from HapMap data (Table 5). Similar patterns of both frequencies were detected between Korean and Japanese populations rather than other populations, suggesting that LPL +13836C>A might be a useful marker for a T2DM association study in the Japanese population as well. The SNP rs343 (+13836C>A) is located in intron 3 on chromosome 8p22. Thus, it is likely that T2DM-associated LPL +13836C>A serves as a disease marker rather than a disease-causing SNP, although the possibility that this SNP may be a regulatory variant in modulating splicing (Baralle and Baralle, 2005) or transcription factor binding (Liao et al., 2004) cannot be excluded.
Table 5.
Allele frequencies and genotype frequencies of LPL +13836C>A (rs343) among different population groups.
Allele frequencies and genotype frequencies of all populations except Korean were obtained from HapMap data (http://www.ncbi.nlm.nih.gov/SNP/snp_ref.cgi?rs=343).
Power analysis was performed using the Quanto program (Gauderman, 2002) to compute sample size or power for the case-control association study of the LPL gene. Assuming α = 0.05, we had 89% power for LPL rs343 which had a minor allele frequency of 0.137 to detect an odds ratio of 0.64 in the protective component of the study in the co-dominant model. We also had 83% and 27% power to detect odds ratio of 0.62 and 0.46 in dominant and recessive models, respectively. The sample sizes of T2DM case for 80% power were 388, 405, and 1954 for the case-control association study of LPL rs343 in the co-dominant model, dominant model, and recessive model, respectively, indicating that the sample size was adequate for our study using both co-dominant and dominant models, but not sufficient using recessive model.
Not only genetic factors (such as family history) but also environmental factors (such as obesity, hypertension, dyslipidemia, blood glucose, and blood insulin) are considered to be crucial risk factors for T2DM. Therefore, understanding the genetic relationship between LPL and those T2DM-related risk factors might help unravel the etiology of T2DM. We analyzed nine LPL SNPs as well as five haplotypes from 470 normal control subjects to detect their association with several T2DM-related risk factors including phenotypes related to obesity, hypertension, dyslipidemia, blood glucose, and blood insulin. Without considering multiple tests, overall results of linear regression analyses controlling for age, sex, and BMI as covariates are summarized in Supplemental Tables 2 and 3.
Without considering multiple tests, the SNP rs343 was also marginally associated with dyslipidemia-related phenotypes (TCHOL and HDLc) as well as the blood gluose-related phenotype (log-HbA1C) (Table 4). Because glucose binds to hemoglobin to produce HbA1C, the level of HbA1C in circulating blood can be used as an indicator of the blood glucose level. Increased levels of blood glucose due to insulin resistance of tissues or the defect of pancreatic β-cell in insulin secretion are responsible for the high levels of HbA1C in the blood. Regression analyses of log-HbA1C with rs343 (+13836C>A) indicated that individuals who have a homozygous A allele have a lower level of HbA1C compared to individuals harboring the C allele (P = 0.018, recessive model; Table 4). This result is consistent with the protective effect of the A allele for T2DM (Table 3). The homozygous A allele also contributes to the high level of HDLc (P = 0.036, recessive model; Table 4). Considering the central role of LPL in HDL formation (Mead et al., 2002), this observation agrees with the beneficial genetic predisposition of the A allele with respect to T2DM (Table 3). The significant relevance of rs343 to TCHOL was also detected from regression analyses, in which a higher TCHOL level was evident in individuals homozygous for the A allele (P = 0.038, recessive model; Table 4). Considering the protective effect of the A allele-containing genotype for T2DM, this result does not appear to be consistent with the association result of rs343 with T2DM (Table 3). However, it is possible that this observed association might be affected by other various genetic and environmental factors or the complicated interactions of both factors.
In our study, the association of SNP rs343 with T2DM (P = 0.002 in the co-dominant model; P = 0.003 in the dominant model) was still significant at the α = 0.05 level even after multiple tests by the FDR estimation, while the association with T2DM-related phenotypes was not retained after multiple tests possibly due to the insufficient sample size (n = 470). Thus, the replication study in the large population would be necessary to prove the association between rs343 and T2DM-related phenotypes. In conclusion, we report one LPL SNP (rs343) that has a significant association in the Korean population with T2DM. This finding supports our hypothesis that the LPL gene product, which controls lipid levels in the blood, might be one of the important genetic factors in determining the onset of T2DM in the Korean population.
Acknowledgements
This study was supported by an intramural grant of the National Institute of Health, Korea.
Abbreviations
- AUCGLU
glucose area under the curve
- AUCINS
insulin area under the curve
- BMI
body mass index
- DBP
diastolic blood pressure
- FDR
false discovery rate
- HbA1C
glycosylated hemoglobin
- HDLc
high density lipoprotein cholesterol
- HOMA-IR
homeostasis model assessment-insulin resistance
- LDLc
low density lipoprotein cholesterol
- LPL
lipoprotein lipase
- SBP
systolic blood pressure
- T2DM
type 2 diabetes mellitus
- TCHOL
total cholesterol
- TG
triglyceride
- UTR
untranslated region
- WHR
waist hip ratio
Supplementary Material
References
- 1.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 2.Baralle D, Baralle M. Splicing in action: assessing disease causing sequence changes. J Med Genet. 2005;42:737–748. doi: 10.1136/jmg.2004.029538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–265. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- 4.Chen P, Jou YS, Fann CS, Chen JW, Wu SY, Pan WH. Lipoprotein lipase gene is linked and associated with hypertension in Taiwan young-onset hypertension genetic study. J Biomed Sci. 2005;12:651–658. doi: 10.1007/s11373-005-7707-0. [DOI] [PubMed] [Google Scholar]
- 5.de Vries R, Borggreve SE, Dullaart RP. Role of lipases, lecithin: cholesterol acyltransferase and cholesteryl ester transfer protein in abnormal high density lipoprotein metabolism in insulin resistance and type 2 diabetes mellitus. Clin Lab. 2003;49:601–613. [PubMed] [Google Scholar]
- 6.Forner K, Lamarine M, Guedj M, Dauvillier J, Wojcik J. Universal false discovery rate estimation methodology for genome-wide association studies. Hum Hered. 2008;65:183–194. doi: 10.1159/000112365. [DOI] [PubMed] [Google Scholar]
- 7.Gauderman WJ. Sample size requirements for association studies of gene-gene interaction. Am J Epidemiol. 2002;155:478–484. doi: 10.1093/aje/155.5.478. [DOI] [PubMed] [Google Scholar]
- 8.Hao K, Di X, Cawley S. LdCompare: rapid computation of single- and multiple-marker r2 and genetic coverage. Bioinformatics. 2007;23:252–254. doi: 10.1093/bioinformatics/btl574. [DOI] [PubMed] [Google Scholar]
- 9.Hoffer MJ, Bredie SJ, Snieder H, Reymer PW, Demacker PN, Havekes LM, Boomsma DI, Stalenhoef AF, Frants RR, Kastelein JJ. Gender-related association between the -93T-->G/D9N haplotype of the lipoprotein lipase gene and elevated lipid levels in familial combined hyperlipidemia. Atherosclerosis. 1998;138:91–99. doi: 10.1016/s0021-9150(98)00007-0. [DOI] [PubMed] [Google Scholar]
- 10.Hurd C, Ocheja A, Cheetham-Wilkinson C, Ouwehand W. HPA-1, -2 and -3 genotyping using the TaqMan reaction. Transfusion Medicine. 2000;10:326–326. [Google Scholar]
- 11.Javorsky M, Kozarova M, Salagovic J, Tkac I. Relationship among urinary albumin excretion rate, lipoprotein lipase PvuII polymorphism and plasma fibrinogen in type 2 diabetic patients. Physiol Res. 2006;55:55–62. doi: 10.33549/physiolres.930704. [DOI] [PubMed] [Google Scholar]
- 12.Julien P, Gagne C, Murthy MR, Levesque G, Moorjani S, Cadelis F, Hayden MR, Lupien PJ. Dyslipidemias associated with heterozygous lipoprotein lipase mutations in the French-Canadian population. Hum Mutat. 1998;(Suppl 1):S148–S153. doi: 10.1002/humu.1380110150. [DOI] [PubMed] [Google Scholar]
- 13.Kalmar T, Seres I, Balogh Z, Kaplar M, Winkler G, Paragh G. Correlation between the activities of lipoprotein lipase and paraoxonase in type 2 diabetes mellitus. Diabetes Metab. 2005;31:574–580. doi: 10.1016/s1262-3636(07)70233-1. [DOI] [PubMed] [Google Scholar]
- 14.Klannemark M, Suurinkeroinen L, Orho-Melander M, Groop L, Taskinen MR. Interaction between the Asn291Ser variant of the LPL gene and insulin resistance on dyslipidaemia in high risk individuals for Type 2 diabetes mellitus. Diabet Med. 2000;17:599–605. doi: 10.1046/j.1464-5491.2000.00343.x. [DOI] [PubMed] [Google Scholar]
- 15.Li B, Ge D, Wang Y, Zhao W, Zhou X, Gu D, Chen R. Lipoprotein lipase gene polymorphisms and blood pressure levels in the Northern Chinese Han population. Hypertens Res. 2004;27:373–378. doi: 10.1291/hypres.27.373. [DOI] [PubMed] [Google Scholar]
- 16.Liao G, Wang J, Guo J, Allard J, Cheng J, Ng A, Shafer S, Puech A, McPherson JD, Foernzler D, Peltz G, Usuka J. In silico genetics: identification of a functional element regulating H2-Ealpha gene expression. Science. 2004;306:690–695. doi: 10.1126/science.1100636. [DOI] [PubMed] [Google Scholar]
- 17.Lowell BB, Shulman GI. Mitochondrial dysfunction and type 2 diabetes. Science. 2005;307:384–387. doi: 10.1126/science.1104343. [DOI] [PubMed] [Google Scholar]
- 18.Ma YQ, Thomas GN, Ng MC, Critchley JA, Chan JC, Tomlinson B. The lipoprotein lipase gene HindIII polymorphism is associated with lipid levels in early-onset type 2 diabetic patients. Metabolism. 2003;52:338–343. doi: 10.1053/meta.2003.50053. [DOI] [PubMed] [Google Scholar]
- 19.Marcais C, Bernard S, Merlin M, Ulhmann M, Mestre B, Rochet-Mingret L, Revol A, Berthezene F, Moulin P. Severe hypertriglyceridaemia in Type II diabetes: involvement of apoC-III Sst-I polymorphism, LPL mutations and apo E3 deficiency. Diabetologia. 2000;43:1346–1352. doi: 10.1007/s001250051537. [DOI] [PubMed] [Google Scholar]
- 20.Mattu RK, Trevelyan J, Needham EW, Khan M, Adiseshiah MA, Richter D, Murray RG, Betteridge DJ. Lipoprotein lipase gene variants relate to presence and degree of microalbuminuria in Type II diabetes. Diabetologia. 2002;45:905–913. doi: 10.1007/s00125-002-0824-7. [DOI] [PubMed] [Google Scholar]
- 21.McPherson R, Jones PH. The metabolic syndrome and type 2 diabetes: role of the adipocyte. Curr Opin Lipidol. 2003;14:549–553. doi: 10.1097/00041433-200312000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Mead JR, Irvine SA, Ramji DP. Lipoprotein lipase: structure, function, regulation, and role in disease. J Mol Med. 2002;80:753–769. doi: 10.1007/s00109-002-0384-9. [DOI] [PubMed] [Google Scholar]
- 23.Mingrone G, Henriksen FL, Greco AV, Krogh LN, Capristo E, Gastaldelli A, Castagneto M, Ferrannini E, Gasbarrini G, Beck-Nielsen H. Triglyceride-induced diabetes associated with familial lipoprotein lipase deficiency. Diabetes. 1999;48:1258–1263. doi: 10.2337/diabetes.48.6.1258. [DOI] [PubMed] [Google Scholar]
- 24.Ng MC, Baum L, So WY, Lam VK, Wang Y, Poon E, Tomlinson B, Cheng S, Lindpaintner K, Chan JC. Association of lipoprotein lipase S447X, apolipoprotein E exon 4, and apoC3 -455T>C polymorphisms on the susceptibility to diabetic nephropathy. Clin Genet. 2006;70:20–28. doi: 10.1111/j.1399-0004.2006.00628.x. [DOI] [PubMed] [Google Scholar]
- 25.Nickerson DA, Tobe VO, Taylor SL. PolyPhred: automating the detection and genotyping of single nucleotide substitutions using fluorescence-based resequencing. Nucleic Acids Res. 1997;25:2745–2751. doi: 10.1093/nar/25.14.2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pillarisetti S, Saxena U. Lipoprotein lipase as a therapeutic target for dyslipidemia. Front Biosci. 2003;8:d238–d241. doi: 10.2741/958. [DOI] [PubMed] [Google Scholar]
- 27.Pounds S, Cheng C. Robust estimation of the false discovery rate. Bioinformatics. 2006;22:1979–1987. doi: 10.1093/bioinformatics/btl328. [DOI] [PubMed] [Google Scholar]
- 28.Pruneta-Deloche V, Marcais C, Perrot L, Sassolas A, Delay M, Estour B, Lagarde M, Moulin P. Combination of circulating antilipoprotein lipase (Anti-LPL) antibody and heterozygous S172 fsX179 mutation of LPL gene leading to chronic hyperchylomicronemia. J Clin Endocrinol Metab. 2005;90:3995–3998. doi: 10.1210/jc.2005-0205. [DOI] [PubMed] [Google Scholar]
- 29.Radha V, Vimaleswaran KS, Ayyappa KA, Mohan V. Association of lipoprotein lipase gene polymorphisms with obesity and type 2 diabetes in an Asian Indian population. Int J Obes (Lond) 2007;31:913–918. doi: 10.1038/sj.ijo.0803547. [DOI] [PubMed] [Google Scholar]
- 30.Rozen S, Skaletsky H. Primer3 on the WWW for general users and for biologist programmers. Methods Mol Biol. 2000;132:365–386. doi: 10.1385/1-59259-192-2:365. [DOI] [PubMed] [Google Scholar]
- 31.Socquard E, Durlach A, Clavel C, Nazeyrollas P, Durlach V. Association of HindIII and PvuII genetic polymorphisms of lipoprotein lipase with lipid metabolism and macrovascular events in type 2 diabetic patients. Diabetes Metab Rev. 2006;32:262–269. doi: 10.1016/s1262-3636(07)70278-1. [DOI] [PubMed] [Google Scholar]
- 32.Solini A, Passaro A, Fioretto P, Nannipieri M, Ferrannini E. Lipoprotein lipase gene variants and progression of nephropathy in hypercholesterolaemic patients with type 2 diabetes. J Intern Med. 2004;256:30–36. doi: 10.1111/j.1365-2796.2004.01332.x. [DOI] [PubMed] [Google Scholar]
- 33.Stram DO, Haiman CA, Hirschhorn JN, Altshuler D, Kolonel LN, Henderson BE, Pike MC. Choosing haplotype-tagging SNPS based on unphased genotype data using a preliminary sample of unrelated subjects with an example from the Multiethnic Cohort Study. Hum Hered. 2003;55:27–36. doi: 10.1159/000071807. [DOI] [PubMed] [Google Scholar]
- 34.Taskinen MR. Quantitative and qualitative lipoprotein abnormalities in diabetes mellitus. Diabetes. 1992;41:12–17. doi: 10.2337/diab.41.2.s12. [DOI] [PubMed] [Google Scholar]
- 35.Taskinen MR. Lipoprotein lipase in diabetes. Diabetes Metab Rev. 1987;3:551–570. doi: 10.1002/dmr.5610030208. [DOI] [PubMed] [Google Scholar]
- 36.Taskinen MR. Diabetic dyslipidemia: from basic research to clinical practice. Diabetologia. 2003;46:733–749. doi: 10.1007/s00125-003-1111-y. [DOI] [PubMed] [Google Scholar]
- 37.Tiffin N, Adie E, Turner F, Brunner HG, van Driel MA, Oti M, Lopez-Bigas N, Ouzounis C, Perez-Iratxeta C, Andrade-Navarro MA, Adeyemo A, Patti ME, Semple CA, Hide W. Computational disease gene identification: a concert of methods prioritizes type 2 diabetes and obesity candidate genes. Nucleic Acids Res. 2006;34:3067–3081. doi: 10.1093/nar/gkl381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tkac I. Metabolic syndrome in relationship to type 2 diabetes and atherosclerosis. Diabetes Res Clin Pract. 2005;68(Suppl 1):S2–S9. doi: 10.1016/j.diabres.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 39.Ukkola O, Savolainen MJ, Salmela PI, von Dickhoff K, Kesaniemi YA. DNA polymorphisms at the lipoprotein lipase gene are associated with macroangiopathy in type 2 (non-insulin-dependent) diabetes mellitus. Atherosclerosis. 1995;115:99–105. doi: 10.1016/0021-9150(94)05504-c. [DOI] [PubMed] [Google Scholar]
- 40.Williams RR, Hunt SC, Hopkins PN, Wu LL, Lalouel JM. Evidence for single gene contributions to hypertension and lipid disturbances: definition, genetics, and clinical significance. Clin Genet. 1994;46:80–87. doi: 10.1111/j.1399-0004.1994.tb04207.x. [DOI] [PubMed] [Google Scholar]
- 41.Yang T, Pang CP, Tsang MW, Lam CW, Poon PM, Chan LY, Wu XQ, Tomlinson B, Baum L. Pathogenic mutations of the lipoprotein lipase gene in Chinese patients with hypertriglyceridemic type 2 diabetes. Hum Mutat. 2003a;21:453–462. doi: 10.1002/humu.9134. [DOI] [PubMed] [Google Scholar]
- 42.Yang W, Huang J, Ge D, Yao C, Duan X, Gan W, Huang G, Zhao J, Hui R, Shen Y, Qiang B, Gu D. Variation near the region of the lipoprotein lipase gene and hypertension or blood pressure levels in Chinese. Hypertens Res. 2003b;26:459–464. doi: 10.1291/hypres.26.459. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.