Abstract
Deciding when an individual with dementia must reduce or stop driving can be a stressful issue for family caregivers. The purpose of this study was to develop a group intervention to assist these caregivers with driving issues and to provide a preliminary evaluation of the comparative effectiveness of this At the Crossroads intervention. Participants were randomized to one of three arms: (1) active intervention (four 2-hour manualized educational/support group meetings; n=31); (2) written materials only (subjects received written materials after a pre-test; n=23); and (3) control (subjects received written materials after a post-test; n=12). Subjects were administered a battery of self-report and interview-based questionnaires at baseline and again two months later. At follow-up, the active intervention group scored significantly better than both other groups on key outcome variables, including self-efficacy, communication, and preparedness. The At the Crossroads caregiver intervention appears to effectively provide education and support needed for caregivers to address driving-related issues with their loved ones.
Keywords: Driving, Dementia, Alzheimer’s Disease, Caregiver, Transportation, Independence, Stress, Support Group, Intervention
Driving is a tremendously complicated and emotionally fraught issue for both patients with dementia and their families. Although Alzheimer’s disease and other degenerative dementias result in the progressive impairment of the cognitive skills necessary for safe driving and ultimately require driving retirement, there is great individual variability in how and when these disorders affect driving abilities (Dubinsky, Stein, & Lyons, 2000; Johansson & Lundberg 1997). Some individuals with mild dementia drive safely for some period of time, while others are unsafe to drive soon after the onset of symptoms (Hunt et al., 1997; Ott et al., 2008). The issue is further complicated by loss of insight that accompanies dementia progression, which may prevent an individual with dementia from making objective decisions about when limiting or stopping driving is necessary (Anstey, Wood, Lord, & Walker, 2005). Self-reports of driving performance in persons with even very mild dementia have been found to be highly inaccurate, potentially due to poor awareness and insight (Adler et al., 1999; Brown et al., 2005; Wild & Cotrell, 2003). The complex issue of driving and dementia is an important public health issue, as there are currently at least five million Americans living with Alzheimer’s disease (the most common cause of degenerative dementia), with this number expected to grow tremendously over the next 30 years as the older population gets larger (Alzheimer’s Association, 2008).
Deciding when an individual with dementia must reduce or stop driving can be one of the most stressful issues faced by individuals with dementia and their families, often described as a struggle with the balance of personal independence and public safety (Fox & Bashford, 1997). Driving also allows individuals to independently stay engaged and connected to friends and family, enjoy an active lifestyle, and spontaneously meet their daily needs (Collia, Sharp, & Giesbrecht, 2003; Marottoli et al., 2000). For many, however, driving is not merely a means of transportation, but, rather, a major aspect of overall independence and autonomy. Therefore, as might be expected, driving cessation is associated with a reduction in out-of-the home activity for the retired driver and may contribute to depression, feelings of isolation, and loneliness (Marottoli et al, 1997, 2000; Ragland et al., 2005). Driving cessation is considered by many to be one of the most significant and deeply personal losses they will face.
Persons with dementia and their family members may look to professionals for advice about driving safety. Due to the lack of routine screening or other mechanisms for detecting poor driving in older persons with cognitive impairment in Departments of Motor Vehicles, physicians are often expected to be the ones to make recommendations to patients and their families about driving cessation. However, physicians often feel that they do not have adequate guidelines or assessments that they can use in the office to determine when patients are unsafe to drive (Carr, Duchek, & Morris, 2000; Friedland, Rudman, Chipman, & Steen, 2006; Perkinson et al., 2005). Additionally, physicians may be concerned about harming the relationship with their patients and damaging the sense of trust, and may worry about legal liability of their recommendations (Friedland et al., 2006). While some guidelines advocate referring patients for a formal driving evaluation, physicians may be hesitant to recommend on-road driving assessments because they are expensive, not readily available outside of urban areas, and not covered by Medicare (Dobbs, Carr, & Morris, 2002). Additionally, the progressive nature of dementia necessitates frequent re-testing, further reducing the feasibility of on-road testing (Dubinsky et al., 2000).
Ultimately, it is likely to be family members or other close care providers who assume the primary responsibility for recognizing and addressing unsafe driving in their loved ones. However, caregivers are left to face this daunting responsibility with few educational resources to assist them on how to initiate conversations, make decisions about driving cessation, and ultimately enforce these decisions (Perkinson et al., 2005). There are several important issues that may prevent family caregivers from actively guiding the transition of their loved one from driver to passenger. These include: fear of angry or dysphoric responses from the driver; feelings of guilt and discomfort in taking away independence from their loved one; anxiety about how transportation needs will be met (especially true for many older female caregivers who traditionally let their spouse do the driving); lack of knowledge about how to determine when driving safety is compromised; and lack of support from other family members in initiating conversations or taking action.
There are several available written publications and web-based materials geared toward caregivers of patients with dementia who are driving, provided by organizations such as the American Automobile Association (AAA), the Alzheimer’s Association, AARP, and several insurance companies. One of the most widely distributed publications that has been disseminated through physician offices and various caregiver support programs, and that has been used in continuing education courses for physicians and other health care professionals (e.g., Meuser, Carr, Berg-Weger, Niewoehner, & Morris, 2006), is the booklet, At the Crossroads: A Guide to Alzheimer’s Disease, Dementia and Driving. The booklet was originally produced and distributed by The Hartford Financial Services Group in 2000, and was based on the findings of a collaborative research by The Hartford and the MIT AgeLab. Although the material found in At the Crossroads and similar publications may be helpful, there have not been any empirical studies of their utility. That is, there is no systematic evidence to show that merely providing these materials to dementia caregivers results in: (1) the caregiver actually reading the material in the first place; and (2) if, indeed, the materials are read, whether they result in any behavior change or other gains. Moreover, it has been found that group-based educational and support interventions for dementia caregivers can be effective in increasing caregivers’ knowledge, reducing their stress and burden, and improving behavior in the dementia patient (e.g., Gallagher-Thompson & Coon, 2007). Therefore, the goals of this project were: (1) to develop a manualized group-based psycho-educational intervention for caregivers of cognitively impaired elders who are still driving; and (2) to provide preliminary efficacy data comparing the group-based intervention to that of providing written materials alone and to routine standard of care.
Method
Overview
This project involved the development of a new caregiver-based psycho-educational group intervention and a subsequent randomized controlled examination of the intervention. Data were collected in 2005 and 2006. The intervention was based on the booklet, At the Crossroads: A Guide to Alzheimer’s Disease, Dementia & Driving, developed for caregivers of individuals with dementia coping with decisions on driving and dementia. The specific educational materials and curriculum used in the intervention were developed by a multidisciplinary team consisting of Alzheimer’s disease researchers and clinicians, gerontologists, and experts in the field of older driver transportation issues. The study was approved by the institutional review boards at the participating educational institutions. All participants provided written informed consent and then received the baseline assessment described below. Participants were then randomized by group to one of three arms: (1) active psycho-educational group intervention (ACT; n = 31); (2) written materials only (WRT; n = 23), in which the subjects received written materials after a baseline assessment; and (3) control (CTL; n = 12), in which the subjects received written materials after a post-test which took place approximately 8 weeks following the baseline assessment. The overall study was designed to address possible threats to validity in this type of caregiver research as outlined by Zarit, Stephens, and Femia (2003).
Subjects
Participants were caregivers who were either a spouse, adult child, or a live-in partner/friend/sibling of a cognitively impaired individual. All care recipients were diagnosed with either mild cognitive impairment (MCI), Alzheimer’s disease, or a related dementia (based on the caregiver’s report only and not confirmed by the physician who provided the diagnosis). At the time of caregiver enrollment, all care recipients were required to have driven an automobile an average of two driving trips per week over the previous month (again as reported by the caregiver participant). Participants were required to have a minimum of four hours face-to-face contact in the previous month with the care recipient, and to have anticipated playing a role in the driving decision. Additional inclusion criteria included: (1) English as primary language; (2) willingness to be considered for all three arms of the study; and (3) if they were to be randomized to the active intervention, had to be available for the scheduled sessions and able to get to the location where they were to be held. Participants were recruited through a variety of methods, including: presentations and distribution of flyers at senior centers, councils on aging, caregiver support groups, and continuing care retirement centers; appearances of study staff on local cable television shows; and stories and announcements in local newspapers, newsletters, and websites.
All participants completed a telephone based screening to determine their eligibility and to address any questions about the research study. The screening resulted in a total sample of 66 caregivers who met all inclusion criteria and remained in the study through post-test. As seen in Table 1, the sample was predominantly female and mostly spouses of male drivers.
Table 1.
Demographic and Other Characteristics of the Study Sample
| Variable | Active Intervention Group (n = 31) | Written Material Only Group (n = 23) | Control Group(n − = 12) |
|---|---|---|---|
| Age | M = 62.8 (sd = 10.9) | M = 68.4 (sd = 12.4) | M = 61.8 (sd = 13.7) |
| Gender | 90% Female | 96% Female | 82% Female |
| Relationship to Driver | Spouse = 74% Adult Child = 23% Other = 3% |
Spouse = 70% Adult Child = 17% Other = 13% |
Spouse = 55% Adult Child = 46% Other = 0% |
Procedure
Participants were administered the baseline assessment by a trained research assistant. Baseline (pre-test) interviews were conducted either in the participant’s home or a convenient location (e.g., a senior center) as requested by the participant. Baseline evaluations were conducted within four weeks of the first scheduled date of the active intervention (if the intervention were to actually be held). Study site was selected prior to baseline by the participant, based on the participant’s geographical location and schedule of the active intervention (if that site were to be assigned to that arm). Sites were all selected prior to group assignment in order to minimize potential bias. Study staff who would have any contact with the participants were kept blind to the site assignment until after all assignments were made. Sites included public libraries, senior centers, and continuing care retirement communities. Sites were then assigned to one of the three treatment arms, with an a priori ratio of 2:2:1 (ACT:WRT:CTL). That is, a site was selected and scheduled as if the active intervention were definitely going to be held there; it was not until after all subjects were assigned to a specific site that the site was then randomized to treatment arm. At the time of baseline evaluation, both the participant and the interviewer were blind to group randomization. There were a total of 14 sites, with 6 sites eventually selected for ACT, 5 sites for WRT, and 3 for CTL. All subjects received a post-test evaluation approximately 8 weeks following baseline (range = 4–12 weeks; M = 7.1, SD = 1.8).
After the baseline visit, participants were informed by mail as to their study arm assignment. Those assigned to the CTL arm were advised that they would be contacted in the future with additional information. Subsequent to the post-test, they received a packet of written materials on driving and dementia and were invited to attend a one-time educational seminar if they so wished. Participants in the WRT arm completed the baseline evaluation and were then given the packet of written information containing: At the Crossroads, a list of additional resources including contact information for the local Alzheimer’s Association, and a listing of local driving evaluation programs. They were also invited to attend a one-time educational seminar on driving and dementia following post-test. Participants in the ACT arm received their baseline evaluation and then attended the four weekly group sessions after which they received their post-test evaluation. To be included in the ACT arm, participants could not miss more than two group sessions. If a participant missed a session, the facilitator contacted the participant and briefly outlined the materials covered during the session.
Description of the Active Intervention
The participants who were enrolled in the psycho-educational intervention groups received four two-hour group educational sessions. The individual group sizes ranged from four to ten caregivers per class, across the total of six different ACT sites. When requested by participants, the care recipient was allowed to come to the site but was not in the room during the group meeting; rather, an additional staff person came to the site and provided companionship for the individual. The same Master’s level research associate facilitated all sessions for all groups. Each group followed the same manualized curriculum for each session. Each session was videotaped (with written permission from participants). These tapes were examined (by members of the research team other than the facilitator) after the study to determine consistency across groups with regard to implementation of the intervention. The intervention was designed to provide caregivers with the knowledge and tools needed for planning, addressing and taking action regarding driving cessation for their loved one. The course incorporated interactive teaching methods, and motivational interviewing practices (Ruback et al., 2005) which were adapted for a group setting. A review of the previous weeks’ material was conducted at the beginning of sessions 2–4. The following provides a brief description of the content of each of the four sessions.
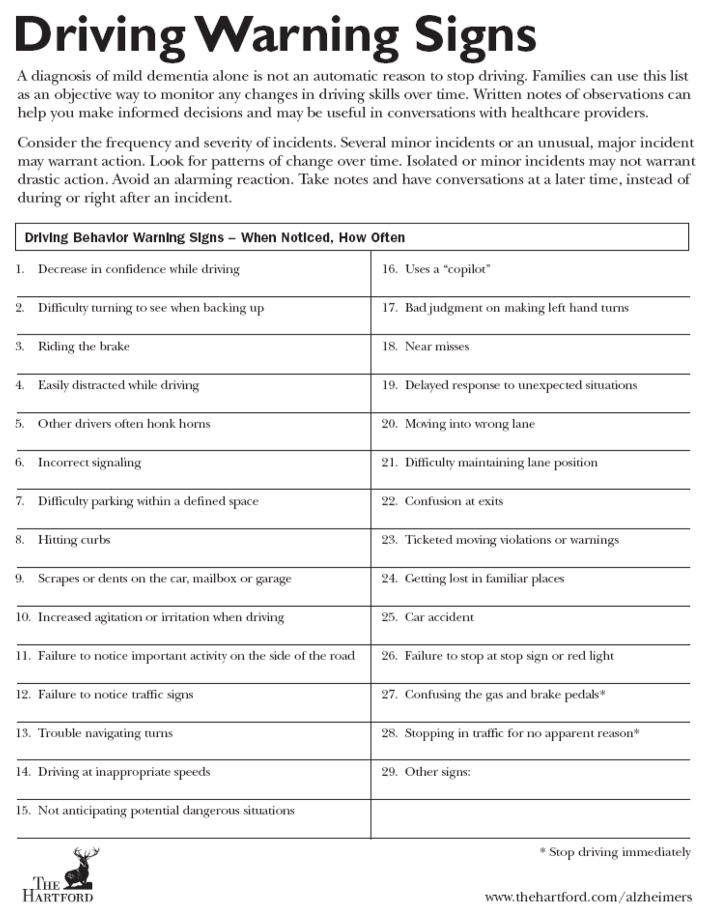
Session one provided an orientation to the course, and background information on the driving and dementia issue. It included definitions of, and basic information on mild cognitive impairment and Alzheimer’s disease. Additionally, information was presented about the cognitive, behavioral, motor, and visual changes associated with brain degeneration in Alzheimer’s disease, and the impact these changes have on specific driving skills. The concept of the decisional balance was introduced and a motivational technique was used to weigh the pros and cons of decisions. The role of impaired insight was discussed, and warning signs of impaired driving were presented to the group. (Figure 1).
Figure 1.
Driving Warning Signs. From At the Crossroads: The Support Group Leaders Kit on Alzheimer’s Disease, Dementia and Driving, produced and distributed by The Hartford Financial Services Group, copyright 2007. Printed by permission of The Hartford Financial Services Group.
Session two included a “tool kit” for the driving transition. Information on conducting guided observations was presented, and the participants engaged in a group activity rating the severity of warning signs of impaired driving for two scenarios. Session two also included a discussion on the caregivers’ circles of support, which encouraged the participants to identify individuals to help with the driving transition. A driving chart was presented, which provided a format for various types of driving activities, as well as trip frequencies and social interactions related to their loved ones’ driving activities. The objective of this activity was to help participants consider the secondary benefits of driving, their relation to quality of life, and possible ways to ensure a continuation of these benefits when the individual ceases driving. Session two also provided information on planning for driving related conversations and a conversation checklist which included an outline for the caregiver to plan for conversations with the driver about the driving issue.
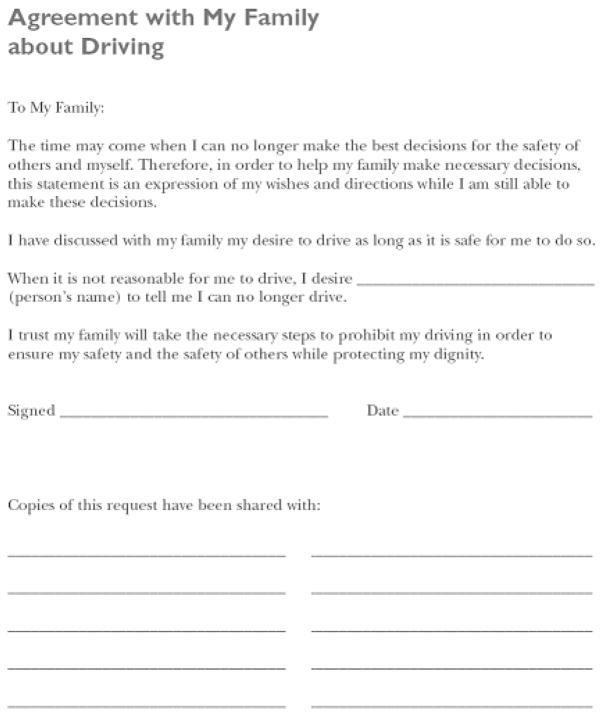
Session three introduced a video case study of a couple who described their experience with the driving and dementia issue; the husband was the individual with dementia. The case study served as a vehicle for modeling the following behaviors to the participants: actively involving the family physician in the process by requesting written documentation stating the husband should not drive, and using opportunities to limit driving. The case study was also intended to inspire and encourage the participants as they became more engaged in taking action around the issue. In this session, participants were given the document “Agreement with My Family about Driving” (Figure 2) and were provided with conversation tips. Information on contacting outside sources of support (health care providers, etc.) and driving evaluation programs was also provided.
Figure 2.
Agreement with My Family about Driving. From At the Crossroads: The Support Group Leaders Kit on Alzheimer’s Disease, Dementia and Driving, produced and distributed by The Hartford Financial Services Group, copyright 2007. Printed by permission of The Hartford Financial Services Group.
Session four included information on last resort techniques, including contacting the department of motor vehicles, and removing the car. Session four also served as a comprehensive review of the main points covered in the previous three weeks, and provided the opportunity for participants to identify and document the next step they wanted to take in the driving transition with their loved one. Finally, certificates were presented to all participants in session four, and a celebration was held to recognize efforts made to date.
At each session, participants were encouraged to complete home assignments between group meetings. Every week, participants were asked to use tracking forms to document any changes in their loved one’s driving and report back on observations. At week one, for the home assignment, the participants were also asked to have a non-threatening driving-related conversation with their loved one (for example, discussing a previous family road trip) in order to begin to broach the topic of driving. At week two, participants were asked to broach the issue of current or future support with a friend or family member. At week three, participants were asked to initiate a conversation with their loved one that they anticipated might be difficult.
Outcome Variables
Primary outcome measures for this preliminary evaluation of the efficacy of the intervention included six aspects of the caregiver’s experience with the driving decision. Because there are no existing published tests with previously explored psychometric properties focusing explicitly on the driving issue, many of the measures were derived specifically for this study and should be considered part of a qualitative analysis, rather than a purely quantitative analysis. The variables of interest for the current study were selected a priori and were administered as part of a larger two-hour interview and test battery examining multiple aspects of caregiving and transportation issues. Each of the six primary outcome measures is briefly described below.
1. Self-Efficacy
A 7-item questionnaire about self-efficacy regarding the ability to handle problems about the loved one’s driving cessation was created, modeled after Fortinsky, Kercher, and Burant’s (2002) Self-Efficacy Questionnaire. Items were rated on a 10-point Likert-type scale with 1 = not at all certain, and 10 = very certain. Sample items included, “How certain are you right now that you can recognize early warning signs of driving problems in your loved one?” and “How certain are you right now that you can take care of the transportation needs of your loved one?”
2. Coping
The Brief COPE scale by Carver (1997) is a commonly used 28-item coping inventory comprising 14 subscales, with each subscale based on two items. The Psychometric properties of the Brief COPE have been described by Carver (1997) and included good reliability and validity with Cronbach alphas ranging from .50 to .90. Among the coping subscales are: Denial, Active Coping, Behavioral Disengagement, Self-distraction, Substance use, Use of emotional support, Use of instrumental support, Venting, Positive reframing, Planning, Humor, Acceptance, Religion, and Self-blame.
3. Stages of Change – Preparation
A two-item scale was created based on the construct of Preparation as one of the stages of behavior change described by Prochaska and Velicer (1997). Both items were rated on a 5-point Likert scale, with 1=Strongly disagree and 5 = Strongly agree. The two items were: (1) “I have been talking with family members/friends about how to address the issue of limiting/stopping driving with my loved one;” and (2) “I have made a plan about how to talk with my loved one about limiting/stopping driving.” The Preparation stage is one of the five stages of change in the Transtheoretical Model of Change (Prochaska & Velicer, 1997), which include: Precontemplation, Contemplation, Preparation, Action, and Maintenance. We chose the Preparation stage as a focus because in this stage, the individual is believed to have already made a commitment to make a change, and has started taking small steps toward action. It would be expected that any participant who would enroll in this study would already be in the Contemplation stage and likely has not taken any action. The goal of the intervention was to begin the process of action-taking.
4. Concern about Relationship
A single, yes-no question was created asking: “Are you ever concerned that your relationship with your loved one will be hurt if you talk about driving? An additional yes-no question was created asking: “Are you ever concerned that your loved one will be angry with you if you talk about not driving?”
5. Communication with Loved One about Driving
Participants were asked (at post-test only) whether or not they had spoken to their loved one about his or her current driving skills or limiting driving.
6. Awareness and Use of “Agreement with My Family about Driving”
In order to assess the awareness of a key component to the At the Crossroads materials, participants were asked whether they were aware of the “Agreement with My Family about Driving,” and, if so, had actually used the Agreement.
Data Analysis
For all continuous outcome variables, analysis of covariance (ANCOVA) was conducted to examine group differences, with the post-test score serving as the dependent variable, assignment to study arm serving as the independent variable, and the pre-test score as covariate. For significant ANCOVA’s, specific between group differences were examined by individual two-group ANCOVAs. For categorical data, cross-tabulations, using frequencies of post-test responses by group membership, were examined by Pearson’s Chi Square. For all initial analyses, an alpha level of 0.05 was employed.
Results
A significant ANCOVA resulted for the Driving-Related Self-Efficacy scale, F (2,60) = 4.42, p < .05. Follow-up tests revealed that the ACT group scored significantly higher than the WRT group which was not different from the CTL group, suggesting that, after the treatment, participants who received the active intervention were higher in their certainty that they would be able to handle driving related issues with their loved ones.
Of the 14 subscales of the Brief COPE, only two demonstrated significant group differences. The Venting subscale ANCOVA was significant, F (2,65) = 3.85, p < .05. Follow-up tests revealed that the ACT group scored significantly higher than the WRT group which was not different from the CTL group, suggesting that participants in the group intervention were more likely to vocalize their unpleasant or negative feelings about the situation than the other groups. The Acceptance subscale ANCOVA was also significant, F (2,65) = 3.22, p<.05. Follow-up tests indicated that the both the ACT and WRT groups were significantly higher than the CTL group on this variable, though the ACT and WRT groups were not different from each other. These results suggest that participants who either received the group intervention or written materials only were more accepting of the situation than those who were in the control arm.
The ANCOVA for the Stages of Change-Preparation scale was significant, F(2,62)=3.80, p < .05). Follow-up ANCOVAs indicated that the ACT group scored significantly higher than the WRT group which was not different from the CTL group, suggesting that participants in the group intervention felt significantly more prepared about how to address the issue of limiting/stopping driving with their loved one, and significantly more likely to have made a plan about how to talk with their loved ones about either limiting or stopping driving than subjects in the other two groups.
On the question about concern that the relationship with the loved one would be hurt if they discuss driving, the overall ANCOVA was significant, F (2,62)=4.54, p<.05. Follow-up ANCOVAs revealed that the ACT group scored significantly higher (i.e., had less concern) than the WRT group and the CTL group which were not significantly different from each other, suggesting that participants in the active group intervention group were less likely than those in either of the other groups to be concerned that their relationship with their loved one would be hurt by discussing the driving issue. The question about concern that the loved one would be angry if they discussed driving also resulted in a significant overall ANCOVA, F (2,63)=4.53, p<.05. Follow-up tests indicated that the ACT group was significantly higher (i.e., less concern) than the WRT group and the CTL group which were not significantly different from each other, again suggesting that the group intervention participants were less likely than those in the other groups to be concerned that their loved one would get angry if they discussed the driving issue.
Ninety percent of the ACT group had spoken with their loved ones about driving during the course of the study. In contrast, 52% of the WRT group and 58% of the CTL group had, X2 (2)=10.23, p<.05.
Overall, 97% of the ACT group reported knowing about the Agreement, with 23% reporting that they had already used it. This is in contrast to the 38% of the WRT group who reported knowing about it and 10% who had used it. None of the control group members had any knowledge of, nor intended to use, the Agreement. The overall Chi Square was significant, X2 (3)=21.31, p<.05.
Discussion
A manualized caregiver group intervention to assist in the driving decision was successfully developed and implemented. Results of a preliminary evaluation of the efficacy of the intervention indicate that, overall, at post-test, participants in the active group intervention scored significantly higher than both other groups on key outcome variables measuring self-efficacy, communication, and preparedness. Specifically, compared with caregivers who received either written materials alone, or routine standard of care (i.e., were not provided with specific information though were able to seek information and support if they so desired), the caregivers who participated in the four-week group intervention: (1) felt more certain they would be able to handle driving related issues with their loved one; (2) felt more prepared about how to address the issue of driving cessation or driving limitations with their loved one; (3) were more likely to have made a plan about how to talk to their loved one about driving cessation or driving limitations; (4) felt less concerned that they would anger their loved one if they talked about not driving; (5) felt less concerned that they would hurt their relationship with their loved one if they talked about driving issues; (6) knew about the “Agreement with My Family About Driving” and, compared to those who knew about it in the written materials only group, were more likely to have used it; (7) had spoken with their loved one about his or her driving; (8) were more likely to vocalize or vent their negativity about the situation; and (9) accepted the reality of the situation and were learning to live with it.
These results suggest that providing caregivers with written materials alone, without an active group intervention, is less useful, and only useful with a small number of individuals. It is possible that those caregivers who are already actively seeking tools and guidance to assist them with the driving decision are likely to read and follow written materials. In contrast, those individuals who are not yet actively seeking assistance or, possibly are in need of additional peer support and interaction, may not utilize or benefit from written materials alone. An important finding from this study is that, although it would appear that all participants were interested in the topic of driving and dementia (by the very act of agreeing to participate), those who were randomized to the control arm did not demonstrate the gains seen in the other arms, and, in particular, the active group intervention.
The results of this study have subsequently been incorporated into a revised edition of At the Crossroads, entitled, At the Crossroads: Family Conversations about Alzheimer’s Disease, Dementia & Driving (available from www.thehartford.com/alzheimers). In addition, a modified kit of all the materials used in the active intervention (though not including a video case) is available for support group leaders and other facilitators dealing with dementia caregivers facing the driving decision. The kit, entitled, At the Crossroads: The Support Group Leaders Kit on Alzheimer’s Disease, Dementia and Driving, is also produced and distributed by The Hartford Financial Services Group (available for order through www.thehartford.com/alzheimers).
Limitations and Future Directions
There are several limitations to the interpretation of these preliminary findings. First, the sample size is relatively small and the control group was substantially smaller than the two other groups. Furthermore, recruitment for the study likely resulted in a sample that is not generalizable. For example, subjects were asked to agree to participate in the study regardless of the group to which they would subsequently be randomized. That is, they had to be motivated to undergo the lengthy evaluations without promise of receiving any formal intervention. The loved ones of the participants in this study also represented a wide range of cognitive impairment, including those with diagnoses of mild cognitive impairment and those with various forms of dementia. The diagnoses and levels of cognitive impairment, however, were only based on the caregiver report. Although this approach likely resulted in a sample that is representative of the caregivers in the community who would participate in this type of intervention, it is not possible to make any inferences regarding the effect of driver characteristics on caregiver response to the intervention. Future studies would benefit from a larger sample size with objective assessments of the drivers’ characteristics.
It is always possible that a group intervention is only as good as the group facilitator, regardless of the content of the sessions. We chose to have only one facilitator conduct all group sessions in order to ensure consistency across groups. The highly manualized content of the sessions should increase the likelihood of similar findings resulting from other facilitators. However, future research would benefit from comparing different facilitators and facilitator characteristics (including peer-facilitators) in order to provide additional guidance for future implementation of the intervention.
It was not the intent of this study to examine the effects of the intervention on driving cessation, per se. That is, the purpose of the intervention is to provide caregivers with the tools to determine when driving cessation should occur and how to go about making that happen in a productive and positive manner. Without directly assessing the driving safety of the cognitively impaired drivers, it is not possible to determine if driving cessation should have occurred during the course of this study. A long-term follow-up of the participants in this study is planned; however, assessment of driving cessation would not be fruitful as it is anticipated that all of the drivers will eventually cease driving due to the progression of the disease. The more important questions to address in future follow-up will be: (1) once driving cessation has occurred, was the caregiver comfortable in the process that led to cessation (i.e., was there adequate support, communication, and planning)?; and (2) did driving cessation occur in a safe and timely fashion, prior to any accident or injury? Future research would also benefit from an evaluation of the feelings, emotional state, and behaviors of the care recipient before, during, and after driving cessation, comparing those whose caregivers participate in the active intervention versus those who do not. The current study did not include any measure of family/caregiver communication prior to the onset of dementia. Because this may have an impact of the ability to address dementia-related driving cessation issues later on, future research would benefit from examining this issue. Finally, it would also be informative to incorporate and study the effect of using a peer-to-peer model in relaying the educational information, as previous research in other settings has shown this to be an extremely effective approach in increasing participant knowledge and benefits (Rummel, Hansen, Helbig, Pitschel, & Kissling, 2005).
The materials developed in this study and available in The Support Group Leaders Kit… could be implemented in a variety of settings with great flexibility. For example, the currently available curriculum is designed to be conducted in three sessions (as opposed to the four used in this study) in order to reduce the time demands on caregivers. These three sessions could be conducted as a stand-alone program or embedded into existing support or psychoeducational groups for early stage dementia caregivers. Materials in the Kit could also be used in a single educational seminar focusing on driving and dementia or used with individual caregivers by geriatricians and other clinicians and service providers. Of course, the efficacy of the implementation of the intervention in ways other than that employed in this study is not known and would be subject to future evaluation.
One important issue pertaining to any caregiver intervention is the fact that many caregivers do not have the flexibility to attend a group intervention because of their need to provide care and supervision to their loved one. Ironically, this is true even in those situations where the cognitively impaired individual continues to drive independently. Furthermore, some caregivers do not feel comfortable in group settings in general, or are reluctant to attend any activity focusing on “driving and dementia” because of fear that, if their loved one found out, he or she would be angry and their relationship would suffer. Finally, many caregivers live in rural areas or are otherwise unable to get to a group activity. For all these reasons, it would be helpful to establish additional methods of implementing this intervention, such as telephone or web-based approaches.
Implications for Gerontology and Geriatrics Education
Older driver safety is a critical issue in today’s society. The impact of driving safety in cognitively impaired elders will grow tremendously over the next few decades as the older population increases and the number of elders with Alzheimer’s disease and other degenerative dementias expands. For example, it is estimated that by the year 2030, there will be almost 8 million older Americans with Alzheimer’s disease (Alzheimer’s Association, 2008). Regardless of the existence or development of regulations, laws, position statements, and practice guidelines regarding driving cessation in people with dementia, the ultimate responsibility and burden regarding driving cessation most often rests on the family caregiver. It is, therefore, imperative that those dealing with dementia caregivers, whether through research, policy making, or clinical practice, be educated about this issue and be provided with tools -- such as those used in the intervention described above – to assist and support caregivers with this difficult and important decision.
Acknowledgments
This work was supported by NIH Grant P30-AG13846 (Boston University Alzheimer’s Disease Core Center). The MIT AgeLab gratefully acknowledges the support of The Hartford Financial Services Group, Inc., and of the US Department of Transportation’s Region I New England University Transportation Center at MIT.
Contributor Information
Robert A. Stern, Associate Professor of Neurology and Co-Director, Alzheimer’s Disease Clinical and Research Program, Boston University School of Medicine, Boston, MA.
Lisa A. D’Ambrosio, Research Scientist, AgeLab, Massachusetts Institute of Technology, Cambridge, MA.
Maureen Mohyde, Director, Corporate Gerontology Group, The Hartford, Southington, CT.
Anastasia Carruth, Research Coordinator, Alzheimer’s Disease Clinical and Research Program, Boston University School of Medicine, Boston, MA.
Beth Tracton-Bishop, Corporate Gerontologist, Corporate Gerontology Group, The Hartford, Southington, CT.
Jennifer C. Hunter, Research Assistant, Alzheimer’s Disease Clinical and Research Program, Boston University School of Medicine, Boston, MA.
Daniel H. Daneshvar, Graduate Assistant, Alzheimer’s Disease Clinical and Research Program, Boston University School of Medicine, Boston, MA.
Joseph F. Coughlin, Director, AgeLab, Massachusetts Institute of Technology, Cambridge, MA.
References
- Adler G, Rottunda S, Christensen K, Kuskowski M, Thuras P. Driving SAFE: Development of a knowledge test for drivers with dementia. Dementia. 2006;5:213–222. doi: 10.1177/1471301206062250. [DOI] [Google Scholar]
- Alzheimer’s Association. Alzheimer’s Disease Facts and Figures. Chicago, IL: Alzheimer’s Association; 2008. [DOI] [PubMed] [Google Scholar]
- Anstey KJ, Wood J, Lord S, Walker JG. Cognitive, sensory and physical factors enabling driving safety in older adults. Clinical Psychology Review. 2005;25:45–65. doi: 10.1016/j.cpr.2004.07.008. [DOI] [PubMed] [Google Scholar]
- Brown LB, Ott BR, Papandonatos GD, Sui Y, Ready RE, Morris JC. Prediction of on-road driving performance in patients with early Alzheimer’s. Journal of the American Geriatrics Society. 2005;53:94–98. doi: 10.1111/j.1532-5415.2005.53017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr DB, Duchek J, Morris JC. Characteristics of motor vehicle crashes of drivers with dementia of the Alzheimer type. Journal of the American Geriatrics Society. 2000;48:100–102. doi: 10.1111/j.1532-5415.2000.tb03023.x. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Collia DV, Sharp J, Giesbrecht L. The 2001 National Household Travel Survey: a look into the travel patterns of older Americans. Journal of Safety Research. 2003;34:461–470. doi: 10.1016/j.jsr.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Dobbs B, Carr DB, Morris JC. Evaluation and Management of the Driver with Dementia. The Neurologist. 2002;8:61–70. doi: 10.1097/00127893-200203000-00001. [DOI] [PubMed] [Google Scholar]
- Dubinsky RM, Stein AC, Lyons K. Practice parameter: Risk of driving and Alzheimer’s disease (An evidence-based review) - Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2000;54:2205–2211. doi: 10.1212/wnl.54.12.2205. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychology and Aging. 2007;22:37–51. doi: 10.1037/0882-7974.22.1.37. [DOI] [PubMed] [Google Scholar]
- Fortinsky RH, Kercher K, Burant CJ. Measurement and correlates of family caregiver self-efficacy for managing dementia. Aging & Mental Health. 2002;6:153–160. doi: 10.1080/13607860220126763. [DOI] [PubMed] [Google Scholar]
- Fox GK, Bashford GM. Driving and dementia: balancing personal independence and public safety. Medical Journal of Australia. 1997;167:406–407. doi: 10.5694/j.1326-5377.1997.tb126643.x. [DOI] [PubMed] [Google Scholar]
- Friedland J, Rudman DL, Chipman M, Steen A. Reluctant regulators: Perspectives of family physicians on monitoring seniors’ driving. Topics in Geriatric Rehabilitation. 2006;22:53–60. [Google Scholar]
- Hunt LA, Murphy CF, Carr D, Duchek JM, Buckles V, Morris JC. Environmental cueing may affect performance on a road test for drivers with dementia of the Alzheimer type. Alzheimer’s Disease and Associated Disorders. 1997;11(Suppl 1):13–16. doi: 10.1097/00002093-199706001-00004. [DOI] [PubMed] [Google Scholar]
- Johansson K, Lundberg C. The 1994 International Consensus Conference on Dementia and Driving: A brief report. Alzheimer Disease & Associated Disorders. 1997;11(Supplement 1):62–69. doi: 10.1097/00002093-199706001-00013. [DOI] [PubMed] [Google Scholar]
- Marottoli RA, Mendes de Leon CF, Glass TA, Williams CS, Cooney LM, Berkman LF, Tinetti ME. Driving cessation and increased depressive symptoms: Prospective evidence from the New Haven EPESE. Journal of the American Geriatrics Society. 1997;45:202–206. doi: 10.1111/j.1532-5415.1997.tb04508.x. [DOI] [PubMed] [Google Scholar]
- Marottoli RA, Mendes de Leon CF, Glass TA, Williams CS, Cooney LM, Berkman LF. Consequences of driving cessation: Decreased out-of-home activity levels. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2000;55B:S334–S340. doi: 10.1093/geronb/55.6.s334. [DOI] [PubMed] [Google Scholar]
- Meuser TM, Carr DB, Berg-Weger M, Niewoehner P, Morris JC. Driving and dementia in older adults: Implementation and evaluation of a continuing education project. The Gerontologist. 2006;46:680–687. doi: 10.1093/geront/46.5.680. [DOI] [PubMed] [Google Scholar]
- Ott BR, Heindel WC, Papandonatos GD, Festa EK, Davis JD, Daiello LA, Morris JC. A longitudinal study of drivers with Alzheimer’s disease. Neurology. 2008;70:1171–1178. doi: 10.1212/01.wnl.0000294469.27156.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkinson MA, Berg-Weger ML, Carr DB, Meuser TM, Palmer JL, Buckles VD, et al. Driving and dementia of the Alzheimer type: Beliefs and cessation strategies among stakeholders. The Gerontologist. 2005;45:676–685. doi: 10.1093/geront/45.5.676. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. American Journal of Health Promotion. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Ragland DR, Satariano WA, MacLeod KE. Driving cessation and increased depressive symptoms. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2005;3A:M399–M403. doi: 10.1093/gerona/60.3.399. [DOI] [PubMed] [Google Scholar]
- Rummel CB, Hansen WP, Helbig A, Pitschel-Walz G, Kissling W. Peer-to-peer psychoeducation in schizophrenia: A new approach. Journal of Clinical Psychiatry. 2005;66:1580–1585. doi: 10.4088/jcp.v66n1214. [DOI] [PubMed] [Google Scholar]
- Wild K, Cotrell V. Identifying driving impairment in Alzheimer’s disease: A comparison of self and observer reports versus driving evaluation. Alzheimer’s Disease and Associated Disorders. 2003;17:27–34. doi: 10.1097/00002093-200301000-00004. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Stephens MAP, Femia EE. The validities of research findings: The case of interventions with caregivers. Alzheimer’s Care Quarterly. 2003;4:216–228. [Google Scholar]