Abstract
Researchers have hypothesized that pain catastrophizing has a social function. Although work has focused on the catastrophizing of individuals with chronic pain (ICPs), little is known about the pain catastrophizing of their significant others. The purpose of this study was to test the validity of a revised version of the original PCS [Sullivan MJL, Bishop S, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess 1995; 7: 432–524.] in which individuals were instructed to report on their own catastrophizing about their significant other’s pain. In Study 1, a confirmatory factor analysis was conducted to determine the factor structure of the PCS-Significant Other (PCS-S) in a diverse sample of university undergraduates (n=264). An oblique second-order 3-factor model with two cross-loadings provided the best fit and this model was invariant across gender and racial groups. This factor structure was cross-validated in Study 2 with a second sample of university undergraduates (n=213). Results indicated that the 3-factor structure with two cross-loadings was a viable model of significant others’ pain catastrophizing across gender and racial groups. In Study 3, this factor structure was replicated and the content validity of the PCS-S was examined in a sample of adult ICPs and their spouses (n=111). Spouse catastrophizing was related to ICP pain severity and interference as well as both spouses’ depressive symptoms. In addition, ICPs were at a greater risk for psychological distress when both spouses had higher levels of catastrophizing. The PCS-S has the potential to be a useful and valid measure of pain catastrophizing in the significant others of ICPs.
Keywords: Pain catastrophizing scale, ICP, Confirmatory factor analyses, Spouses
1. Introduction
Pain catastrophizing is an exaggerated, negative focus on pain and is related to psychological distress, pain severity, and other negative outcomes in pain samples (Affleck et al., 1999; Cano, 2004; Keefe et al., 1989; Turner et al., 2000, 2002, 2004). Pain catastrophizing may serve a communal coping function such that individuals with chronic pain (ICPs) catastrophize about their pain to elicit support from others (Sullivan et al., 2001a; Thorn et al., 2003). Research has supported this hypothesis (Cano, 2004; Giardino et al., 2003; Keefe et al., 2003; Sullivan et al., 2004). Significant others living or interacting with ICPs may also catastrophize about ICPs’ pain. Indeed, health problems in one spouse can cause increased worry and psychological distress in the healthy spouse (Coyne and Smith, 1991; Davis-Ali et al., 1993). In turn, catastrophizing cognitions could translate into behaviors related to support provision. For instance, significant others who catastrophize about their partners’ pain may desire more control over the ICPs’ health behaviors or engage in more advice-giving. Healthy spouses’ own beliefs or attitudes are important factors in determining the tactics they use to influence health-related behavior (Butterfield and Lewis, 2002). Pain catastrophizing in significant others might also be related to both partners’ psychological distress, just as pain catastrophizing is related to distress in ICPs. For instance, catastrophizing spouses may increase the likelihood that both spouses maintain their focus on the ICP’s pain, thereby increasing hopelessness and distress about the illness and its impact on their relationship.
Therefore, it is wise to consider assessing cognitions such as pain catastrophizing in the significant others of ICPs. Other researchers have adapted measures to assess pain and disability in the significant others of ICPs (e.g. Kerns and Rosenberg, 1995; Romano et al., 1989) and research has confirmed that significant other perceptions are important factors in ICP and spouse outcomes (Cano et al., 2004; Cremeans-Smith et al., 2003; Geisser et al., 2005; Riemsma et al., 2000; Romano et al., 1989). Similar research on spouse catastrophizing would enhance the theoretical understanding of the social context of pain catastrophizing. In addition, this research could inform clinical work by identifying significant others who might benefit from cognitive-behavioral therapy.
To this end, we conducted three studies to investigate the usefulness of the significant other version of the Pain Catastrophizing Scale (PCS-S). In the first study, we conducted a factor analysis to determine the factor structure of the PCS-S. We cross-validated the factor structure in the second study. In both studies, we tested factor structure invariance across gender and racial/ethnic groups. Finally, in the third study, we examined the correlates of pain catastrophizing in a community sample of ICPs and their spouses. Another purpose of the third study was to determine whether spouse catastrophizing was independently related to both spouses’ well-being. If so, a case could be made for further investigation of spouse catastrophizing as an important variable in the pain experience.
2. Study 1
2.1. Method
2.1.1. Participants
The sample consisted of 264 undergraduate students taking psychology classes in Fall 2004 at a Midwestern university in an urban area. The sample was predominately female (77.3%, n=204) and participants were 20.7 (SD 5.7) years old on average. The sample was ethnically diverse with 55.7% (n=147) of the participants self-identifying as Caucasian, 26.5% as African-American, 4.0% as Hispanic, 3.4 and 3.0% as Asian or Middle Eastern, respectively, and 7.2% of participants reporting other ethnicities or as multiracial. All participants reported being in a romantic relationship with the majority reporting dating in an exclusive relationship (64.8%, n=171). Thirty-four (12.9%) of the participants reported that they had chronic pain. When reporting on chronic pain in others, 11.9% (n= 31) of participants reported that their romantic partner had chronic pain and 51.5% (n=135) of participants reported similar problems in family or friends.
2.1.2. Measures
An adapted version of the pain catastrophizing scale (Sullivan et al., 1995) was used in this study to assess the extent to which significant others catastrophize about their romantic partner’s pain. The opening sentence of the measure was changed from ‘When I feel pain…’ to ‘When my significant other feels pain…’ When appropriate, individual items were also changed to reflect the respondent’s catastrophizing about their significant other’s pain. Participants responded to each item using a Likert-type scale from 0 (‘not at all’) to 4 (‘all the time’). Participants are not directed to a particular time frame but the wording gives the impression that participants are to report on current levels of pain catastrophizing. The significant other version of the Pain Catastrophizing Scale assesses the same three dimensions of pain catastrophizing as the original scale. These three dimensions are magnification (three items; e.g. ‘I wonder whether something serious may happen’), rumination (four items; e.g. ‘I keep thinking about how much it hurts’), and helplessness (six items; e.g. ‘There is nothing I can do to reduce the intensity of the pain’).
In addition to the PCS-S, participants provided demographic information, including information about gender, ethnicity, and age.
2.1.3. Procedure
All participants consented to be in this study. The undergraduate students participated in this study in one of two ways. Most participants (n=240) completed the study as part of a mass screening that occurs each semester in all Introduction to Psychology (PSY 101) courses. The remaining participants responded to advertisements in other psychology classes. All participants received extra credit in their psychology classes upon completion of the study.
2.2. Results
2.2.1. Data analysis plan
We conducted a series of confirmatory factor analyses (CFA) to determine the model that best fit the factor structure of the PCS-S. CFA was chosen over exploratory factor analysis (EFA) because there is consistent evidence supporting the factor structure of the PCS in adults (Crombez et al., 2003; Osman et al., 1997, 2000; Sullivan et al., 1995; Van Damme et al., 2002) and in children (PCS-child version; Crombez et al., 2003). There is no reason to think that the factor structure of pain catastrophizing would be different for significant others. EFA, in contrast, is commonly used when the associations between latent factors and observed variables are unknown.
Several models were tested based on existing factor analytic studies of the PCS (Crombez et al., 2003; Osman et al., 1997, 2000; Sullivan et al., 1995; Van Damme et al., 2002). Model 1 was a 1-factor model with 13 indicators of a single latent factor of pain catastrophizing. Model 2 was an oblique 2-factor model according to Osman et al. (1997). In this model, seven items loaded onto a magnification-helplessness latent factor and six items loaded onto a rumination latent factor. Model 3 was an oblique 3-factormodel put forth by Sullivan et al. (1995) and supported by others (Crombez et al., 2003; Osman et al., 1997, 2000; Sullivan et al., 1995; Van Damme et al., 2002). The rumination factor consisted of four items, the magnification factor consisted of three items, and the helplessness factor consisted of six items. Models 4 and 5 included cross-loadings of items (items that loaded onto two factors) as described below. Model 6 was similar to Model 5 except that it included a second-order factor of pain catastrophizing that accounted for the covariance in the three first-order factors of rumination, magnification, and helplessness. Crombez et al. (2003) and Osman et al. (2000) found support for this model. We also examined invariance in the factor structure and factor loadings of the best fitting model across gender and racial groups. Each model was tested using the Amos 5.0 program. Finally, we examined the descriptive statistics and reliability of the resulting factors.
2.2.2. Confirmatory factor analysis
Multiple fit statistics for models 1–3 are displayed in the Study 1 section of Table 1. Model 2 was a significantly better fitting model than Model 1, Δχ2 (2)=33.96, P<.001 and Model 3 was a significantly better fitting model than Model 2, Δχ2 (2)=78.83, P<.001 and Model 1, Δχ2 (2)=112.78, P<.001. Of these three models, Model 3 demonstrated the best fit but did not achieve acceptable fit (i.e. Comparative Fit Index [CFI]≥.90, Tucker–Lewis Index [TLI]= close to .95; Normed Fit Index [NFI]≥.90; Root Mean Squared Error of Approximation [RMSEA]≤.08; (Byrne, 2001)).
Table 1.
Goodness of fit statistics for confirmatory factor analyses of models tested in Studies 1–3
| Model | ML x2 | df | CFI | TLI | NFI | RMSEA |
|---|---|---|---|---|---|---|
| Study 1 (n=264) | ||||||
| 1. Single latent factor | 319.09 | 65 | .82 | .79 | .79 | .12 |
| 2. Oblique two factor | 285.13 | 64 | .85 | .81 | .81 | .12 |
| 3. Oblique three factor | 206.31 | 62 | .90 | .87 | .86 | .09 |
| 4. Oblique three factor with item 1 cross-loaded | 151.55 | 61 | .94 | .92 | .90 | .08 |
| 5. Oblique three factor with items 1 and 9 cross-loaded | 123.74 | 60 | .96 | .94 | .92 | .06 |
| 6. Second-order factor | 123.74 | 60 | .96 | .94 | .92 | .06 |
| Study 2 (n=213) | ||||||
| 1. Single latent factor | 355.36 | 65 | .82 | .78 | .79 | .16 |
| 2. Oblique two factor | 316.86 | 64 | .84 | .81 | .81 | .14 |
| 3. Oblique three factor | 218.48 | 62 | .90 | .87 | .87 | .11 |
| 4. Oblique three factor with item 1 cross-loaded | 165.79 | 61 | .90 | .92 | .94 | .09 |
| 5. Oblique three factor with items 1 and 9 cross-loaded | 145.82 | 60 | .95 | .93 | .91 | .08 |
| 6. Second-order factor | 145.82 | 60 | .95 | .93 | .91 | .08 |
| Study 3 (n=111) | ||||||
| 1. Single latent factor | 260.42 | 65 | .71 | .65 | .65 | .16 |
| 2. Oblique two factor | 222.94 | 64 | .76 | .71 | .70 | .15 |
| 3. Oblique three factor | 149.54 | 62 | .87 | .84 | .80 | .11 |
| 4. Oblique three factor with item 1 cross-loaded | 117.20 | 61 | .92 | .89 | .84 | .09 |
| 5. Oblique three factor with items 1 and 9 cross-loaded | 105.23 | 60 | .93 | .91 | .86 | .08 |
| 6. Second-order factor | 105.23 | 60 | .93 | .91 | .86 | .08 |
ML, maximum-likelihood; CFI, comparative fit index; TLI, Tucker–Lewis index; NFI, normed fit index; RMSEA, root mean squared error of approximation.
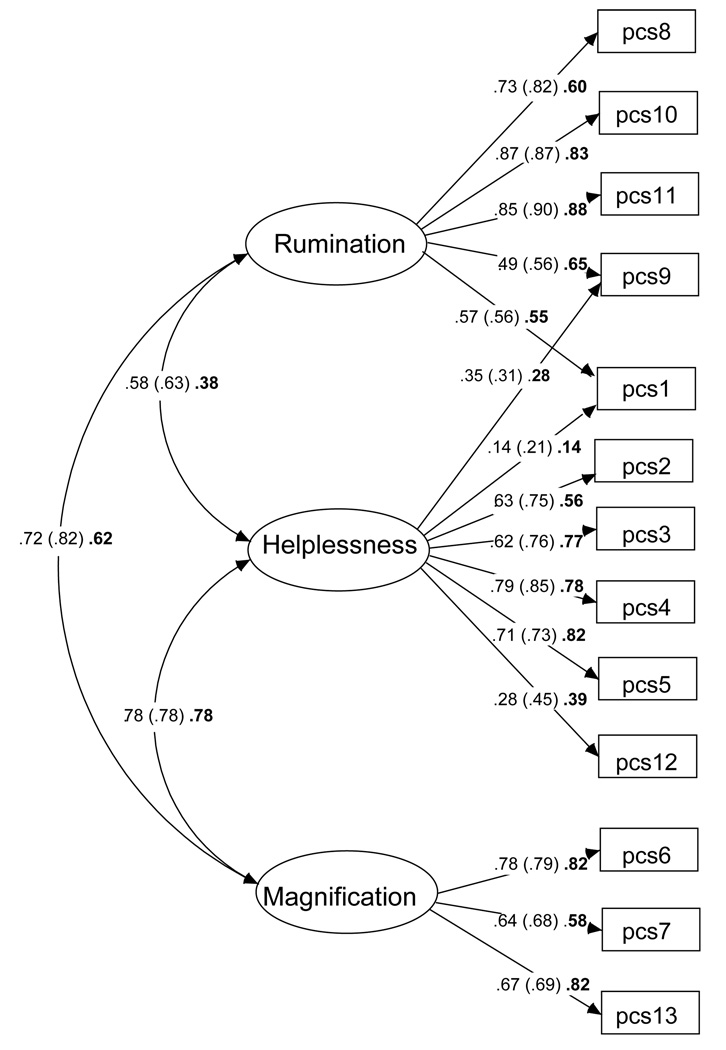
Because of the poor fit, we examined modification indices, standardized covariance residuals, and critical ratios for differences between parameters to determine likely misspecification in the model and potential cross-loadings. First, the standardized covariance residuals indicated that the correlation between item 1 (‘I worry all the time about whether his/her pain will end’) and each of the four rumination items (i.e. 8–11) was substantially underestimated. Modification indices also provided strong evidence for an association of item 1 with items 8, 10, and 11. The wording of the item also suggests a ruminative helplessness in the significant other. Existing evidence also showed that helplessness items may cross-load onto the rumination factor (Osman et al., 1997). Therefore, item 1 was allowed to cross-load onto rumination in Model 4 (see Table 1). Model fit improved significantly from Model 3 to Model 4, Δχ2 (1)=44.76, P<.001. However, further examination of the modification indices and residuals indicated another overlap between rumination and helplessness, this time between a rumination item (item 9: ‘I can’t seem to keep it out of my mind’) and the helplessness factor. Again, the wording of the item appears to tap both rumination as well as a sense of helplessness in the participant to be able to do anything about their significant other’s pain. Moreover, evidence suggests that rumination items cross-load onto the helplessness factor (Sullivan et al., 1995). Therefore, item 9 was also allowed to cross-load onto helplessness in Model 5, which resulted in a model with adequate fit (see Table 1). Note that once models are modified and tested in this way, they are exploratory in nature. A comparison of Models 4 and 5, indicated a significant improvement in fit, Δχ2 (1)=27.81, P<.001. The second-order model (Model 6) fit the data as well as Model 5, which is similar to the finding in the Crombez et al. (2003) study of the child version of the scale. The standardized coefficients (i.e. factor loadings) and correlations between the three factors are presented in Fig. 1. We present the oblique 3-factor model (Model 5) because there was no improvement in fit from Model 5 to the second-order factor model (Model 6).
Fig. 1.
Oblique 3-factor model of the PCS-S displaying standardized regression coefficients (i.e. factor loadings). Study 1 coefficients are presented first. Study 2 coefficients are presented within parentheses. Study 3 coefficients are presented in bold text.
2.2.3. Invariant factor structure
We conducted further analyses to determine whether the oblique 3-factor model was invariant across gender and racial groups. The factor loadings and inter-correlations were constrained to be equal across groups. The multi-group analysis showed that the model fit the data equally well for male and female participants, χ2 (138)=219.81, P<.0001; CFI=.95; TLI=.94; NFI=.87; RMSEA=.05.
Next, the multi-group analysis was conducted to test whether the model was adequate for both Caucasians (n=147) and African-Americans (n=70). Participants of other ethnic groups (n=19; e.g. Hispanic, Arabic) were not included because their racial identification was not collected and participants of other races (n=28; e.g. Native American, Asian) were not included because there were too few in the sample to allow for meaningful analysis. The analysis for race showed that the model fit was acceptable for both Caucasians and African-Americans, χ2 (138)=212.08, P<.0001; CFI=.94; TLI=.94; NFI=.85; RMSEA=.05. When this analysis was repeated comparing Caucasian and all other participants (i.e. African-American, and other racial and ethnic groups), the results were similar, χ2 (138)=224.92, P<.0001; CFI=.94; TLI=.93; NFI=.86; RMSEA=.05.
In sum, the multi-group analyses demonstrated that the 3-factor oblique model was invariant across genders and racial groups. Across groups, the factors of the PCS-S were stably inter-correlated and the items were stable for their loadings on the rumination, helplessness, and magnification factors.
2.2.4. Descriptive statistics and demographic analyses
The PCS-S subscales had adequate to excellent inter-item reliabilities across genders and racial groups (see Table 2 and Table 3). Reliabilities were calculated based on the primary loadings of items so that results could be compared to previous studies. That is, item 1 was included in the reliability analyses for the helplessness factor whereas item 9 was included in the reliability analyses for the rumination factor.
Table 2.
Mean significant other pain catastrophizing total and subscale scores for men and women
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| M | SD | α | M | SD | α | |
| Study 1 | Men (n=60) | Women (n=204) | ||||
| Rumination | 8.73 | 4.20 | .87 | 8.66 | 4.47 | .86 |
| Magnification | 5.45 | 2.85 | .73 | 5.37 | 3.17 | .74 |
| Helplessness | 7.13 | 3.74 | .62 | 7.16 | 4.38 | .77 |
| Total PCS-S score | 21.32 | 9.40 | .87 | 21.19 | 10.53 | .90 |
| Study 2 | Men (n=60) | Women (n=153) | ||||
| Rumination | 8.47 | 3.96 | .88 | 8.61 | 4.85 | .91 |
| Magnification | 5.33 | 2.90 | .73 | 5.35 | 3.33 | .77 |
| Helplessness | 7.32 | 4.94 | .84 | 7.58 | 5.06 | .83 |
| Total PCS-S score | 21.12 | 10.65 | .92 | 21.55 | 11.86 | .92 |
| Study 3 | Men (n=67) | Women (n=44) | ||||
| Rumination | 10.09 | 3.65 | .83 | 9.36 | 4.06 | .87 |
| Magnification | 5.42 | 3.22 | .75 | 5.16 | 3.17 | .81 |
| Helplessness | 7.43 | 4.38 | .76 | 7.61 | 4.84 | .81 |
| Total PCS-S score | 22.94 | 9.60 | .88 | 22.14 | 10.46 | .91 |
PCS-S, pain catastrophizing scale-significant other version.
Table 3.
Mean significant other pain catastrophizing total and subscale scores for African-Americans and Caucasians
| African-Americans |
Caucasians |
|||||
|---|---|---|---|---|---|---|
| M | SD | α | M | SD | α | |
| Study 1 | African-Americans (n=70) | Caucasians (n=147) | ||||
| Rumination | 9.33 | 4.38 | .81 | 8.11 | 4.55 | .90 |
| Magnification | 5.43 | 3.43 | .73 | 5.29 | 2.89 | .71 |
| Helplessness | 7.06 | 4.39 | .74 | 6.99 | 4.29 | .77 |
| Total PCS-S score | 21.81 | 10.40 | .87 | 20.39 | 10.51 | .91 |
| Study 2 | African-Americans (n=72) | Caucasians (n=101) | ||||
| Rumination | 8.89 | 4.72 | .87 | 8.04 | 4.46 | .92 |
| Magnification | 5.10 | 3.15 | .66 | 5.30 | 3.22 | .81 |
| Helplessness | 7.72 | 5.10 | .81 | 6.88 | 4.62 | .83 |
| Total PCS-S score | 21.71 | 11.30 | .90 | 20.22 | 11.21 | .93 |
| Study 3 | African-Americans (n=70) | Caucasians (n=147) | ||||
| Rumination | 10.81 | 3.91 | .83 | 9.07 | 3.82 | .86 |
| Magnification | 5.52 | 3.81 | .83 | 5.03 | 2.72 | .69 |
| Helplessness | 8.38 | 5.24 | .80 | 6.83 | 4.09 | .76 |
| Total PCS-S score | 24.71 | 11.00 | .89 | 20.93 | 9.26 | .89 |
PCS-S, pain catastrophizing scale-significant other version.
T-tests were conducted between male and female and between Caucasian and African-American participants to determine whether there were any group differences. There were no significant differences between men and women on the subscales or total scores of the PCS-S. Similarly, there were no differences between Caucasian and African-Americans, with the exception of a trend on rumination with African-Americans reporting more rumination (M=9.33, SD=4.38) than Caucasians (M=8.11, SD=4.55), t (215)=1.87, P<.06. Age was significantly correlated negatively with each of the three subscales, rs (261)=−.12 to −.23, Ps<.01, as well as with the total pain catastrophizing score, r (261)=−.20, P<.01. Three participants did not complete age information so the sample size was reduced for these correlations.
2.2.5. Discussion
Study 1 demonstrated that a 3-factor model with two cross-loadings provided the best fit to the PCS-S data. In addition, the factor structure was invariant across gender and racial groups. There were no significant differences between gender and racial groups in levels of catastrophizing but age was negatively correlated with each PCS-S subscale as well as the total pain catastrophizing score. Note that factor analyses are considered exploratory once the models are modified to achieve a better fit as in the case of Models 4–6. Therefore, another sample was recruited to determine whether the 3-factor structure with cross-loadings could be replicated.
3. Study 2
3.1. Method
The purpose of Study 2 was to replicate the factor structure of Model 5 (i.e. oblique three factor model with two cross-loadings) presented in Study 1. Recall that Model 5 was chosen as the model of choice because there was no improvement in fit from Model 5 to Model 6 (i.e. the second-order factor model). The participants in Study 2 were 213 undergraduate students taking Psychology 101 classes in Winter 2005 at the same university as in Study 1. The sample was predominately female (71.8%, n=153) and participants were 21.0 (SD 4.9) years old on average. The sample was ethnically diverse with 47.4% (n=101) of the participants self-identifying as Caucasian, 33.8% (n=72) as African-American, 2.8% (n=6) as Hispanic, 4.7% (n=10) and 4.7% (n=10) as Asian or Middle Eastern, respectively, and 6.6% (n=14) of participants reporting other ethnicities or as multi-racial. The majority of the sample reported dating in an exclusive relationship (56.6%, n=120). Thirty-eight (17.8%) of the participants reported that they have chronic pain. When reporting on chronic pain in others 11.5% (n=24) of participants reported that their romantic partner had chronic pain and 49.1% (n=104) of participants reported similar problems in family or friends.
3.1.1. Measures and procedure
The measures and procedure were the same as in Study 1 with the exception that all participants were undergraduates completing the mass screening procedure.
3.2. Results
3.2.1. Confirmatory factor analysis
The same six models that were tested in Study 1 were tested with this calibration sample. The Study 2 section of Table 1 demonstrates that the model fit was acceptable for Models 5 and 6, models that included the cross-loadings of items 1 and 9. As in Study 1, the fit of Model 5 was significantly better than that of Model 4, Δχ2 (1)=19.97, P<.001. Model 5 is displayed in Fig. 1. The standardized coefficients for the oblique 3-factor models in Study 2 are presented within the parentheses.
3.2.2. Invariant factor structure
We conducted multi-group analyses to determine whether the oblique 3-factor model was invariant across gender and racial groups. The factor loadings and inter-correlations were constrained to be equal across groups. The multi-group analysis showed that the model fit the data equally well for male and female participants, χ2 (138)=280.52, P<.0001; CFI=.92; TLI=.90; NFI=.85; RMSEA=.07.
Similarly, the analysis for race showed that the model fit was acceptable for both Caucasians (n=101) and African- Americans (n=72), χ2 (138)=272.18, P<.0001; CFI=.90; TLI=.89; NFI=.82; RMSEA=.08. When this analysis was repeated comparing Caucasian and all other participants (i.e. African-American, and other racial and ethnic groups), the results were similar, χ2 (138)=268.74, P<.0001; CFI=.92; TLI=.92; NFI=.85; RMSEA=.07.
As in Study 1, the multi-group analyses in Study 2 demonstrated that the 3-factor oblique model was invariant across genders and racial groups.
3.2.3. Descriptive statistics and demographic analyses
The PCS-S subscales again had acceptable to excellent inter-item reliabilities across genders and racial groups (see Table 2 and Table 3). Reliabilities were calculated based on the primary loadings of items so that results could be compared to Study 1 as well as previous studies. Item 1 was included in the reliability analyses for the helplessness factor and item 9 was included in the reliability analyses for the rumination factor.
T-tests were conducted to determine whether there were any group differences. Similar to Study 1 there were no significant differences between men and women or between Caucasians and African-Americans. Age was again significantly correlated negatively with each of the three subscales, rs (211)=K.24 to −.26, Ps<.01, as well as with the total pain catastrophizing score, r (211)=−.28, P<.01. Two participants were excluded from the correlational analysis involving age because they did not provide their age information.
3.2.4. Discussion
This study confirmed that the 3-factor model with two cross-loadings provided an adequate fit to the PCS-S data. As in Study 1, the model was invariant across gender and racial groups and there were no significant differences across groups in mean levels of catastrophizing. The next step was to test to PCS-S in a sample of married couples in which one spouse has chronic musculoskeletal pain to determine whether the PCS-S is associated with ICP and spouse outcomes.
4. Study 3
4.1. Method
4.1.1. Participants
An ethnically diverse sample of couples was recruited through newspaper advertisements in the Detroit metropolitan area for a larger study of couples and chronic pain (n=111). A subset of the ICP participants was described in Cano (2004). ICPs and their spouses reported diverse ethnic and racial backgrounds (55.0 and 54.1% Caucasian, 36.9 and 37.8% African-American, respectively; 8.1% other racial/ethnic groups such as Native American, Asian, and Hispanic/Latino). ICPs were predominately female (n=67, 60.4%) and were 52.98 (SD=13.42) years old on average, while their spouses were 53.36 (SD=13.64) years old, on average. The couples had been married a mean of 20.59 (SD=16.45) years. ICPs and their spouses had completed an average of 14.17 (SD=2.68) and 14.37 (SD=2.67) years of education, respectively. The couples reported an average income of $56,022 (SD=$34,516). The ICPs reported mean pain duration of 114 (SD=125) months. The most common location for ICPs to experience pain was the lower back. Eighty-six percent (n=96) had received a diagnosis for the pain, and of those who had received a diagnosis the most prevalent pain problem was Osteoarthritis (n=44, 45.8%).
4.1.2. Measures
ICPs were administered the PCS (Sullivan et al., 1995) whereas their partners were administered the PCS-S to assess pain catastrophizing. Inter-item reliabilities for the PCS and PCS-S subscales were adequate to excellent for both sets of spouses (ICPs subscale αs=.78–.91; spouse αs=.77–.84). Similarly, the inter-item reliabilities for the total scale scores were excellent (ICP α=.95; spouses α=.89). The three subscales were highly inter-correlated for each group of spouses (ICPs rs=.73–.78, Ps<.001; healthy spouses rs=.53–.70, Ps<.001). Means and standard deviations on PCS and PCS-S are presented in Table 4.
Table 4.
Means and standard deviations of pain catastrophizing subscales and total scores for ICPs and their spouses
| ICPs |
Spouses |
t | |||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Rumination | 8.01 | 4.90 | 9.80 | 3.82 | −3.00* |
| Magnification | 4.21 | 3.33 | 5.32 | 3.19 | −3.09* |
| Helplessness | 7.64 | 6.30 | 7.50 | 4.55 | .21 |
| Total PCS | 19.03 | 13.22 | 22.62 | 9.90 | −2.80* |
P<.01; ICPs, individuals with chronic pain; PCS, pain catastrophizing scale.
Both spouses’ depressive symptoms were assessed with the Mood and Anxiety Symptom Questionnaire (MASQ) (Watson and Clark, 1991). The MASQ assesses depressive and anxiety symptoms and has a stable factor structure across community and patient groups including chronic pain samples (Geisser et al., in press; Watson et al., 1995a,b). For the purposes of this study, we used the nonspecific depression score (12 items) consisting of diffuse symptoms of depression (e.g. felt sad, felt discouraged). Participants were asked to focus on the past week including the day of participation and reported how much they have felt each symptom item on a Likert-type scale from 1 (‘not at all’) to 5 (‘extremely’). Inter-item reliability of this subscale was excellent for both partners (pain spouses α=.91; healthy spouses α=.90). Mean scores for patients and spouses were 22.58 (SD=9.00) and 20.14 (SD=7.80). The inter-item reliabilities for the current sample are comparable to those reported in Watson et al. (1995a). In addition, the current sample’s means were comparable to Watson et al. (1995a)’s student and adult samples, but were slightly lower than mean depressive symptoms of individuals seeking treatment for substance abuse.
Pain severity and interference were assessed with the Multidimensional Pain Inventory Patient and Spouse versions (Kerns and Rosenberg, 1995; Kerns et al., 1985). ICPs reported on their own pain severity and interference while their partners reported their perceptions of the ICPs’ pain severity. The pain severity scale consists of three items and the interference scale consists of nine items. Participants were directed to report on current pain and interference although no specific timeframe was used. Participants responded on a 0 (e.g. ‘no pain,’ ‘no change’) to 6 (e.g. ‘extreme pain’, ‘extreme change’) Likert-type scale. The reliabilities of both subscales were excellent (ICP pain severity and interference αs=.80 and .84, respectively; spouse pain severity and interference αs=.85 and .93, respectively).
4.1.3. Procedure
Potential participants were screened on the telephone to determine their eligibility. Eligible participants were couples in which at least one spouse had a current chronic musculoskeletal pain problem of at least a 6-month duration. Couples were also required to be married and living together. Exclusionary criteria included presence of psychotic symptoms, presence of cognitive impairment as assessed with a phone version of the Mini-Mental Status Examination (Folstein et al., 1975), and presence of a terminal illness. Eligible couples attended a 3-h lab session and completed consent forms, surveys, interviews, and videotaped interactions as part of the larger study. Couples were paid $100 upon completion of the study.
4.2. Results
4.2.1. Data analysis plan
First, a series of factor analyses were conducted to determine whether the factor structure and model fit was similar to those of Studies 1 and 2. The relationships between demographic variables and PCS-S scores were examined. We then conducted within-couples analyses (i.e. paired samples t-tests and repeated measures Analysis of Variance) to determine whether levels of catastrophizing were similar in ICPs and their spouses and to explore demographic characteristics as moderators of the differing levels of pain catastrophizing within couples. Correlations were also conducted between ICP and spouse pain catastrophizing, perceptions of pain severity and interference, and depressive symptoms to determine if spouse and ICP catastrophizing relate similarly to pain and distress. As indicated earlier, spouse depressive symptoms were included because it is likely that spouses’ catastrophizing might relate to their own psychological distress. Gender and racial group differences in these results were also explored. Finally, we conducted several hierarchical regressions to examine whether spouse pain catastrophizing was related to psychological distress in both spouses. We entered ICPs’ reports of pain severity and interference in the first step of the analysis and both spouses’ catastrophizing scores in the second step. The interaction between spouses’ total catastrophizing was entered in the third step to determine whether high levels of catastrophizing in both spouses was related to elevated depressive symptoms in both spouses.
4.2.2. Confirmatory factor analysis
The same six models that were tested in Studies 1 and 2 were tested in this sample (see Study 3 section of Table 1). The model fit was adequate for Models 5 and 6, which included the cross-loadings of items 1 and 9. As in Studies 1 and 2, the fit of Model 5 was significantly better than that of Model 4, Δχ2 (1)=11.97, P<.001 and the factor loadings were similar (see bold type in Fig. 1). The smaller sample size in Study 3 may account for the lower values of the fit indices. Indeed, NFI is particularly susceptible to fit underestimation in smaller samples (Byrne, 2001). Factor invariance across gender and racial groups was not examined due to the smaller sample; however, gender and racial group analyses are presented below.
4.2.3. Descriptive statistics and demographic analyses
As in Studies 1 and 2, the PCS-S subscales and total score had acceptable to excellent inter-item reliabilities across genders and racial groups (see Table 2 and Table 3).
PCS-S mean scores are displayed in Table 2 and Table 3. Note that these scores are similar to the means presented for Studies 1 and 2. There were no gender or racial group differences in any of the PCS-S subscales or the total score, replicating the findings in Studies 1 and 2. Age was significantly correlated with the PCS-S rumination subscale, r (111)=−.22, P<.05, but was not significantly correlated with the helplessness or magnification scales, or with the total PCS-S score.
4.2.4. Within-couples analyses
Paired sample t-tests showed that spouses engaged in significantly more magnification, rumination, and overall catastrophizing than their spouses who were ICPs (see Table 4). We also conducted a repeated measures analysis of variance (ANOVA) with the total pain catastrophizing score representing the repeated measure within the couple to test whether ICP-spouse differences in pain catastrophizing depended on group membership. Group effects included gender (male versus female ICP) and racial group (African-American versus Caucasian). Participants reporting racial or ethnic group identifications other than African-American or Caucasian were excluded from the analysis (n=9). Age was included as a covariate. Two participants neglected to provide their age so they are also excluded. Therefore, n=100 for the following analysis.
Results showed that the ICP-spouse difference on pain catastrophizing was no longer significant when accounting for age, gender, and race, F (1, 95)=.81, P>.37. Age and gender did not moderate the ICP-spouse difference in pain catastrophizing, Ps>.10. However, there was a significant racial group by pain catastrophizing interaction, F (1, 95)=4.91, P<.03. Post hoc analyses indicated that the ICP-spouse difference in pain catastrophizing was significant for Caucasian couples (ICP M=15.79, SD=12.33; Spouse M=22.05, SD=9.31; t [59]=−3.91, P<.0001) but not significant for African-American couples (ICP M=23.68, SD=13.19; Spouse M=23.80, SD=10.80; t [39]=−.06, P>.95).
4.2.5. Correlations
Next we examined the correlations between the PCS and PCS-S with pain severity, interference, and depressive symptoms. Both partners’ pain catastrophizing scores were significantly correlated with one another, (rumination r=.25, P<.05; helplessness r=.22, P<.05; magnification r=.33, P<.001; Total PCS r=.35, P<.001). Because the patterns of correlations were similar for each PCS subscale and for the parsimonious presentation of results, only the total pain catastrophizing scores were used in the following analyses. As shown in Table 5, the PCS and PCS-S were significantly related to both partners’ perceptions of pain severity and interference. As might be expected, there were some significant differences in the strength of the correlations, which may correspond to the repeated finding in the literature that one’s own cognitions are more strongly related to one another than with an other’s cognitions. While both partners’ pain catastrophizing scores were correlated with ICPs’ depressive symptoms, only the healthy spouses’ pain catastrophizing scores were correlated with the healthy spouses’ depressive symptoms; however, an r to z transformation showed that the two correlations were not significantly different from each other. Note also that the correlation between ICP catastrophizing and ICP depressive symptoms was significantly stronger than the correlation between spouse catastrophizing and spouse symptoms, z=3.81, P<.01. The correlations remained significant when controlling for age.
Table 5.
Correlations between pain catastrophizing and pain severity, interference, and depressive symptoms
| Pain catastrophizing |
||
|---|---|---|
| ICPs | Spouses | |
| Pain severity—ICP Reporta | .41*** | .19* |
| Pain severity—Spouse Reportb | .28** | .45*** |
| Pain interference—ICP Report | .43*** | .34*** |
| Pain interference—Spouse Reportc | .25** | .49*** |
| ICP depressive symptomsd | .56*** | .35*** |
| Spouse depressive symptoms | .13 | .26** |
P<.05
P<.01
P<.001
n=111; ICPs, individuals with chronic pain. Superscripts indicate significant differences between correlations as indicated by r to z transformations.
z=2.54, P<.05.
z=2.13, P<.05.
z=2.92; P<.05
z=2.76; P<.05.
Because researchers have demonstrated gender and racial group differences on catastrophizing (Chibnall and Tait, 2005; Sullivan et al., 2000), we also tested for possible group differences in these correlations. To conserve space, we only report on the significantly different correlations. Copies of the correlations by group are available from the first author upon request. ICP pain catastrophizing was more strongly related to pain severity in female ICPs (z=2.33, P<.05). In fact, the correlation for females was significant (r [44]=.48, P<.001) whereas the correlation for men was marginally significant (r [67]=.29, P<.06). Pain catastrophizing was more strongly related to depressive symptoms in male (r [67]=.51, P<.001) than in female ICPs (r [44]=.44, P<.001; z=2.19, P<.05). There were no other significant differences between men and women or between African-American and Caucasian ICP or spouse participants on the correlations between pain catastrophizing and the other variables. These results indicate that ICP and spouse pain catastrophizing scores are correlated with pain severity, interference, and depressive symptoms regardless of age, gender, or racial group membership.
4.2.6. Hierarchical regressions
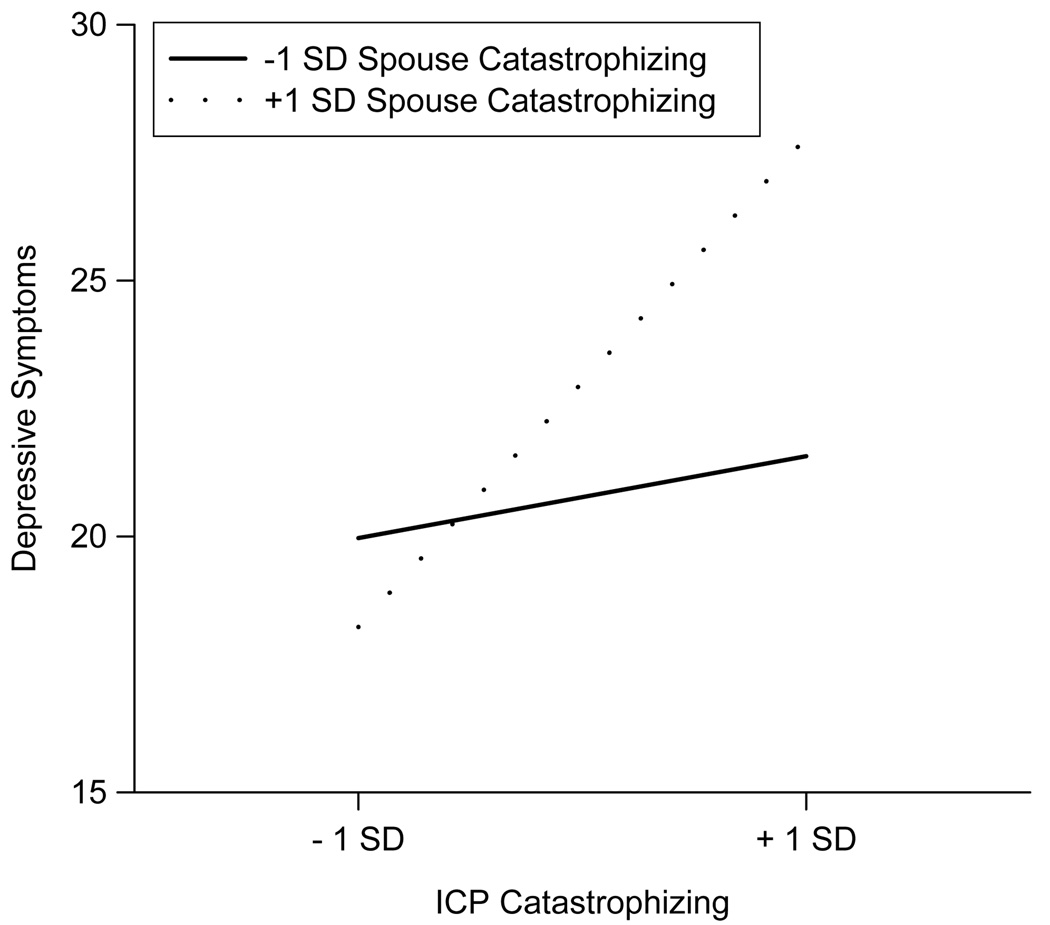
To follow up on the correlation analyses, we examined the independent contributions of both partners’ pain catastrophizing to the variance in depressive symptoms in both ICPs and spouses. The interaction between both spouses’ pain catastrophizingwas also examined as a correlate of depressive symptoms. Age, gender, and racial group were not entered in this regression analysis because the previous correlations did not show consistent differences in how pain catastrophizing is related to depressive symptoms for both ICPs and spouses; moreover, the addition of three main effects and several higher order interaction terms would adversely affect power. For ICPs, there was a significant interaction between both spouses’ pain catastrophizing scores that accounted for 4% of the variance in their depressive symptoms (see Table 6). Post hoc probing of this interaction showed that ICPs’ catastrophizing was related to their depressive symptoms at higher levels (i.e. +1 SD) of spouse catastrophizing (b=.36, SE=.07, B=.52, t=5.16, P<.0001) but not at lower levels (i.e. −1 SD) of spouse catastrophizing (b=.06, SE=.09, B=.09, t=.67, P>.50). In other words, there was a synergistic interaction between ICP and spouse catastrophizing such that ICPs with higher levels of catastrophizing who also have spouses with higher levels of catastrophizing were at a greater risk for psychological distress (see Fig. 2). These results remained when spouse depressive symptoms were entered into Step 1.
Table 6.
Summary of hierarchical regressions for couples’ pain catastrophizing in relating to depressive symptoms
| B | SE | β | ΔR2 | |
|---|---|---|---|---|
| DVZICP depressive symptoms | ||||
| Step 1 | .31** | |||
| Pain severity | .56 | .25 | .23* | |
| Pain interference | .26 | .07 | .38** | |
| Step 2 | .13** | |||
| ICP pain catastrophizing | .24 | .06 | .36** | |
| Spouse pain catastrophizing | .10 | .07 | .11 | |
| Step 3 | .04** | |||
| ICP X spouse pain catastrophizing | .02 | .01 | .74** | |
| DVZspouse depressive symptoms | ||||
| Step 1 | .04 | |||
| Pain severity | .46 | .26 | .22 | |
| Pain interference | −.01 | .08 | −.02 | |
| Step 2 | .04 | |||
| ICP pain catastrophizing | .02 | .06 | .03 | |
| Spouse pain catastrophizing | .18 | .09 | .23* | |
| Step 3 | .01 | |||
| ICP X spouse pain catastrophizing | −.01 | .01 | −.24 |
n=111; B, unstandardized regression coefficient; SE, standard error of B; β, standardized regression coefficient; DV, dependent variable; ICP, individual with chronic pain.
P<.05
P<.01.
Fig. 2.
Interaction between ICP and spouse catastrophizing on ICP depressive symptoms.
There was no significant interaction for healthy spouses (see Table 6). However, spouse catastrophizing remained a significant correlate of spouse depressive symptoms when controlling for their perceptions of the ICPs’ pain severity and interference.
4.2.7. Discussion
This third study demonstrated that the 3-factor model with two cross-loadings provided an adequate fit to the PCS-S data in a sample of spouses of ICPs. Additional analyses showed that pain catastrophizing was correlated within couples and that ICP-spouse differences in catastrophizing may occur when the ICP is Caucasian but not when the ICP is African-American. In addition, spouse pain catastrophizing was correlated with ICPs’ and spouses’ perceptions of ICP pain severity and interference as well as with both spouses’ depressive symptoms. However, ICP pain catastrophizing appears to be related to their own depressive symptoms when their spouses are also high on catastrophizing. These results suggest that the PCS-S may be a useful instrument in assessing spouse cognitions that are relevant to the pain experience.
5. General discussion
The purpose of this series of studies was to determine whether the PCS-S is an appropriate measure of pain catastrophizing in significant others of ICPs. Studies 1 and 2 demonstrated that acceptable fit was achieved with an oblique 3-factor model. These results are similar to those of previous studies showing that an oblique 3-factor model and the similar second-order model best fit the original PCS and a child version of the PCS (Crombez et al., 2003; Osman et al., 1997, 2000; Sullivan et al., 1995; Van Damme et al., 2002). The models were invariant across genders, as was found by Crombez et al. (2003) who demonstrated gender invariance in their 3-factor model of the PCS-Child version. Moreover, we found that our 3-factor models were invariant across Caucasian and African-American participant groups. We also found that there were few differences between men and women and between racial groups in the levels of catastrophizing. These findings suggest that the PCS-S may be used with male, female, Caucasian, and African-American groups with some confidence. Significant correlations with age were found suggesting that older participants use catastrophizing less, perhaps because of increased maturity and reliance on a broader array of coping strategies.
A difference between our findings and those of some previous studies was that we identified two cross-loadings between rumination and helplessness items and factors. Cross-loadings in factor analysis are not unusual and have been found by other researchers testing the factor structure of the original PCS (Osman et al., 1997; Sullivan et al., 1995). It is possible that rumination and helplessness are temporally related. For instance, an individual who feels helpless about a significant other’s situation may then ruminate about the future of the partner’s health as well as prospects of their own health. Likewise, rumination about pain may increase feelings of helplessness and lack of control over pain. Additional research is needed to determine if there is a temporal association between the dimensions of pain catastrophizing. The cross-loadings found in the current study may also suggest that significant others experience rumination and helplessness about pain as more similar than ICPs catastrophizing about their own pain. Alternatively, significant others might interpret some rumination and helplessness items as having the same meaning. Clearly, a replication study is needed of the 3-factor model with two cross-loadings in different samples of significant others (e.g. different geographic regions) to provide further support for the model.
Study 3 was designed to examine the PCS-S in a sample of couples facing chronic musculoskeletal pain. The confirmatory factor analysis of the PCS-S replicated the oblique 3-factor model with two cross-loadings found in Studies 1 and 2, providing further support for the factor structure of the PCS-S. However, because of the smaller sample size in Study 3, we were not able to examine factor invariance across gender and racial groups. The fact that inter-item reliabilities were stable and that there were no gender or racial group differences in mean scores across groups suggests that the PCS-S may be an appropriate measure of significant other pain catastrophizing in a variety of samples. However, additional research with significant others of ICPs is needed to confirm factor invariance across demographic groups. Age was negatively related to only one PCS-S subscale (i.e. rumination), which is different from the findings in Studies 1 and 2. Developmental changes in cognition and coping may account for this difference across samples.
We also investigated within-couples relationships in pain catastrophizing. Partners’ catastrophizing were significantly and positively correlated with each other, providing additional evidence for the validity of the PCS-S. In addition, gender and racial group differences were examined. For Caucasian participants, spouses reported more pain catastrophizing than the ICPs. No differences were found for African-American participants or based on the gender of the ICP. The roles of partners of ICPs may be perceived differently in African-American and Caucasian couples. Perhaps, Caucasian couples are taught to empathize with their partners in a way that leads to more spouse catastrophizing while African-American couples are taught to be supportive in other ways. Alternatively, the differences within Caucasian couples may be due to their lower levels of catastrophizing compared to Caucasian spouses, African-American ICPs, and African-American spouses.
Correlation results demonstrated that ICP and spouse catastrophizing were related to psychological distress, providing some evidence for criterion-related validity. However, the association between catastrophizing and depressive symptoms was significantly weaker in spouses than in ICPs. Researchers have argued that the moderate correlations found between ICP catastrophizing and depression scores in previous studies demonstrate that pain catastrophizing is independent of, but related to, depressive symptoms (Cano, 2004; Sullivan et al., 2001b). The current research suggests that catastrophizing and depression might be even more distinct in spouses. However, the construct of spouse pain catastrophizing will require further development and comparison with other constructs such as worry before stronger recommendations for its measurement can be made.
Spouse catastrophizing was also correlated with ICP depressive symptoms. Specifically, ICP catastrophizing was not related to their own depressive symptoms when their spouses reported low levels of catastrophizing but was positively related to their own depressive symptoms when their spouses also reported a high level of catastrophizing. This result was found when accounting for spouses’ perceptions of pain and interference and their own depressive symptoms, indicating a robust effect. It is possible that catastrophizing in both spouses results in specific behaviors that may exacerbate depressive symptoms in ICPs. For instance, the typical high catastrophizing couple may consist of a worried ICP and a healthy spouse who is over-involved in the ICP’s care and emotional wellbeing (i.e. solicitous). In these cases, ICPs may be concerned about the future of their pain and perceive themselves as a burden on their spouses. High catastrophizing couples may also be unable to meet each other’s need for intimacy because they are so focused on the pain problem. On the other hand, a catastrophizing ICP who has a partner low in catastrophizing might be better able to manage their thoughts and feelings. ICPs who express their concerns to their low catastrophizing spouses may be met with support, validation, and reassurance as suggested in the communal coping model of catastrophizing (Sullivan et al., 2001a; Thorn et al., 2003). Therefore, these ICPs may be protected from high levels of depressive symptoms. No such interaction was found for spouse depressive symptoms. Spouses’ depressive symptoms may be more a function of their own interpretations of events. Future research will determine whether these processes are at work.
The studies presented here have several strengths including racial diversity in each sample, testing of gender and race invariance in Studies 1 and 2, and the use of three samples, but there are also limitations. First, the samples in Studies 1 and 2 consisted of undergraduates, most of who were women and who did not have significant others with current chronic pain conditions. However, the original PCS was not developed as an instrument solely for use in chronic pain samples. Pain catastrophizing is a factor in acute pain as well (e.g. Sullivan et al., 2004). It is likely that many of the significant others of participants in Studies 1 and 2 had experienced pain of various types that did not meet the 6-month duration definition of chronic pain. Moreover, similar inter-item reliabilities and mean scores across all three studies suggest that pain catastrophizing is a phenomenon that is not limited to older significant others of ICPs. Second, although the models in Studies 1–3 showed adequate fit, it is possible that the small samples resulted in underestimates of some of the fit indices (e.g. NFI; Byrne, 2001). Additional research is needed to test the factor structure in larger samples, samples with a higher proportion of men, and in clinical and non-clinical samples of ICPs and their spouses. Third, due to the number of variables in the Study 3 regression analyses, we were unable to test higher order interactions including age, gender, and race variables. Although the current study demonstrated few significant differences in the relationship of catastrophizing to other variables (i.e. pain severity, interference, depressive symptoms), we recommend that researchers conduct work in this area with larger samples to determine whether such interactions exist.
Nonetheless, the three studies reported here provide preliminary evidence supporting the use of the PCS-S as a measure of pain catastrophizing in the significant others of ICPs. The assessment of significant other catastrophizing may offer clinicians and researchers the ability to conduct comprehensive assessments of intra-personal aspects of chronic pain that may have inter-personal effects. This study demonstrated that a high degree of catastrophizing in both partners might increase ICPs’ risk for psychological distress. By assessing both partners, rather than the ICP alone, clinicians may be more accurate in the identification of ICPs at risk. In terms of treatment, researchers have shown that reductions in catastrophizing are related to improvements in depressive symptoms (Burns et al., 2003; Jensen et al., 2001). Future research may show that a couples focus on reducing catastrophizing in both partners may be beneficial for both partners.
Acknowledgements
Annmarie Cano was supported by grant K01 MH066975 while working on this paper. The authors thank the members of the Relationships and Health Lab for their help in conducting this study.
References
- Affleck G, Tennen H, Keefe FJ, Lefebvre JC, Kashikar-Zuck S, Wright K, Starr K, Caldwell DS. Everyday life with osteoarthritis or rheumatoid arthritis: independent effects of disease and gender on daily pain, mood, and coping. Pain. 1999;83:601–609. doi: 10.1016/S0304-3959(99)00167-0. [DOI] [PubMed] [Google Scholar]
- Burns JW, Kubilus A, Bruehl S, Harden RN, Lofland K. Do changes in cognitive factors influence outcome following multidisciplinary treatment for chronic pain? A cross-lagged panel analysis. J Consult Clin Psych. 2003;71:81–91. doi: 10.1037//0022-006x.71.1.81. [DOI] [PubMed] [Google Scholar]
- Butterfield RM, Lewis MA. Health-related social influence: a social ecological perspective on tactic use. J Soc Pers Relat. 2002;19:505–526. [Google Scholar]
- Byrne BM. Structural equation modeling with amos: basic concepts, applications, and programming. Mahwah, NJ: Lawrence Erlbaum; 2001. [Google Scholar]
- Cano A. Pain catastrophizing and social support in married individuals with chronic pain: the moderating role of pain duration. Pain. 2004;110:656–664. doi: 10.1016/j.pain.2004.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano A, Johansen AB, Geisser M. Spousal congruence on disability, pain, and spouse responses to pain. Pain. 2004;109:258–265. doi: 10.1016/j.pain.2004.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chibnall JT, Tait RC. Confirmatory factor analysis of the pain catastrophizing scale in African American and Caucasian workers’ compensation claimants with low back injuries. Pain. 2005;113:369–375. doi: 10.1016/j.pain.2004.11.016. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Smith DAF. Couples coping with a myocardial infarction: a contextual perspective on wives’ distress. J Pers Soc Psychol. 1991;61:404–412. doi: 10.1037//0022-3514.61.3.404. [DOI] [PubMed] [Google Scholar]
- Cremeans-Smith JK, Stephens MAP, Franks MM, Martire LM, Druley JA, Wojno WC. Spouses’ and physicians’ perceptions of pain severity in older women with osteoarthritis: dyadic agreement and patients’ well-being. Pain. 2003;106:27–34. doi: 10.1016/s0304-3959(03)00268-9. [DOI] [PubMed] [Google Scholar]
- Crombez G, Bijttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, Verstraeten K. The child version of the Pain Catastrophizing Scale (PCS-C): a preliminary validation. Pain. 2003;104:639–646. doi: 10.1016/S0304-3959(03)00121-0. [DOI] [PubMed] [Google Scholar]
- Davis-Ali SH, Chesler MA, Chesney BK. Recognizing cancer as a family disease: worries and support reported by patients and spouses. Soc Work Health Care. 1993;19:45–65. doi: 10.1300/J010v19n02_02. [DOI] [PubMed] [Google Scholar]
- Folstein M, Folstein S, McHugh P. Mini-mental state: a practical method for grading the state of patients for the clinician. J Psychiatr Res. 1975;31:251–259. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Geisser M, Cano A, Foran H. Psychometric properties of the Mood and Anxiety Symptom Questionnaire in chronic pain patients. Clin J Pain. doi: 10.1097/01.ajp.0000146180.55778.4d. in press. [DOI] [PubMed] [Google Scholar]
- Geisser ME, Cano A, Leonard MT. Factors associated with marital satisfaction and mood among spouses of persons with chronic back pain. J Pain. 2005;6:518–525. doi: 10.1016/j.jpain.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Giardino ND, Jensen MP, Turner JA, Ehde DM, Cardenas DD. Social environment moderates the association between catastrophizing and pain among persons with a spinal cord injury. Pain. 2003;106:19–25. doi: 10.1016/s0304-3959(03)00226-4. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Turner JA, Romano JM. Changes in beliefs, catastrophizing, and coping are associated with improvement in multidisciplinary pain treatment. J Consult Clin Psychol. 2001;69:655–662. doi: 10.1037//0022-006x.69.4.655. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Brown GK, Wallston KA, Caldwell DS. Coping with rheumatoid arthritis pain: catastrophizing as a maladaptive strategy. Pain. 1989;37:51–56. doi: 10.1016/0304-3959(89)90152-8. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Lipkus I, Lefebvre JC, Hurwitz H, Clipp E, Smith J, Porter L. The social context of gastrointestinal cancer pain: a preliminary study examining the relation of patient pain catastrophizing to patient perceptions of social support and caregiver stress and negative responses. Pain. 2003;103:151–156. doi: 10.1016/s0304-3959(02)00447-5. [DOI] [PubMed] [Google Scholar]
- Kerns RD, Rosenberg R. Pain-relevant responses from significant others: development of a significant-other version of the MPI scales. Pain. 1995;61:245–249. doi: 10.1016/0304-3959(94)00173-C. [DOI] [PubMed] [Google Scholar]
- Kerns RD, Turk DC, Rudy TE. The West Haven-Yale multidimensional pain inventory. Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O’Neill E. Factor structure, reliability, and validity of the Pain Catastrophizing Scale. J Behav Med. 1997;20:589–605. doi: 10.1023/a:1025570508954. [DOI] [PubMed] [Google Scholar]
- Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, Grittman L. The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. J Behav Med. 2000;23:351–365. doi: 10.1023/a:1005548801037. [DOI] [PubMed] [Google Scholar]
- Riemsma RP, Taal E, Rasker JJ. Perceptions about perceived functional disabilities and pain of people with rheumatoid arthritis: differences between patients and their spouses and correlates of well-being. Arthritis Care Res. 2000;13:255–261. doi: 10.1002/1529-0131(200010)13:5<255::aid-anr3>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Romano JM, Turner JA, Clancy SL. Sex differences in the relationship of pain patient dysfunction to spouse adjustment. Pain. 1989;39:289–295. doi: 10.1016/0304-3959(89)90042-0. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Bishop S, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7:432–524. [Google Scholar]
- Sullivan MJL, Tripp DA, Santor D. Gender differences in pain and pain behavior: the role of catastrophizing. Cogn Ther Res. 2000;24:121–134. [Google Scholar]
- Sullivan MJL, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001a;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Rodgers WM, Kirsch I. Catastrophizing, depression and expectancies for pain and emotional distress. Pain. 2001b;91:147–154. doi: 10.1016/s0304-3959(00)00430-9. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Adams H, Sullivan ME. Communicative dimensions of pain catastrophizing: social cueing effects on pain behaviour and coping. Pain. 2004;107:220–226. doi: 10.1016/j.pain.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Thorn BE, Ward LC, Sullivan MJL, Boothby JL. Communal coping model of catastrophizing: conceptual model building. Pain. 2003;106:1–2. doi: 10.1016/s0304-3959(03)00228-8. [DOI] [PubMed] [Google Scholar]
- Turner JA, Jensen MP, Romano JM. Do beliefs, coping, and catastrophizing independently predict functioning in patients with chronic pain? Pain. 2000;85:115–125. doi: 10.1016/s0304-3959(99)00259-6. [DOI] [PubMed] [Google Scholar]
- Turner JA, Jensen MP, Warms CA, Cardenas DD. Catastrophizing is associated with pain intensity, psychological distress, and pain-related disability among individuals with chronic pain after spinal cord injury. Pain. 2002;98:127–134. doi: 10.1016/s0304-3959(02)00045-3. [DOI] [PubMed] [Google Scholar]
- Turner JA, Mancl L, Aaron LA. Pain-related catastrophizing: a daily process study. Pain. 2004;110:103–111. doi: 10.1016/j.pain.2004.03.014. [DOI] [PubMed] [Google Scholar]
- Van Damme S, Crombez G, Bijttebier P, Goubert L, Van Houdenhove B. A confirmatory factor analysis of the Pain Catastrophizing Scale: invariant factor structure across clinical and non-clinical populations. Pain. 2002;96:319–324. doi: 10.1016/S0304-3959(01)00463-8. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Mood and anxiety symptom questionnaire. Iowa City, IA: University of Iowa, Department of Psychology; 1991. Unpublished manuscript. [Google Scholar]
- Watson D, Clark LA, Weber K, Assenheimer JS. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. J Abnorm Psychol. 1995a;104(1):15–25. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. J Abnorm Psychol. 1995b;104(1):3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]