Abstract
Objectives. We identified factors associated with testing HIV positive in a prison system performing voluntary HIV testing on inmates and estimated the number of undetected HIV cases to evaluate the efficacy of risk-factor–based HIV testing.
Methods. We used logistic regression to estimate associations between HIV serostatus and HIV risk behaviors, mental health, coinfection status, and sociodemographic characteristics for prisoners entering the North Carolina Department of Correction from January 2004 through May 2006. We estimated the number of undetected HIV cases on the basis of age-, gender-, and race-specific HIV prevalences among prisoners and in the state.
Results. Nearly 3.4% (718/21 419) of tested prisoners were HIV positive. The strongest risk factors for infection among men were having sex with men (odds ratio [OR] = 8.0), Black race (OR = 6.2), other non-White race (OR = 7.4), and being aged 35 to 44 years (OR = 4.1). The strongest risk factor among women was Black race (OR = 3.8). Among HIV-positive prisoners, 65% were coinfected with HCV. We estimated that between 24% (223) and 61% (1101) of HIV cases remained undetected.
Conclusions. The associations between HIV serostatus and a variety of factors highlight the potential limitations of risk-factor–based HIV testing in prisons, as do the high number of potential undetected HIV cases.
The prevalence of HIV among correctional populations in the United States is several times that of the general population, and it has been estimated that between 13% and 19% of all HIV-infected individuals in the United States are released from a correctional facility each year.1 The vast majority of these infections are acquired in the community.2 Given prisoners' limited access to routine health care prior to their incarceration, prisons are an important venue for the provision of HIV prevention, testing, and treatment services.3 An accurate description of the size and attributes of the HIV-infected prison population would facilitate evaluation and improvement of these services.
A better understanding of the characteristics of the HIV-infected prison population may be particularly timely with regard to evaluation and improvement of testing policies. As of 2004, 29 state prison systems provided voluntary (i.e., consent-based) HIV testing to inmates, of which 12 targeted “high-risk” prisoners for testing.4 In 2003 and 2006, the Centers for Disease Control and Prevention (CDC) recommended the expansion of routine opt-out HIV testing5,6; thus, prison systems that traditionally targeted high-risk inmates for HIV testing are now under pressure to revise their testing policies. The presence of strong associations between inmate characteristics and infection status would support the continuation of risk-factor–based HIV testing; alternatively, the presence of modest associations would support the abandonment of risk-factor–based testing in favor of routine opt-out testing.
Determining the inmate characteristics associated with HIV infection could also be useful in facilitating the provision of other services. For example, positive associations between HIV infection and short sentence length could signal the need for rapid initiation of transition services in preparation for infected inmates' release. Similarly, positive associations between HIV infection and mental conditions or illegal substance use could suggest the need for greater coordination of these services for inmates with these characteristics.
Only a few studies have examined the characteristics and behaviors of HIV-positive prisoners in the United States, and most of these studies were conducted in relatively small prison systems in the Northeast.7–9 Similar studies have rarely been conducted in other parts of the country, including the South, which is the US region with the highest rate of incarceration,10 the highest number of new AIDS diagnoses, and the highest number of people living with—and dying from—AIDS.11
Our goal was to determine associations between HIV infection and inmate characteristics among a population of inmates who had been voluntarily tested for HIV in a large Southern state prison system, the North Carolina Department of Correction (NC DOC). We also used prevalences derived from tested prisoners and from statewide data to estimate a plausible range of undetected HIV cases among NC DOC inmates.
METHODS
The study population comprised adult prisoners who entered the NC DOC between January 1, 2004, and May 30, 2006, and received a voluntary HIV test while incarcerated during the study period.
Upon admission, prisoners are assessed for vocational skill, educational achievement, illicit substance use, and mental and physical health. The medical evaluation includes routine testing for syphilis and tuberculosis (TB); testing for HCV is conducted when clinically indicated. Male inmates are screened for the following conventional HIV risk behaviors: (1) blood transfusion during the period 1978–1985, (2) sex with multiple partners, (3) sex as or with a sex worker, (4) needle sharing, and (5) sex with men. Female prisoners are assessed for behaviors 1 through 4 as well as sex with injection drug users and sex with men who have sex with men (MSM).
Following this assessment, inmates of unknown serostatus are supposed to have an opportunity to test for HIV; inmates self-reporting a previous HIV diagnosis typically receive confirmatory testing before initiation of antiretroviral therapy. Inmates may also request an HIV test at any time during their incarceration. All HIV-positive inmates are tested for HCV. Assessments of inmates' social and criminal histories are conducted by a NC DOC case analyst and are informed by data collected prior to sentencing.
Electronic Records and Data Linking
The NC DOC provided us with electronic records of the data just described. Dates and results of all tests for syphilis, HCV, and HIV conducted during the study period were provided in a separate database by Quest Diagnostics (Madison, NJ), a private company contracted by the NC DOC to process diagnostic lab work.
Electronic prison and lab data were linked using a unique prison identification number (PIN) assigned to all inmates upon first admission. The PIN was present in all prison records and was missing in less than 3% of lab records. Lab records with missing PINs were excluded from our analyses. Only records of prisoners tested for HIV were included for analysis.
Before analysis, each inmate record was assigned a unique study identification number; all other identifying information (name, date of birth, and PIN) was removed. Only records of inmates who were 18 years or older at the time of prison admission were included for analysis.
Coding of Infectious Disease Test Results and Mental Health Conditions
Inmates were classified as HIV positive if an enzyme-linked immunosorbent assay was reactive and a Western blot test was interpreted as positive; they were classified as HCV-positive if they had a reactive HCV antibody test; and they were classified as positive for active syphilis if the Rapid Plasma Reagin titer was 1:8 or greater.12 All prisoners were tested for TB using a Mantoux screening test at admission. Because Mantoux results were not electronically available, we used electronic medication prescription data to classify prisoners' TB status. Inmates who were prescribed anti-TB medications within 30 days of admission were coded as having TB.
We used electronic records to determine whether prisoners had been diagnosed with selected Axis I and Axis II Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), mental health disorders. Prisoners diagnosed with both Axis I and Axis II disorders were coded as having an Axis I disorder only.
Model-Based Analyses
The proportion of HIV-infected prisoners was calculated for the following categories: sociodemographic characteristics, conventional HIV risk behaviors, drug use, conviction history, mental health disorder, TB disease, syphilis infection, and HCV infection.
Conventional HIV risk behaviors for women were only recorded in 1 of the 2 intake facilities that process females, resulting in risk-behavior data for 41% of females. Among men, HIV risk behavior assessments were recorded in 92% of records. For each of the 22 independent variables of interest, bivariate associations with HIV serostatus were estimated with a gender-specific logistic regression. Then multivariate gender-specific logistic regression models for HIV serostatus were fit conditionally on (1) all conventional HIV risk behaviors and (2) all characteristics with statistically significant (P < .05) bivariate associations. Prisoners lacking records with risk-behavior assessments were excluded from the multivariate logistic regression models.
Estimating HIV Cases Among Untested Inmates
Most female prisoners were tested for HIV, but more than two thirds of male prisoners were not tested, so we estimated a plausible range of unidentified (i.e., untested) male HIV cases. First we stratified the population of untested males by age (5 categories) and race (Black, White, and other [which includes NC DOC categories Indian, Asian/Oriental, Other, and Unknown]). Second, we multiplied the number (Ni) of untested prisoners within each of these strata by corresponding stratum-specific prevalence estimates ( ) obtained from the population of male prisoners tested for HIV. Thus, the estimate of the number of HIV cases (
) obtained from the population of male prisoners tested for HIV. Thus, the estimate of the number of HIV cases ( ) took the form of a weighted sum of prevalence estimates:
) took the form of a weighted sum of prevalence estimates:
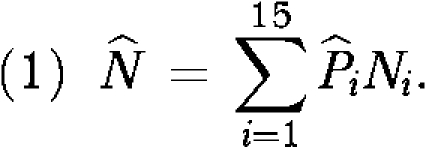 |
We repeated the same approach, using age- and race-specific prevalence estimates ( ) for the general population of men in North Carolina. We calculated state prevalence estimates among men by dividing the age- and race-specific number of North Carolina men known to be HIV positive as reported to the state health department (W. Jones, MPH, written communication, 2007) by the corresponding stratum-specific population denominators of men derived from US census data. To enhance the stability of these state estimates, we pooled HIV case and census data from 2000 to 2005. For both sets of calculations, we assumed that the age distribution of untested prisoners was fixed. We used SAS v9.1 (SAS Institute, Cary, NC) to conduct all analyses.
) for the general population of men in North Carolina. We calculated state prevalence estimates among men by dividing the age- and race-specific number of North Carolina men known to be HIV positive as reported to the state health department (W. Jones, MPH, written communication, 2007) by the corresponding stratum-specific population denominators of men derived from US census data. To enhance the stability of these state estimates, we pooled HIV case and census data from 2000 to 2005. For both sets of calculations, we assumed that the age distribution of untested prisoners was fixed. We used SAS v9.1 (SAS Institute, Cary, NC) to conduct all analyses.
RESULTS
During the study period, 54 644 prisoners 18 years or older entered the North Carolina prison system. Of these prisoners, we included in our study population the 21 419 prisoners (39% of the total) with an HIV test result for their most recent incarceration.
Table 1 presents characteristics of the HIV-tested population. About one third of the population was female, and nearly half the population was Black. More than one third of men and nearly two thirds of women had used crack or cocaine. Only 1% of men reported having sex with men, but 3% of males and 9% of females reported sharing needles; 17% of females also reported having sex with men who shared needles. Of the 21 419 prisoners tested for HIV, 3.4% overall (718) were HIV positive (3.6% of men and 2.6% of women). Eighty-four percent of prisoners testing positive had been previously diagnosed with HIV in North Carolina.
TABLE 1.
Characteristics and Behaviors of Adult Inmates Tested for HIV Following Incarceration in the North Carolina State Prison System: January 2004–May 2006
| Women, % (N = 5958) | Men, % (N = 15 461) | |
| Age, y | ||
| ≥ 45 | 12.2 | 16.5 |
| 35–44 | 33.9 | 31.8 |
| 25–34 | 36.4 | 36.7 |
| 18–24 | 17.5 | 15.1 |
| Race/Ethnicity | ||
| Black | 42.8 | 49.7 |
| Other | 3.0 | 4.7 |
| White | 54.2 | 45.6 |
| Education | ||
| College | 13.1 | 8.4 |
| High school diploma or GED | 46.0 | 50.3 |
| Less than a high school diploma | 40.9 | 41.3 |
| Unemployeda | 66.5 | 31.3 |
| Marrieda | 15.1 | 15.5 |
| IQ test results | ||
| ≤ 80 | 13.7 | 21.4 |
| 81–100 | 55.0 | 55.2 |
| ≥ 101 | 31.4 | 23.3 |
| Previous time served, mo | ||
| None | 57.8 | 36.8 |
| ≤ 6 | 15.8 | 15.1 |
| 7–12 | 11.3 | 10.9 |
| ≥ 13 | 15.2 | 37.3 |
| Sentence length,b mo | ||
| ≥ 19 | 14.5 | 29.4 |
| 7–18 | 23.1 | 25.5 |
| 3–6 | 31.8 | 20.7 |
| < 3 | 30.7 | 24.4 |
| Drug-related conviction ever | 41.8 | 35.6 |
| Sex-related conviction ever | 1.2 | 5.5 |
| Cocaine or crack use ever | 64.9 | 38.4 |
| Heroin use ever | 6.1 | 2.4 |
| Same-gender sexual partner everc | 15.2 | 1.0 |
| Multiple sexual partners everc | 27.1 | 18.0 |
| Prostitution evercd | 16.7 | 6.8 |
| Share needles everc | 9.4 | 3.2 |
| Blood transfusion everc | 2.9 | 0.9 |
| Sex with needle sharer evere | 16.2 | … |
| Sex with MSM evere | 3.2 | … |
| Mental health disorderf | ||
| Axis I | 6.4 | 3.0 |
| Axis II | 4.6 | 2.9 |
| HCV | ||
| Positive | 9.4 | 7.5 |
| Negative | 2.7 | 3.1 |
| No test | 87.9 | 89.4 |
| Syphilis | ||
| Positive | 5.9 | 5.3 |
| Negative | 93.5 | 89.4 |
| No test | 0.6 | 5.3 |
| Tuberculosis | 1.0 | 4.2 |
Note. GED = general equivalency diploma; MSM = men who have sex with men. For women, n = 5958; for men, n = 15 461.
Data missing for ≤ 5 observations per gender.
Data missing for 421 (7%) women and 778 (5%) men.
Data not collected from 59% of women and 9% of men.
Using a sex worker or engaging in sex work.
Data not collected from 59% of women and all men.
Axis I: psychosis, bipolar disorder, major depression, generalized anxiety and dementia. Axis II: personality disorder and developmental disability.
Stratified by race and age, the proportion of male prisoners infected with HIV ranged from 0% to 9.5%. The proportion was greatest among Blacks aged 45–54 years (Table 2). The age- and race-stratified proportions of infected female prisoners generally followed the same pattern as the men. Across ages, Blacks accounted for 82% of HIV-infected men and 75% of HIV-infected women. The proportions of HIV-infected prisoners coinfected with TB, syphilis, and HCV were 2.5%, 9.2%, and 67.8%, respectively. These proportions varied little by gender.
TABLE 2.
HIV Infection Prevalence Among Adult Inmates Entering the North Carolina State Prison System, by Age, Race/Ethnicity, and Gender: January 2004–May 2006
| Black |
Other |
White |
||||
| Age, y | Total, No. | HIV Positive, % (No.) | Total, No. | HIV Positive, % (No.) | Total, No. | HIV Positive, % (No.) |
| Men | ||||||
| ≥ 55 | 203 | 6.9 (14) | 3 | 0.0 (0) | 124 | 0.0 (0) |
| 45–54 | 1275 | 9.5 (121) | 56 | 5.4 (3) | 885 | 1.1 (10) |
| 35–44 | 2513 | 8.2 (206) | 178 | 5.6 (10) | 2226 | 1.4 (31) |
| 25–34 | 2592 | 4.0 (103) | 356 | 3.9 (14) | 2720 | 1.0 (26) |
| 18–24 | 1098 | 1.7 (19) | 138 | 2.2 (3) | 1094 | 0.2 (2) |
| Total | 7681 | 6.0 (463) | 731 | 4.1 (30) | 7049 | 1.0 (69) |
| Women | ||||||
| ≥ 55 | 33 | 6.1 (2) | 0 | 0.0 (0) | 36 | 2.8 (1) |
| 45–54 | 307 | 4.2 (13) | 15 | 6.7 (1) | 338 | 0.9 (3) |
| 35–44 | 913 | 6.5 (59) | 64 | 4.7 (3) | 1045 | 1.8 (19) |
| 25–34 | 846 | 3.7 (31) | 79 | 1.3 (1) | 1241 | 0.6 (8) |
| 18–24 | 449 | 2.7 (12) | 23 | 0.0 (0) | 569 | 0.5 (3) |
| Total | 2548 | 4.6 (117) | 181 | 2.8 (5) | 3229 | 1.1 (34) |
HIV prevalence was greater among those with a history of any conventional HIV risk behavior (men 6.5%, women 4.0%) than among those without (men 2.6%, women 1.7%), but the majority of HIV cases arose from the 79% of men and 57% of women without a history of HIV risk behaviors. Of the 718 HIV cases, 242 (34%) had a history of at least 1 conventional HIV risk behavior, 317 (44%) had no history of any conventional risk behaviors, and 159 (22%) had no assessment data.
Among male prisoners reporting as MSM, the proportion infected with HIV was nearly 30%; among those who reported either sharing needles or having sex with a sex worker, the proportion infected was about 10% (Table 3). Five percent of male cocaine users were HIV positive. Sixty percent of HIV-positive men (293/492) reported no conventional HIV risk behaviors.
TABLE 3.
Covariate-Adjusted Associations Between Characteristics of Adult Male Inmates in the North Carolina State Prison System and HIV Infection: January 2004–May 2006
| HIV Positive |
|||
| Total | % (No.) | OR (95% CI) | |
| Age, y | |||
| ≥ 45 | 2546 | 5.8 (148) | 3.88 (2.30, 6.54) |
| 35–44 | 4917 | 5.0 (247) | 4.07 (2.46, 6.74) |
| 25–34 | 5668 | 2.5 (143) | 2.63 (1.59, 4.37) |
| 18–24 (Ref) | 2330 | 1.0 (24) | 1.00 |
| Race/Ethnicity | |||
| Black | 7681 | 6.0 (463) | 6.21 (4.60, 8.41) |
| Other | 731 | 4.1 (30) | 7.36 (4.36, 12.42) |
| White (Ref) | 7049 | 1.0 (69) | 1.00 |
| Education | |||
| College | 1294 | 4.9 (64) | 1.45 (1.01, 2.08) |
| High school diploma or GED | 7776 | 3.7 (284) | 1.28 (1.02, 1.59) |
| Less than a high school diploma (Ref) | 6391 | 3.3 (214) | 1.00 |
| Employment | |||
| Unemployed | 4836 | 5.8 (279) | 1.68 (1.37, 2.06) |
| Employed (Ref) | 10620 | 2.7 (283) | 1.00 |
| Marital status | |||
| Not married/separated | 13071 | 3.8 (491) | 1.21 (0.89, 1.63) |
| Married (Ref) | 2388 | 3.0 (71) | 1.00 |
| IQ test results | |||
| ≤ 80 | 3312 | 5.8 (193) | 1.83 (1.30, 2.57) |
| 81–100 | 8540 | 3.5 (299) | 1.21 (0.89, 1.63) |
| ≥ 101 (Ref) | 3609 | 1.9 (70) | 1.00 |
| Previous time served, mo | |||
| ≥ 13 | 5765 | 5.7 (326) | 1.84 (1.39, 2.44) |
| 7–12 | 1680 | 3.4 (57) | 1.46 (1.01, 2.13) |
| ≤ 6 | 2330 | 3.0 (70) | 1.11 (0.76, 1.61) |
| None (Ref) | 5686 | 1.9 (109) | 1.00 |
| Sentence length, mo | |||
| ≥ 19 | 4311 | 4.0 (172) | 1.74 (1.31, 2.32) |
| 7–18 | 3745 | 4.0 (150) | 1.81 (1.36, 2.42) |
| 3–6 | 3044 | 4.0 (121) | 1.96 (1.45, 2.65) |
| < 3 (Ref) | 3583 | 2.8 (99) | 1.00 |
| Heroin use ever | |||
| Yes | 369 | 6.8 (25) | 1.80 (1.07, 3.02) |
| No (Ref) | 15092 | 3.6 (537) | 1.00 |
| Cocaine or crack use ever | |||
| Yes | 5932 | 5.0 (298) | 1.30 (1.06, 1.60) |
| No (Ref) | 9529 | 2.8 (264) | 1.00 |
| Same-gender sexual partner ever | |||
| Yes | 144 | 29.9 (43) | 8.04 (5.17, 12.51) |
| No (Ref) | 14008 | 3.2 (446) | 1.00 |
| Multiple sexual partners ever | |||
| Yes | 2548 | 5.9 (150) | 1.41 (1.08, 1.84) |
| No (Ref) | 11604 | 2.9 (339) | 1.00 |
| Prostitution evera | |||
| Yes | 961 | 10.7 (103) | 1.64 (1.20, 2.24) |
| No (Ref) | 13191 | 2.9 (386) | 1.00 |
| Shared needles ever | |||
| Yes | 447 | 9.4 (42) | 2.14 (1.38, 3.31) |
| No (Ref) | 13705 | 3.3 (447) | 1.00 |
| Blood transfusion prior to 1986 | |||
| Yes | 130 | 3.8 (5) | 0.40 (0.15, 1.07) |
| No (Ref) | 14022 | 3.5 (484) | 1.00 |
| Sex-related conviction ever | |||
| Yes | 846 | 3.5 (30) | 0.86 (0.53, 1.41) |
| No (Ref) | 14615 | 3.6 (532) | 1.00 |
| Drug-related conviction ever | |||
| Yes | 5503 | 4.0 (219) | 0.79 (0.64, 0.98) |
| No (Ref) | 9958 | 3.4 (343) | 1.00 |
| Mental health disorderb | |||
| Axis I | 465 | 4.9 (23) | 1.17 (0.65, 2.10) |
| Axis II | 453 | 5.1 (23) | 1.60 (0.96, 2.66) |
| Neither (Ref) | 14543 | 3.5 (516) | 1.00 |
| HCV | |||
| Positive | 1161 | 33.2 (385) | … |
| Negative | 473 | 34.7 (164) | … |
| Syphilis | |||
| Positive | 816 | 6.3 (51) | 1.50 (1.05, 2.13) |
| Negative (Ref) | 13823 | 3.6 (498) | 1.00 |
| Tuberculosis | |||
| Positive | 650 | 2.3 (15) | 0.42 (0.22, 0.80) |
| Negative (Ref) | 14811 | 3.7 (547) | 1.00 |
Note. OR = odds ratio; CI = confidence interval; GED = general equivalency diploma.
Using a sex worker or engaging in sex work.
Axis I: psychosis, bipolar disorder, major depression, generalized anxiety, and dementia. Axis II: personality disorder and developmental disability.
In the model-based analyses for men, most of the prisoner-characteristics variables of interest had statistically significant bivariate associations with HIV status. Exceptions were marital status, sex-related or drug-related conviction, mental health diagnosis, blood transfusion history, and TB disease.
In the multivariate analysis for men (Table 3), all age groups older than the referent (18–24 years) were associated with greater prevalence of HIV infection, with the strength of the association increasing with age. Men in the racial categories Black (odds ratio [OR] = 6.02; 95% confidence interval [CI] = 4.48, 8.10) and other (OR = 7.40; 95% CI = 4.43, 12.36) were more likely than were Whites to be HIV infected. HIV infection was also more likely among high school graduates, those with a general equivalency diploma, and college graduates than among those who did not complete secondary school. Men previously incarcerated for 7 or more months were at greater risk for infection than were those who had never been incarcerated. Heroin use, cocaine or crack use, coinfection with syphilis, and several HIV risk behaviors (sex with men, multiple sexual partners, sex with prostitutes, and needle sharing) were all associated with increased risk of HIV infection.
Information for conventional HIV risk behaviors for female inmates was only collected in 1 of the 2 female intake facilities. Women in the facility with missing data had longer sentences (median: 4.0 months vs 1.6 months) and were slightly older (mean: 34.6 years vs 33.0 years) than women in the facility without missing data, but the groups did not differ by race or reported use of crack or cocaine. Among women with available data, 10% of those reporting sex with a male partner who had sex with men and 8% of those reporting blood transfusions prior to 1986 were HIV positive, but the number of cases for each was fewer than 10. About 5% of women reporting multiple sexual partners or prostitution were HIV infected (Table 4). Thirty-six percent of HIV-positive women with behavioral assessment data (24 of 67) reported no conventional HIV risk behaviors.
TABLE 4.
Covariate-Adjusted Associations Between Characteristics of Adult Female Inmates in the North Carolina State Prison System and HIV Infection: January 2004–May 2006
| HIV Positive |
|||
| Total | % (No.) | OR (95% CI) | |
| Age, y | |||
| ≥ 45 | 729 | 2.74 (20) | 1.78 (0.44, 7.15) |
| 35–44 | 2022 | 4.01 (81) | 2.55 (0.73, 8.86) |
| 25–34 | 2166 | 1.85 (40) | 1.97 (0.56, 6.97) |
| 18–24 (Ref) | 1041 | 1.44 (15) | 1.00 |
| Race/Ethnicity | |||
| Black | 2548 | 4.59 (117) | 3.57 (1.89, 6.73) |
| Other | 181 | 2.76 (5) | 2.38 (0.53, 10.74) |
| White (Ref) | 3229 | 1.05 (34) | 1.00 |
| Education | |||
| College | 780 | 2.18 (17) | … |
| High school diploma or GED | 2742 | 2.48 (68) | … |
| Less than high school | 2436 | 2.91 (71) | … |
| Employment | |||
| Unemployed | 3962 | 2.98 (118) | 1.50 (0.78, 2.87) |
| Employed (Ref) | 1994 | 1.91 (38) | 1.00 |
| Marital status | |||
| Not married/separated | 5057 | 2.71 (137) | 0.75 (0.37, 1.54) |
| Married (Ref) | 901 | 2.11 (19) | 1.00 |
| IQ test results | |||
| ≤ 80 | 813 | 4.67 (38) | 2.00 (0.86, 4.68) |
| 81–100 | 3276 | 2.72 (89) | 1.33 (0.64, 2.79) |
| ≥ 101 (Ref) | 1869 | 1.55 (29) | 1.00 |
| Previous time served, mo | |||
| ≥ 13 | 904 | 4.87 (44) | 1.01 (0.49, 2.09) |
| 7–12 | 670 | 3.88 (26) | 0.98 (0.44, 2.17) |
| ≤ 6 | 942 | 2.34 (22) | 0.61 (0.28, 1.36) |
| None (Ref) | 3442 | 1.9 (64) | 1.00 |
| Sentence length, mo | |||
| ≥ 19 | 803 | 3.11 (25) | … |
| 7–18 | 1277 | 2.51 (32) | … |
| 3–6 | 1758 | 2.45 (43) | … |
| < 3 | 1699 | 2.71 (46) | … |
| Heroin use ever | |||
| Yes | 366 | 3.55 (13) | 0.50 (0.11, 2.19) |
| No (Ref) | 5592 | 2.56 (143) | 1.00 |
| Cocaine or crack use ever | |||
| Yes | 3869 | 3.33 (129) | 1.21 (0.59, 2.50) |
| No (Ref) | 2089 | 1.29 (27) | 1.00 |
| Multiple sexual partners ever | |||
| Yes | 666 | 4.95 (33) | 2.16 (1.13, 4.14) |
| No (Ref) | 1788 | 1.90 (34) | 1.00 |
| Prostitution evera | |||
| Yes | 410 | 5.61 (23) | 0.93 (0.46, 1.86) |
| No (Ref) | 2044 | 2.15 (44) | 1.00 |
| Shared needles ever | |||
| Yes | 231 | 3.46 (8) | 1.04 (0.42, 2.54) |
| No (Ref) | 2223 | 2.65 (59) | 1.00 |
| Blood transfusion prior to 1986 | |||
| Yes | 71 | 8.45 (6) | 2.64 (1.02, 6.81) |
| No (Ref) | 2383 | 2.56 (61) | 1.00 |
| Sex with needle sharer ever | |||
| Yes | 397 | 4.03 (16) | 1.38 (0.63, 3.01) |
| No (Ref) | 2057 | 2.48 (51) | 1.00 |
| Sex with MSM ever | |||
| Yes | 79 | 10.13 (8) | 2.21 (0.85, 5.73) |
| No (Ref) | 2375 | 2.48 (59) | 1.00 |
| Sex-related conviction ever | |||
| Yes | 71 | 2.82 (2) | … |
| No | 5887 | 2.62 (154) | … |
| Drug-related conviction ever | |||
| Yes | 2488 | 3.58 (89) | 2.13 (1.21, 3.75) |
| No (Ref) | 3470 | 1.93 (67) | 1.00 |
| Mental health disorderb | |||
| Axis I | 379 | 3.69 (14) | 1.83 (0.72, 4.69) |
| Axis II | 272 | 1.10 (3) | 0.68 (0.09, 5.23) |
| Neither (Ref) | 5307 | 2.62 (139) | 1.00 |
| HCV | |||
| Positive | 557 | 18.31 (102) | … |
| Negative | 162 | 29.01 (47) | … |
| Syphilis | |||
| Positive | 352 | 4.26 (15) | 1.33 (0.55, 3.25) |
| Negative (Ref) | 5573 | 2.49 (139) | 1.00 |
| Tuberculosis | |||
| Positive | 57 | 5.26 (3) | … |
| Negative | 5901 | 2.59 (153) | … |
Note. OR = odds ratio; CI = confidence interval; GED = general equivalency diploma; MSM = men who have sex with men.
Using a sex worker or engaging in sex work.
Axis I: psychosis, bipolar disorder, major depression, generalized anxiety, and dementia. Axis II: personality disorder and developmental disability.
In the model-based analyses for women, there were statistically significant (P < .05) bivariate associations between HIV infection and age 35–44 years, Black race, other race, unemployment, IQ less than 100, previous imprisonment, crack or cocaine use, drug crimes, syphilis infection, and all conventional HIV risk behaviors except for needle sharing. In the multivariate analyses for women (Table 4), association with age was not detected, but women in the racial categories Black (OR = 4.34; 95% CI = 2.86, 6.59) and other (OR = 2.68; 95% CI = 1.02, 7.02) were more likely to be HIV infected than were Whites. Crack or cocaine use, drug crime conviction, and 13 or more months of previous incarceration were also associated with increased risk for HIV infection, although point estimates for these effects were all relatively modest (OR < 2).
HCV testing was limited to about 10% of the study population, but it was provided to almost all HIV-infected prisoners and to prisoners previously diagnosed with HCV. Because the population tested for HCV was small and unrepresentative of the population of prisoners tested for HIV, we do not present associations between HCV and HIV infection status here.
There were 32 241 male prisoners who went untested for HIV during the study period. We estimated that the prevalence of known male HIV cases in the state ranged from 0.02% to 2.08% across 15 age–race strata; the prevalence of HIV among male prisoners tested for HIV ranged from 0.18% to 9.64% across the 15 strata. On the basis of the state data, we estimated that 223 HIV-infected prisoners (24% of the estimated total) remained untested. When this estimate was based on the prevalence of HIV among tested prisoners, we estimated that 1101 HIV-infected prisoners (61% of the estimated total) remained untested (data available as a supplement to the online version of this article at http://www.ajph.org).
DISCUSSION
We have described the burden of HIV infection among prisoners tested for HIV, estimated a plausible range of the number of HIV cases among the untested prison population, and determined individual characteristics and behaviors associated with HIV infection among prisoners.
About 85% of female prisoners and 31% of male prisoners were tested for HIV during the study period. Among tested inmates, 2.6% of women and 3.6% of men were HIV infected. These estimates are greater than prevalence estimates from the neighboring state prison system in South Carolina (female 2.1%, male 2.2%),4 which tests all inmates for HIV. The estimates are also more than 6 times greater than those for the general North Carolina and United States populations (our calculation).13–15
Because the vast majority of the female prisoners received an HIV test, and because we found only modest differences in testing across demographic and behavioral characteristics, our estimate of the proportion testing positive (2.6%) reasonably estimates the prevalence of HIV in female inmates. For males, however, elective testing combined with a moderate testing rate likely resulted in a high estimate of seropositivity that is unrepresentative of the general male prison population.
With HIV test data from less than one third of all male prisoners, we estimated the number of HIV cases among the untested male prison population. Although our estimates of undetected HIV cases ranged widely, they could provide a useful guide when considering the potential public health benefits and the financial costs of expanded HIV testing (and subsequent treatment), as is now recommended by the CDC.6
In addition to HIV, infectious diseases such as TB, syphilis, hepatitis B, and HCV are common among correctional populations. Coinfection with these diseases can complicate HIV therapies and lead to greater morbidity and mortality. Of these infections, HCV is typically the most prevalent in correctional populations.1 Untreated HIV–HCV coinfection leads to shorter survival times and greater mortality than does HIV infection alone.16 In comparison with HCV infection alone, HIV–HCV coinfection leads to more rapid progression of liver fibrosis. HCV may also exacerbate the side effects of some antiretrovirals used to treat HIV, limiting their use.16 National estimates suggest that about 20% of the prison population is HCV infected.1 We found that in the NC DOC, more than 65% of HIV-positive prisoners were coinfected with HCV, a result similar to that reported among Maryland inmates.9 The high prevalence of HCV among HIV-positive prisoners underscores the need to coordinate HIV and HCV care, both in prison and after release.
Among male prisoners, most of the characteristics and behaviors we assessed were associated with HIV serostatus, but the majority of these associations were modest in magnitude (OR < 2). Exceptions included MSM (OR = 8.04) and, to a lesser degree, history of sharing needles (OR = 2.14). Age and race were moderately associated with HIV infection, with Black race (OR = 6.21), other race (OR = 7.36), and age 35–44 years (OR = 4.07) showing the strongest risk of infection.
Among female prisoners, ORs ranged between 2 and 3 for associations between HIV infection and multiple sexual partners, pre-1986 blood transfusion, sex with MSM, and drug-related imprisonments. Black race had the strongest association with HIV infection (OR = 3.57). In a study of females incarcerated in the Connecticut prison system, Altice et al. found that the strongest behavioral risk factor for HIV infection was sexual intercourse with an HIV-positive partner (OR = 9.1), followed by injection drug use (OR = 6.1).8 In that population, associations between HIV status and other risk factors such as noninjection drug use and race were of a magnitude similar to the associations we found in our study population. Two routine clinical laboratory markers, leukopenia (OR = 9.4) and hypoalbuminemia (OR = 7.2), were also associated with HIV infection among female Connecticut prisoners; but as is the case in the NC DOC, these data may not be routinely available in many correctional settings at intake, when testing is frequently offered.
The goal of targeted testing is to increase the efficiency of case detection. Twelve prison systems with voluntary HIV testing services report that they target high-risk inmates for HIV, but the specific criteria for testing have not been reported.4 In our study population, the modest strength of associations for most prisoner characteristics and behaviors suggests that targeted testing based on conventional HIV risk behaviors will likely miss a large proportion of HIV cases. This method of case detection is reliant upon prisoners' willingness to disclose sensitive behaviors. Among our study population, more than one half of HIV-positive prisoners with a recorded HIV risk assessment failed to disclose any risk behaviors. The high proportion of HIV-positive prisoners coinfected with HCV strongly suggests that, at the very least, injection drug use was greatly underreported.
Echoing the CDC's 2006 recommendations, we suggest that testing should be widely encouraged among all prisoners, because many will be unlikely to disclose risk behaviors. Encouragement, however, should not extend into coercion. As in the community, prisoners should maintain their right to accept or decline HIV testing. It is also imperative that, with expanded testing, prison systems provide adequate treatment services and bridge the divide between correctional health care and community health care. In the North Carolina prison system, HIV treatment is widely available, and programs to bridge correctional and community HIV care are currently being expanded.
Our study had a few known limitations. As we described, HIV risk assessments were not documented in 1 of the 2 intake facilities for women, limiting our examination of conventional HIV risk behaviors among women to 41% of the population. The records with missing data, however, corresponded to only about 6% of the total study population.
Most prisoners were assessed for HIV risk behaviors, but reluctance to disclose risk behaviors likely attenuated the magnitude of associations between risk behaviors and HIV infection. Although our data suggest the limited usefulness of targeted HIV testing, a more definitive assessment should include construction of receiver operator curves to evaluate the potential trade-off between sensitivity and specificity of different risk-factor–based testing algorithms. Also, collection of sensitive data could be improved in future investigations by the use of audio computer-assisted interviews,17 but that was not possible for this retrospective investigation.
Additionally, we were limited to serostatus results among prisoners voluntarily tested for HIV, and our estimates for males were based on less than one third of the male prison population. We have found that across several domains, male prisoners tested for HIV were dissimilar from male prisoners who remained untested in prison18; similarly, HIV-infected inmates included in this study may be different from infected inmates who remained untested and were thus excluded from this study. Finally, our results could have been biased by differential disclosure of seropositivity across groups of prisoners.
Prison systems continue to grapple with HIV testing and treatment in their facilities. The increased prevalence of HIV in correctional settings has been demonstrated repeatedly, but HIV prevalence varies regionally and across different demographic and risk groups.4,7,9,19,20 We have improved upon existing estimates of HIV burden among inmates in a large prison system in the South, and we estimated that between 23% and 63% of all HIV cases in prisons may be undetected. We found only moderate associations between HIV serostatus and most reported HIV risk behaviors, and relatively few prisoners acknowledged behaviors strongly associated with infection; thus, testing that is dependent upon prisoners' disclosure is likely to miss a substantial number of HIV infections. Prison systems predominantly testing high-risk inmates should reevaluate their testing policies in light of the 2003 and 2006 CDC recommendations.
Acknowledgments
This work was funded by a National Research Service Award from the National Institutes of Health (fellowship F30 MH077546-01).
The authors thank Peter Leone and Bill Miller for their thoughtful suggestions on an earlier version of this article. We also thank administrators and staff of the North Carolina Department of Correction for their assistance with this project. We dedicate this article to the late Andrew H. Kaplan, MD.
Human Participant Protection
This project was approved by institutional review boards at the University of North Carolina, Chapel Hill, and the North Carolina Department of Correction.
References
- 1.The Health Status of Soon-to-Be-Released Inmates: A Report to Congress. Chicago, IL: National Commission on Correctional Health Care; 2002. Vol 1 [Google Scholar]
- 2.Macalino GE, Vlahov D, Sanford-Colby S, et al. Prevalence and incidence of HIV, hepatitis B virus, and hepatitis C virus infections among males in Rhode Island prisons. Am J Public Health 2004;94(7):1218–1223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hammett TM, Gaiter JL, Crawford C. Reaching seriously at-risk populations: health interventions in criminal justice settings. Health Educ Behav 1998;25(1):99–120 [DOI] [PubMed] [Google Scholar]
- 4.Maruschak LM. HIV in Prisons, 2004. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2006 [Google Scholar]
- 5.Advancing HIV Prevention: Interim Technical Guidance for Selected Interventions. Atlanta, GA: Centers for Disease Control and Prevention; 2003 [Google Scholar]
- 6.Centers for Disease Control and Prevention Revised recommendations for HIV testing of adults, adolescentspregnant women in health-care settings. MMWR Recomm Rep 2006;55(RR14):1–17 [PubMed] [Google Scholar]
- 7.Altice FL, Mostashari F, Selwyn PA, et al. Predictors of HIV infection among newly sentenced male prisoners. J Acquir Immune Defic Syndr Hum Retrovirol 1998;18(5):444–453 [DOI] [PubMed] [Google Scholar]
- 8.Altice FL, Marinovich A, Khoshnood K, Blankenship KM, Springer SA, Selwyn PA. Correlates of HIV infection among incarcerated women: implications for improving detection of HIV infection. J Urban Health 2005;82(2):312–326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Solomon L, Flynn C, Muck K, Vertefeuille J. Prevalence of HIV, syphilis, hepatitis B, and hepatitis C among entrants to Maryland correctional facilities. J Urban Health 2004;81(1):25–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sabol WJ, Minton TD, Harrison PM. Prison and Jail Inmates at Midyear 2006. Washington, DC: Bureau of Justice Statistics, US Department of Justice; 2007 [Google Scholar]
- 11.HIV/AIDS Surveillance Report, 2005. Atlanta, GA: Centers for Disease Control and Prevention; 2007. Vol 17 [Google Scholar]
- 12.Sexually Transmitted and Other Reproductive Tract Infections: A Guide to Essential Practice. Geneva, Switzerland: World Health Organization; 2005 [Google Scholar]
- 13.Epidemiologic Profile for HIV/STD Prevention & Care Planning. Raleigh, NC: North Carolina Department of Health and Human Services; 2007 [Google Scholar]
- 14.Glynn M, Rhodes P. Estimated HIV prevalence in the United States at the end of 2003. Abstract presented at: National HIV Prevention Conference; 2005; Atlanta GA: Abstract T1-B1101 [Google Scholar]
- 15.US Census Bureau Annual Estimates of the Population for the United States, Regions, States, and for Puerto Rico: April 1, 2000 to July 1, 2006 (NST-EST2006-01). Available at: http://www.census.gov/popest/states/NST-ann-est.html Accessed August 15, 2007
- 16.Brau N. Chronic hepatitis C in patients with HIV/AIDS: a new challenge in antiviral therapy. J Antimicrob Chemother 2005;56(6):991–995 [DOI] [PubMed] [Google Scholar]
- 17.Macalino GE, Celentano DD, Latkin C, Strathdee SA, Vlahov D. Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-seronegative injection drug users. AIDS Educ Prev 2002;14(5):367–378 [DOI] [PubMed] [Google Scholar]
- 18.Rosen DL, Schoenbach VJ, Wohl DA, White BL, Stewart PW, Golin CE. An evaluation of HIV testing in a large Southern prison system. Am J Public Health 2009;suppl 2; In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoxie NJ, Chen MH, Prieve A, Haase B, Pfister J, Vergeront JM. HIV seroprevalence among male prison inmates in the Wisconsin Correctional System. WMJ 1998;97(5):28–31 [PubMed] [Google Scholar]
- 20.Wu ZH, Baillargeon J, Grady JJ, Black SA, Dunn K. HIV seroprevalence among newly incarcerated inmates in the Texas correctional system. Ann Epidemiol 2001;11(5):342–346 [DOI] [PubMed] [Google Scholar]


