Abstract
HIV continues to be transmitted at unacceptably high rates among African Americans, and most HIV-prevention interventions have focused on behavioral change.
To theorize additional approaches to HIV prevention among African Americans, we discuss how sexual networks and drug-injection networks are as important as behavior for HIV transmission. We also describe how higher-order social structures and processes, such as residential racial segregation and racialized policing, may help shape risk networks and behaviors. We then discuss 3 themes in African American culture—survival, propriety, and struggle—that also help shape networks and behaviors.
Finally, we conclude with a discussion of how these perspectives might help reduce HIV transmission among African Americans.
HIV is spreading faster among African Americans than it is among other US populations. Specific understanding of the dynamics of HIV transmission and of social structures and processes within and affecting African American communities may help us develop effective HIV prevention methods. To develop more effective HIV transmission among African Americans, we must develop a specific understanding of the dynamics of HIV transmission. In this essay, we present ideas about causal pathways that have received relatively little attention in the HIV/AIDS literature but that might contribute to African American's elevated HIV risk. These pathways suggest areas for future research and action.
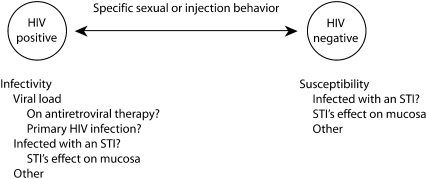
TRANSMISSION AS A CONDITIONAL PROBABILITY
HIV transmission occurs as a conditional probability. It requires, first of all, that an HIV-negative person be exposed to the virus. The vast majority of HIV transmission in the United States today occurs during sex or injection drug use. The probability that sex between serodiscordant individuals will result in HIV transmission may be elevated if either party has a sexually transmitted infection (STI). In observational studies, STIs appear to increase infectiousness in HIV-positive people and susceptibility in HIV-negative people.1–5 However, recent studies in which STIs have been treated without a concomitant reduction in HIV incidence cast some doubt on this hypothesis.6 Additionally, the infectiousness of an HIV-positive person depends on the person's viral load, which in turn depends upon the person's adherence level, how long the person has been infected, and whether the person is taking antiretroviral medications. Figure 1 illustrates this logic.
FIGURE 1.
Factors in a potential HIV transmission event.
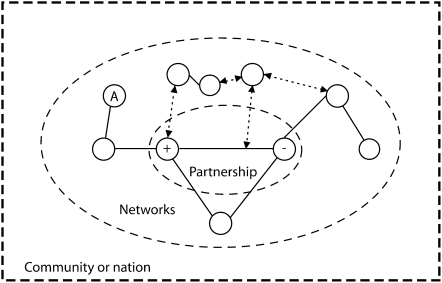
The probability that an uninfected person will have an infected sexual or injection partner is a function of both parties' particular social and behavioral histories, their places in social and risk networks, and the combination of social factors and choices that lead them to have sex or inject with particular partners. Networks are links among people; in “social networks” these links are social ties, and in “risk networks” they are ties among people that can spread disease. HIV-risk networks composed of sexual and drug-injection linkages, together with related social-network links, are illustrated in Figure 2. Each risk-network or social-network member possesses an array of relevant characteristics, such as race/ethnicity, gender, HIV status, STI status, the extent to which they engage in normative communication (intravention), the content of any intravention, the strands of racial/ethnic culture in which they are embedded (a concept that is explained later), factors that limit behavioral choice (such as financial need to engage in survival sex, dependence on a sexual partner, housing constraints due to urban desertification,7,8 or drug addiction), and their attitudes to social, prevention, and medical services, among many others. The immediate network of a partnership also has its own HIV prevalence, which may affect the rate of new infections within the network.
FIGURE 2.
The contexts of sexual and drug-injecting partnerships.
Note. Circles represent people, solid lines represent shared sexual or injection behaviors, dotted lines represent social influence and normative communication, and dashed lines represent levels of analysis.
HIV infection often clusters among certain parts of a risk network,9 which is hardly surprising given that HIV transmission occurs through the high-risk behavior linkages that connect people in a network. Sexual networks also structure patterns of STIs and the consequent impacts on infectiousness and susceptibility to HIV.10–14 Social-influence networks are considerably denser than injecting and sexual networks, because most people interact with more people who influence them, or whom they influence, than with sexual or injecting partners.
The characteristics of personal sexual and injection networks are important for understanding racial/ethnic disparities in infection with HIV and other STIs. African Americans are more likely to have HIV-positive injection and sexual partners than are Whites.15–17 These disparities result from a combination of the higher prevalence rates of HIV and other STIs among African Americans and a high degree of assortative mixing, i.e., the tendency of members of racial/ethnic groups to have sex or inject drugs with partners from within their own group. This finding helps explain why infection rates are currently higher among African Americans, but it cannot explain how these disparities originated.17 There is no evidence that racial/ethnic disparities in infection rates result from differences in rates of high-risk sexual or injection behaviors per se.
We believe that research on sexual and injection networks in many communities over time is sorely needed to understand why African Americans have higher HIV infection rates. Little of this research has been conducted,18 but it would help us to learn whether and how networks of African Americans differ from networks of other racial/ethnic groups. This kind of research would also allow us to study how the structures and processes presented in Figures 2 and 3 affect network location and structure, and how these effects operate over time.7,8,17 For example, we know that behavioral subgroups may create subcultural ties that lead to sexual or drug-injection ties. This process is clearest for subcultures that form around attendance at group-sex parties, but sexual networks also seem to occur within drug-using subcultures, which may lead to sexual ties being formed between injecting and noninjecting drug users.19
FIGURE 3.
Racialized social structures and processes as a context for HIV-relevant cultural themes, subcultures, networks, and behaviors among African Americans.
Understanding the behaviors that people engage in with each other is also important because behavior change can reduce HIV transmission. Factors that affect a person's behavior include personal characteristics such as knowledge and attitudes, social norms through which social network members exert influence on the person's behaviors, the personal characteristics of the person's partner, the social normative pressures to which the person is subjected, and the partners' discussions and negotiations concerning the specific behaviors in which they will engage. Like all negotiations, these behavioral negotiations are shaped in part by the resources and social relationships of the people who engage in them. Risk and protective behaviors are also shaped by broader cultural contexts, the actions of social-control agencies such as police (whose tactics may be particularly likely to affect drug-using behaviors, commercial sex activities, and highly stigmatized behaviors such as male–male partner seeking in public environments), and the nature and availability of social and medical services relevant to these behaviors.20
SELECTED DYNAMICS OF HIV/AIDS AMONG AFRICAN AMERICANS
Given this model of HIV transmission through communities, it is clear that HIV transmission and prevention within African American communities should be influenced both by outside forces and structures that shape the economics, culture, social networks, sexual and drug-using networks, and social and medical care of African Americans, and by cultural, social, and political actions, forces, and structures within the African American community. Many of these influencing factors are racialized—that is, structured in accordance with racial categories—in ways that are almost always to the disadvantage of African Americans and other subordinated racial/ethnic groupings. Figure 3 presents some of these interacting forces and processes diagrammatically. It differs from the model presented by Farley17 in giving greater attention to the specificities of racism, the cultural themes among African Americans, and how these relate to sexual and injection behaviors and their associated risk networks.
It would take many volumes to discuss what is known about the myriad forces, structures, and histories of action that have come together to produce the current high rates of HIV infection and mortality among African Americans. We obviously cannot present this mass of material here. Instead, we emphasize materials that we think have been understudied or underutilized, and we do so within an overall framework that may help us understand how to synthesize existing research and identify issues on which too little research has been conducted. We focus the remainder of this review on some understudied aspects of the relationships of different cultural themes to risk behaviors and of the relationships of social control interventions to HIV-risk and protective behaviors and networks.
This restriction is very selective. For example, we do not discuss the inadequate social and medical resources available to African Americans21 and the role that this inadequacy plays in creating the long delays between STI or HIV infection and treatment among African Americans.
CULTURE, RISK BEHAVIORS, AND PROTECTIVE BEHAVIORS
As we consider how behaviors among African Americans are shaped, it is important to remember that infections are not a simple product of behavior alone. This is demonstrated by studies showing that although African Americans have higher rates of HIV than do other US populations, they do not have higher rates of sexual risk behaviors.16,22 Nor are African Americans more likely to use drugs than other are racial/ethnic groups, although they may have higher (but still low) rates of drug injection than do other US populations.23 Rather, explanations for African Americans' higher HIV rates probably lie in racial/ethnic oppression, such as discriminatory rates of arrest and incarceration,24 economic deprivation, inadequate access to medical and social care, and differences in the density, turnover, or concurrency of risk networks. Still, risk behavior is important, and interventions to reduce behavioral risk can reduce rates of HIV transmission.25–27
As discussed earlier, culture—particularly social norms and values—helps shape behavior. There is a widespread consensus in the HIV-prevention field that those conducting behavioral interventions must be “culturally competent” in the culture of the population in which they work. Wyatt et al.28 have recently discussed the need to take account of and conduct research on cultural variation within the African American community regarding sexuality. To better understand such cultural variations, we must examine the constitutive elements of African American culture and how they interact with sexual and drug-use subcultures, networks, and behaviors.
Wyatt et al.,28 Chapman and Berggren,29 and Marshall30 agree with Du Bois31 that African American culture has developed through a dialectical interaction among a history of oppression, struggles to survive within an oppressive social order, struggles against oppression, and the various other developments and struggles occurring within the broader community, national, and global social orders. These interactions and experiences have created a mixture of beliefs, ideals, values, norms, and myths within African American populations, meaning that any given African American group or individual has access to a rich variety of cultural traditions as guides for interpretation and action.
Thus, “culturally competent” public health intervention or intravention must be able to understand how these cultural traditions and themes can operate to increase or decrease risk, or to support or oppose public policies or programs to prevent HIV infection. However, to the best of our knowledge, there has been very little discussion of what these themes are within African American culture, how they interact within individuals, families, or larger groups, and how they can best be understood.
RELEVANT THEMES IN AFRICAN AMERICAN CULTURE
We propose that several discrete and interacting cultural themes can be observed in the African American response to the HIV/AIDS epidemic. Research that studies these interacting—and somewhat conflicting—themes in some depth may be very valuable in helping to shape future efforts to prevent HIV transmission among African Americans. (These themes appear inside the box in Figure 3.)
Survival
A “survival” theme is consistently present in African American culture. A subset of the survival theme is the “code of the streets” that Elijah Anderson32 discusses, which centers around a need in some neighborhoods for men to preserve a reputation as being willing to respond to provocation with violence. This code also emphasizes manhood as physicality and as men “scoring” with women sexually. The code of the streets creates cultural environments conducive to high-risk sex, drug dealing, and drug use.
A more positive element of the survival theme is the rapid spread of messages of danger and of ways to avoid it through community grapevines. We noted this as a possible reason why African American drug injectors reduced several high-risk behaviors to avoid HIV/AIDS more than did either White or Hispanic injectors in New York City in the 1980s.33
The reluctance of some African Americans to participate in some forms of medical care or scientifically supported risk reduction may also have its roots in the survival theme, given African Americans' long history of medical apartheid and medical mistreatment in the United States.34–37 The same might be true for the belief that the government created HIV/AIDS to kill Africans and African Americans.38 These attitudes might lead some African Americans to avoid HIV testing or treatment. In addition, the belief that HIV/AIDS was created to kill African Americans may interact with beliefs that family planning is an attempt to reduce the number of African Americans, causing reductions in condom use.39
Propriety
The socially conservative and traditionally moralistic “propriety” theme reflects the widespread religious involvement of many African Americans and the tendency of oppressed groups to conform to the “official” norms of the dominant social order.28,40–43 This theme has contributed to the reluctance of many African American parents to discuss sex with their children28 and to the reluctance of many African American politicians, media outlets, churches, and other organizations to address HIV or to support some HIV prevention interventions, such as syringe exchange.40,44 Discussing sex or HIV or establishing programs to prevent HIV among drug users tends to involve talking about “improper” subjects. If such activities are conducted in public, there is a further concern about accepting the racist stigmatization of African Americans as centers of sexual impropriety and drug use.
The propriety theme may also delay or prevent risky sex or drug behavior in some youth, although we are unaware of any research on this topic. In our experience training frontline HIV public health workers and staff of drug abuse treatment centers, we found that some African American service providers exhibited adherence to the propriety theme during their training. They tended to stigmatize drug use and nontraditional sex. Although many of the drug treatment workers have accepted risk-reduction approaches to drug use, they continue to view sexual risk through perspectives that emphasize abstinence and morality rather than risk reduction. Because a large amount of HIV transmission among both injecting and noninjecting drug users occurs sexually,45–48 the strength of the propriety theme among some African American drug service providers may contribute to high rates of HIV transmission.
Struggle
The “struggle” theme in African American culture has grown out of long traditions of both micropolitical struggle49 and more overtly political movements against oppression, both within institutions and in the nation as a whole. (“Micropolitical struggle” refers to the numerous but often-overlooked small-scale contestations between local groups of oppressed people and those who dominate them.)
One form taken by this struggle theme is that many African Americans who are responding to the HIV epidemic as outreach workers, researchers, or policymakers have pasts in the freedom and Black Power movements of the 1960s and 1970s. These pasts often lead these African Americans to see HIV policies and programs as continuations of past struggles. Their valuable experiences have also given them skills in working with people both collectively and through individual “counseling” interactions.
Both Cohen40 and Quimby and Friedman44 discuss other aspects of the struggle theme. They present data showing that many African American organizations and officials in New York City and elsewhere responded slowly and unsympathetically to HIV among injection drug users, sex workers, and men who have sex with men. In these authors' analyses, after the uprisings (sometimes called “riots”) of the 1960s and early 1970s, many community organizations, including some drug treatment programs, churches, and community groups, received money and other support from governments and philanthropic bodies in exchange for these organizations functioning as agencies to help control discontent. Over time, this role melded with the status-based propriety-theme moralism that historically has pervaded “respectable” middle-class Black organizations, with the result that these agencies have sometimes responded slowly to the HIV/AIDS epidemic or have opposed certain initiatives, such as syringe exchange.
A better understanding of the dynamics of the struggle theme can inform responses to conflicting interpretations of how HIV/AIDS policy, prevention, and treatment initiatives fit into African American struggles, thus perhaps helping these initiatives win community acceptance.
We know little about how these cultural themes interact with the norms and values of sexual and drug-using subcultures to affect risk and protective behaviors; likewise, we know little about how these themes shape local HIV prevention and care programs. Research on these issues could be highly valuable to public health efforts.
SOCIAL-CONTROL INTERVENTIONS, RISK BEHAVIORS, AND RISK NETWORKS
The United States is the most repressive country in the world in terms of the proportion and number of residents incarcerated.50 Incarceration in the United States is highly racialized. At the beginning of 2008, more than 1 in every 100 US adults was incarcerated in a US prison or jail. The proportion of African American men who were incarcerated dwarfs this national figure, however: 1 in every 15 African American men is behind bars.
Police are less likely to prevent open drug markets or commercial sex markets in poor African American and other “oppressed minority” sections of cities than in White areas. 9,51,52 This means that outsiders with money—whether African American, White, or otherwise—come to these areas to buy drugs or sexual services, which can be a significant portion of the income coming into some very poor neighborhoods. This money may lure some local youth into the drug trade or the sex trade and thence into unsafe sexual or injecting behaviors.
Racialized processes of police patrol, arrests, and incarceration may also affect the structures of sexual and injection networks in these localities. Because men are more likely to be incarcerated than women, the resulting low male-to-female ratios may reduce women's ability to negotiate condom use, may lead men to have more sexual partners, and may create higher concurrency in community sexual networks. Furthermore, arrests increase network turnover by removing people from existing sexual and injection relationships. When arrested people return to the community, they may reestablish their previous relationships without disrupting ties formed in their absence. This would create larger networks with more members who engage in risk behaviors with larger numbers of other persons, resulting in a community network with higher levels of concurrency, turnover, and centrality, which can increase the spread of HIV through a community.11–14,53
Policing also directly affects high-risk drug-use behaviors, networks, and interventions. Drug injectors who reside in areas where policing leads them to fear arrest and punishment may avoid syringe exchanges,54–56 may inject more rapidly and thus with less effort to avoid infection,57–59 or may inject in multiperson injection spots (e.g., shooting galleries)60 to escape detection. All of these behaviors are associated with riskier injection practices.56,60–62 Arrests may likewise increase risk among commercial sex workers and men who seek male sex partners in street venues.
WHAT INTERVENTIONS MIGHT BE FEASIBLE FOR WHOM?
A wide variety of HIV interventions exist. One critical question to ask of any intervention is: Who is the intervention agent? Given the array of causal structures and relationships we have discussed, it is clear that changing some of these structures or relationships may require large-scale sociopolitical movements; other structures or relationships may be changed by public health agencies working in conjunction with health service providers and community-based organizations; and changing other relationships or structures may require collective activity—whether organized as intravention processes or as collective self-organization—from the populations at risk. 63–66
In light of these facts, we suggest that the following areas require research or action from public health professionals and agencies to reduce HIV among African Americans. (These suggestions are not meant to deny the importance of traditional behavioral interventions, syringe exchange, condom distribution in prisons, or other efforts; we simply seek to highlight areas that may be less salient in other contexts.)
First, given the ways that social networks and subcultures shape behaviors and structure the flow of STIs through communities, much could be learned if the Centers for Disease Control and Prevention and other health agencies were to alter their HIV surveillance methodologies to obtain drug use and STI data as well as the traditional “risk group” data. Studies have shown that HIV, genital herpes, syphilis, and perhaps other STIs may be particularly prevalent among both noninjecting and injecting users of heroin, methamphetamines, cocaine, and crack.67–69 To the (currently debated) extent that STIs facilitate HIV transmission,6 and given the elevated rate of STIs among African Americans,70–72 we suggest that HIV and STI prevention and care among African American drug users (both injection and noninjection) might help reduce HIV transmission. Such efforts should be mounted immediately in jails, prisons, drug treatment programs, harm reduction agencies, and STI treatment centers. In addition, harm reduction and drug treatment efforts should be located where people go for STI treatment.
Another major implication of this paper is that social-justice struggles that counteract the racialized economic, social control, and other macro-level social processes that form the outer set of circles in Figure 3 are an important part of HIV prevention in African American populations. One pathway through which this activity can and should occur is large-scale social movements that build upon, deepen, and transform the struggle cultures of African Americans and others. Most governmental health agencies will have at best a limited role to play in such social movements and indeed may intervene to restrain them. Employees of these agencies may be able to be more active than the agencies themselves.
In some instances, health departments, the Centers for Disease Control and Prevention, and other agencies already are addressing HIV-related aspects of policing, social control, and incarceration. For example, in some jurisdictions, agencies within or funded by local governments provide harm reduction training to police so that police officers do not harass syringe exchange clients or sex traders, which greatly facilitates HIV-related risk reduction. These efforts can be extended to incorporate joint health department and police development of police strategies that do not encourage HIV transmission or that reduce incarceration rates, thus reducing the network turnover and concurrency that incarceration produces.
Finally, community groups and health agencies might consider efforts to establish HIV/AIDS impact assessments (including attention to their possible impacts on racial/ethnic disparities) as review criteria for community redevelopment proposals, police activities, and other community activities.
Acknowledgments
Support for this article was obtained from the National Institute of Drug Abuse (grants R01 DA13336, P30 DA11041, and 1R21DA023391-01).
We would like to acknowledge the intellectual contributions of Benjamin Bowser and Anthony Lemelle to this article.
Human Participant Protection
No protocol approval was necessary because the writing of this article did not involve human research participants.
References
- 1.Chan DJ. Fatal attraction: sex, sexually transmitted infections and HIV-1. Int J STD AIDS 2006;17:643–651 [DOI] [PubMed] [Google Scholar]
- 2.Berman SM, Cohen MS. STD treatment: how can it improve HIV prevention in the South? Sex Transm Dis 2006;33:S50–S57 [DOI] [PubMed] [Google Scholar]
- 3.Quinn T. Association of sexually transmitted diseases and infection with the human immunodeficiency virus: biological cofactors and markers of behavioural interventions. Int J STD AIDS 1996;7(suppl 2):17–24 [DOI] [PubMed] [Google Scholar]
- 4.Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect 1999;75:3–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coombs RW, Reichelderfer PS, Landay AL. Recent observations on HIV type-1 infection in the genital tract of men and women. AIDS 2003;17:455–480 [DOI] [PubMed] [Google Scholar]
- 6.Gray RH, Wawer MJ. Reassessing the hypothesis on STI control for HIV prevention. Lancet 2008;371:2064–2065 [DOI] [PubMed] [Google Scholar]
- 7.Wallace R. Social disintegration and the spread of AIDS–II. Meltdown of sociogeographic structure in urban minority neighborhoods. Soc Sci Med 1993;37:887–896 [DOI] [PubMed] [Google Scholar]
- 8.Wallace D, Wallace R. A Plague on Your Houses New York, NY: Verso; 1998 [Google Scholar]
- 9.Friedman S, Curtis R, Neaigus A, Jose B, Des Jarlais DC. Social Networks, Drug Injectors' Lives, and HIV/AIDS. New York, NY: Kluwer/Plenum; 1999 [Google Scholar]
- 10.Potterat JJ, Muth SQ, Rothenberg RB, et al. Sexual network structure as an indicator of epidemic phase. Sex Transm Infect 2002;78(suppl 1):i152–i158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Potterat JJ, Zimmerman-Rogers H, Muth SQ, et al. Chlamydia transmission: concurrency, reproduction number, and the epidemic trajectory. Am J Epidemiol 1999;150:1331–1339 [DOI] [PubMed] [Google Scholar]
- 12.Potterat JJ, Rothenberg RB, Muth SQ. Network structural dynamics and infectious disease propagation. Int J STD AIDS 1999;10:182–185 [DOI] [PubMed] [Google Scholar]
- 13.Rothenberg RB, Sterk C, Toomey KE, et al. Using social network and ethnographic tools to evaluate syphilis transmission. Sex Transm Dis 1998;25:154–160 [DOI] [PubMed] [Google Scholar]
- 14.Rothenberg RB, Potterat JJ, Woodhouse DE, Muth SQ, Darrow WW, Klovdahl AS. Social network dynamics and HIV transmission. AIDS 1998;12:1529–1536 [DOI] [PubMed] [Google Scholar]
- 15.Kottiri BJ, Friedman SR, Neaigus A, Curtis R, Des Jarlais DC. Risk networks and racial/ethnic differences in the prevalence of HIV infection among injection drug users. J Acquir Immune Defic Syndr 2002;30:95–104 [DOI] [PubMed] [Google Scholar]
- 16.Hallfors DD, Iritani BJ, Miller WC, Bauer DJ. Sexual and drug behavior patterns and HIV and STD racial disparities: the need for new directions. Am J Public Health 2007;97:125–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farley TA. Sexually transmitted diseases in the Southeastern United States: location, race, and social context. Sex Transm Dis 2006;33:S58–S64 [DOI] [PubMed] [Google Scholar]
- 18.Friedman SR, Bolyard M, Mateu-Gelabert P, et al. Some data-driven reflections on priorities in AIDS network research. AIDS Behav 2007;11:641–651 [DOI] [PubMed] [Google Scholar]
- 19.Friedman S, Bolyard M, Khan M, et al. Group sex events and HIV/STI risk in an urban network. J Acquir Immune Defic Syndr 2009;49:440–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedman S, Rossi D, Phaswana-Mafuya N. Globalization and interacting large-scale processes and how they may affect the HIV/AIDS epidemic. In: Pope C, White R, Malow R, eds HIV/AIDS: Stories of a Global Epidemic New York, NY: Routledge; 2008:491–500 [Google Scholar]
- 21.Smedley B, Stith A, Nelson A. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: National Academies Press; 2003 [PMC free article] [PubMed] [Google Scholar]
- 22.National Institute on Drug Abuse Drug Use Among Racial/Ethnic Minorities. Bethesda, MD: National Institutes of Health; 2003. NIH publication 03-3888 [Google Scholar]
- 23.Cooper H, Friedman SR, Tempalski B, Friedman R, Keem M. Racial/ethnic disparities in injection drug use in large US metropolitan areas. Ann Epidemiol 2005;15:326–334 [DOI] [PubMed] [Google Scholar]
- 24.Friedman SR, Cooper HL, Tempalski B, et al. Relationships of deterrence and law enforcement to drug-related harms among drug injectors in US metropolitan areas. AIDS 2006;20:93–99 [DOI] [PubMed] [Google Scholar]
- 25.HIV/AIDS Prevention Research Synthesis Project Compendium of HIV Prevention Interventions With Evidence of Effectiveness. Atlanta, GA: Centers for Disease Control and Prevention; 1999 [Google Scholar]
- 26.Kirby D, Short L, Collins J, et al. School-based programs to reduce sexual risk behaviors: a review of effectiveness. Public Health Rep 1994;109:339–360 [PMC free article] [PubMed] [Google Scholar]
- 27.Lyles CM, Kay LS, Crepaz N, et al. Best-evidence interventions: findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000–2004. Am J Public Health 2007;97:133–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wyatt GE, Williams JK, Myers HF. African-American sexuality and HIV/AIDS: recommendations for future research. J Natl Med Assoc 2008;100:44–48, 50–51 [DOI] [PubMed] [Google Scholar]
- 29.Chapman RR, Berggren JR. Radical contextualization: contributions to an anthropology of racial/ethnic health disparities. Health (London) 2005;9:145–167 [DOI] [PubMed] [Google Scholar]
- 30.Marshall WE. AIDS, race and the limits of science. Soc Sci Med 2005;60:2515–2525 [DOI] [PubMed] [Google Scholar]
- 31.Du Bois W. The Souls of Black Folk: Essays and Sketches Chicago, IL: A. C. McClurg; 1903 [Google Scholar]
- 32.Anderson E. Code of the Street New York, NY: W. W. Norton; 1999 [Google Scholar]
- 33.Friedman SR, Sotheran JL, Abdul-Quader A, et al. The AIDS epidemic among Blacks and Hispanics. Milbank Q 1987;65:455–499 [PubMed] [Google Scholar]
- 34.Gamble VN. A legacy of distrust: African Americans and medical research. Am J Prev Med 1993;9:35–38 [PubMed] [Google Scholar]
- 35.Thomas SB, Quinn SC. The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the black community. Am J Public Health 1991;81:1498–1505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shavers-Hornaday VL, Lynch CF, Burmeister LF, Torner JC. Why are African Americans under-represented in medical research studies? Impediments to participation. Ethn Health 1997;2:31–45 [DOI] [PubMed] [Google Scholar]
- 37.Washington H. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans From Colonial Times to the Present. New York, NY: Doubleday Broadway Publishing Group; 2007 [Google Scholar]
- 38.Bogart LM, Thorburn S. Relationship of African Americans' sociodemographic characteristics to belief in conspiracies about HIV/AIDS and birth control. J Natl Med Assoc 2006;98:1144–1150 [PMC free article] [PubMed] [Google Scholar]
- 39.Ross MW, Essien EJ, Torres I. Conspiracy beliefs about the origin of HIV/AIDS in four racial/ethnic groups. J Acquir Immune Defic Syndr 2006;41:342–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cohen C. The Boundaries of Blackness: AIDS and the Breakdown of Black Politics. Chicago, IL: University of Chicago Press; 1999 [Google Scholar]
- 41.Lanternari V. The Religions of the Oppressed New York, NY: Alfred A. Knopf; 1963 [Google Scholar]
- 42.Mattis JS. Religion and African American political life. Polit Psychol 2001;22:263–278 [Google Scholar]
- 43.Miller RL., Jr African American churches at the crossroads of AIDS. Focus 2001;16:1–4 [PubMed] [Google Scholar]
- 44.Quimby E, Friedman SR. Dynamics of black mobilization against AIDS in New York City. Soc Probl 1989;36(4):403–415 [Google Scholar]
- 45.Doherty MC, Garfein RS, Monterroso E, Brown D, Vlahov D. Correlates of HIV infection among young adult short-term injection drug users. AIDS 2000;14:717–726 [DOI] [PubMed] [Google Scholar]
- 46.Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and non-injection drug users. J Urban Health 2003;80:iii7–iii14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kral AH, Bluthenthal RN, Lorvick J, Gee L, Bacchetti P, Edlin BR. Sexual transmission of HIV-1 among injection drug users in San Francisco, USA: risk-factor analysis. Lancet 2001;357:1397–1401 [DOI] [PubMed] [Google Scholar]
- 48.Neaigus A, Miller M, Friedman SR, et al. Potential risk factors for the transition to injecting among non-injecting heroin users: a comparison of former injectors and never injectors. Addiction 2001;96:847–860 [DOI] [PubMed] [Google Scholar]
- 49.Scott J. Domination and the Arts of Resistance: Hidden Transcripts. New Haven, CT: Yale University Press; 1990 [Google Scholar]
- 50.The Pew Center on the States 1 in 100: Behind Bars in America 2008. Washington, DC: The Pew Charitable Trust; 2008 [Google Scholar]
- 51.Friedman SR, Mateu-Gelabert P, Curtis R, et al. Social capital or networks, negotiations, and norms? A neighborhood case study. Am J Prev Med 2007;32:S160–S170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Curtis R, Friedman S, Neaigus A, Jose B, Goldstein M, Ildefonso G. Street-level drug market structure and HIV risk. Soc Networks 1995;17(3–4):229–249 [Google Scholar]
- 53.Adimora AA, Schoenbach VJ, Martinson FE, Donaldson KH, Fullilove RE, Aral SO. Social context of sexual relationships among rural African Americans. Sex Transm Dis 2001;28:69–76 [DOI] [PubMed] [Google Scholar]
- 54.Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Med Anthropol 1997;18:61–83 [DOI] [PubMed] [Google Scholar]
- 55.Davis CS, Burris S, Kraut-Becher J, Lynch KG, Metzger D. Effects of an intensive street-level police intervention on syringe exchange program use in Philadelphia, PA. Am J Public Health 2005;95:233–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors' ability to practice harm reduction: a qualitative study. Soc Sci Med 2005;61:673–684 [DOI] [PubMed] [Google Scholar]
- 57.Maher L, Dixon D. Policing and public health: law enforcement and harm minimization in a street-level drug market. Br J Criminol 1999;39(4):488–512 [Google Scholar]
- 58.Strike C, Myers T, Millson M. Finding a place for needle exchange programs. Crit Public Health 2004;14(3):261–275 [Google Scholar]
- 59.Aitken C, Moore D, Higgs D, Kelsall J, Kerger M. The impact of a police crackdown on a street drug scene: evidence from the street. Int J Drug Policy 2002;13(3):193–202 [Google Scholar]
- 60.Tempalski B. The Uneven Geography of Syringe Exchange Programs in the United States: Need, Politics, and Place. Seattle, WA: Department of Geography, University of Washington; 2005 [Google Scholar]
- 61.Bluthenthal R, Kral A, Erringer E, Edlin BR. Drug paraphernalia laws and injection-related infectious disease risk among drug injectors. J Drug Issues 1999;29(1):1–16 [Google Scholar]
- 62.Bluthenthal R, Lorvick J, Kral A, Erringer E, Kahn JG. Collateral damage in the war on drugs: HIV risk behaviors among injection drug users. Int J Drug Policy 1999;10(1):25–38 [Google Scholar]
- 63.Friedman S, Des Jarlais D, Ward TP. Social models for changing health-relevant behavior. In: DiClemente R, Peterson J, eds Preventing AIDS: Theories & Methods of Behavioral Interventions New York, NY: Plenum Press; 1994:95–116 [Google Scholar]
- 64.Friedman SR, de Jong W, Rossi D, et al. Harm reduction theory: users' culture, micro-social indigenous harm reduction, and the self-organization and outside-organizing of users' groups. Int J Drug Policy 2007;18:107–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Friedman SR, Maslow C, Bolyard M, Sandoval M, Mateu-Gelabert P, Neaigus A. Urging others to be healthy: “intravention” by injection drug users as a community prevention goal. AIDS Educ Prev 2004;16:250–263 [DOI] [PubMed] [Google Scholar]
- 66.Friedman SR, Bolyard M, Maslow C, Mateu-Gelabert P, Sandoval M. Harnessing the power of social networks to reduce HIV risk. Focus 2005;20:5–6 [PubMed] [Google Scholar]
- 67.Adimora AA, Schoenbach VJ, Martinson FE, et al. Heterosexually transmitted HIV infection among African Americans in North Carolina. J Acquir Immune Defic Syndr 2006;41:616–623 [DOI] [PubMed] [Google Scholar]
- 68.Friedman SR, Flom PL, Kottiri BJ, et al. Drug use patterns and infection with sexually transmissible agents among young adults in a high-risk neighbourhood in New York City. Addiction 2003;98:159–169 [DOI] [PubMed] [Google Scholar]
- 69.Sena AC, Muth SQ, Heffelfinger JD, O'Dowd JO, Foust E, Leone P. Factors and the sociosexual network associated with a syphilis outbreak in rural North Carolina. Sex Transm Dis 2007;34:280–287 [DOI] [PubMed] [Google Scholar]
- 70.Eng T, Butler W, eds The Hidden Epidemic: Confronting Sexually Transmitted Diseases. Washington, DC: National Academies Press; 1997 [PubMed] [Google Scholar]
- 71.Laumann EO, Youm Y. Racial/ethnic group differences in the prevalence of sexually transmitted diseases in the United States: a network explanation. Sex Transm Dis 1999;26:250–261 [DOI] [PubMed] [Google Scholar]
- 72.Xu F, Sternberg MR, Kottiri BJ, et al. Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States. JAMA 2006;296:964–973 [DOI] [PubMed] [Google Scholar]