Abstract
Objectives. We evaluated the efficacy of a primary care intervention targeting pregnant African American women and focusing on psychosocial and behavioral risk factors for poor reproductive outcomes (cigarette smoking, secondhand smoke exposure, depression, and intimate partner violence).
Methods. Pregnant African American women (N = 1044) were randomized to an intervention or usual care group. Clinic-based, individually tailored counseling sessions were adapted from evidence-based interventions. Follow-up data were obtained for 850 women. Multiple imputation methodology was used to estimate missing data. Outcome measures were number of risks at baseline, first follow-up, and second follow-up and within-person changes in risk from baseline to the second follow-up.
Results. Number of risks did not differ between the intervention and usual care groups at baseline, the second trimester, or the third trimester. Women in the intervention group more frequently resolved some or all of their risks than did women in the usual care group (odds ratio = 1.61; 95% confidence interval = 1.08, 2.39; P = .021).
Conclusions. In comparison with usual care, a clinic-based behavioral intervention significantly reduced psychosocial and behavioral pregnancy risk factors among high-risk African American women receiving prenatal care.
Adverse pregnancy outcomes are particularly common among women who are members of racial/ethnic minority groups.1–4 African American infants are 3.4 times more likely than are White infants to die in the neonatal period, a disadvantage that persists even when mothers have appropriately early and equal access to prenatal care.5 In Washington, DC, death rates among non-Hispanic African American infants remain unacceptably high (17.0 per 1000 live births in 2005) despite an overall decline in infant mortality from 18.6 per 1000 live births in 1992 to 14.0 per 1000 births in 2005.6 Psychosocial and behavioral risks are recognized as potential contributors to poor reproductive outcomes.7–9 Poverty,10 limited social support,11 smoking,12 illicit drug use,13 depression,14 anxiety,14,15 and intimate partner violence (IPV)16,17 are all associated to varying degrees with pregnancy complications, premature and low-birthweight deliveries, stillbirths, and infant mortality.
There is increasing recognition of the role of primary care in screening, diagnosis, and treatment of behavioral, mental health, and psychosocial concerns,18–27 because of the significant association between medical morbidity and behavioral and mental health problems.28 Although interventions involving primary care providers may have limited success, they can be cost-effective.18,24 Because access to and use of behavioral and mental health care remain problematic, especially among members of underserved minority groups,29–32 making such care available through primary care services may avert missed opportunities.
Prenatal care may be a venue to address behavioral and mental health issues that can potentially affect the health of pregnant women and their unborn children.33 The guidelines of the American College of Obstetrics and Gynecology and the American Academy of Pediatrics34,35 suggest ways primary care providers can screen for behavioral and psychosocial risk factors. Despite these guidelines, many providers still fail to screen pregnant women,35–38 with screening rates varying according to type of provider,36,39 risk factors,36 population group,40 and provider risk perceptions.41 Furthermore, when implemented, psychosocial and behavioral interventions have been only moderately successful.42,43
Such inconsistent results may arise from multiple factors, including differences in study design, participant engagement, and intervention content or implementation, including approaches that address only 1 of multiple, co-occurring psychosocial or behavioral risk factors. Behavioral and psychosocial factors associated with poor pregnancy outcomes are related to and serve as risk factors for one another44; therefore, an alternative approach would be to provide an intervention simultaneously addressing multiple psychosocial and behavioral risk factors among pregnant women, as has been done in relation to other health risks.45–47
A recent study focusing on 3569 Medicaid-eligible pregnant women examined the effects of the Prenatal Plus Program in Colorado with respect to smoking, inadequate prenatal weight gain, and “psychosocial problems” (defined as “significant or severe stress as a result of personal or family safety needs, lack of support systems, or an inability to meet basic needs”).48(p1955) Women who had at least 10 Prenatal Plus visits were more likely than were women who did not to reduce these risks; in addition, only 7.0% of women who resolved all of their risks delivered low-birthweight infants, whereas 13.2% of those who resolved none of their risks did so. In spite of these promising results, the nonexperimental nature of the Colorado study may have created unquantifiable biases favoring the intervention.
Moreover, only 4% of all births in Colorado, and 7% of Prenatal Plus deliveries, occurred among African American women, the group at greatest risk of adverse pregnancy outcomes. Thus, further experimental investigations in which rigorous randomized trial designs are used to assess vulnerable African American women are needed to better appreciate the potential merits of an integrated intervention focusing on psychosocial and behavioral risk factors during pregnancy.
We conducted a randomized clinical trial testing the efficacy of an integrated intervention targeting multiple behavioral and psychosocial risk factors among pregnant African American women in the District of Columbia. The risk factors we chose to address were cigarette smoking, secondhand smoke exposure, depression, and IPV.
METHODS
The National Institutes of Health (NIH)–DC Initiative to Reduce Infant Mortality in Minority Populations is a long-standing and ongoing research collaboration between 4 major academic institutions in Washington, DC (the Children's National Medical Center, Georgetown University, George Washington University, and Howard University), the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Center for Minority Health and Health Disparities, and Research Inangle Institute International. As part of this collaboration, we undertook a randomized clinical trial (Healthy Outcomes of Pregnancy Education, or DC-HOPE) to evaluate the benefits of an integrated behavioral and psychosocial intervention delivered during routine prenatal care. (Details on or copies of the training materials, instruments, and the DC-HOPE intervention are available from the authors.)
Study Design
In this randomized study, we assessed a clinic-based intervention focusing on 4 psychosocial and behavioral risk factors (cigarette smoking, secondhand smoke exposure, depression, and IPV) associated with poor pregnancy outcomes. A site- and risk-specific block randomization design was used, and women were randomized to an intervention group or a usual care group. Interviewers collecting outcome information were unaware of participants’ group assignments. Primary and secondary study hypotheses were specified in advance.
Screening, Recruitment, and Retention
Details of the study screening, recruitment, and retention methods (including the methods used in calculating the required sample size) have been previously described,49 and only a brief description is provided here. Determination of sample size requirements was essential to ensure that the necessary statistical power was available to test the hypothesis that the multidisciplinary integrated intervention would produce reductions in the risk factors targeted. According to conventional assumptions, the study required that data be available from 1050 women (equally divided between the 2 randomized groups) to allow detection of a 10% to 20% reduction in risk factors among those in the intervention group.
Between July 2001 and October 2003, we collaborated with 6 prenatal care sites in Washington, DC, serving a predominantly African American population to conduct a 2-stage consent and enrollment process. Women were approached while they were waiting for routine prenatal care appointments and invited to immediately complete a 10-minute audio computer-assisted self-interview (ACASI) to assess their potential eligibility for the study. Approximately 9 days after completing the screening interview, women were administered a baseline telephone interview during which more-detailed information was gathered; this information served as the basis for behavioral change comparisons at follow-up. At the conclusion of this interview, each eligible consenting woman was randomized into the intervention or usual care group.
Eligible women were 18 years or older, were no more than 28 weeks pregnant, were African American or Latina, and had at least 1 of the 4 risk factors of interest. Follow-up data-collection telephone interviews were conducted during the second and third trimesters of pregnancy (22–26 and 34–38 weeks estimated gestational age, respectively). Intervention and follow-up activities continued until July 2004.
Participants were compensated for their time and effort; they received $5 for completing the ACASI screening, $15 for completing each telephone interview, and a 30-minute telephone card after providing consent. Women in the intervention group received an additional $10 at each intervention session conducted during their pregnancy.
Women who reported suicidal ideation during screening or follow-up interviews were immediately referred to an emergency mental health consultation team. The mental health consultant contacted and evaluated each such participant for actual suicidality. Referrals were made as needed, and women found to be potentially suicidal (n = 10) were excluded from the study.
Integrated Intervention
The behavioral intervention has been described in detail elsewhere.50 Briefly, the intervention, based on the behavioral change literature specific to the psychosocial and behavioral risks targeted, was designed to be delivered in prenatal care clinics. To assess smoking and secondhand smoke exposure, the DC-HOPE project incorporated elements from the successful Smoking Cessation or Reduction in Pregnancy Program Treatment (SCRIPT) trial,51 the transtheoretical model of behavior change, the “pathways to change” self-help manual, and cognitive–behavioral therapy.52 Similarly, we adapted a group cognitive–behavioral therapy treatment developed by Miranda and Munoz53 that had been used successfully with low-income, ethnic-minority obstetrics and gynecology patients suffering from depression. A single-visit intervention developed by Parker et al.54 for women experiencing IPV was modified to provide ongoing evaluation, guidance, and feedback throughout pregnancy.
Eight prenatal sessions were required to deliver the complete intervention, but a minimum of 4 sessions was deemed “adequate” on the basis of the amount of material that could be covered in that number of sessions. Individualized counseling provided an integrated and tailored approach to the multiple risks reported by each woman; intervention sessions occurred immediately before or after routine prenatal care, for an average of 35 minutes and no more than 45 minutes. Participants were presented with material during intervention sessions that required their active engagement with tasks such as identifying smoking triggers, developing strategies for mood management, and conducting a danger assessment.
In each session, the interventionists (referred to as “pregnancy advisors”) and participants developed a plan for “homework” designed to reinforce the intervention in the woman's real-life circumstances. The majority of the pregnancy advisors had master's degrees in counseling disciplines such as psychology as well as experience in interpersonal counseling, health education, or behavior change; 2 were registered nurses. All received 3 weeks of intensive training in addition to ongoing supervision to ensure their familiarity with, and fidelity to, the integrated intervention. Pregnancy advisors were trained to address multiple risk factors in an integrated fashion that was responsive to each woman's circumstances and to promote an overall sense of mastery and self-efficacy based on an integrated approach to the risk behaviors addressed in the study (i.e., smoking, secondhand smoke exposure, depression, and IPV). A single pregnancy advisor was assigned to each clinic to provide consistency of care for participating women.
Data Collection
Validated instruments assessing cigarette smoking, secondhand smoke exposure, depression, and IPV were used for the ACASI screening and the baseline and follow-up telephone assessments.55–60 In addition to standard sociodemographic data and information on the 4 risk factors, the baseline telephone interview collected information regarding drug and alcohol use, relevant obstetric history, and the participant's attitude toward her current pregnancy. As already mentioned, telephone interviewers (and their supervisors) were unaware of the participant's randomization group. (Details regarding study instrumentation are available on request from the authors.)
Data Analysis
We used an intention-to-treat approach to evaluate the overall benefits of the intervention and to avoid bias. Participants were analyzed according to their randomized care-group assignment, regardless of actual receipt of intervention or withdrawal from the study.61
Multiple imputation methodology was used to estimate missing data for the purposes of the intention-to-treat analysis. The sequential regression methodology described by Raghunathan et al62 was employed in calculating these estimates. A linear, logistic, or polytomous regression model was used to impute continuous, binary, or categorical missing values. Imputation was performed multiple times to create 5 complete data sets; variability among the imputed data sets reflected the uncertainty inherent in predicting unknown values. IVEware imputation and variance estimation software (Survey Methodology Program, University of Michigan, Ann Arbor, MI) was used in completing these procedures.63
In conducting our analyses, we used standard statistical techniques to separately assess each of the 5 imputed data sets. We then combined the results via the MIANALYZE procedure in SAS version 9.1.3 (SAS Institute, Cary, NC) to obtain the overall results for the multiply imputed data. The final parameter estimates were averages of the estimates from the 5 imputed data sets, and the associated standard errors accounted for both within- and between-imputation variance.
Basic descriptive statistics were used to gather information on the characteristics of the participants, both overall and stratified by randomization assignment. Relevant comparisons were conducted via general linear models (for continuous variables) and generalized linear models (for categorical variables; Table 1 ). The GLM and GENMOD procedures in SAS were used in all of the analyses.
TABLE 1.
Participant Characteristics (N = 913): Healthy Outcomes of Pregnancy Education (DC-HOPE) Project, Washington, DC, 2001–2004
| Total Sample | Intervention Group | Usual Care Group | P | |
| Trimester of prenatal care initiation, No. (%) | .509 | |||
| First trimester | 551 (60.3) | 279 (61.6) | 272 (59.1) | |
| Second trimester | 344 (37.7) | 163 (36.0) | 181 (39.3) | |
| Third trimester | 18 (2.0) | 11 (2.3) | 7 (1.6) | |
| Gestational age at baseline, wk, mean (SE) | 19.0 (0.2) | 19.4 (0.3) | 18.6 (0.3) | .081 |
| Maternal age, y, mean (SE) | 24.6 (0.2) | 24.4 (0.3) | 24.8 (0.3) | .217 |
| Educational level, no. (%) | .649 | |||
| Less than high school | 284 (31.1) | 141 (31.3) | 143 (31.0) | |
| High school or equivalent | 424 (46.5) | 214 (47.3) | 210 (45.6) | |
| At least some college | 205 (22.4) | 97 (21.4) | 108 (23.4) | |
| Employment status, no. (%) | .562 | |||
| Employed | 324 (35.5) | 157 (34.8) | 167 (36.2) | |
| Not employed but worked prior to pregnancy | 338 (37.0) | 164 (36.3) | 174 (37.7) | |
| Not employed and did not work prior to pregnancy | 247 (27.1) | 130 (28.7) | 117 (25.4) | |
| Not employed and work status prior to pregnancy unknown | 4 (0.4) | 1 (0.2) | 3 (0.7) | |
| Relationship status, no. (%) | .686 | |||
| Single/separated/widowed/divorced | 694 (76.0) | 341 (75.5) | 353 (76.6) | |
| Married or living with partner | 219 (24.0) | 111 (24.5) | 108 (23.4) | |
| No. of household members, mean (SE) | 3.9 (0.1) | 3.9 (0.1) | 4.0 (0.1) | .161 |
| Household income < $2000 per mo, no. (%) | 475 (72.2) | 241 (74.8) | 234 (69.7) | .140 |
| Medicaid recipient, no. (%) | 720 (78.9) | 366 (80.9) | 355 (77.0) | .153 |
| WIC recipient, no. (%) | 398 (43.5) | 203 (44.9) | 195 (42.2) | .422 |
| Supplemental food program recipient, no. (%) | 668 (73.3) | 330 (73.4) | 337 (73.2) | .951 |
| Public assistance/TANF recipient, no. (%) | 398 (43.7) | 196 (43.4) | 202 (43.9) | .891 |
| Alcohol use during present pregnancy, no. (%) | 208 (22.7) | 103 (22.7) | 105 (22.8) | .969 |
| Illicit drug use during present pregnancy, no. (%) | 120 (13.1) | 66 (14.6) | 54 (11.7) | .201 |
| Pregnancy wanted, no. (%) | 693 (75.9) | 346 (76.4) | 347 (75.4) | .713 |
| Pregnancy history | ||||
| Previous pregnancy, no. (%) | 774 (84.8) | 377 (83.4) | 397 (86.1) | .252 |
| Previous live birth, no. (%) | 633 (69.3) | 306 (67.7) | 327 (70.9) | .290 |
| No. of live births,a mean (SE) | 2.2 (0.1) | 2.2 (0.1) | 2.2 (0.1) | .979 |
| Previous miscarriage,b no. (%) | 302 (39.0) | 147 (38.9) | 155 (39.1) | .967 |
| Previous stillbirth,b no. (%) | 39 (5.0) | 16 (4.2) | 23 (5.8) | .325 |
Note. WIC = Special Supplemental Nutrition Program for Women, Infants, and Children; TANF = Temporary Assistance for Needy Families. For the intervention group, n = 452. For the usual care group, n = 461. With the exception of trimester of prenatal care initiation and gestational age at baseline, information was self-reported by participants.
Among women with a previous live birth (or births).
Among women with a previous pregnancy (or pregnancies).
To evaluate the impact of the integrated intervention on risk reduction between the baseline and second follow-up interviews, we used logistic regression procedures to model the probability of women resolving all versus none of their risks and the probability of their resolving at least 1 versus none of their risks (Table 2 ). We used the LOGISTIC procedure in SAS to conduct analyses focusing on the individual imputations. Control variables included maternal age, education, marital status, employment status, enrollment in federal assistance programs (i.e., Medicaid and the Special Supplemental Nutrition Program for Women, Infants, and Children), and drug and alcohol use at baseline; previous premature delivery, pregnancy loss, or live birth; early initiation of prenatal care; gestational age at baseline; smoking, secondhand smoke exposure, depression, and IPV at the time of the ACASI screening; and total number of risks at baseline.
TABLE 2.
Changes in Risk Status From Baseline to Second Follow-Up: Healthy Outcomes of Pregnancy Education (DC-HOPE) Project, Washington, DC, 2001–2004
| Total Sample, No. (%) | Intervention Group, No. (%) | Usual Care Group, No. (%) | P | |
| Risk resolution between baseline and second follow-up | .031 | |||
| No. of risks increased | 103 (11.3) | 44 (9.7) | 59 (12.8) | |
| No risks resolved | 326 (35.7) | 146 (32.3) | 180 (39.0) | |
| Some risks resolved | 311 (34.0) | 162 (35.9) | 148 (32.2) | |
| All risks resolved | 174 (19.0) | 100 (22.1) | 74 (16.0) | |
| Some risks resolved | .019 | |||
| Yes | 484 (53.0) | 262 (58.0) | 222 (48.2) | |
| No | 429 (47.0) | 190 (42.0) | 239 (51.8) | |
| All vs no risks resolved | .064 | |||
| No risks resolved | 429 (71.2) | 190 (65.6) | 239 (76.4) | |
| All risks resolved | 174 (28.8) | 100 (34.4) | 74 (23.6) |
Note. For the total sample, N = 913. For the intervention group, n = 452. For the usual care group, n = 461.
Preliminary analyses identified no covariates that differed significantly between the 2 randomized groups (Table 1). Nonetheless, these variables descriptive of socioeconomic status and previous pregnancy outcomes were included as covariates so that their cumulative effects could be accounted for in the final model.
Outcome Variables
To assess the effects of the intervention, 2 approaches were used to quantify behavioral changes occurring during pregnancy and to compare the 2 randomized groups at baseline, the first follow-up (second trimester), and the second follow-up (third trimester). The first approach contrasted the distribution of number of risks as reported by women in the 2 groups at each time point. The second quantified within-person change over time to assess the benefits of the intervention in line with the method used to evaluate the Colorado Prenatal Plus Program.48 According to this integrated approach, each woman was characterized with respect to number of risks at the baseline interview. This number could range from 0 (for women whose reported risks at screening were not present when they were assessed at baseline, either because of behavioral change or because of the change in instrumentation) to 4 (for those women reporting active smoking, secondhand smoke exposure, depression, and IPV).
At the eligibility screening, women who reported that they had smoked in the 6 months preceding their pregnancy or since learning they were pregnant were defined as smokers; at study enrollment, women were defined as smokers if they had smoked at least a puff of a cigarette in the previous week. At the eligibility screening, secondhand smoke exposure was defined as exposure to smokers at home, in the same room, or in a car; at enrollment, it was defined as having been in the same room or area in which someone was smoking in the past week.
The Beck Depression Inventory II64,65 was used to evaluate depression at the eligibility screening, and the Hopkins Symptom Checklist66,67 was used to assess depression at study enrollment (women who had a score above 0.75 on the latter instrument were categorized as depressed). To assess IPV at the eligibility screening, women were asked whether a current or previous partner, boyfriend, or husband or the baby's father had pushed, shoved, slapped, kicked, or physically hurt them or forced them to have sexual intercourse in the past year; they were also asked whether they were afraid of their current partner. At study enrollment, IPV was confirmed if a woman reported having been subjected to any of the actions addressed in the revised Conflict Tactics Scale67,68 at least once by her partner in the past year.
Next, each woman was characterized in 1 of 3 ways on the basis of data provided in the follow-up telephone interviews conducted during the third trimester. That is, women were classified as (1) having resolved all of their risks, (2) having resolved some but not all of their risks, or (3) having resolved none of their risks or having increased their number of risks. A woman was defined as having “resolved” a risk if she had eliminated 1 of the behaviors or exposures of interest (i.e., she had quit smoking, she had not been exposed to secondhand smoke, her depression scores were below the clinical cutoff, or she had experienced no IPV episodes).
The primary measure of intervention effectiveness was the comparison of the proportion of women in the 2 randomized groups who had resolved all or some of their risks and the proportion of women who had resolved none of their risks. In addition, we compared the proportion of participants in the intervention and usual-care groups who had resolved all of their risks and the proportion who had resolved none of their risks.
RESULTS
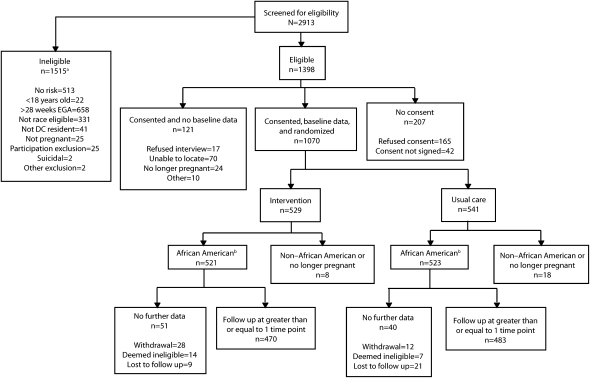
A total of 4213 women were invited to participate in the ACASI screenings at the 6 collaborating clinic sites. Of these women, 649 refused and 651 never completed the screening to determine their eligibility. As shown in Figure 1, 1398 of the 2913 women screened with respect to demographic characteristics and risk were eligible for participation; 1070 provided baseline data and consented to participate. Some of the remaining 328 women refused to complete the baseline interview (n = 17) or refused to provide consent (n = 207), and some were excluded because attempts to recontact them were unsuccessful (n = 70), because they were no longer pregnant (n = 24), or as a result of other reasons (n = 10).
FIGURE 1.
Screening, eligibility, recruitment, and retention: Healthy Outcomes of Pregnancy Education (DC-HOPE) project, Washington, DC, 2001–2004.
Note. EGA = estimated gestational age.
aMore than 1 reason for ineligibility may apply.
bOnly African American women who were still pregnant at the time of the baseline interview were used in this analysis.
The 1070 women with complete baseline data were randomized to the intervention group (n = 529) or the usual-care group (n = 541). After exclusion of women who identified themselves as non–African American Latinas (n = 22) and women who had completed their pregnancy prior to the baseline interview (n = 4), there were 521 African American women in the intervention group and 523 in the usual-care group.
In the intervention group, 81% (n = 423) of participants provided follow-up data during the second or third trimester (or both trimesters), as compared with 82% (n = 427) in the usual care group. In spite of this overall success, 43% of the 1044 randomized women did not complete the first follow-up interview, and 31% did not complete the second follow-up interview. In addition, we excluded from all subsequent analyses 131 women who were screened into the study on the basis of the limited data obtained in the self-interview but who reported no risk factors at baseline. Women's most common reason for not participating in the second follow-up interview was that they were no longer pregnant (this was the case for 178 women).
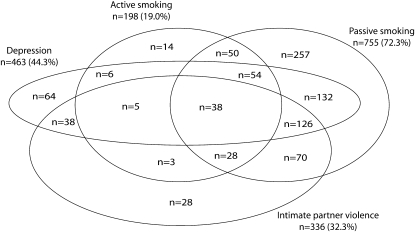
The baseline characteristics of the 913 women included in our analyses are shown in Table 1, and the distribution of baseline risks is illustrated in Figure 2. Secondhand smoke exposure was the most common risk targeted, occurring both in isolation (among 28.2% of the women) and with other risk factors, notably depression (14.5%) and depression in combination with IPV (13.8%). Of risk factors occurring in isolation, cigarette smoking was least common (1.6%); 7.0% of women were depressed, and 3.1% had experienced IPV. It is apparent, however, that the majority of women enrolled (60.2%) faced multiple risk factors at baseline.
FIGURE 2.
Distribution of eligible women, by risk factor, at the baseline interview: Healthy Outcomes of Pregnancy Education (DC-HOPE) project, Washington, DC, 2001–2004.
Note. The total eligible sample was N = 1913.
The mean number of intervention sessions attended by the 452 women in the intervention group was 3.9; 16.4% of these women attended no intervention sessions. More than half (53.9%) attended at least 4 sessions.
The distribution of risks did not differ significantly between the intervention and usual care groups at either the first or second follow-up assessment during pregnancy trimesters 2 and 3 (P = .505 and P = .135, respectively). As can be seen in Table 2, we subsequently compared the groups by assessing individual change over time in 3 categories (all risks resolved, some risks resolved, and no risks resolved). Forty-two percent of the intervention group and 51.8% of the usual care group resolved none of their risks during pregnancy. Thus, overall, 58.0% of women assigned to the intervention group resolved some or all of their risks, whereas only 48.2% of those receiving usual care did so (unadjusted P = .019).
Multiple logistic modeling was used to estimate the benefits of the intervention; results are displayed in Table 3. Preliminary models included all covariates identified in the Methods section. Significant effects were retained in the final reduced model. Women randomized to the intervention group more frequently resolved at least 1 (vs none) of their risks than did those randomized to the usual care group (odds ratio [OR] = 1.61; 95% confidence interval [CI] = 1.08, 2.39; P = .021). Significant covariates in the model were number of baseline risks and smoking risk at ACASI screening.
TABLE 3.
Results From Risk Reduction Logistic Regression Models: Healthy Outcomes of Pregnancy Education (DC-HOPE) Project, Washington, DC, 2001–2004
| Odds Ratio (95% Confidence Interval) | P | |
| Model 1a | ||
| Intercept | 0.34 (0.21, 0.56) | <.001 |
| Care group (intervention vs usual care) | 1.78 (1.02, 3.11) | .043 |
| Active smoking at ACASI screening (yes vs no) | 0.57 (0.38, 0.87) | .010 |
| IPV at ACASI screening (yes vs no) | 1.90 (1.17, 3.07) | .010 |
| Model 2b | ||
| Intercept | 0.14 (0.08, 0.23) | <.001 |
| Care group (intervention vs usual care) | 1.61 (1.08, 2.39) | .021 |
| No. of risks at baseline (1 risk increase) | 3.34 (2.65, 4.20) | <.001 |
| Active smoking at ACASI screening (yes vs no) | 0.47 (0.32, 0.69) | <.001 |
| Model 3c | ||
| Intercept | 0.25 (0.16, 0.40) | <.001 |
| Care group (intervention vs usual care) | 2.47 (1.41, 4.32) | .003 |
| IPV at ACASI screening (yes vs no) | 2.60 (1.56, 4.34) | <.001 |
| Model 4d | ||
| Intercept | 0.11 (0.06, 0.21) | <.001 |
| Care group (intervention vs usual care) | 2.22 (1.38, 3.57) | .002 |
| No. of risks at baseline (1 risk increase) | 3.40 (2.59, 4.46) | <.001 |
| Active smoking at ACASI screening (yes vs no) | 0.51 (0.33, 0.78) | .002 |
| IPV at ACASI screening (yes vs no) | 1.77 (1.10, 2.85) | .019 |
Note. ACASI = audio computer-assisted self-interview; IPV = intimate partner violence.
Model predicting resolution of all vs no risks (n = 602).
Model predicting resolution of some vs no risks (n = 913).
Model predicting resolution of all vs no risks among women who attended with 4 or more intervention sessions and all women in the usual care group (n = 469).
Model predicting resolution of some vs no risks among women who attended with 4 or more intervention sessions and all women in the usual care group (n = 705).
Supplemental analyses comparing women who resolved all of their risks and women who resolved none of their risks (ignoring the 311 women who resolved some of their risks) also revealed that those in the intervention group were more successful than were those in the usual care group (OR = 1.78; 95% CI = 1.02, 3.11; P = .043). Significant covariates were smoking and IPV risk at ACASI screening. Additional supplemental analyses compared women who had attended at least 4 intervention sessions and all women in the usual care group with respect to resolving all risks as opposed to no risks (OR = 2.47; 95% CI = 1.41, 4.32; P = .003) and with respect to resolving some risks as opposed to no risks (OR = 2.22; 95% CI = 1.38, 3.57; P = .002). These comparisons were, however, nonexperimental in that women were not randomly allocated to participate in a different number of intervention sessions.
DISCUSSION
Reproductive health outcomes remain problematic for urban women of color. Significant gaps in the content of prenatal care and in its ability to address psychosocial and behavioral risk factors may contribute to this situation. Our results are part of a growing body of literature documenting the feasibility and efficacy of clinic-based interventions designed to promote the health of traditionally disadvantaged groups. The prenatal care intervention described here was successful in resolving the psychosocial and behavioral risks targeted, even when it was delivered in busy community-based clinics serving urban women with primarily public insurance coverage.
Our findings confirm the benefits of an intervention targeting multiple psychosocial and behavioral pregnancy risk factors simultaneously, as suggested by a similar but quasi-experimental study focusing on the Colorado Prenatal Plus Program. The factors addressed in our study were similar but not identical to those addressed in the Colorado study, and our sample consisted of exclusively high-risk African American women, whereas the Colorado study included multiethnic Medicaid-eligible patients.48
Our study also demonstrates the feasibility of using trained nonmedical professionals to deliver primary care interventions, although further work is required to rigorously identify optimal methods for providing such services. Further research should also be directed toward understanding how factors such as resiliency, social support, and coping contribute to both initial participation in an intervention and naturally occurring change.
It spite of its success, our study involved significant limitations. First, many of the psychosocial–behavioral factors that can potentially affect pregnancy outcomes were not included in the intervention assessed here, notably illicit substance and alcohol use along with anxiety and stress. Similarly, our cognitive–behavioral intervention was not designed to influence the socioeconomic challenges that frequently coexist with the risk factors targeted in this study. Second, the recruited population appeared only modestly invested in taking part in our intervention. Even after potentially unenthusiastic participants had been eliminated through a 2-stage screening and consent process, a significant proportion of women randomized to the intervention group attended fewer than 4 sessions, estimated to be the minimum adequate exposure. Third, we considered only complete elimination of risks, rather than a reduction in risks, which may have led to underestimations of intervention effects.
Although the 3 limitations just described may have collectively resulted in underestimations of effects, a fourth limitation—our reliance on women's self-reports of risk—may have led to overestimations: because the intervention group may have developed a greater social-desirability awareness in reporting behavioral improvements, our estimates of changes in this group may have been inflated. Finally, in common with all intervention research, our results are generalizable only to the group of women who met our inclusion and exclusion criteria and consented to participate in our study.
Nonetheless, this study provides evidence that a clinic-based behavioral intervention targeting pregnant African American women led to reductions in selected risk factors for poor reproductive outcomes. Larger studies are needed to extend these findings and determine whether reducing risks improves pregnancy outcomes such as low birthweight and prematurity. However, risk reduction in itself is an important goal, and the data provided here support the incorporation of psychosocial and behavioral interventions into primary care settings.
Acknowledgments
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Center on Minority Health and Health Disparities, National Institutes of Health (grants 3U18HD030445, 3U18HD030447, 5U18HD31206, 3U18HD031919, and 5U18HD036104).
We thank the field work staff, the interviewers, and the data management staff. Also, we thank the participants, who welcomed us into their lives in hopes of helping themselves and their children.
Human Participant Protection
This study was approved by the institutional review boards of Howard University (as the designated clinical site institution), RTI International, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
References
- 1.Dominguez TP. Race, racism, and racial disparities in adverse birth outcomes. Clin Obstet Gynecol 2008;51:360–370 [DOI] [PubMed] [Google Scholar]
- 2.Hessol NA, Fuentes-Afflick E. Ethnic differences in neonatal and postneonatal mortality. Pediatrics 2005;115:e44–e51 [DOI] [PubMed] [Google Scholar]
- 3.Arias E, MacDorman MF, Strobino DM, Guyer B. Annual summary of vital statistics—2002. Pediatrics 2003;112:1215–1230 [DOI] [PubMed] [Google Scholar]
- 4.MacDorman MF, Minino AM, Strobino DM, Guyer B. Annual summary of vital statistics—2001. Pediatrics 2002;110:1037–1052 [DOI] [PubMed] [Google Scholar]
- 5.Healy AJ, Malone FD, Sullivan LM, et al. Early access to prenatal care: implications for racial disparity in perinatal mortality. Obstet Gynecol 2006;107:625–631 [DOI] [PubMed] [Google Scholar]
- 6.Kung H-C, Hoyert DL, Xu J, Murphy SL. Deaths: Final data for 2005. Natl Vital Stat Rep April 24, 2008;56(10). [PubMed] [Google Scholar]
- 7.Gonzalez-Calvo J, Jackson J, Hansford C, Woodman C. Psychosocial factors and birth outcome: African American women in case management. J Health Care Poor Underserved 1998;9:395–419 [DOI] [PubMed] [Google Scholar]
- 8.Sable MR, Wilkinson DS. Impact of perceived stress, major life events and pregnancy attitudes on low birth weight. Fam Plann Perspect 2000;32:288–294 [PubMed] [Google Scholar]
- 9.Zimmer-Gembeck MJ, Helfand M. Low birthweight in a public prenatal care program: behavioral and psychosocial risk factors and psychosocial intervention. Soc Sci Med 1996;43:187–197 [DOI] [PubMed] [Google Scholar]
- 10.Berkowitz GS. An epidemiologic study of preterm delivery. Am J Epidemiol 1981;113:81–92 [DOI] [PubMed] [Google Scholar]
- 11.Berkowitz GS, Papiernik E. Epidemiology of preterm birth. Epidemiol Rev 1993;15:414–443 [DOI] [PubMed] [Google Scholar]
- 12.Cnattingius S. The epidemiology of smoking during pregnancy: smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob Res 2004;6(suppl 2):S125–S140 [DOI] [PubMed] [Google Scholar]
- 13.Feldman JG, Minkoff HL, McCalla S, Salwen M. A cohort study of the impact of perinatal drug use on prematurity in an inner-city population. Am J Public Health 1992;82:726–728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orr ST, James SA, Blackmore Prince C. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am J Epidemiol 2002;156:797–802 [DOI] [PubMed] [Google Scholar]
- 15.Chung TK, Lau TK, Yip AS, Chiu HF, Lee DT. Antepartum depressive symptomatology is associated with adverse obstetric and neonatal outcomes. Psychosom Med 2001;63:830–834 [DOI] [PubMed] [Google Scholar]
- 16.Murphy CC, Schei B, Myhr TL, Du Mont J. Abuse: a risk factor for low birth weight? A systematic review and meta-analysis. CMAJ 2001;164:1567–1572 [PMC free article] [PubMed] [Google Scholar]
- 17.Neggers Y, Goldenberg R, Cliver S, Hauth J. Effects of domestic violence on preterm birth and low birth weight. Acta Obstet Gynecol Scand 2004;83:455–460 [DOI] [PubMed] [Google Scholar]
- 18.An LC, Zhu SH, Nelson DB, et al. Benefits of telephone care over primary care for smoking cessation: a randomized trial. Arch Intern Med 2006;166:536–542 [DOI] [PubMed] [Google Scholar]
- 19.Anderson RT, King A, Stewart AL, Camacho F, Rejeski WJ. Physical activity counseling in primary care and patient well-being: do patients benefit? Ann Behav Med 2005;30:146–154 [DOI] [PubMed] [Google Scholar]
- 20.Estabrooks PA, Glasgow RE, Dzewaltowski DA. Physical activity promotion through primary care. JAMA 2003;289:2913–2916 [DOI] [PubMed] [Google Scholar]
- 21.Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA 2003;289:3145–3151 [DOI] [PubMed] [Google Scholar]
- 22.Writing Group for the Activity Counseling Trial Research Group Effects of physical activity counseling in primary care: the Activity Counseling Trial: a randomized controlled trial. JAMA 2001;286:677–687 [DOI] [PubMed] [Google Scholar]
- 23.Ludman E, Von Korff M, Katon W, et al. The design, implementation, and acceptance of a primary care-based intervention to prevent depression relapse. Int J Psychiatry Med 2000;30:229–245 [DOI] [PubMed] [Google Scholar]
- 24.Ockene JK, Kristeller J, Pbert L, et al. The Physician-Delivered Smoking Intervention Project: can short-term interventions produce long-term effects for a general outpatient population? Health Psychol 1994;13:278–281 [DOI] [PubMed] [Google Scholar]
- 25.Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA 2004;292:935–942 [DOI] [PubMed] [Google Scholar]
- 26.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med 2002;22:267–284 [DOI] [PubMed] [Google Scholar]
- 27.Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2004;140:557–568 [DOI] [PubMed] [Google Scholar]
- 28.Kelly R, Zatzick D, Anders T. The detection and treatment of psychiatric disorders and substance use among pregnant women cared for in obstetrics. Am J Psychiatry 2001;158:213–219 [DOI] [PubMed] [Google Scholar]
- 29.Alegria M, Canino G, Rios R, et al. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino Whites. Psychiatr Serv 2002;53:1547–1555 [DOI] [PubMed] [Google Scholar]
- 30.Chow JC, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. Am J Public Health 2003;93:792–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Serv Res 2006;41:1979–2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Virnig B, Huang Z, Lurie N, Musgrave D, McBean AM, Dowd B. Does Medicare managed care provide equal treatment for mental illness across races? Arch Gen Psychiatry 2004;61:201–205 [DOI] [PubMed] [Google Scholar]
- 33.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res 2003;18:156–170 [DOI] [PubMed] [Google Scholar]
- 34.American College of Obstetricians and Gynecologists Psychosocial risk factors: perinatal screening and intervention. Int J Gynaecol Obstet 2000;69:195–200 [PubMed] [Google Scholar]
- 35.Durant T, Colley Gilbert B, Saltzman LE, Johnson CH. Opportunities for intervention: discussing physical abuse during prenatal care visits. Am J Prev Med 2000;19:238–244 [DOI] [PubMed] [Google Scholar]
- 36.Herzig K, Huynh D, Gilbert P, Danley DW, Jackson R, Gerbert B. Comparing prenatal providers’ approaches to four different risks: alcohol, tobacco, drugs, and domestic violence. Women Health 2006;43:83–101 [DOI] [PubMed] [Google Scholar]
- 37.Peoples-Sheps MD, Hogan VK, Ng'andu N. Content of prenatal care during the initial workup. Am J Obstet Gynecol 1996;174:220–226 [DOI] [PubMed] [Google Scholar]
- 38.Rodriguez MA, Bauer HM, McLoughlin E, Grumbach K. Screening and intervention for intimate partner abuse: practices and attitudes of primary care physicians. JAMA 1999;282:468–474 [DOI] [PubMed] [Google Scholar]
- 39.Zapka JG, Pbert L, Stoddard AM, Ockene JK, Goins KV, Bonollo D. Smoking cessation counseling with pregnant and postpartum women: a survey of community health center providers. Am J Public Health 2000;90:78–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sarnoff R, Adams E, Shauffler H, Abrams B. Disparities in reported prenatal care advice from health care providers among women of Mexican origin in California. J Immigr Health 2001;3:77–84 [DOI] [PubMed] [Google Scholar]
- 41.Horan DL, Chapin J, Klein L, Schmidt LA, Schulkin J. Domestic violence screening practices of obstetrician-gynecologists. Obstet Gynecol 1998;92:785–789 [DOI] [PubMed] [Google Scholar]
- 42.Hayes BA, Muller R. Prenatal depression: a randomized controlled trial in the emotional health of primiparous women. Res Theory Nurs Pract 2004;18:165–183 [DOI] [PubMed] [Google Scholar]
- 43.Villar J, Farnot U, Barros F, Victora C, Langer A, Belizan JM. A randomized trial of psychosocial support during high-risk pregnancies. The Latin American Network for Perinatal and Reproductive Research. N Engl J Med 1992;327:1266–1271 [DOI] [PubMed] [Google Scholar]
- 44.Chander G, McCaul ME. Co-occurring psychiatric disorders in women with addictions. Obstet Gynecol Clin North Am 2003;30:469–481 [DOI] [PubMed] [Google Scholar]
- 45.Emmons KM, McBride CM, Puleo E, et al. Project PREVENT: a randomized trial to reduce multiple behavioral risk factors for colon cancer. Cancer Epidemiol Biomarkers Prev 2005;14:1453–1459 [DOI] [PubMed] [Google Scholar]
- 46.Toobert DJ, Glasgow RE, Strycker LA, Barrera M, Jr, Ritzwoller DP, Weidner G. Long-term effects of the Mediterranean lifestyle program: a randomized clinical trial for postmenopausal women with type 2 diabetes. Int J Behav Nutr Phys Act 2007;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nigg CR, Allegrante JP, Ory M. Theory-comparison multiple-behavior research: common themes advancing health behavior research. Health Educ Res 2002;17:670–679 [DOI] [PubMed] [Google Scholar]
- 48.Ricketts SA, Murray EK, Schwalberg R. Reducing low birthweight by resolving risks: results from Colorado's Prenatal Plus Program. Am J Public Health 2005;95:1952–1957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.El-Khorazaty MN, Johnson AA, Kiely M, et al. Recruitment and retention of low-income minority women in a behavioral intervention to reduce smoking, depression, and intimate partner violence during pregnancy. BMC Public Health 2007;7:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Katz KS, Blake SM, Milligan RA, et al. The design, implementation and acceptability of an integrated intervention to address multiple behavioral and psychosocial risk factors among pregnant African American women. BMC Pregnancy Childbirth 2008;8:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Windsor RA. Counselling smokers in Medicaid maternity care: the SCRIPT project. Tob Control 2000;9(suppl 1):i62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hall SM, Munoz RF, Reus VI. Cognitive-behavioral intervention increases abstinence rates for depressive-history smokers. J Consult Clin Psychol 1994;62:141–146 [DOI] [PubMed] [Google Scholar]
- 53.Miranda J, Munoz R. Intervention for minor depression in primary care patients. Psychosom Med 1994;56:136–141 [DOI] [PubMed] [Google Scholar]
- 54.Parker B, McFarlane J, Soeken K, Silva C, Reel S. Testing an intervention to prevent further abuse to pregnant women. Res Nurs Health 1999;22:59–66 [DOI] [PubMed] [Google Scholar]
- 55.Beck AT, Steer RA, Brown GK. BDI-Fast Screen for Medical Patients. San Antonio, TX: Psychological Corp; 2000 [Google Scholar]
- 56.Hovell MF, Zakarian JM, Matt GE, Hofstetter CR, Bernert JT, Pirkle J. Effect of counselling mothers on their children's exposure to environmental tobacco smoke: randomised controlled trial. BMJ 2000;321:337–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McFarlane J, Parker B. Preventing abuse during pregnancy: an assessment and intervention protocol. MCN Am J Matern Child Nurs 1994;19:321–324 [PubMed] [Google Scholar]
- 58.Melvin CL, Tucker P. Measurement and definition for smoking cessation intervention research: the smoke-free families experience. Tob Control 2000;9(suppl 3):III87–III90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Derogatis L. SCL-90-R: Administration, Scoring and Procedures Manual. Minneapolis, MN: National Computer Systems; 1994 [Google Scholar]
- 60.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scale (CTS2): development and preliminary psychometric data. J Fam Issues 1996;17:283–316 [Google Scholar]
- 61.Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 1999;319:670–674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Raghunathan TE, Solenberger P, Van Hoewyk J. IVEware: Imputation and Variance Estimation Software: User Guide. Ann Arbor, MI: Survey Methodology Program, University of Michigan; 2002 [Google Scholar]
- 63.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol 2001;27:85–95 [Google Scholar]
- 64.Beck AT, Steer RA, Brown GK. BDI Fast Screen for Medical Patients Manual. San Antonio, TX: Psychological Corporation; 2000 [Google Scholar]
- 65.Steer RA, Cavalieri TA, Leonard DM, Beck AT. Use of the Beck Depression Inventory for primary care to screen for major depression disorders. Gen Hosp Psychiatry 1999;21:106–111 [DOI] [PubMed] [Google Scholar]
- 66.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci 1974;19:1–15 [DOI] [PubMed] [Google Scholar]
- 67.Lipman RS, Covi L, Shapiro A. The Hopkins Checklist (HSCL): factors derived from the HSCL-90. J Affect Disord 1979;1:9–24 [DOI] [PubMed] [Google Scholar]
- 68.Straus MA. Manual for the Conflict Tactics Scales. Durham: Family Research Laboratory, University of New Hampshire; 1995 [Google Scholar]
- 69.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scale (CTS2): development and preliminary psychometric data. J Fam Issues 1996;17:283–316 [Google Scholar]