Abstract
Purpose
We developed a near ocular dominance test modeled after the distance hole-in-the card test, and assessed both test-retest reliability of four tests of ocular dominance and agreement between tests.
Methods
46 subjects ages 18 to 78 years with visual acuity 20/40 or better in each eye were enrolled from a primary care practice. All subjects had normal eye examinations, with the exception of refractive error, and were examined in their habitual correction. Subjects were tested twice each with the distance hole-in-the-card test, new near hole- in-the-card test, near convergence test, and the Pediatric Eye Disease Investigator Group (PEDIG) fixation preference test. Test-retest reliability and agreement between tests were evaluated with the Kappa statistic.
Results
There was substantial to almost perfect test-retest reliability for the distance hole-in-the-card test, new near hole-in-the-card test, convergence test, and PEDIG fixation preference test (Kappa, k=0.77, 0.62, 0.84, 0.77, respectively). In contrast, the agreement between the new near hole in the card test and the other three tests – distance hole in the card, near convergence, and PEDIG fixation preference– was moderate to slight (k=0.41, 0.19, 0.11, respectively). Agreement was moderate to fair (k=0.47, 0.32) between the distance hole in the card test and the near convergence test, and between the distance-hole-in-the-card test and the PEDIG fixation preference test. Agreement was fair (k=0.27) between the near convergence test and the PEDIG fixation preference test.
Conclusions
Although there was excellent test-retest reliability of each ocular dominance test, there was only moderate to slight agreement between tests. Results of ocular dominance tests seem to vary depending on both the testing distance and the specific activity performed as part of the testing procedure.
INTRODUCTION
Ocular dominance is the preference to process visual input from one eye over the other. The relationship between ocular dominance and fixation preference is controversial.1 Nevertheless, assessing ocular dominance, or fixation preference, may be important in treating a variety of ophthalmic conditions such as amblyopia and refractive error, particularly if some individuals have different dominance for near versus distance tasks. Few studies have addressed the potential difference between near and distance dominance.
The present study was designed to determine if ocular dominance, or preferred fixation, varies by test distance and activity. Four tests of ocular dominance, or fixation preference, were compared, including a new near dominance test. For simplicity, these tests will be collectively referred to as tests of ocular dominance. The study also determined test-retest reliability of each test.
METHODS
Subjects
Institutional review board approval was obtained for the testing protocol and procedures. Each subject provided informed consent and Health Insurance Portability and Accountability Act authorization. We enrolled 46 subjects, ages 18 to 78 years. This convenience sample size of 40 to 50 subjects was chosen because there were no preliminary data available to formally calculate sample size. Visual acuity was 20/40 or better at distance and near in each eye while wearing habitual correction No subjects were included who were deliberately prescribed monovision lenses. This was confirmed by requiring the maximum interocular difference to be no greater than 0.1 logMAR at distance and at near, a difference which is within visual acuity test-retest variability.2 We excluded subjects who had an interocular difference of 0.2 logMAR or greater and subjects with any manifest strabismus (constant or intermittent), based on the cover test at distance and near. Subjects were recruited during a well-eye examination at a general eye clinic. All subjects had an otherwise normal complete eye examination, with the exception of refractive error, if present, and were tested in their habitual correction, if applicable.
Questions on dominance and handedness
Each subject was asked four questions: “Which is your dominant eye?,” “To which eye do you hold/sight a gun?,” “To which eye do you hold a camera?,” and “Are you right-handed, left-handed, or ambidextrous?” The response to each question was recorded and analyzed individually. Following the questions, a single examiner (MLR) performed the dominance and fixation tests.
Ocular dominance testing
Ocular dominance was determined by four separate tests: 1) distance hole-in- the-card test, 2) near convergence test, 3) Pediatric Eye Disease Investigator Group (PEDIG) fixation preference test, and 4) the new near hole-in-the-card test, described herein.
The distance hole-in-the-card test was performed first. The subject was given a piece of black paper with a three cm diameter circular hole in the center of the card. The subject was instructed to hold the paper with both hands straight ahead at arm’s length while viewing a single 20/50 letter at 10 feet with both eyes. The examiner covered the left eye and asked the subject if they could still see the letter. The examiner then covered the right eye and asked again if the subject could still see the letter. The eye that could see the letter was recorded as the dominant eye (right or left). If the subject was able to see the letter with both the right and the left eye, the dominant eye was recorded as “neither.”
The near convergence test was performed with an approximately 20/50 equivalent letter (1 mm in height and width) on a near point fixation stick held at 40 cm. The stick was brought toward the bridge of the subject’s nose until binocular fixation broke, unless the subject maintained fixation to the bridge of the nose. The eye that maintained fixation was recorded (right or left). If the subject maintained fixation with both eyes, then “neither” was recorded.
The third test performed was the PEDIG fixation preference test. The PEDIG designed this test to be used for the Amblyopia Treatment Studies to evaluate which eye is used for reading when patients are on atropine penalization therapy. A near point fixation stick with a vertical column of letters (1 mm in height and width) was used for near fixation, tested at 40 cm. The subject was instructed to read the letters while the examiner inserted a 14 prism diopter base-down prism in front of their right eye and observed the fixation pattern. A rapid cover-uncover test was used to confirm which eye was fixating (right, left, or alternate eyes). The examiner then placed the base-down prism over the left eye and observed the fixation pattern, followed by a rapid cover-uncover test to confirm fixation. The examiner recorded one of five possible responses (Table 1).
Table 1.
The Pediatric Eye Disease Investigator Group (PEDIG) fixation preference test
| Category | Criteria |
|---|---|
| Right eye fixation | Only fixates with right eye only or immediate refixation to right eye |
| Prefers right eye fixation | Holds fixation for 1 second or more with left eye but does not freely alternate |
| Alternates fixation | Alternates fixation |
| Prefers left eye fixation | Holds fixation for 1 second or more with right eye but does not freely alternate |
| Left eye fixation | Fixates with left eye only or immediate refixation to left eye |
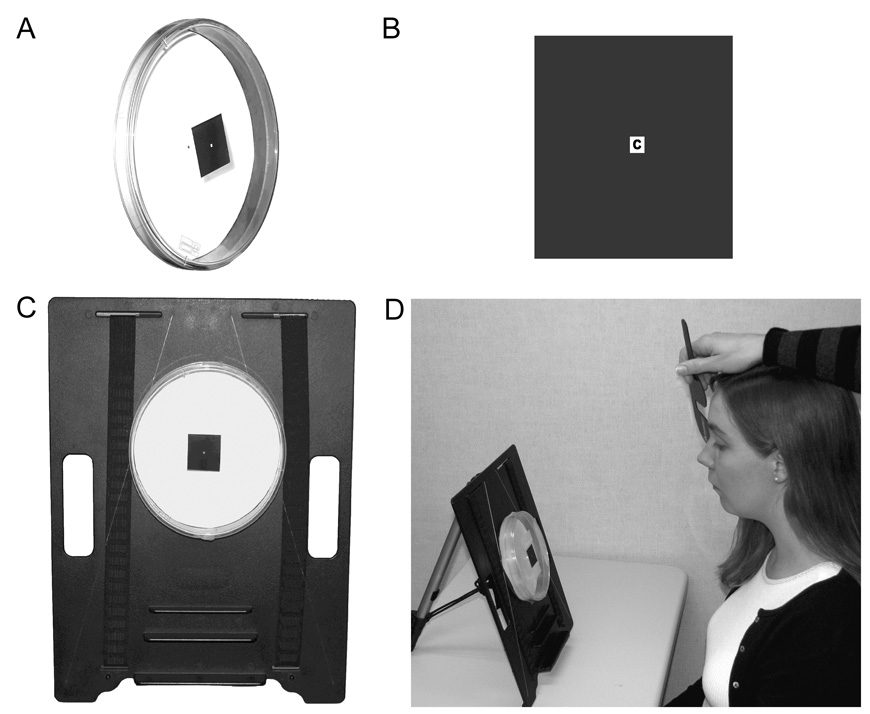
The fourth test performed was a new near hole-in-the-card test, based on the principle of the distance hole-in-the-card test (Figure). A 25 mm × 150 mm Falcon® polyethylene culture dish was used (BD Biosciences, San Jose, CA, Figure, panel A). A 30 mm black square with a 1.5 mm square opening was attached to the front of the culture dish (Figure, panel B) centered over a letter (1 mm in height and width) fixed to a white background inside the base of the dish. The distance between the hole and the viewing letter was therefore 25 mm. The culture dish was attached to a reading stand (Figure, panel C). The subject sat at a desk in front of the reading stand and adjusted the height of the chair if necessary in order to visualize the letter through the opening with both eyes open. After the subject viewed the letter binocularly, the subject was instructed not to move their head. The examiner covered the left eye and asked the subject if they could still see the letter. The examiner then covered the right eye and asked again if the subject could still see the letter. The eye that could see the letter was recorded as the dominant eye (right or left). If the subject was able to see the letter with both the right and the left eye, the dominant eye was recorded as “neither.”
Figure. Near hole-in-the-card test.
This test was based on the design of the distance hole-in-the-card test. (A) A 25 mm × 150 mm Falcon® polyethylene culture dish was used (BD Biosciences, San Jose, CA). (B) A 30 mm black square with a 1.5 mm square opening was attached to the front of the culture dish centered over a letter (1 mm in height and width) that was fixed to a white background inside the dish. (C) The apparatus was attached to a reading stand to allow the proper viewing angle. (D) The near-hole-in-the-card test is shown in use.
After all four tests were administered in succession, they were re-administered a second time in the same order to evaluate test-retest reliability.
Statistical analysis
Test-retest reliability and agreement between tests was evaluated with the Kappa statistic. The response in the first administered test was used for comparison between each of the four dominance tests and for comparison with the subject’s responses to the questions. The PEDIG fixation preference test data were collapsed from five categories to three categories to allow comparison to the other tests and questions: “Prefers right” and “right fixation” were collapsed into “right,” “prefers left” and ‘left fixation” were collapsed into “left,” and “alternates” was called “neither.”
The Kappa tests were interpreted as follows:3 Perfect agreement, k = 1.0; Almost perfect agreement, k = 0.81–1.0; Substantial agreement, k = 0.61 – 0.80; Moderate agreement, k = 0.41–0.60; Fair agreement, k = 0.21 – 0.40; Slight agreement, k = 0.00 – 0.20. All analyses were conducted using SAS software version 9.1.3 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
Subject demographics
Forty-six subjects between the ages of 18 and 78 years (median age of 42.5 years) were enrolled. Seventy-two percent (33 of 46) were female. Visual acuity ranged from 20/20 to 20/40 (median 20/20) at distance and 20/15 to 20/40 (median 20/20) at near. Ninety-six percent (44 of 46) of the subjects were white.
Questions on dominance and handedness
Fifty-seven percent (26 of 46) of subjects reported right eye dominance when responding to the question, “Which is your dominant eye?” Over half of the subjects (27 of 46) reported that they sight a gun using their right eye and thirty-five percent (16 of 46) did not know which eye they would use to sight a gun. Most subjects (40 of 46) reported that they would use their right eye when using a camera. Furthermore, almost all of the subjects (43 of 46) were right-handed, one was ambidextrous, and two were left-handed.
Test-retest reliability for each dominance test
Test-retest reliability was substantial or almost perfect for all four dominance or fixation tests. The near convergence test had almost perfect test-retest reliability (k = 0.84, Table 2). The distance hole-in-the-card test, the PEDIG fixation preference test, and the new near hole-in-the-card test had substantial agreement (k = 0.77, 0.77, 0.62 respectively, Table 2).
Table 2.
Agreement of ocular dominance tests
| Distance hole-in-the-card test | Near hole-in-the-card test | PEDIG fixation preference test | Near convergence test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Left | Neither | Right | Left | Neither | Right | Left | Neither | Right | Left | Neither | Right | ||
 |
Left | 16 | 0 | 3 | 7 | 0 | 12 | 7 | 11 | 1 | 13 | 3 | 3 |
| Neither | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Right | 2 | 0 | 25 | 0 | 0 | 27 | 0 | 18 | 9 | 4 | 7 | 16 | |
 |
Left | 4 | 0 | 3 | 2 | 5 | 0 | 5 | 1 | 1 | |||
| Neither | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||
| Right | 1 | 0 | 38 | 5 | 24 | 10 | 12 | 9 | 18 | ||||
 |
Left | 7 | 0 | 0 | 5 | 1 | 1 | ||||||
| Neither | 4 | 25 | 0 | 11 | 7 | 11 | |||||||
| Right | 0 | 2 | 8 | 1 | 2 | 7 | |||||||
 |
Left | 15 | 0 | 2 | |||||||||
| Neither | 0 | 10 | 0 | ||||||||||
| Right | 4 | 0 | 15 | ||||||||||
Agreement between different ocular dominance tests
None of the tests compared had perfect, almost perfect, or substantial agreement. The distance hole-in-the-card test had moderate agreement with both the near convergence test (k=0.47) and the near hole-in-the-card test (k = 0.41, Table 2).
All other pairs of tests had fair to slight agreement (Table 2). The distance hole-in-the-card test had fair agreement with the PEDIG fixation preference test (k = 0.32). The near convergence test had fair agreement with the PEDIG fixation preference test (k = 0.27). The near hole-in-the-card test had slight agreement with the near convergence test (k = 0.19) and the PEDIG fixation preference test (k = 0.11).
Agreement between ocular dominance tests and questions
Self-reported dominance (in response to the question “Which is your dominant eye?”) agreed moderately well with dominance determined by the distance hole-in-the-card test (k = 0.50). Self-reported dominance had fair agreement with the PEDIG fixation preference test (k = 0.33), near hole-in-the-card test (k = 0.28), and near convergence test (k = 0.27). Handedness, which eye they used to sight a gun, and which eye used to sight a camera agreed slightly or poorly with all four dominance tests.
DISCUSSION
We found excellent test-retest reliability for each ocular dominance test. Nevertheless, there was only moderate to slight agreement between each possible pairing of tests, and moderate to poor agreement between each possible pairing of tests with questions. The poor agreement between tests appears to be the result of differences in testing distance and in the specific activity performed with each test, and raises several issues regarding the uses of ocular dominance tests in clinical practice.
The optimum method for evaluating ocular dominance is a topic of controversy. There is no accepted gold standard. According to Mapp,4 ocular dominance tests can be broadly divided into 1) sighting tests (e.g., the hole in the card tests), 2) sensory tests (e.g., binocular rivalry tests5, 6), and 3) asymmetry in visual acuity or contrast sensitivity. We limited our study to visually normal adults with no more than 0.1 logMAR interocular difference in acuity, and therefore did not study asymmetry of visual acuity. We also did not test binocular rivalry as described by Handa et al5, 6 because we wanted to use simple office based methods.
Our present study raises the question of whether a single test of ocular dominance can be used to adequately represent which eye an individual subject uses for most activities. Several authors have also found little to moderate correlation between dominance tests.7, 8 Furthermore, Pointer reported little correlation among handedness, the dominant eye (determined by a sighting dominance test), and the eye with best visual acuity.9 Several authors10–12 suggest that the dominant eye in a sighting task is merely a result of the ease or habit of using a particular eye to perform the task. Mapp also suggests that the sighting dominant eye has no special role for visual or oculomotor processes for the normal population.4 Crider reported that 93% of 830 subjects showed dominance of one eye, but many subjects performed differently on different sighting tests.13 Our study also found lack of agreement between tests, as only two comparisons had moderate agreement: the distance hole-in-the-card test versus the near convergence test and the distance hole-in-the-card test versus the near hole-in-the-card test. Overall, we found moderate to poor agreement between tests and between questions and tests; therefore, using a single question or test appears inadequate to assess dominance.
Regarding the clinical relevance of dominance, some authors have suggested that dominance is important in determining whether a monocular condition is likely to be symptomatic or not. Waheed and Laidlaw studied the association between visual handicap, laterality, and historical eye dominance in 44 patients with macular holes.14 Seventy-six percent with a macular hole in their dominant eye presented due to symptoms, whereas only 36% with a macular hole in their non-dominant eye presented due to symptoms.14 Nevertheless, another smaller study of 10 patients with macular degeneration found that dominance (as assessed by distance sighting) does not play a role in patients seeking care (De Alba F, Mirza R, and Jay W: The Role of Ocular Dominance in Patients Presenting with Asymmetric Macular Degeneration [abstract]. Invest Ophthalmol Vis Sci 2005; 46: eSupplement p625).
The relationship between ocular dominance and patient satisfaction with monovision by intraocular lens implantation has been investigated by Handa et al,15 who determined ocular dominance using the distance hole-in-the-card sighting dominance test and a binocular rivalry balance sensory dominance technique. The authors conclude that strength of sighting dominance seems to be an important factor for patient satisfaction with monovision.15 Nevertheless, for a given patient with monovision the difference between near and distance dominance may be important, and our study suggests that some subjects may be left eye dominant for distance and right eye dominant for near (Table 2). This subject is worthy of further study.
In treating amblyopia, the role of fixation preference, and the best method of assessing fixation preference, is not clear. In a randomized trial of patching versus atropine for amblyopia, some subjects treated with atropine improved despite no apparent switch of near fixation to the amblyopic eye.16, 17 This finding raises the question of whether fixation on a light or toy, the method used in these studies, adequately indicates which eye a child is using for near fixation. The PEDIG fixation preference test might be considered the closest surrogate to everyday near reading tasks, but it is interesting that it did not agree well with the near hole-in-the-card test and the near convergence test in our study. It is possible that the differential intensity of the tasks (reading versus sighting a single letter) accounts for some of the differences between tests, but if specific activity was the most important factor in dominance, one would hypothesize that the two sighting tasks (distance hole-in-the-card test and near hole-in-the-card test) would be similar. This was not the case.
While we found good overall test-retest reliability for each dominance test, in a few subjects (e.g., six of 46 (13%) for the near convergence test), ocular dominance varied from one test administration to the other (Table 2). Our findings may have been strengthened if we had administered each dominance test three or more times, allowing a summary of responses when disagreement occurred between administrations.
Our study shows substantial test-retest reliability for each ocular dominance test, but only moderate to slight agreement between tests. It appears that results of ocular dominance tests vary depending on testing distance and depending on the specific activity performed as part of the testing procedure. Further work is needed to define the relationships between ocular dominance tests and tests of fixation preference.
Acknowledgments
Supported by: National Institutes of Health Grants EY015799 and EY011751 (JMH), Research to Prevent Blindness, Inc., New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, MN
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Study was conducted in the Department of Ophthalmology, Mayo Clinic College of Medicine.
Presented in part as a paper presentation at the Association for Research in Vision and Ophthalmology Annual Meeting, May, 2006.
Potential Financial Conflicts: None
REFERENCES
- 1.von Noorden GK, Campos EC. Examination of the Patient - IV. In: Lampert R, Cox K, Burke D, editors. Binocular Vision and Ocular Motility: Theory and Management of Strabismus. 6th ed. St. Louis, MO: Mosby; 2002. pp. 246–297. [Google Scholar]
- 2.Holmes JM, Beck RW, Repka MX, Leske DA, Kraker RT, Blair RC, et al. The amblyopia treatment study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–1353. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 3.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 4.Mapp AP, Ono H, Barbeito R. What does the dominant eye dominate? A brief and somewhat contentious review. Perception & Psychophysics. 2003;65:310–317. doi: 10.3758/bf03194802. [DOI] [PubMed] [Google Scholar]
- 5.Handa T, Mukuno K, Uozato H, Niida T, Shoji N, Shimizu K. Effects of dominant and nondominant eyes in binocular rivalry. Optometry & Vision Science. 2004;81:377–383. doi: 10.1097/01.opx.0000135085.54136.65. [DOI] [PubMed] [Google Scholar]
- 6.Handa T, Uozato H, Higa R, Nitta M, Kawamorita T, Ishikawa H, et al. Quantitative measurement of ocular dominance using binocular rivalry induced by retinometers. Journal of Cataract & Refractive Surgery. 2006;32:831–836. doi: 10.1016/j.jcrs.2006.01.082. [DOI] [PubMed] [Google Scholar]
- 7.Buxton C, Crosland H. The concept of "eye preference". Am J Psychol. 1937;49:458–461. [Google Scholar]
- 8.Washburn M, Faison C, Scott R. A comparison between the Miles A-B-C method and retinal rivalry as tests of ocular dominance. Am J Psychol. 1934;46:633–636. [Google Scholar]
- 9.Pointer JS. Sighting dominance, handedness, and visual acuity preference: three mutually exclusive modalities? Ophthalmic Physiol Opt. 2001;21:117–126. doi: 10.1046/j.1475-1313.2001.00549.x. [DOI] [PubMed] [Google Scholar]
- 10.Ono H, Barbeito R. The cyclopean eye vs. the sighting-dominant eye as the center of visual direction. Perception & Psychophysics. 1982;32:201–210. doi: 10.3758/bf03206224. [DOI] [PubMed] [Google Scholar]
- 11.Barbeito R. Sighting dominance: an explanation based on the processing of visual direction in tests of sighting dominance. Vision Res. 1981;21:855–860. doi: 10.1016/0042-6989(81)90185-1. [DOI] [PubMed] [Google Scholar]
- 12.Miles W. Ocular dominance: methods and results. Psychol Bull. 1928;25:155–156. [Google Scholar]
- 13.Crider B. A battery of tests for the dominant eye. J Gen Psychol. 1944;31:179–190. [Google Scholar]
- 14.Waheed K, Laidlaw DA. Disease laterality, eye dominance, and visual handicap in patients with unilateral full thickness macular holes. Br J Ophthalmol. 2003;87:626–628. doi: 10.1136/bjo.87.5.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Handa T, Mukuno K, Uozato H, Niida T, Shoji N, Minei R, et al. Ocular dominance and patient satisfaction after monovision induced by intraocular lens implantation. Journal of Cataract & Refractive Surgery. 2004;30:769–774. doi: 10.1016/j.jcrs.2003.07.013. [DOI] [PubMed] [Google Scholar]
- 16.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs. patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120:268–278. doi: 10.1001/archopht.120.3.268. [DOI] [PubMed] [Google Scholar]
- 17.Pediatric Eye Disease Investigator Group. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111:2076–2085. doi: 10.1016/j.ophtha.2004.04.032. [DOI] [PubMed] [Google Scholar]