Abstract
The integration of knowledge concerning the regulation of MT, a highly conserved, low molecular weight, cystein-rich metalloprotein, on its proposed functions is necessary to clarify how MT affects cellular processes. MT expression is induced/enhanced in various tissues by a number of physiological mediators. The cellular accumulation of MT depends on the availability of cellular zinc derived from the diet. MT modulates the binding and exchange/transport of heavy metals such as zinc, cadmium, or copper under physiological conditions and cytoprotection from their toxicities, and the release of gaseous mediators such as hydroxyl radicals or nitric oxide. In addition, MT reportedly affects a number of cellular processes, such as gene expression, apoptosis, proliferation, and differentiation. Given the genetic approach, the apparently healthy status of MT-deficient mice argues against an essential biological role for MT; however, this molecule may be critical in cells/tissues/organs in times of stress, since MT expression is also evoked/enhanced by various stresses. In particular, because metallothionein (MT) is induced by inflammatory stress, its roles in inflammation are implied. Also, MT expression in various organs/tissues can be enhanced by inflammatory stimuli, implicating in inflammatory diseases. In this paper, we review the role of MT of various inflammatory conditions.
1. Introduction
Metallothioneins (MTs) discovered as cadmium-binding protein from horse kidney approximately five decades ago, and were later characterized as a low molecular weight protein with a high cysteine content and a high affinity for divalent important metals, such as zinc and copper, and unimportant ones, such as cadmium and mercury (Margoshes) [1]. Because of their high metal content and unusual bioinorganic structure, they are classified as metalloproteins [2]. MTs are unusually rich in cysteine residues that coordinate multiple zinc and copper atoms under physiological conditions.
2. Classification
In mice, there are 4 MT genes that reside in a 50-kb region on chromosome 8 [3]. The mouse MT-I and–II genes are expressed at all stages of development in many cell types of most organs; they are coordinately regulated by metals, glucocorticoids, and inflammatory stress [4]. MT-III is expressed predominantly in not only neurons but also in glia and male reproductive organs [5–7]. MT-IV is expressed in differentiating stratified squamous epithelial cells [3]. All four MT genes are expressed in the maternal deciduum [8]. In humans, whereas, MTs are encoded by a family of genes consisting of 10 functional MT isoforms, and the encoded proteins are conventionally subdivided into 4 groups: MT-1, MT-2, MT-3, and MT-4 proteins [9]. While a single MT-2A gene encodes MT-2 protein, MT-1 protein comprises many subtypes encoded by a set of MT-1 genes (MT-1A, MT-1B, MT-1E, MT-1F, MT-1G, MT-1H, and MT-1X), accounting for the microheterogeneity of the MT-1 protein [2]. As shown above, there are multiple MT genes, expressed in distinct patterns, suggesting that they possess important functions; however, whether they have redundant or divergent functions under both physiological and pathological conditions is not fully understood, although the known functions of MTs include metalloregulatory roles in cell growth, differentiation, and apoptosis and the enhanced synthesis of MTs in rapidly proliferating tissues, implying their crucial role in normal and neoplastic cell growth [10].
3. Characteristics
These intracellular proteins are characterized by their unusually high cysteine content (30%) and lack of aromatic amino acids. Because of their thiol rich content, MTs can bind to a number of trace metals such as cadmium, mercury, platinum, and silver, and protect cells and tissues against the toxicity of these metals. Furthermore, MTs are among the most abundant components interacting with the biologically essential metals zinc and copper. MT metal-thiolate fractions, being dynamic and of a high affinity, also facilitate metal exchange in tissues [11].
MTs are present in a great variety of eukaryotes [12], functioning as antioxidants; they also play a protective role against hydroxyl-free radicals. This is relevant in tumors which are known to be markedly radiosensitive, where radiotherapy is the treatment of choice [13].
4. Function under Physiological Conditions
The putative functions of MT include intracellular metal metabolism and/or storage, metal donation to target apometalloproteins (especially zinc finger proteins and enzymes), metal detoxification, and protection against oxidants and electrophils [14]. Evidence for these functions originally came from traditional animal, cell culture, and in vitro models. Furthermore, these studies have been supported by experiments using murine models with the targeted deletion or transgenic overexpression of MT genes. MT most likely functions in the regulation of zinc metabolism [14]. Elevations of dietary zinc induce/enhance intestinal MT [15], whereas maximal intestinal Zn accumulation seems to depend on MT synthesis [16]. MT (−/−) mice accumulate less zinc in the distal gastrointestinal tract when fed a high zinc diet [17]. In most studies, zinc absorption was inversely related to the intestinal MT content after MT was induced by dietary, parenteral zinc, or by fasting [14]. Studies using transgenic and knockout mice have confirmed that MT can alter the processing of zinc taken orally because the serum zinc concentration was inversely related to the intestinal MT level in these mice after single oral doses of zinc [17, 18]. In turn, urinary Zn excretion levels measured during a fast or Zn intake restriction were greater in MT (−/−) mice than in MT (+/+) mice [19]. As well, the increase in hepatic Zn concentration after the administration of lipopolysaccharide (LPS) was found in MT (+/+) but not in MT (−/−) mice [20]. These results suggest that MT has the ability to retain Zn under physiological and pathological conditions. On the other hand, tissue Zn concentration was reduced, and the sensitivity to Zn deficiency during pregnancy was enhanced in MT (−/−) mice [21], and further, Zn deficiency caused abnormalities in neonate kidney differentiation in MT (−/−) mice [22]. Conversely, in MT-transgenic mice, Zn was accumulated in female organs, and the teratogenicity of Zn deficiency during pregnancy was significantly ameliorated. Taken together, MT is likely to have a Zn metabolizing activity in the individual level [23].
Besides, MT demonstrates strong antioxidant properties. MT protein levels in rodent liver [24, 25] and mRNA levels in hepatic cell lines [26] are increased following injection with compounds that result in free radical formation, for example, carbon tetrachloride, menadione, or paraquat. An injection of ferric nitrilotriacetate, which produces reactive oxygen species (ROS), induces transcriptional level of MT in the liver and kidney [27]. These findings suggest that MT plays a role in oxidative stress. Consistent with this, MT is able to scavenge a wide range of ROS including superoxide, hydrogen peroxide, hydroxyl radicals, and nitric oxide [19, 28, 29]. In particular, it has been shown that the ability of MT to capture hydroxyl radicals, which are primarily responsible for the toxicity of ROS, is three hundred-times greater than that of glutathione [30], the most abundant antioxidant in the cytosol [19]. Further, metal-thiolate clusters are reportedly oxidized in vitro; thus, they could scavenge deleterious oxygen radicals. Compelling genetic evidence for this concept comes from work using yeast. In brief, yeast that cannot synthesize copper MTs are more sensitive to oxidative stress if they also lack superoxide dismutase, suggesting that yeast MT has antioxidant functions [31]. In addition, the expression of monkey MTs under the control of the yeast MT promoter also protects against oxidative stress [31]. Many agents that induce oxidative stress, such as chloroform, turpentine, diethyl maleate, paraquat, and H2O2, can also induce MT-I and MT-II in vitro and in vivo [24, 26, 32]. This strongly suggests that MT is involved in protecting against oxidative damage. Conversely, mammalian cells that express excess MTs appear to be resistant to the toxic effects of nitric oxide [33] and many electrophilic antineoplastic agents [34], which are capable of reacting with the cysteines of MT. Further, relatively recent studies have demonstrated that MT is induced by oxidative stress-producing chemicals [35], and exhibits cytoprotection against oxidative stress-related organ damage in vivo [36, 37].
Despite the confirmed roles of MT under physical conditions, as mentioned above, a complete identification of all the functions of this unique protein within an integrative context has yet to emerge, particularly under pathophysiological conditions. Particularly, since proinflammatory cytokines including interleukin (IL)-1, IL-6, and interferon-γ also induce hepatic MT gene expression in vivo [38–40], the roles of MT in inflammation have been focused on. There are conflicting reports about the role of MT in inflammatory processes. In fact, MT (−/−) mice were resistant to tumor necrosis factor (TNF)-induced lethal shock compared to MT (+/+) mice [38]. MT-I-overexpressing mice are more sensitive to the lethal effects of TNF than MT (+/+) mice [38]. In contrast, Kimura et al. have reported that MT (−/−) mice are more susceptible to LPS-induced lethal shock in D-galactosamine (GalN)-sensitized mice through the reduction of alpha (1)-acid glycoprotein than MT (+/+) mice [41]. Accordingly, it seems that the roles of MT in inflammation depend on pathophysiologic conditions (site, route of stimuli, and type).
Whereas, to date, inflammatory diseases such as systemic inflammatory response syndrome including acute lung injury, allergic asthma, oxidative lung injury, and acute liver injury are as yet refractory and/or hindering daily life, possibly due to the incomplete understanding of molecular targets. Thus, investigation for the role of MT in these inflammatory diseases may provide hint for novel therapeutic options.
5. Function of MT under Pathophysiological Conditions in Inflammation
5.1. Role of MT in Lung Injury Related to LPS
Previous as well as our recent studies have shown the expression of MT in the lung [39, 42]. Immunohistopathological examination led to the detection of immunoreactive MT-I/II proteins in the lungs in endothelial and alveolar epithelial cells of MT (+/+) mice, whereas they were not detected in those of MT (−/−) mice. Furthermore, the expression was confirmed to be enhanced by oxidative stimuli like LPS and ozone (O3) exposure (data not shown).
The intratracheal instillation of LPS produces a well-recognized model of acute lung injury, leading to the activation of alveolar macroghages, tissue infiltration of neutrophils, and interstitial edema [43]. Although the inhalation of LPS has been reported to induce MT expression in the lung in vivo [39, 42], there is no evidence regarding the direct contribution of MT in acute lung injury related to LPS.
MT (−/−) and MT (+/+) mice were administered vehicle or LPS (125 μg/kg) intratracheally. Thereafter, the cellular profile of the bronchoalveolar lavage (BAL) fluid, pulmonary edema, lung histology, expression of proinflammatory molecules, and nuclear localization of nuclear factor-κ B (NF-κ B) in the lung were evaluated. As a result, MT (−/−) mice were more susceptible than MT (+/+) mice to neutrophilic lung inflammation and lung edema, which was induced by intratracheal challenge with LPS. After LPS challenge, MT deficiency enhanced the vacuolar degeneration of pulmonary endothelial and type I alveolar epithelial cells, and caused a focal loss of the basement membrane. However, unexpectedly, LPS treatment induced no significant differences neither in the enhanced expression of proinflammatory cytokines and chemokines, nor in the activation of the NF-κ B pathway in the lung between the two genotypes. Lipid peroxide levels in the lungs were significantly higher in LPS-treated MT (−/−) than LPS-treated MT (+/+) mice. These findings suggest that MT protects against acute lung injury related to LPS. The effects are possibly mediated via the enhancement of pulmonary endothelial and epithelial integrity, not via inhibition of the NF-κ B pathway [44].
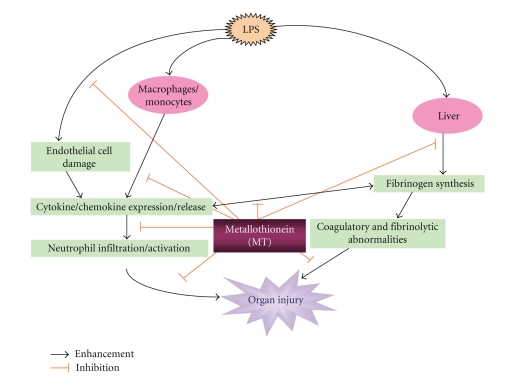
Next, MT (−/−) and MT (+/+) mice were administered vehicle or LPS (30 mg/kg) intraperitoneally. Thereafter, coagulatory parameters, organ histology (lung, liver, and kidney), and the local expression of proinflammatory molecules were evaluated. As a result, compared with MT (+/+) mice, MT (−/−) mice showed a significant prolongation of the prothrombin time (PT) and activated partial thromboplastin time (APTT), a significant increase in the levels of fibrinogen and fibrinogen/fibrin degradation products, and a significant decrease in activated protein C, after LPS treatment. LPS induced inflammatory organ damage in the lung, kidney, and liver in both genotypes of mice. The damage including neutrophil infiltration in the organs was more prominent in MT (−/−) than MT (+/+) mice after LPS treatment. In both genotypes of mice, LPS enhanced the protein expression of interleukin (IL)-1β, IL-6, granulocyte/macrophage-colony-stimulating factor, macrophage inflammatory protein (MIP)-1α, MIP-2, macrophage chemoattractant protein-1, and keratinocyte-derived chemoattractant (KC) in the lung, kidney, and liver and circulatory levels of IL-1β, IL-6, MIP-2, and KC. In overall trends, however, the levels of these proinflammatory proteins were greater in MT (−/−) than in MT (+/+) mice after LPS challenge. Our results suggest that MT protects against coagulatory and fibrinolytic disturbance and multiple organ damage including lung injury induced by LPS, at least partly, via inhibition of the local expression of proinflammatory proteins in this model (Figure 1) [45]. Nonetheless, its underlying mechanistic pathways including new ones (e.g., Toll-like receptors [46], NALP inflammasomes [47], neurotensin [48], RANK-RANKL [49]) remain to be explored in future.
Figure 1.
Hypothesized mechanisms of cytoprotection of MT in LPS-related inflammation. Figure reproduced with some modifications with permission from FASEB journal [45].
5.2. Role of MT in Allergic Inflammation
Bronchial asthma is a complex syndrome, characterized by obstruction, hyperresponsiveness, and persistent inflammation of the airways. Inflammation in asthma is characterized by an accumulation of eosinophils, lymphocytes, and neutrophils in the bronchial wall and lumen [50–52]. The mechanisms via which inflammatory cells alter airway function in asthmatic conditions include the release of Th2 cytokines (IL-4, IL-5, and IL-13) and chemotactic mediators such as thymus and activation-regulated chemokine, macrophage-derived chemokine, and eotaxin, and various proteases as well as the generation of reactive oxygen species. Thus, next, we determined the role of MT in allergic airway inflammation induced by ovalbumin (OVA) using MT (−/−) mice. MT (−/−) and MT (+/+) mice were intratracheally challenged with OVA (1 μg/body) biweekly 3 times. Thereafter, the cellular profile of the BAL fluid, lung histology, and expression of proinflammatory molecules in the lung were evaluated. After the final OVA challenge, significant increases were noted in the numbers of total cells, eosinophils, and neutrophils in BAL fluid in MT (−/−) mice compared to those in MT (+/+) mice. Histopathologically, in the presence of OVA, the number of inflammatory cells including eosinophils and neutrophils in the lung was larger in MT (−/−) than in MT (+/+) mice. The protein level of IL-1β was significantly greater in MT (−/−) than in MT (+/+) mice after OVA challenge. Immunohistochemistry showed that the formations of 8-hydroxy-2′-deoxyguanosine, a proper marker of oxidative DNA damage, and nitrotyrosine in the lung were more intense in MT (−/−) than in MT (+/+) mice after OVA challenge. These results indicate that endogenous MT protects against allergic airway inflammation induced by OVA, at least partly, via suppression of the enhanced lung expression of IL-1β and via its antioxidative potential [53].
5.3. Role of MT in Oxidative Lung Injury
Ozone (O3) is a highly toxic principal oxidant found in urban environments throughout the world. Experimental research has shown that O3 inhalation causes airway inflammation/injury in vivo [54]. Furthermore, O3 is a strong oxidizing agent that can be rapidly converted into a number of ROS, including hydrogen peroxide [55, 56]. In fact, O3-induced lung inflammation/injury comprises oxidative stress-related tissue injury [57–59]. Also, O3 exposure reportedly results in oxidative stress in the airway, possibly through the disruption of iron homeostasis [59]; iron can increase oxidant generation after O3 interaction with aqueous media and produce hydroxyl radicals [60, 61]. On the other hand, lung expression of MT is reportedly induced by O3 exposure in vivo [62, 63]. Thus, we next examined the role of MT in lung inflammation induced by subacute exposure to O3 using MT (−/−) mice. After subacute exposure to O3 (0.3 ppm), the cellular profile of BAL fluid, pulmonary edema, lung histology, and expression of proinflammatory molecules in the lung were evaluated. Exposure to O3 induced lung inflammation and enhanced vascular permeability, which was significantly greater in MT (−/−) than in MT (+/+) mice. Electron microscopically, O3 exposure induced the vacuolar degeneration of pulmonary endothelial and epithelial cells, and interstitial edema with focal loss of the basement membrane, which was more prominent in MT (−/−) than in MT (+/+) mice. O3-induced lung expression of IL-6 was significantly greater in MT (−/−) than in MT (+/+) mice; however, lung expression of the chemokines such as eotaxin, macrophage chemoattractant protein-1, and keratinocyte-derived chemoattractant was comparable between both genotypes of mice in the presence of O3. Following O3 exposure, the formation of oxidative stress-related molecules/adducts, such as heme oxygenase-1, inducible nitric oxide synthase, 8-OHdG, and nitrotyrosine in the lung was significantly greater in MT (−/−) than in MT (+/+) mice. Collectively, MT protects against O3-induced lung inflammation, at least partly, via the regulation of pulmonary endothelial and epithelial integrity and its antioxidative property (64).
5.4. Role of MT in Lethal Liver Injury
Liver has high levels of Zn- and Cu-bound MT and has a high capacity to regenerate. MT is reportedly involved in hepatocyte regeneration after partial hepatectomy [64–67] and chemical injury [68]. Similarly, previous studies have shown that induction of MT can protect animals from hepatotoxicity of several chemicals, such as ethanol, carbon tetrachloride, acetaminophen, and cadmium [69].
Hepatic dysfunction due to liver disorders such as viral hepatitis, liver cirrhosis, and hepatocellular carcinoma is frequently associated with lethal coagulopathy such as DIC. Kimura et al. previously reported that MT is protective against acute liver injury induced by LPS/D- GalN through the suppression of TNF-α production/release using MT (−/−) mice [41]. An animal model of acute (lethal) liver injury using LPS/D-GalN develops severe coagulopathy with histological evidence of DIC [70] quite similar to that in humans. Furthermore, most coagulatory factors as well as MT are produced mainly in the liver, indicating a possible role of MT in the pathogenesis of hepatic disorder-related coagulopathy. Besides, our above mentioned study has implicated MT in pathophysiology of coagulatory disturbance [45]. To expand the findings by Kimura et al., therefore, we explored the role of MT in coagulatory disturbance during acute liver injury induced by LPS/D-GalN. Both MT (−/−) and MT (+/+) mice were injected intraperitoneally with 30 μg/kg of LPS and 800 mg/kg of D-GalN dissolved in vehicle. Five hours after the injection, blood samples were collected and platelet counts and coagulatory parameters were measured. LPS/D-GalN challenge significantly decreased platelet number in both genotypes of mice in a time-dependent fashion as compared to vehicle challenge. However, in the presence of LPS/D-GalN, the decrease was significantly greater in MT (−/−) than in MT (+/+) mice. LPS/D-GalN challenge caused prolongation of the plasma coagulatory parameters such as PT and APTT in both genotypes of mice as compared with vehicle challenge. In the presence of LPS/D-GalN, PT and APTT were longer in MT (−/−) than in MT (+/+) mice. The level of fibrinogen significantly decreased 5 hours after LPS/D-GalN challenge in both genotypes of mice as compared to vehicle challenge. After LPS/D-GalN challenge, the level was significantly lower in MT (−/−) than in MT (+/+) mice. As compared to vehicle administration, LPS/D-GalN administration elicited an increase in the plasma level of von Willebrand factor in both genotypes of mice. Further, in the presence of LPS/D-GalN, the level was significantly greater in MT (−/−) than in MT (+/+) mice ([71].
6. Conclusion
MTs play important roles in the physiological condition, such as heavy metal homeostasis and radical scavenging. Furthermore, through a genetic approach, MT has been shown to protect against various types of (including LPS-related, allergic, and oxidative) inflammatory conditions in mice, implicating MT-induction/enhancement and/or zinc supplementation to induce/enhance MT as possible therapeutic options for inflammatory diseases, although additional research is needed to conclude its clinical utility.
References
- 1.Kägi JHR, Valee BL. Metallothionein: a cadmium- and zinc-containing protein from equine renal cortex. The Journal of Biological Chemistry. 1960;235(12):3460–3465. [PubMed] [Google Scholar]
- 2.Thirumoorthy N, Manisenthil Kumar KT, Sundar AS, Panayappan L, Chatterjee M. Metallothionein: an overview. World Journal of Gastroenterology. 2007;13(7):993–996. doi: 10.3748/wjg.v13.i7.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quaife CJ, Findley SD, Erickson JC, et al. Induction of a new metallothionein isoform (MT-IV) occurs during differentiation of stratified squamous epithelia. Biochemistry. 1994;33(23):7250–7259. doi: 10.1021/bi00189a029. [DOI] [PubMed] [Google Scholar]
- 4.Palmiter RD. Molecular biology of metallothionein gene expression. Experientia Supplementum. 1987;52:63–80. doi: 10.1007/978-3-0348-6784-9_4. [DOI] [PubMed] [Google Scholar]
- 5.Masters BA, Quaife CJ, Erickson JC, et al. Metallothionein III is expressed in neurons that sequester zinc in synaptic vesicles. The Journal of Neuroscience. 1994;14(10):5844–5857. doi: 10.1523/JNEUROSCI.14-10-05844.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uchida Y, Takio K, Titani K, Ihara Y, Tomonaga M. The growth inhibitory factor that is deficient in the Alzheimer's disease brain is a 68 amino acid metallothionein-like protein. Neuron. 1991;7(2):337–347. doi: 10.1016/0896-6273(91)90272-2. [DOI] [PubMed] [Google Scholar]
- 7.Moffatt P, Séguin C. Expression of the gene encoding metallothionein-3 in organs of the reproductive system. DNA and Cell Biology. 1998;17(6):501–510. doi: 10.1089/dna.1998.17.501. [DOI] [PubMed] [Google Scholar]
- 8.Liang L, Fu K, Lee DK, Sobieski RJ, Dalton T, Andrews GK. Activation of the complete mouse metallothionein gene locus in the maternal deciduum. Molecular Reproduction and Development. 1996;43(1):25–37. doi: 10.1002/(SICI)1098-2795(199601)43:1<25::AID-MRD4>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 9.West AK, Stallings R, Hildebrand CE, Chiu R, Karin M, Richards RI. Human metallothionein genes: structure of the functional locus at 16q13. Genomics. 1990;8(3):513–518. doi: 10.1016/0888-7543(90)90038-v. [DOI] [PubMed] [Google Scholar]
- 10.Jin R, Chow VT-K, Tan P-H, Thameem Dheen S, Duan W, Bay B-H. Metallothionein 2A expression is associated with cell proliferation in breast cancer. Carcinogenesis. 2002;23(1):81–86. doi: 10.1093/carcin/23.1.81. [DOI] [PubMed] [Google Scholar]
- 11.Kondo Y, Woo ES, Michalska AE, Choo KH, Lazo JS. Metallothionein null cells have increased sensitivity to anticancer drugs. Cancer Research. 1995;55(10):2021–2023. [PubMed] [Google Scholar]
- 12.Kägi JHR, Schäffer A. Biochemistry of metallothionein. Biochemistry. 1988;27(23):8509–8515. doi: 10.1021/bi00423a001. [DOI] [PubMed] [Google Scholar]
- 13.Jayasurya A, Bay BH, Yap WM, Tan NG. Correlation of metallothionein expression with apoptosis in nasapharyngeal carcinoma. British Journal of Cancer. 2000;82(6):1198–1203. doi: 10.1054/bjoc.1999.1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis SR, Cousins RJ. Metallothionein expression in animals: a physiological perspective on function. Journal of Nutrition. 2000;130(5):1085–1088. doi: 10.1093/jn/130.5.1085. [DOI] [PubMed] [Google Scholar]
- 15.Cousins RJ, Lee-Ambrose LM. Nuclear zinc uptake and interactions and metallothionein gene expression are influenced by dietary zinc in rats. Journal of Nutrition. 1992;122(1):56–64. doi: 10.1093/jn/122.1.56. [DOI] [PubMed] [Google Scholar]
- 16.Richards MP, Cousins RJ. Mammalian zinc homeostasis: requirement for RNA and metallothionein synthesis. Biochemical and Biophysical Research Communications. 1975;64(4):1215–1223. doi: 10.1016/0006-291x(75)90822-0. [DOI] [PubMed] [Google Scholar]
- 17.Tran CD, Butler RN, Philcox JC, Rofe AM, Howarth GS, Coyle P. Regional distribution of metallothionein and zinc in the mouse gut: comparison with metallothionien-null mice. Biological Trace Element Research. 1998;63(3):239–251. doi: 10.1007/BF02778942. [DOI] [PubMed] [Google Scholar]
- 18.Coyle P, Philcox JC, Rofe AM. Metallothionein-null mice absorb less Zn from an egg-white diet, but a similar amount from solutions, although with altered intertissue Zn distribution. Journal of Nutrition. 1999;129(2):372–379. doi: 10.1093/jn/129.2.372. [DOI] [PubMed] [Google Scholar]
- 19.Sato M, Kondoh M. Recent studies on metallothionein: protection against toxicity of heavy metals and oxygen free radicals. The Tohoku Journal of Experimental Medicine. 2002;196(1):9–22. doi: 10.1620/tjem.196.9. [DOI] [PubMed] [Google Scholar]
- 20.Philcox JC, Sturkenboom M, Coyle P, Rofe AM. Metallothionein in mice reduces intestinal zinc loss during acute endotoxin inflammation, but not during starvation or dietary zinc restriction. Journal of Nutrition. 2000;130(8):1901–1909. doi: 10.1093/jn/130.8.1901. [DOI] [PubMed] [Google Scholar]
- 21.Andrews GK, Geiser J. Expression of the mouse metallothionein-I and -II genes provides a reproductive advantage during maternal dietary zinc deficiency. Journal of Nutrition. 1999;129(9):1643–1648. doi: 10.1093/jn/129.9.1643. [DOI] [PubMed] [Google Scholar]
- 22.Kelly EJ, Quaife CJ, Froelick GJ, Palmiter RD. Metallothionein I and II protect against zinc deficiency and zinc toxicity in mice. Journal of Nutrition. 1996;126(7):1782–1790. doi: 10.1093/jn/126.7.1782. [DOI] [PubMed] [Google Scholar]
- 23.Dalton T, Fu K, Palmiter RD, Andrews GK. Transgenic mice that overexpress metallothionein-I resist dietary zinc deficiency. Journal of Nutrition. 1996;126(4):825–833. doi: 10.1093/jn/126.4.825. [DOI] [PubMed] [Google Scholar]
- 24.Bauman JW, Madhu C, McKim JM, Jr., Liu Y, Klaassen CD. Induction of hepatic metallothionein by paraquat. Toxicology and Applied Pharmacology. 1992;117(2):233–241. doi: 10.1016/0041-008x(92)90242-k. [DOI] [PubMed] [Google Scholar]
- 25.Min K-S, Mukai S, Ohta M, Onosaka S, Tanaka K. Glucocorticoid inhibition of inflammation-induced metallothionein synthesis in mouse liver. Toxicology and Applied Pharmacology. 1992;113(2):293–298. doi: 10.1016/0041-008x(92)90127-e. [DOI] [PubMed] [Google Scholar]
- 26.Dalton T, Palmiter RD, Andrews GK. Transcriptional induction of the mouse metallothionein-I gene in hydrogen peroxide-treated Hepa cells involves a composite major late transcription factor/antioxidant response element and metal response promoter elements. Nucleic Acids Research. 1994;22(23):5016–5023. doi: 10.1093/nar/22.23.5016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Min K-S, Morishita F, Tetsuchikawahara N, Onosaka S. Induction of hepatic and renal metallothionein synthesis by ferric nitrilotriacetate in mice: the role of MT as an antioxidant. Toxicology and Applied Pharmacology. 2005;204(1):9–17. doi: 10.1016/j.taap.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 28.Thornalley PJ, Vasak M. Possible role for metallothionein in protection against radiation-induced oxidative stress. Kinetics and mechanism of its reaction with superoxide and hydroxyl radicals. Biochimica et Biophysica Acta. 1985;827(1):36–44. doi: 10.1016/0167-4838(85)90098-6. [DOI] [PubMed] [Google Scholar]
- 29.Kumari MVR, Hiramatsu M, Ebadi M. Free radical scavenging actions of metallothionein isoforms I and II. Free Radical Research. 1998;29(2):93–101. doi: 10.1080/10715769800300111. [DOI] [PubMed] [Google Scholar]
- 30.Vliagoftis H, Schwingshackl A, Milne CD, et al. Proteinase-activated receptor-2-mediated matrix metalloproteinase-9 release from airway epithelial cells. Journal of Allergy and Clinical Immunology. 2000;106(3):537–545. doi: 10.1067/mai.2000.109058. [DOI] [PubMed] [Google Scholar]
- 31.Tamai KT, Gralla EB, Ellerby LM, Valentine JS, Thiele DJ. Yeast and mammalian metallothioneins functionally substitute for yeast copper-zinc superoxide dismutase. Proceedings of the National Academy of Sciences of the United States of America. 1993;90(17):8013–8017. doi: 10.1073/pnas.90.17.8013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Min K-S, Terano Y, Onosaka S, Tanaka K. Induction of hepatic metallothionein by nonmetallic compounds associated with acute-phase response in inflammation. Toxicology and Applied Pharmacology. 1991;111(1):152–162. doi: 10.1016/0041-008x(91)90144-4. [DOI] [PubMed] [Google Scholar]
- 33.Schwarz MA, Lazo JS, Yalowich JC, et al. Metallothionein protects against the cytotoxic and DNA-damaging effects of nitric oxide. Proceedings of the National Academy of Sciences of the United States of America. 1995;92(10):4452–4456. doi: 10.1073/pnas.92.10.4452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palmiter RD. The elusive function of metallothioneins. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(15):8428–8430. doi: 10.1073/pnas.95.15.8428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bauman JW, Liu J, Liu YP, Klaassen CD. Increase in metallothionein produced by chemicals that induce oxidative stress. Toxicology and Applied Pharmacology. 1991;110(2):347–354. doi: 10.1016/s0041-008x(05)80017-1. [DOI] [PubMed] [Google Scholar]
- 36.Sato M, Bremner I. Oxygen free radicals and metallothionein. Free Radical Biology and Medicine. 1993;14(3):325–337. doi: 10.1016/0891-5849(93)90029-t. [DOI] [PubMed] [Google Scholar]
- 37.Takano H, Satoh M, Shimada A, Sagai M, Yoshikawa T, Tohyama C. Cytoprotection by metallothionein against gastroduodenal mucosal injury caused by ethanol in mice. Laboratory Investigation. 2000;80(3):371–377. doi: 10.1038/labinvest.3780041. [DOI] [PubMed] [Google Scholar]
- 38.Waelput W, Broekaert D, Vandekerckhove J, Brouckaert P, Tavernier J, Libert C. A mediator role for metallothionein in tumor necrosis factor-induced lethal shock. Journal of Experimental Medicine. 2001;194(11):1617–1624. doi: 10.1084/jem.194.11.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De SK, McMaster MT, Andrews GK. Endotoxin induction of murine metallothionein gene expression. The Journal of Biological Chemistry. 1990;265(25):15267–15274. [PubMed] [Google Scholar]
- 40.Sato M, Sasaki M, Hojo H. Tissue specific induction of metallothionein synthesis by tumor necrosis factor-α . Research Communications in Chemical Pathology and Pharmacology. 1992;75(2):159–172. [PubMed] [Google Scholar]
- 41.Kimura T, Itoh N, Takehara M, et al. Sensitivity of metallothionein-null mice to LPS/D-galactosamine-induced lethality. Biochemical and Biophysical Research Communications. 2001;280(1):358–362. doi: 10.1006/bbrc.2000.4085. [DOI] [PubMed] [Google Scholar]
- 42.Hur T, Squibb K, Cosma G, et al. Induction of metallothionein and heme oxygenase in rats after inhalation of endotoxin. Journal of Toxicology and Environmental Health. Part A. 1999;56(3):183–203. doi: 10.1080/009841099158141. [DOI] [PubMed] [Google Scholar]
- 43.Brigham KL, Meyrick B. Endotoxin and lung injury. American Review of Respiratory Disease. 1986;133(5):913–927. [PubMed] [Google Scholar]
- 44.Takano H, Inoue K-I, Yanagisawa R, et al. Protective role of metallothionein in acute lung injury induced by bacterial endotoxin. Thorax. 2004;59(12):1057–1062. doi: 10.1136/thx.2004.024232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Inoue K-I, Takano H, Shimada A, et al. Role of metallothionein in coagulatory disturbance and systemic inflammation induced by lipopolysaccharide in mice. The FASEB Journal. 2006;20(3):533–535. doi: 10.1096/fj.05-3864fje. [DOI] [PubMed] [Google Scholar]
- 46.Dasari P, Nicholson IC, Zola H. Toll-like receptors. Journal of Biological Regulators and Homeostatic Agents. 2008;22(1):17–26. [PubMed] [Google Scholar]
- 47.Martinon F, Gaide O, Pétrilli V, Mayor A, Tschopp J. NALP inflammasomes: a central role in innate immunity. Seminars in Immunopathology. 2007;29(3):213–229. doi: 10.1007/s00281-007-0079-y. [DOI] [PubMed] [Google Scholar]
- 48.Katsanos GS, Anogianaki A, Castellani ML, et al. Biology of neurotensin: revisited study. International Journal of Immunopathology and Pharmacology. 2008;21(2):255–259. doi: 10.1177/039463200802100201. [DOI] [PubMed] [Google Scholar]
- 49.Galliera E, Locati M, Mantovani A, Corsi MM. Chemokines and bone remodeling. International Journal of Immunopathology and Pharmacology. 2008;21(3):485–491. doi: 10.1177/039463200802100301. [DOI] [PubMed] [Google Scholar]
- 50.Busse WW, Lemanske RF., Jr. Asthma. The New England Journal of Medicine. 2001;344(5):350–362. doi: 10.1056/NEJM200102013440507. [DOI] [PubMed] [Google Scholar]
- 51.Bradley BL, Azzawi M, Jacobson M, et al. Eosinophils, T-lymphocytes, mast cells, neutrophils, and macrophages in bronchial biopsy specimens from atopic subjects with asthma: comparison with biopsy specimens from atopic subjects without asthma and normal control subjects and relationship to bronchial hyperresponsiveness. Journal of Allergy and Clinical Immunology. 1991;88(4):661–674. doi: 10.1016/0091-6749(91)90160-p. [DOI] [PubMed] [Google Scholar]
- 52.Gibson PG, Simpson JL, Saltos N. Heterogeneity of airway inflammation in persistent asthma: evidence of neutrophilic inflammation and increased sputum interleukin-8. Chest. 2001;119(5):1329–1336. doi: 10.1378/chest.119.5.1329. [DOI] [PubMed] [Google Scholar]
- 53.Inoue K-I, Takano H, Yanagisawa R, et al. Role of metallothionein in antigen-related airway inflammation. Experimental Biology and Medicine. 2005;230(1):75–81. doi: 10.1177/153537020523000110. [DOI] [PubMed] [Google Scholar]
- 54.Johnston RA, Mizgerd JP, Shore SA. CXCR2 is essential for maximal neutrophil recruitment and methacholine responsiveness after ozone exposure. American Journal of Physiology. 2005;288(1):L61–L67. doi: 10.1152/ajplung.00101.2004. [DOI] [PubMed] [Google Scholar]
- 55.Pryor WA. Mechanisms of radical formation from reactions of ozone with target molecules in the lung. Free Radical Biology and Medicine. 1994;17(5):451–465. doi: 10.1016/0891-5849(94)90172-4. [DOI] [PubMed] [Google Scholar]
- 56.Ballinger CA, Cueto R, Squadrito G, et al. Antioxidant-mediated augmentation of ozone-induced membrane oxidation. Free Radical Biology and Medicine. 2005;38(4):515–526. doi: 10.1016/j.freeradbiomed.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 57.Mudway IS, Kelly FJ. Ozone and the lung: a sensitive issue. Molecular Aspects of Medicine. 2000;21(1-2):1–48. doi: 10.1016/s0098-2997(00)00003-0. [DOI] [PubMed] [Google Scholar]
- 58.Samet JM, Hatch GE, Horstman D, et al. Effect of antioxidant supplementation on ozone-induced lung injury in human subjects. American Journal of Respiratory and Critical Care Medicine. 2001;164(5):819–825. doi: 10.1164/ajrccm.164.5.2008003. [DOI] [PubMed] [Google Scholar]
- 59.Ghio AJ, Turi JL, Madden MC, et al. Lung injury after ozone exposure is iron dependent. American Journal of Physiology. 2007;292(1):L134–L143. doi: 10.1152/ajplung.00534.2005. [DOI] [PubMed] [Google Scholar]
- 60.Grimes HD, Perkins KK, Boss WF. Ozone degrades into hydroxyl radical under physiological conditions. A spin trapping study. Plant Physiology. 1983;72(4):1016–1020. doi: 10.1104/pp.72.4.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Byvoet P, Balis JU, Shelley SA, Montgomery MR, Barber MJ. Detection of hydroxyl radicals upon interaction of ozone with aqueous media or extracellular surfactant: the role of trace iron. Archives of Biochemistry and Biophysics. 1995;319(2):464–469. doi: 10.1006/abbi.1995.1318. [DOI] [PubMed] [Google Scholar]
- 62.Johnston CJ, Oberdörster G, Finkelstein JN. Recovery from oxidant-mediated lung injury: response of metallothionein, MIP-2, and MCP-1 to nitrogen dioxide, oxygen, and ozone exposures. Inhalation Toxicology. 2001;13(8):689–702. doi: 10.1080/08958370126867. [DOI] [PubMed] [Google Scholar]
- 63.Johnston CJ, Reed CK, Avissar NE, Gelein R, Finkelstein JN. Antioxidant and inflammatory response after acute nitrogen dioxide and ozone exposures in C57Bl/6 mice. Inhalation Toxicology. 2000;12(3):187–203. doi: 10.1080/089583700196239. [DOI] [PubMed] [Google Scholar]
- 64.Zimmermann A. Regulation of liver regeneration. Nephrology Dialysis Transplantation. 2004;19(supplement 4):iv6–iv10. doi: 10.1093/ndt/gfh1034. [DOI] [PubMed] [Google Scholar]
- 65.Fausto N. Liver regeneration. Journal of Hepatology. 2000;32(1) supplement 1:19–31. doi: 10.1016/s0168-8278(00)80412-2. [DOI] [PubMed] [Google Scholar]
- 66.Koniaris LG, McKillop IH, Schwartz SI, Zimmers TA. Liver regeneration. Journal of the American College of Surgeons. 2003;197(4):634–659. doi: 10.1016/S1072-7515(03)00374-0. [DOI] [PubMed] [Google Scholar]
- 67.Tohyama C, Suzuki JS, Hemelraad J, Nishimura N, Nishimura H. Induction of metallothionein and its localization in the nucleus of rat hepatocytes after partial hepatectomy. Hepatology. 1993;18(5):1193–1201. [PubMed] [Google Scholar]
- 68.Mehendale HM. Tissue repair: an important determinant of final outcome of toxicant-induced injury. Toxicologic Pathology. 2005;33(1):41–51. doi: 10.1080/01926230590881808. [DOI] [PubMed] [Google Scholar]
- 69.Klaassen CD, Liu J, Choudhuri S. Metallothionein: an intracellular protein to protect against cadmium toxicity. Annual Review of Pharmacology and Toxicology. 1999;39:267–294. doi: 10.1146/annurev.pharmtox.39.1.267. [DOI] [PubMed] [Google Scholar]
- 70.Diaz-Buxo JA, Blumenthal S, Hayes D, Gores P, Gordon B. Galactosamine-induced fulminant hepatic necrosis in unanesthetized canines. Hepatology. 1997;25(4):950–957. doi: 10.1002/hep.510250427. [DOI] [PubMed] [Google Scholar]
- 71.Inoue K-I, Takano H, Satoh M. Protective role of metallothionein in coagulatory disturbance accompanied by acute liver injury induced by LPS/D-GalN. Thrombosis and Haemostasis. 2008;99(5):980–983. doi: 10.1160/TH07-10-0637. [DOI] [PubMed] [Google Scholar]