Abstract
The aim of this study was to explore the information flow of hospice interdisciplinary meetings focusing on information access, exchange and documentation. The study participants were members of four hospice interdisciplinary teams in the Midwestern United States. Team members included a diverse range of professionals including physicians, nurses, social workers, bereavement counselors, and others. A total of 81 patient care discussions were videotaped and transcribed. A content analysis revealed several themes that needed to be addressed to improve the overall information flow, such as access to and recording of information, documentation of services, obtaining information from absent team members, data redundancy and updating of recorded information. On average, 5% of all utterances when discussing a patient case were focused on soliciting information from the member who had access to the patient chart. In 12.3% of all discussions, members referred to an absent member who could have provided additional information. In 8.6% of all discussions the same facts were repeated three times or more. Based on the findings we propose guidelines that can address potential informational gaps and enhance team communication in hospice.
Keywords: Hospice, interdisciplinary team, communication, information flow
Introduction
Interdisciplinary collaboration and teamwork are essential components of efficient health care services. In hospice care, team meetings are not only desirable for the delivery of services, but also required by law in the US. The Medicare Hospice Benefit introduced in 1983 provides specific federal guidelines that require hospice agencies to adopt an interdisciplinary approach to patient care. It is required that patients' care be overseen and managed by an interdisciplinary group consisting at least of a physician, nurse, social worker, and counselor (Hoyer, 1998). A holistic approach for interdisciplinary teams (IDTs) allows experts in different disciplines to evaluate and provide feedback to the care plan, and ensures comprehensive care. Such an approach has been found to reduce overall health care costs (Dyeson, 2005), and increase client satisfaction (Reese & Raymer, 2004). The US federal mandate requires hospice agencies to facilitate IDT meetings that provide a platform for team members to share responsibilities and design their assigned tasks (Sabur, 2003), review and modify the care plan, if necessary, and oversee the coordination and provision of hospice services.
Research on patient care teams suggests that teams with greater cohesiveness and improved communication are associated with better clinical outcome measures and higher levels of patient satisfaction (Grumbach & Bodenheimer, 2004). In order for the interdisciplinary approach to achieve its potential, team meetings need to maximize their efficiency pertaining to information access and exchange among members as well as accurately document their actions and decisions. As Larson and LaFasto (1989) point out, a team needs to utilize an effective communication system with the following four features: focus on accessible information; utilization of information from credible sources; opportunities for informal communication; and documentation of decisions in planning for communication. In order to improve the structure and process of team meetings, interactions among team members need to be studied and potential challenges or deficiencies need to be identified.
The aim of this study is to explore the information flow of hospice IDT meetings focusing on information access, exchange and documentation. Furthermore, we aim to identify guidelines or tools that can address potential informational gaps and enhance team communication in hospice.
Methods
In order to gain an understanding of information flow during hospice IDT meetings, we studied actual meetings. The study participants were members of four hospice interdisciplinary teams in the Midwestern United States. Team members included a diverse range of hospice care providers including physicians, nurses, social workers, bereavement counselors, chaplains, volunteer coordinators and home health aides. IDT meetings were videotaped for patients who had consented to participate in a larger intervention study. Because not all hospice patients had consented to participate, the entire meeting was not taped. Video-recordings consisted of the team's discussion of the patient's plan of care for patients who had previously consented to participate. When the team was about to start discussing a consenting patient, a graduate research assistant (GRA) would initiate the video-recording of the session. The study was approved by the University of Missouri Institutional Review Board (IRB) and the appropriate boards of the participating hospice agencies. Videotapes of the recorded sessions were transcribed and a content analysis was performed.
A content analysis can be either theory driven, data driven or follow a hybrid approach (Boyatzis, 1998). For this study we followed a data driven approach to determine the informational needs of IDT members during these meetings and the overall information flow (including information access, exchange and documentation). Figure 1 highlights the components of information flow under study based on an expansion of the team communication features described by Larson and LaFasto (1989). Using constant comparative analysis, we analyzed the data in multiple levels: the individual text line (open coding), the clustering of ideas (axial coding) and the pulling together of the concept or theory (selective coding) (Boyatzis, 1998). For the open coding the “utterance” (e.g., a simple sentence, an independent clause, nonrestrictive dependent clause, multiple predicate) served as the unit of analysis. A list of major thematic elements was extracted by thorough study and coding of the transcripts. The analysis was organized into an expanding list of themes. Analysis and coding was conducted by two members of the research team (GD, KW); in cases of discrepancies in the coding, these were discussed until consensus was reached. Finally, a member of the research team (KW) viewed the actual videotapes of the meetings and took notes to gain additional insight into the team dynamics and processes.
Figure 1.
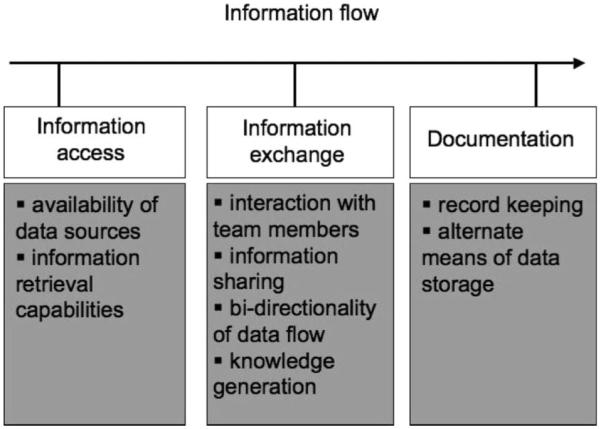
Dimensions of information flow.
Results
In a period of five months (from December 2006 to April 2007) a total of 81 patient care discussions on 24 patients were videotaped and transcribed. The following themes referring to information flow during the team meetings were identified:
Access to information
This reflects on the participants' need to access the same baseline information during the meeting. Only one patient chart was available during these sessions, making it challenging for multiple team members to consult the chart while discussing a case. On average, 5% of all utterances when discussing a patient case were focused on soliciting information from the member who had access to the patient chart. Example:
Nurse (RN): She is … Can you pull that sheet out and look at the chart?
Medical Director (MD): She's eighty-one with lung cancer
Recording of information
This issue highlights the challenge that often occurred in identifying a record keeper for the team meetings as this was not always determined prior to the meeting. Furthermore, in some instances team members were missing information discussed in previous meetings. Example:
RN: Well her brother is visiting but he apparently can't stay for very long. It's too much for him, (caregiver name) goes and stays with her as long as she can in the morning ….
Social Worker (SW): Who is writing on her?
RN: Well I have her chart but I've been too busy expounding on her to write anything down.
Documentation of delivered services
The transcripts often revealed a lack of readily available information about team members who were scheduled to visit the patient or had conducted prior visits. Example:
Bereavement Coordinator (BR): And I know that (name) sees her too (calls the SW to get her attention) - does (name) see her too?
SW: Yes, ah yeah I think she has been I don't know whether (name) has seen her or not.
BR (to Chaplain CHP): If you haven't you probably will …
Obtaining information from absent staff
An update on delivered services or details on the patient's status were in some cases not available as on-call staff members who could have provided this information, were not present at the meeting. In 10 out of 81 case discussions (12.3%), members referred to an absent member who could have provided additional information. Example:
CHP: Yea, I think it was (Name of RN), and uh, once you admitted him then (Name) took over and our nurse was up there last night, and he was having so much trouble breathing … I think. (Name) started the IV. Um, and he had gotten two liters and I think what (Name of RN) did was, I mean the man was having so much difficulty and so tight that he called (Name of RN) to talk with him and I think what it all boiled down to, the way (Name of RN) left it, was that the patient finally refused any more IV fluid … so … I don't know, I think (Name of RN) said he turned him and moved him and some things
Data redundancy-retelling
Several segments of the team meetings were spent repeating information previously discussed. The reporting of information was repeated not only from week to week but in some cases within the same team meeting. In seven out of the 81 discussions (8.6%) the same facts were repeated three times or more within the same discussion. Example:
RN1: (patient name) remains at (facility name), and I know at one point we talked about taking him off but we kept him on
MD: just because his disease was progressing so slowly?
CHP: Where is he located?
RN1: (facility name)
DR: so he only uses oxygen for his shortness of breath?
RN2: he uses it all of the time, yes, very diminished lungs (several minutes later)
RN1: I think that he is oxygen dependent, I think he's not driving anymore, people are driving him if he needs to go anywhere.
SW: Where is he at?
RN1: (facility name)
Volunteer Coordinator (VOL): Majority oxygen dependent, 5 liters
SW: does that go up?
MD: Its 5 liters here, increased with exertion
RN1: he increases it with exertion
SW: So he is oxygen dependent?
Update of recorded information
This challenge pertained specifically to medication orders. The transcripts clearly demonstrate the challenge that team members often face in determining what the current medication orders are, when and who ordered them, and what the dosage is. Example:
SW (to RN): Is she supposed to get more meds?
RN (to SW): hmm?
SW (to RN): She's supposed to get more meds?
RN: Uh, I'm sure she is, she's supposed to have `em daily, like some of (drug name) and some of those she's suppose to have them daily.
VOL (to RN): So doesn't get up until—
RN (to VOL): —til she get's up, … …
RN: Anyway so, we changed the (drug name 1), the time released (drug name 1) to the (drug name 2) Patch, right? And we are getting the (drug name 3) for the breakthrough pain
VOL (to RN): And you changed the (drug name 2) to (drug name 1)
RN (to VOL): The (drug name 1) to the (drug name 2).
RN: And then she also was on (drug name 3) and the doctor changed that to (drug name 4) which is a concentrate, it's 20 milligrams per ml and I'd have to look at the order, I think was going to be like half a ml to a ml like every 4 hours, I think …
The observation of the videotapes revealed that in some cases team membership varied during the meeting (i.e., members left early or attended late).
Discussion
Findings indicate that the current information flow during team meetings bears some challenges that may potentially be decreasing the overall effectiveness of these meetings. As Larson and LaFasto (1989) argue, the potential for collective problem-solving is often unrealized and the promise of collective achievement is often not addressed. This challenge is clearly demonstrated in the hospice field as documented by our findings. For example, the retelling of the same facts or questions resulting from lack of access to the patient charts could lead to an increase of the team meeting duration and decrease of overall productivity. Furthermore, documentation gaps can affect decision making when decisions are based on inaccurate, incomplete or out-dated information or solely on recollection of events rather than detailed and up-to-date records. Finally, gaps in the information flow of the team meetings can potentially lead to a lack of coordination for the scheduled services, as members may have different levels of access to information sources or may not all be present during the decision making process.
Based on the deficiencies and gaps identified in this analysis, we propose a set of guidelines to improve information flow in hospice team meetings:
The efficiency of team meetings can be increased if a leader or facilitator is defined who plans the structure and procedures of the meetings (Whetton & Cameron, 1995). Such planning can ensure that all members have access to the required information and that meetings are scheduled to include all relevant stakeholders (to address the challenge of requiring feedback from absent members). A leader or facilitator can also address conflict and misperceptions. Research on satisfaction levels of interdisciplinary team members in hospice care reveal that within one team there can be significant differences in satisfaction among team members (Monroe & DeLoach, 2004). Common problems in IDT meetings include interpersonal conflicts and “turfdom” wherein team members become protective of their discipline and their contributions based on their expertise (Larson, 2003). In this context, challenges arise when team members concentrate on their personal goals rather than the team's goals (Reese & Sontag, 2001). A leader or facilitator can address such challenges by ensuring that the discussion is balanced allowing for all team members to actively participate and ensure that no one member or discipline dominates the meeting and the decision making process. A facilitator can also address conflict and implement techniques to proactively address issues that may impede information flow.
The study findings highlight the importance of ensuring access to patient charts for all team members during the team meeting. This can be accomplished with several tools ranging from simple solutions (such as basic information sheets as handouts or a projector that displays a summary of the patient chart visible to all team members) to more sophisticated solutions (laptops or Personal Digital Assistants-PDAs for all members that enable access to an electronic medical record for patients). Visual aids are important foundations for a successful meeting (Whetton & Cameron, 1995).
Patient care discussions require structured documentation. Documentation needs to become a priority for the team leader or facilitator and the responsibility for an individual identified before the meeting begins. An electronic information system can obviously also address broader issues of documentation. Our findings highlight potential barriers to accurate and complete documentation resulting in some cases from lack of process structure (e.g., it is not clear who is taking notes and how much information to record) or failure to integrate notes from previous meetings into the patient record. The assignment of the record keeping role prior to each meeting and the oversight of the inclusion of meeting notes into the patient record can also reduce the data redundancy during the IDT meetings where the same information is being repeated several times.
Information technology can be utilized to include members who cannot be physically present during the team meetings. Such tools can include regular phones or videophones if there is need for visual feedback, or even web-based platforms for communication. There are several technology related theoretical models that address how information technology affects group processes. Media richness theory, for example, is concerned with questions of media choice (i.e., when to use what medium effectively) during a group process. This theory (Daft & Lengel, 1986) argues that the amount of information communicated differs with respect to a medium's richness. The underlying premise is that resolving ambiguity and reducing uncertainty are the main goals of communication. Not all media are capable of resolving uncertainty and ambiguity during a group process and the richness of the media should be matched to the task at hand to prevent over-simplification or added complication. Other theories such as social presence are concerned with the consequences of media choices in a group process. Social presence theory (Short et al., 1976), focusing primarily on telephony and telephone conferencing, argues that the social impact of a communication medium depends on the social presence it allows the communicators to have. Social presence relates to the degree of acoustic, visual, and physical contact that the medium permits. According to this theory, text-based forms of interaction (e-mail, instant messaging) are less social, and therefore less conducive to social influence than audiovisual media or face-to-face interactions in group processes. Selecting the appropriate information technology application includes consideration of the team structure, dynamics, training and experience and alternative communication platforms. Technology can become a powerful tool if introduced to address the end users' needs and not to disrupt but rather enhance the social and product function of a group process. The domain of hospice care as an application field for IT remains largely unexplored.
The design and structure of teams must be dynamic, namely open for ongoing evaluation and revision, if necessary. The structure and underlying model for team meetings need to adjust to potential changes in the patient needs, the health care system and policy and the expertise of team members. Furthermore, team members should explore the selection of tools and techniques to enhance communication and information flow.
The design of the meeting space can impact the effectiveness of the team. Research has shown that space allotment in the practice site influences productivity, work attitudes, and perceptions of confidentiality (Lindeke et al., 1998). Facility design has the potential to improve collaboration when the infrastructure enhances formal and informal interactions. Our tapes indicate that in many instances teams meet with open doors and participants have trouble hearing due to noise from the outside or lower their voice when they discuss sensitive information. Members who come late to the meetings sometimes stand as there is no seating available or bring a chair from another room which can disturb the team process. Efforts to improve the meeting space should address issues of convenience, seating space, privacy and noise control.
Our findings demonstrate that there is no patient and family involvement in the IDT meetings. Practical constraints such as geographic distance, time conflicts and the frailty of the patient often prohibit patients and their informal caregivers to be physically present during these meetings. However, the family focus of hospice philosophy requires IDT meetings to be designed as to include the patient and the family (Connor et al., 2002). The inclusion of patients and their families in IDT meetings is expected to improve patient and caregiver satisfaction, communication and coordination of care (Vuokila-Oikkonen et al., 2002), and access to specialists (Axford et al., 2002; Andrews et al., 1998). Thus, many researchers, practitioners and policy makers are calling for an increase of the involvement of patients and family members in IDT activities (Macdonald et al., 2002; Saltz & Schaefer, 1996). Once again, technology can address some of the practical barriers allowing for a “virtual” participation of patients and family members in IDT meetings (whether via regular telephony that facilitates a phone conference or videoconferencing software and hardware that allows for audiovisual feedback). Such an application could also allow other health care providers to participate in the meeting such as nursing home staff members, physician office staff and pharmacists. In that case, technology does not only enhance communication but introduces new stakeholders into the team and affects the team dynamics.
In addition to specific tools that can be applied during the IDT meetings, there are obviously overall structural characteristics resulting from the organizational nature of a hospice agency that contribute to the development and maintenance of interdisciplinary teams. Bronstein (2003) argues that these items include manageable caseloads, an organizational culture that supports and encourages interdisciplinary collaboration, professional autonomy, administrative support, and the time and space for collaboration to occur. Organizational elements that contribute to poor group performance include lack of coordination, poorly defined member roles and responsibilities, and poor or no leadership (Hirokawa et al., 2000).
Conclusion
The findings indicate that the effectiveness of interdisciplinary teams requires a platform and an appropriate infrastructure to support the information exchange among team members, knowledge sharing and the documentation of the team's interactions and decisions. A holistic care model is based on solicitation of input from and dissemination of information to a diverse group of professionals. Teamwork requires a detailed communications strategy that establishes effective channels of information flow and sharing. Information technology tools can assist the documentation process and information retrieval both during and in-between team meetings. Hospice care depends on the success of interdisciplinary teamwork as it aims to provide comprehensive care that will enhance quality of life and dignity for patients at the end of life. Multiprofessional teams in hospice have to cultivate clear and concise communication within the group. Ensuring accurate flow of information between various disciplines requires structured documentation and ubiquitous accessibility of the patient record. The proposed guidelines are applicable to health care systems worldwide and aim to enhance the structure and performance of teams regardless of the specific policies or administrative processes that vary from one setting to another.
This study demonstrates that the improvement of interprofessional communication requires a careful analysis of the interactions among hospice team members and identification of possible barriers to information flow.
Acknowledgement
This project was funded by the National Institutes of Health (NIH) National Cancer Institute R21 CA 120179: Patient and Family Participation in Hospice Interdisciplinary Teams.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Andrews J, Seaver E, Whiteley J, Stevens G. Family members as participants on craniofacial teams. Infant-Toddler Intervention: The Transdisciplinary Journal. 1998;8:127–134. [Google Scholar]
- Axford AT, Askill C, Jones AJ. Virtual multidisciplinary teams for cancer care. Journal of Telemedicine & Telecare. 2002;8:3–4. doi: 10.1177/1357633X020080S202. [DOI] [PubMed] [Google Scholar]
- Boyatzis RE. Sage Publications; Thousand Oaks, CA: 1998. Transforming qualitative information: Thematic analysis and code development. [Google Scholar]
- Bronstein LR. A model for interdisciplinary collaboration. Social Work. 2003;48(3):297–306. doi: 10.1093/sw/48.3.297. [DOI] [PubMed] [Google Scholar]
- Connor SR, Egan KA, Kwilosz DM, Larson DG, Reese DJ. Interdisciplinary approaches to assisting with end-of-life care and decision making. American Behavioral Scientist. 2002;46:340–356. [Google Scholar]
- Daft RL, Lengel RH. Organizational information requirements, media richness and structural design. Management Science. 1986;32(5):554–571. [Google Scholar]
- Dyeson TB. The home health care team: What can we learn from the hospice experience? Home Health Care Management & Practice. 2005;17:125–127. [Google Scholar]
- Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? Journal of the American Medical Association. 2004;291:1246–1251. doi: 10.1001/jama.291.10.1246. [DOI] [PubMed] [Google Scholar]
- Hirokawa RY, DeGooyer D, Valde K. Using narratives to study task group effectiveness. Small Group Research. 2000;31(5):573–592. [Google Scholar]
- Hoyer T. A history of the Medicare Hospice Benefit. The Hospice Journal. 1998;13:61–69. doi: 10.1080/0742-969x.1998.11882888. [DOI] [PubMed] [Google Scholar]
- Larson CE, LaFasto FM. Team work: What must go right/what can go wrong. Sage Publications; Newbury Park: 1989. [Google Scholar]
- Larson D. Exploring the nature of the interdisciplinary team: An excerpt from The Helper's Journey. Hospice Palliative Insights. 2003;4:6–8. [Google Scholar]
- Lindecke L, Hauck M, Tanner M. Creating spaces that enhance nurse practitioner practice. Journal of Pediatric Health Care. 1998;12(3):125–129. doi: 10.1016/s0891-5245(98)90242-5. [DOI] [PubMed] [Google Scholar]
- Macdonald E, Herrman H, Hinds P, Crowe J, McDonald P. Beyond interdisciplinary boundaries: Views of consumers, carers and non-government organisations on teamwork. Australasian Psychiatry. 2002;10:125–129. [Google Scholar]
- Monroe J, DeLoach RJ. Job satisfaction: How do social workers fare with other interdisciplinary team members in hospice settings? Omega. 2004;49:327–346. [Google Scholar]
- Reese DJ, Raymer TB. Relationships between social work involvement and hospice outcomes: Results of the National Hospice Social Work Survey. Social Work. 2004;49:415–422. doi: 10.1093/sw/49.3.415. [DOI] [PubMed] [Google Scholar]
- Reese DJ, Sontag M. Successful interprofessional collaboration on the hospice team. Health & Social Work. 2001;26:167–175. doi: 10.1093/hsw/26.3.167. [DOI] [PubMed] [Google Scholar]
- Sabur S. Measuring the success of the interdisciplinary team. Hospice Palliative Insights. 2003;4:47–49. [Google Scholar]
- Saltz CC, Schaefer T. Interdisciplinary teams in health care: Integration of family caregivers. Social Work in Health Care. 1996;22:59–69. doi: 10.1300/J010v22n03_04. [DOI] [PubMed] [Google Scholar]
- Short JA, Williams E, Christie B. The social psychology of telecommunications. John Wiley & Sons; New York, NY: 1976. [Google Scholar]
- Vuokila-Oikkonen P, Janhonen S, Nikkonen M. Patient initiatives in psychiatric care concerning shame in the discussion in co-operative team meetings. Journal of Psychiatric & Mental Health Nursing. 2002;9:23–32. doi: 10.1046/j.1365-2850.2002.00406.x. [DOI] [PubMed] [Google Scholar]
- Whetton D, Cameron C. Developing management skills. Scott, Foresman; Glenview, IL: 1995. Principles for managing meetings. [Google Scholar]


