In this volume, France, et al. [5] report reduced pain response in neonates with a maternal family history of hypertension. Their results add a radical new twist to the mysterious link between hypoalgesia and blood pressure dysregulation in the early stages of hypertension. France, et al. [5] suggest that maternal transmission of hypertension-associated hypoalgesia could result from mitochondrial DNA. However, there is a compelling need to also consider environmental mechanisms of maternal transmission, especially the effects of prenatal maternal stress hormones on fetal neurodevelopment.
The prenatal intrauterine environment is a rich and dynamic milieu that can influence development of complex fetal regulatory systems, including the mechanisms that control blood pressure and responses to pain. Citing the correlation of birth weight with subsequent adult blood pressure, Barker [2] hypothesizes that reduced availability of nutrients during fetal development causes relatively permanent changes in renal function. However, the action of maternal stress hormones suggests an additional link between maternal risk for hypertension and neonatal pain response.
Growing evidence suggests that maternal stress hormones can affect the developing fetus in ways that could promote vulnerability to chronic disease. For example, young adult men and women at risk for hypertension have reduced pain sensitivity and exaggerated blood pressure reactivity during psychological stress [6]. Exaggerated blood pressure reactivity appears to result from diminished central opioidergic inhibition of the sympathoadrenomedullary and hypothalamic-pituitary-adrenocortical axes [9]. This produces periodic abnormal elevations in plasma levels of epinephrine, norepinephrine and cortisol in persons at risk for hypertension [1,9]. The associated hypoalgesia is complex and probably involves both opioid and non-opioid pathways [4,6]. During pregnancy, the neuroendocrine profile of women at risk for hypertension may have direct consequences on the developing fetal nervous system.
Studies of stress during pregnancy support links between maternal blood pressure reactivity and fetal development. For example, we found that increased maternal blood pressure response to stress during pregnancy predicts subsequent birth outcome, including reduced birth weight, gestational age, and rate of fetal weight gain [7]. Reduced rate of fetal weight gain indicates an influence on fetal development, not simply early onset of labor. Thus maternal blood pressure control mechanisms can have a profound influence on the developing fetus.
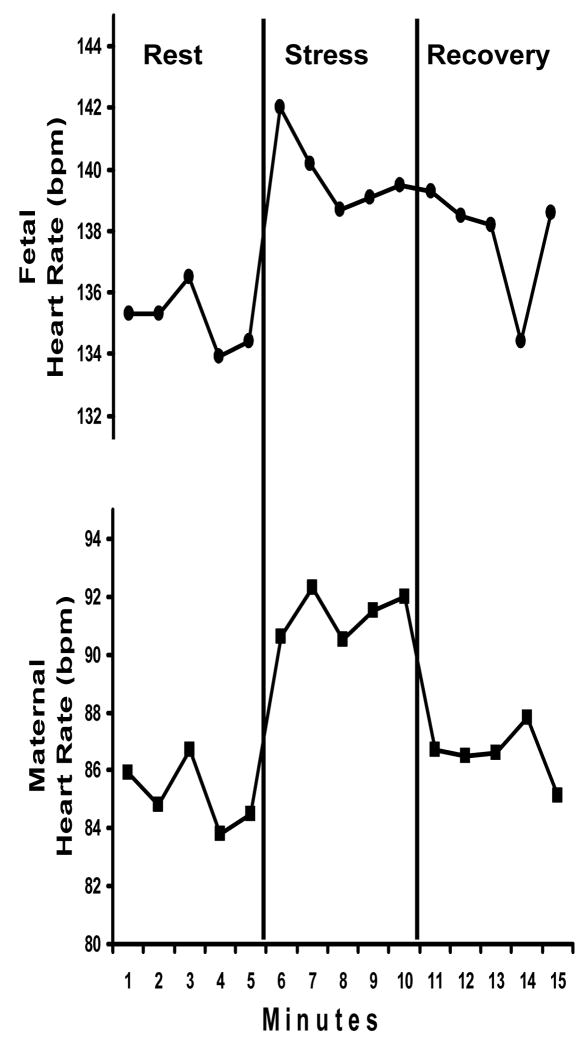
Maternal blood and fetal blood does not mix directly, but the exchange of oxygen, nutrients and other molecules including hormones, occurs through the placenta. Thus the fetal circulation reflects the permeability of the placenta to stress hormones in maternal blood. As a striking example of this maternal/fetal pathway, we observed that both maternal heart rate and fetal heart rate increase during maternal stress in 20 third trimester primigravidae [8]. Figure 1 shows simultaneous minute by minute changes in fetal and maternal heart rates before, during and after maternal performance on a stressful arithmetic challenge. The fetal tachycardia during maternal stress indicates a direct consequence of maternal stress reactions on fetal tissue and systems.
Figure 1.
The effect of maternal stress on fetal heart rate. Simultaneous minute by minute changes in fetal heart rate and maternal heart rate (bpm) before, during and after maternal performance on a stressful mental arithmetic challenge.
Therefore, a feasible link between maternal family history of hypertension and neonatal hypoalgesia is found the neuroendocrine cascade evoked during psychological stress in mothers at risk for development of hypertension. Animal models suggest that maternal stress can alter adrenocortical function in the offspring [3]. We do not yet know the precise impact of maternal stress hormones on neuroplasticity, but bathing the developing fetal nervous system in stress hormones of maternal origin could program pervasive neurodevelopmental remodeling. The resulting neuroendocrine changes could alter the sensitivity of stress pathways, pain control mechanisms and ultimately, blood pressure control systems.
France, et al. [5] raise the possibility of maternal genotypic transmission of hypertension-associated hypoalgesia, but do not elaborate on potential environmental explanations. Selective transmission could occur through maternal nutrition, toxins or colostral opioids in breast milk [10]. However, I believe these data inspire a different hypothesis: Maternal stress hormones influence fetal neurodevelopment, neonatal pain response and ultimately, risk for hypertension in the offspring.
Acknowledgments
The author has no conflict of interest related to this editorial.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.al’Absi M, Wittmers LE. Enhanced adrenocortical responses to stress in hypertension-prone men and women. Ann Behav Med. 2003;25:25–33. doi: 10.1207/S15324796ABM2501_04. [DOI] [PubMed] [Google Scholar]
- 2.Barker DJP. Birth Weight and Hypertension. Hypertension. 2006;48:357–358. doi: 10.1161/01.HYP.0000236552.04251.42. [DOI] [PubMed] [Google Scholar]
- 3.Emack J, Kostaki A, Walker CD, Matthews SG. Chronic maternal stress affects growth, behaviour and hypothalamo-pituitary-adrenal function in juvenile offspring. Horm Behav. 2008;54(4):514–20. doi: 10.1016/j.yhbeh.2008.02.025. [DOI] [PubMed] [Google Scholar]
- 4.France CR. Hypoalgesia and risk for hypertension. Psychophysiol. 1999;36:683–692. [PubMed] [Google Scholar]
- 5.France CR. Maternal family history of hypertension attenuates neonatal pain response. Pain. doi: 10.1016/j.pain.2008.12.010. in press. [DOI] [PubMed] [Google Scholar]
- 6.McCubbin JA, Helfer SG, Switzer FS, Galloway C, Griffith WV. Opioids analgesia in persons at risk for hypertension. Psychosom Med. 2006;68(1):116–120. doi: 10.1097/01.psy.0000195742.24850.79. [DOI] [PubMed] [Google Scholar]
- 7.McCubbin JA, Lawson EJ, Cox S, Sherman JJ, Norton JA, Read JA. Prenatal maternal blood pressure response to stress predicts birth weight and gestational age: A preliminary study. Am J Obstet Gynecol. 1996;175(3):706–712. doi: 10.1053/ob.1996.v175.a74286. [DOI] [PubMed] [Google Scholar]
- 8.McCubbin JA, Lawson EJ, Sherman JJ, Norton JA. Fetal heart rate and transplacental stress reactivity: A new paradigm for psychophysiology. Psychophysiol. 1996;33(Suppl 1):S60–S60. [Google Scholar]
- 9.McCubbin JA, Surwit RS, Williams RB, Nemeroff CB, McNeilly M. Altered pituitary hormone response to naloxone in hypertension development. Hypertension. 1989;14:636–44. doi: 10.1161/01.hyp.14.6.636. [DOI] [PubMed] [Google Scholar]
- 10.Zanardo V, Nicoluss S, Carlo G, Marzari F, Faggian D, Favaro F, Plebani M. Beta endorphin concentrations in human milk. J Ped Gastroenterol Nutrit. 2001;33:160–164. doi: 10.1097/00005176-200108000-00012. [DOI] [PubMed] [Google Scholar]