Abstract
Background
Comorbid anxiety symptoms are common in late-life depression (LLD) and predict poorer treatment outcomes. No research has delineated the impact of different dimensions of anxiety (such as worry/anxious apprehension and panic/anxious arousal) on treatment response in LLD. We explored the impact of the dimensions of worry and panic on acute and maintenance treatment outcomes in LLD.
Methods
We measured anxiety symptoms in 170 LLD subjects receiving protocolized treatment. Exploratory principal components analysis was used to delineate dimensions of anxiety symptoms. We defined sub-groups based on factor scores. We used survival analysis to test the association of pre-treatment anxiety dimensions with time to response and time to recurrence of LLD.
Results
The principal component analysis found two factors: “worry” and “panic”. Three sub-groups were defined: low panic-low worry, low panic-high worry, and high panic-high worry. The low panic-high worry and high panic-high worry sub-groups had longer time to response than the low panic-low worry sub-group. Time to recurrence was longer in low panic-low worry subjects randomized to drug. Among subjects with high worry, there was no difference between those with low versus high panic regarding both time to response and time to recurrence of LLD.
Conclusion
High levels of worry were associated with longer time to response and earlier recurrence with pharmacotherapy for LLD. There was no additional effect of panic symptoms on treatment outcomes when accounting for the effects of excessive worry. These results suggest that worry symptoms should be a focus of strategies to improve acute and maintenance treatment response in LLD.
Keywords: depression, anxiety, elderly, worry, panic, treatment response
Introduction
The most common clinical presentation of late-life depression (LLD) includes anxiety symptoms in addition to those of depression (1, 2). Several studies have found that greater severity of anxiety symptoms in LLD is associated with an increased risk of treatment dropout (3, 4), a decreased response to acute antidepressant treatment (3-5), and a longer time to both response (6-8) and remission (9-11). Persistent symptoms of anxiety after the remission of LLD also predict earlier recurrence (12, 13). In a recent controlled maintenance trial of LLD, we reported that baseline anxiety symptoms predict both increased time to remission and decreased time to recurrence (14).
The above analyses treated anxiety as a single variable; however, anxiety is multidimensional, encompassing phenotypically and neurobiologically different facets such as anxious apprehension (or worry) and anxious arousal (with the clinical corollary of panic) (15, 16). One could potentially expect different effects of these dimensions on treatment response. Moreover, generalized anxiety disorder (GAD), characterized by pervasive and uncontrollable worry, tends to be more treatment resistant than panic disorder (PD), characterized by anxious arousal (17). The differential impact of worry and panic on treatment response in LLD is largely unknown at this time. To explore this issue, we conducted a secondary analysis in the group of subjects in which we have previously reported the negative effect of global anxiety symptoms on treatment response in LLD (14). The goal of this study was to explore the impact of different symptomatic dimensions of anxiety on acute and maintenance treatment outcomes in LLD. We hypothesized that, given the increased treatment resistance of GAD compared with PD in the elderly, the apprehension/worry dimension of anxiety would have a more prominent negative impact on acute and maintenance treatment response of LLD than the arousal/panic dimension.
Method
Data for this analysis were provided by the second study of Maintenance Therapies in Late Life Depression (MTLD-II) conducted at the University of Pittsburgh Intervention Research Center for the Study of Late-Life Mood Disorders between 1999 and 2004. Details of the study protocol are described elsewhere (18). In brief, participants were 70 years old and older, with a diagnosis established with the Structured Clinical Interview for DSM-IV (SCID) of non-psychotic, non-bipolar major depressive disorder (single-episode or recurrent) (19), a 17-item Hamilton Depression Rating Scale (HDRS) of 15 or higher (20), and a Mini Mental State Examination (MMSE) score of 17 or higher (21). In the acute treatment phase, patients received open pharmacotherapy and weekly interpersonal psychotherapy (IPT) (22) until they achieved sustained response (defined as a HDRS score of 10 or less for three consecutive weeks). Pharmacotherapy consisted of paroxetine started at 10 mg/day and titrated as necessary up to a maximum of 40 mg/day. Patients who responded to acute treatment entered 16 weeks of continuation treatment to stabilize their response; they received the same pharmacotherapy and IPT every two weeks. Patients who maintained response during continuation treatment were then randomly assigned to one of four maintenance treatments: 1) pharmacotherapy/monthly clinical management visits; 2) placebo/monthly clinical management visits; 3) pharmacotherapy/monthly maintenance IPT; 4) placebo/monthly maintenance IPT. Patients remained in maintenance therapy for two years, or until recurrence of a major depressive episode. Adjudication of recurrence required an HDRS score of ≥15, meeting DSM-IV criteria for a major depressive episode during a SCID interview, and having an independent geriatric psychiatrist confirm the diagnosis. All patients provided written informed consent to a protocol approved by the University of Pittsburgh Institutional Review Board.
Symptoms of anxiety were measured using the anxiety scale from the Brief Symptom Inventory [BSI (23)]. The BSI is a validated self-report scale developed from the SCL-90-R with strong test–retest and internal consistency reliabilities. Factor analytic studies of the internal structure of the scale have demonstrated its construct validity (23). The anxiety subscale consists of six items: nervousness, suddenly scared, feeling fearful, feeling tense, feeling restless, and spells of panic. Each item is rated on a 5-point scale (0 = symptom not present, 4 = extremely severe).
The analysis of acute treatment outcome included 170 subjects who participated in the acute treatment phase and had pre-treatment BSI scores available. Of these, 99 remitted and participated in randomly assigned maintenance treatment and were included in the analysis of maintenance outcome.
Statistical analysis
We observed that the BSI-anxiety scale appeared to have two subscales, with three items measuring anxious apprehension/worry (nervousness, feeling tense, feeling restless) and three items measuring anxious arousal/panic (suddenly scared, feeling fearful, spells of panic). To examine if the factor structure was consistent with our observations we used a principal components analytic method for the exploratory factor analysis with a varimax rotation. This method is similar to the method used by Derogantis and Melisaratos in the original BSI paper (24). Anxiety factor scores were computed using the mean of the items in each of the factors identified by the principal components analysis. We examined the internal consistency of each of the factors obtained and the correlation between the factors.
The factor scores were plotted using a smoothed bivariate density function, and cut-off points were examined to define separate groups based on high and low factor scores. We used Kaplan-Meier survival analysis to assess the effect of pre-treatment high and low factor scores on time to response during acute treatment and time to recurrence during maintenance treatment. We analyzed the difference between baseline core HDRS scores for the three sub-groups (core HDRS = items 1, 2, 3 and 7, representing depressed mood, guilt, suicide, work/activities) (25, 26). We used the core HDRS to avoid confounding effect by the anxiety-related items from the complete HDRS (25).
Due to the small sample and different treatments during maintenance, we used the stratified log-rank test from StatXact (27) to examine the effect of pre-treatment anxiety factors on time-to-recurrence separately for drug groups (paroxetine or placebo). In the previously reported parent study, maintenance IPT was not shown to have an effect on time to recurrence or rates of recurrence of major depressive episodes (18).
The analyses were performed using SAS Proc Factor, version 9.2 (SAS Institute, Cary, NC).
Results
1. Dimensions of anxiety in the BSI anxiety scale
Exploratory principal components analyses of the six BSI items, described in Table 1, defines a two-factor structure. Thus, each item loaded onto only one of the two extracted factors: three items -- nervousness, feeling tense, and feeling restless -- loaded on one factor, representing the construct of worry, and explained 56% of the variance. Three other items --suddenly scared, feeling fearful, and spells of panic -- loaded on another factor, representing the construct of panic, explained 16% of the variance. Internal consistency was good for both factors, with Cronbach's alphas of 0.78 for worry and 0.83 for panic. The Pearson correlation coefficient showed a moderately high correlation between the two factors (r = 0.59, n=166, p<0.0001). These results were consistent with our initial observation regarding the two different dimensions of anxiety nested in the BSI anxiety scale, and supported our strategy to delineate the effects of worry and panic on treatment response in LLD. However, given the moderately high correlation between the two factors, we decided against using the factors as continuous, independent variables, instead deciding to plot the score distribution and identify subgroups, as detailed below.
Table 1.
Factor loadings of the two-factor solution from the principal components analysis of 6 BSI items.
| Items | Factor1 Panic |
Factor 2 Worry |
|---|---|---|
| suddenly scared for no reason | 0.898 | 0.190 |
| spells of terror or panic | 0.817 | 0.231 |
| feeling fearful | 0.747 | 0.365 |
| feeling tense or keyed up | 0.200 | 0.888 |
| nervousness or shakiness inside | 0.246 | 0.825 |
| feeling so restless you couldn't sit still | 0.276 | 0.681 |
Based on the bivariate distribution of the worry and panic factor scores, a cutoff point of 1 was used for both worry and panic factors to split the groups into high-versus-low worry and high-versus-low panic respectively. The cutoff point of 1 has also demonstrated predictive validity in previous analyses based on the total anxiety BSI score (14). We confirmed the adequacy of the cutoff points through screen-plot analysis of the bivariate distribution. Thus we obtained four sub-groups: low panic – low worry, high panic – low worry, low panic – high worry, and high panic – high worry. Due to the small number of subjects (n=4) who had high panic - low worry, we excluded these subjects from further analyses.
Demographic and clinical characteristics of the sample are described in Table 2. There was no statistical significant difference between the core HDRS baseline scores for the three sub-groups (see table 2). Subjects with high worry – high panic were more likely than the other two sub-groups to have an earlier age of onset and recurrent LLD (versus single-episode LLD). Subjects with high worry-high panic were more likely than the other two sub-groups to receive rescue benzodiazepine treatment during the acute treatment trial (see table 2).
Table 2.
Demographic and clinical characteristics of patients by level of Brief Symptom Inventory (BSI) worry and BSI panic scores.
| Low Low (LL) (N=60) |
High Worry Low Panic (HL) (N=68) |
High Worry High Panic (HH) (N=38) |
F/Chi-square | DF | P value | |
|---|---|---|---|---|---|---|
| Current Agea | 76.8 (5.2) | 76.5 (6.1) | 76.6 (4.7) | 0.05 | 2,163 | 0.95 |
| % Female (N) | 58.3 (n=35) | 66.2 (n=45) | 73.7 (n=28) | 2.48 | 2 | 0.29 |
| % Caucasian (N) | 95.0 (n=57) | 94.1 (n=64) | 86.8 (n=33) | 2.62 | 2 | 0.27 |
| Education level (years) | 12.6 (2.9) | 13.2 (3.0) | 13.4 (2.9) | 1.10 | 2,163 | 0.34 |
| CIRS-G* | 10.0 (3.4) | 9.8 (4.1) | 10.6 (4.8) | 0.48 | 2,163 | 0.62 |
| HDRS 17 core items subscale ** | 6.7 (1.5) | 7.3 (1.5) | 7.3 (1.6) | 2.72 | 2,163 | 0.07 |
| Age at onset of first episode of depression | 63.6 (17.9) | 64.3 (17.3) | 54.7 (21.1) | 3.73 | 2,163 | 0.03 HL > HH |
| % with recurrent MDD | 38.3 (n= 23/60) |
39.7 (n=27/68) |
71.1 (n=27/38) |
12.08 | 2 | 0.002 HH > LL, HL |
| % taking benzodiazepine during acute treatment | 21.7 (n=13/60) |
39.7 (n= 27/68) |
55.3 (n=21/38) |
11.73 | 2 | 0.003 HL, HH > LL |
| Duration of current episode (weeks)b | 119.5 (224.8) median=35.5 |
126.2 (235.1) median = 48.0 |
64.4 (86.0) median = 36.0 |
1.33 | 2,163 | 0.27 |
| % with a co-morbid diagnosis of any anxiety disorder at baseline (N) | 20.3 (n=12/59) |
28.4 (n=19/67) |
41.7 (n=15/36) |
5.00 | 2 | 0.08 |
All results are mean (SD) unless indicated otherwise. Means and standard deviations are reported in the original units.
SQRT transformation used in the analyses.
LN transformation used in the analyses.
CIRS-G = Cumulative Illness Rating Scale for Geriatrics
HDRS 17 core item subscale = 17-item version of the Hamilton Depression Rating Scale items 1, 2, 3, 7.
2. Association of worry and panic with LLD response during acute treatment
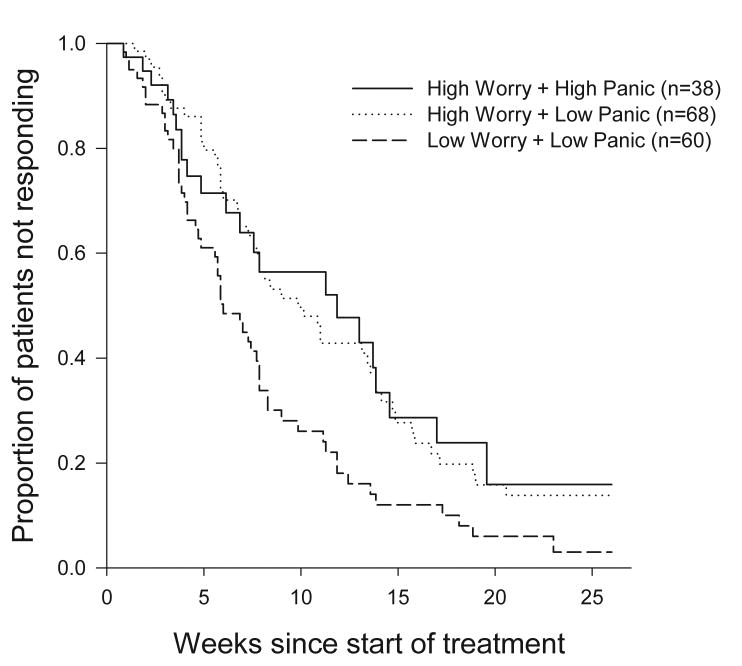
Significantly more subjects with low panic-low worry achieved response than subjects with either low panic-high worry or high panic-high worry: among subjects with low panic-low worry, 88.3% (53/60) achieved response; among subjects with low panic – high worry 73.5% (50/68) achieved response; among subjects with high panic – high worry, 57.9% (22/38) achieved response (Wilcoxon chi-square 11.78, df=2, p=0.003). There was no difference between the proportion of low panic-high worry subjects who achieved response and the proportion of high panic-high worry subjects who achieved response (chi-square=2.74, df=1, p = 0.09).
Time to response also differed among the 3 groups (Wilcoxon chi-square = 9.81, df=2, p=0.007). Subjects with both low panic- high worry and with high panic-high worry had a median time to response significantly longer than those with low panic – low worry: 9.9 weeks [95%CI: 7.6 – 13.6] and 11.9 weeks respectively [95%CI = 6.9 – 14.6] vs. 6.0 [95%CI: 4.9-7.9] weeks (Wilcoxon chi-square= 8.67, df =1, p=0.003 and Wilcoxon chi-square = 3.98, df=1, p= 0.046). Subjects with low panic- high worry did not differ significantly from subjects with high panic – high worry in term of median time to response (Wilcoxon chi square= 0.03, df =1, p=0.86) (see figure 1 and table 3).
Figure 1.
Co-morbid dimensions of anxiety and time to response. Subjects with high worry-high panic and subjects with high worry-low panic had a median time to response significantly longer than those with low worry-low panic (Wilcoxon chi-square = 9.81, df = 2, p=0.007)
Table 3.
Association of worry and panic with LLD response during acute and maintenance treatment
| Time to response/recurrence | Low panic – low worry Subgroup (A) | Low panic- high worry Subgroup (B) | High panic – high worry subgroup (C) | Differences between groups |
|---|---|---|---|---|
| Time to response - weeks (median/95%CI) | 6.0 [4.9-7.9] | 9.9 [7.6-13.6] | 11.9 [6.9-14.6] | A vs. B: Wilcoxon chi-square= 8.67, df=1, p=0.003 |
| A vs. C: Wilcoxon chi-square = 3.98, df=1, p=0.046 | ||||
| B vs. C: Wilcoxon chi-square = 0.03, df=1, p=0.86 | ||||
| Time to recurrence (on drug) – weeks (mean/standard error) | 66.9 [5.2] | 35.0 [2.3] | 55. 4 [10.7] | A vs. B: Log-rank Monte Carlo p=0.015 (99% CI = 0.01-0.02) |
| A vs. C: Log-rank Monte Carlo p=0.048 (99% CI = 0.04 – 0.05) | ||||
| B vs. C: Log-rank Monte Carlo p= 0.98 (99% CI = 0.98-0.99) | ||||
3. Association of worry and panic with recurrence of major depressive episodes during maintenance treatment
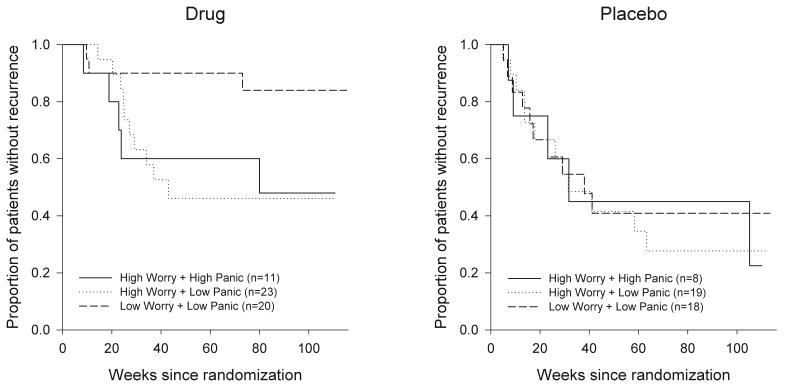
Time to recurrence in the subjects randomized to Paroxetine differed when stratified by worry and panic (Log rank Monte Carlo estimate of p= 0.038, 99%CI = 0.03 – 0.04). Post hoc tests focusing on the difference between the three sub-groups showed that subjects with low panic-high worry and high panic – high worry had shorter time to recurrence than subjects with the low panic - low worry (Log rank Monte Carlo estimate of p = 0.015, 99%CI = 0.01-0.02 and p=0.048, 99% CI = 0.04-0.05 respectively). There was no difference between subjects with low panic – high worry group and subjects with high panic – high worry with regard to time of recurrence (Log-rank Monte Carlo p= 0.902, 99%CI = 0.89-91) (See figure 2 and table 3).
Figure 2.
Co-morbid dimensions of anxiety symptoms and time to recurrence. The mean time to recurrence was significantly longer in low worry-low panic subjects randomized to drug (log-rank p=0.038). There was no difference between subjects with high worry-low panic and high worry-high panic with regard to time to recurrence of late-life depression.
Discussion
In this study of the differential impact of dimensions of anxiety on pharmacotherapy of LLD, high worry severity was associated with longer time to response and shorter time to recurrence of major depressive episodes. In contrast, high panic severity did not add to the burden of worry symptoms on the treatment response variability of LLD.
It is worth noting that these results were obtained in subjects treated with paroxetine, an SSRI that is indicated for the treatment of both major depressive disorder and several anxiety disorders (28). However, in our older subjects, the benefits of paroxetine were diminished when depression and anxiety were co-occurring (14).
Our study suggests the importance of different dimensions of anxiety in late life. The most common comorbid diagnosis in late-life depression is Generalized Anxiety Disorder (GAD), and consequently its main clinical feature – excessive and uncontrollable worry – is common as well. Although panic symptoms can be common in depression, it appears they are less common in older adults than in younger adults (29). The reason for this is unclear but may result from brain changes with aging that reduce the arousal or panic response, selective mortality that leads to survivor cohorts in elderly, or the fact that measures of anxiety created for young adults may be inadequately sensitive to its presentation in older adults (29).
Although subjects with low panic - high worry and those with high panic - high worry differed with regard to number of previous MDD episodes (more subjects with high panic - high worry had a history of recurrent MDD), there was no difference in time to response or in time to recurrence between the two sub-groups. Given the well-known predicting role of previous episodes of depression on treatment response in LLD (30), our results may suggest at least an equally prominent predictive role of these various anxiety dimensions, especially of the worry spectrum symptoms.
Our results may be considered in the context of reports suggesting that there is a psychometric and neuroanatomical distinction between two types of anxiety: anxious arousal and anxious apprehension (31, 32). Clinically, anxious arousal is noticed mainly in disorders characterized by intense fear (panic disorder, post-traumatic stress disorder, phobias), whereas anxious apprehension is noticed more in disorders characterized by pathological worry and rumination (GAD and obsessive-compulsive disorder). Evidence points toward different neuroanatomical substrates for these dimensions (33). Thus, disorders involving intense fear (i.e. panic disorder, PTSD and phobias) are characterized by a hyperactive amygdala coupled with a hypoactive prefrontal cortex, while disorders involving anxiety apprehension and its symptoms of worry and rumination (such as GAD and OCD) are more likely characterized by hyperactivity of the prefrontal cortex (33). These results are based on younger cohorts and their relevance to geriatric psychopathology is not yet known. However, there is strong evidence of prefrontal dysfunction in late-life depression and its predictive role for antidepressant treatment response (34-36). Thus, one can speculate that the worse impact of worry on depression treatment in the elderly is correlated to the prefrontal dysfunction associated with anxious apprehension (37).
Our study has several strengths. While our study is a secondary analysis testing a post-hoc hypothesis, it is based on data obtained in a randomized trial conducted under double-blind, placebo-controlled conditions. The original trial's design allowed us to examine the impact of different dimensions of anxiety on the long-term outcome of pharmacotherapy of LLD. Limitations include the use of a single measure of anxiety, preventing us from detecting more subtle variations of the anxiety spectrum symptoms. Also, the two dimensions of anxiety – BSI worry and BSI panic -- have been constructed based on a limited number of symptoms (accessible with the BSI anxiety scale), and for BSI worry we lacked a specific item inquiring directly about excessive and uncontrollable worry. Moreover, our sample size did not allow us to use a confirmatory factor analysis and thus, our results were obtained using an exploratory principal components analysis. Also, we could not analyze the entire spectrum of worry-panic distribution because we had a very limited number of subjects with high panic – low worry. This limitation reduced our power and precludes us from drawing conclusions regarding the differential impact of worry and panic on treatment response in LLD. Thus, based on this dataset, we can only infer that panic does not appear to increase the risk in terms of response to, and recurrence during with antidepressant treatment when accounting for the effects of excessive worry.
To our knowledge this is the first study reporting the impact of different dimensions of anxiety on short- and long-term treatment of depression in the elderly. Further research is needed to focus more specifically on the predictive power of different dimensions of anxiety, to define neurobiological correlates of these dimensions, and to define how these may be relevant to treatment response variability as potential moderators or mediators.
Acknowledgments
Supported by NIMH P50 071944, MH 43832 the John A. Hartford Foundation Center of Excellence in Geriatric Psychiatry and the University of Pittsburgh Medical Center (UPMC) endowment in Geriatric Psychiatry.
Footnotes
Conflict of Interest: Carmen Andreescu and Amy Begley have no conflict of interest to report. Eric J. Lenze has received research support from OrthoMcNeill, Novartis and Forest Pharmaceuticals. Benoit H. Mulsant has received research support or honoraria from Astra-Zeneca, Bristol-Myers Squibb, Eli Lilly, Forest Laboratories, GlaxoSmithKline, Janssen, Lundbeck, and Pfizer; he holds stock (all less than $10,000) in Akzo-Nobel, Alkermes, AstraZeneca, Biogen Idec, Celsion, Elan, Eli Lilly, Forest and Orchestra Therapeutics. Dr. Wetherell has received research support from Forest Pharmaceuticals. Sati Mazumdar directly purchased stocks from Forest (less than $10,000). Charles F. Reynolds III has received pharmaceutical supplies for his NIH-sponsored research from GlaxoSmithKline, Pfizer Inc., Eli Lilly and Co., Bristol Meyers Squibb, Wyeth Pharmaceuticals and Forest Pharmaceuticals.
References
- 1.Beekman AT, de Beurs E, van Balkom AJ, Deeg DJ, van Dyck R, van Tilburg W. Anxiety and depression in later life: Co-occurrence and communality of risk factors. Am J Psychiatry. 2000;157(1):89–95. doi: 10.1176/ajp.157.1.89. [DOI] [PubMed] [Google Scholar]
- 2.Larkin BA, Copeland JR, Dewey ME, Davidson IA, Saunders PA, Sharma VK, et al. The natural history of neurotic disorder in an elderly urban population. Findings from the Liverpool longitudinal study of continuing health in the community. Br J Psychiatry. 1992;160:681–6. doi: 10.1192/bjp.160.5.681. [DOI] [PubMed] [Google Scholar]
- 3.Fawcett J. The detection and consequences of anxiety in clinical depression. J Clin Psychiatry. 1997;58 Suppl 8:35–40. [PubMed] [Google Scholar]
- 4.Flint AJ, Rifat SL. Anxious depression in elderly patients. Response to antidepressant treatment. Am J Geriatr Psychiatry. 1997;5(2):107–15. [PubMed] [Google Scholar]
- 5.Steffens DC, McQuoid DR. Impact of symptoms of generalized anxiety disorder on the course of late-life depression. Am J Geriatr Psychiatry. 2005;13(1):40–7. doi: 10.1176/appi.ajgp.13.1.40. [DOI] [PubMed] [Google Scholar]
- 6.Mulsant BH, Reynolds CF, 3rd, Shear MK, Sweet RA, Miller M. Comorbid anxiety disorders in late-life depression. Anxiety. 1996;2(5):242–7. doi: 10.1002/(SICI)1522-7154(1996)2:5<242::AID-ANXI6>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 7.Dew MA, Reynolds CF, 3rd, Houck PR, Hall M, Buysse DJ, Frank E, et al. Temporal profiles of the course of depression during treatment. Predictors of pathways toward recovery in the elderly. Archives of General Psychiatry. 1997;54(11):1016–24. doi: 10.1001/archpsyc.1997.01830230050007. see comment. [DOI] [PubMed] [Google Scholar]
- 8.Lenze EJ, Mulsant BH, Dew MA, Shear MK, Houck P, Pollock BG, et al. Good treatment outcomes in late-life depression with comorbid anxiety. J Affect Disord. 2003;77(3):247–54. doi: 10.1016/s0165-0327(02)00177-5. [DOI] [PubMed] [Google Scholar]
- 9.Alexopoulos GS, Katz IR, Bruce ML, Heo M, Ten Have T, Raue P, et al. Remission in depressed geriatric primary care patients: a report from the PROSPECT study. American Journal of Psychiatry. 2005;162(4):718–24. doi: 10.1176/appi.ajp.162.4.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clayton PJ, Grove WM, Coryell W, Keller M, Hirschfeld R, Fawcett J. Follow-up and family study of anxious depression. Am J Psychiatry. 1991;148(11):1512–7. doi: 10.1176/ajp.148.11.1512. [DOI] [PubMed] [Google Scholar]
- 11.Emmanuel J, Simmonds S, Tyrer P. Systematic review of the outcome of anxiety and depressive disorders. Br J Psychiatry Suppl. 1998;(34):35–41. [PubMed] [Google Scholar]
- 12.Dombrovski AY, Mulsant BH, Houck PR, Mazumdar S, Lenze EJ, Andreescu C, et al. Residual symptoms and recurrence during maintenance treatment of late-life depression. J Affect Disord. 2007 doi: 10.1016/j.jad.2007.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flint AJ. Epidemiology and comorbidity of anxiety disorders in later life: implications for treatment. Clin Neurosci. 1997;4(1):31–6. [PubMed] [Google Scholar]
- 14.Andreescu C, Lenze EJ, Dew MA, Begley AE, Mulsant BH, Dombrovski AY, et al. Effect of comorbid anxiety on treatment response and relapse risk in late-life depression: controlled study. Br J Psychiatry. 2007;190:344–9. doi: 10.1192/bjp.bp.106.027169. [DOI] [PubMed] [Google Scholar]
- 15.Mobbs D, Petrovic P, Marchant JL, Hassabis D, Weiskopf N, Seymour B, et al. When fear is near: threat imminence elicits prefrontal-periaqueductal gray shifts in humans. Science. 2007;317(5841):1079–83. doi: 10.1126/science.1144298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wetherell JL, Le Roux H, Gatz M. DSM-IV criteria for generalized anxiety disorder in older adults: distinguishing the worried from the well. Psychol Aging. 2003;18(3):622–7. doi: 10.1037/0882-7974.18.3.622. [DOI] [PubMed] [Google Scholar]
- 17.Gould RA, Safren SA, Washington DO, Otto MW. A meta-analytic review of cognitive-behavioral treatments. In: Heimberg RG, T CL, M DS, editors. Generalized anxiety disorder: Advances in research and practice. New York: Guildford Press; 2004. [Google Scholar]
- 18.Reynolds CF, 3rd, Dew MA, Pollock BG, Mulsant BH, Frank E, Miller MD, et al. Maintenance treatment of major depression in old age. N Engl J Med. 2006;354(11):1130–8. doi: 10.1056/NEJMoa052619. [DOI] [PubMed] [Google Scholar]
- 19.First M, S R, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I Disorders - Patient Edition (SCID-I/P) (Version 2.0) 1995 [Google Scholar]
- 20.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 22.Klerman GL, W M, Rounsaville BJ, Chevron E. Interpersonal Psychotherapy of Depression. 1984 [Google Scholar]
- 23.Derogatis LR, M N. The Brief Symptom Inventory: an introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- 24.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605. [PubMed] [Google Scholar]
- 25.Shafer AB. Meta-analysis of the factor structures of four depression questionnaires: Beck, CES-D, Hamilton, and Zung. J Clin Psychol. 2006;62(1):123–46. doi: 10.1002/jclp.20213. [DOI] [PubMed] [Google Scholar]
- 26.Dombrovski AY, Blakesley-Ball RE, Mulsant BH, Mazumdar S, Houck PR, Szanto K, et al. Speed of improvement in sleep disturbance and anxiety compared with core mood symptoms during acute treatment of depression in old age. Am J Geriatr Psychiatry. 2006;14(6):550–4. doi: 10.1097/01.JGP.0000218325.76196.d1. [DOI] [PubMed] [Google Scholar]
- 27.Cytel Software Corporation C, MA. StatXact 8: Statistical Software for Exact Nonparametric Inference.
- 28.Pae CU, Patkar AA. Paroxetine: current status in psychiatry. Expert Rev Neurother. 2007;7(2):107–20. doi: 10.1586/14737175.7.2.107. [DOI] [PubMed] [Google Scholar]
- 29.Lenze EJ, Mulsant BH, Shear MK, Schulberg HC, Dew MA, Begley AE, et al. Comorbid anxiety disorders in depressed elderly patients. Am J Psychiatry. 2000;157(5):722–8. doi: 10.1176/appi.ajp.157.5.722. [DOI] [PubMed] [Google Scholar]
- 30.Bosworth HB, Hays JC, George LK, Steffens DC. Psychosocial and clinical predictors of unipolar depression outcome in older adults. Int J Geriatr Psychiatry. 2002;17(3):238–46. doi: 10.1002/gps.590. [DOI] [PubMed] [Google Scholar]
- 31.Heller W, Nitschke JB, Etienne MA, Miller GA. Patterns of regional brain activity differentiate types of anxiety. J Abnorm Psychol. 1997;106(3):376–85. doi: 10.1037//0021-843x.106.3.376. [DOI] [PubMed] [Google Scholar]
- 32.Shankman SA, Klein DN. The relation between depression and anxiety: an evaluation of the tripartite, approach-withdrawal and valence-arousal models. Clin Psychol Rev. 2003;23(4):605–37. doi: 10.1016/s0272-7358(03)00038-2. [DOI] [PubMed] [Google Scholar]
- 33.Berkowitz RL, Coplan JD, Reddy DP, Gorman JM. The human dimension: how the prefrontal cortex modulates the subcortical fear response. Rev Neurosci. 2007;18(3-4):191–207. doi: 10.1515/revneuro.2007.18.3-4.191. [DOI] [PubMed] [Google Scholar]
- 34.Bae JN, MacFall JR, Krishnan KR, Payne ME, Steffens DC, Taylor WD. Dorsolateral prefrontal cortex and anterior cingulate cortex white matter alterations in late-life depression. Biol Psychiatry. 2006;60(12):1356–63. doi: 10.1016/j.biopsych.2006.03.052. [DOI] [PubMed] [Google Scholar]
- 35.Alexopoulos GS. Frontostriatal and limbic dysfunction in late-life depression. Am J Geriatr Psychiatry. 2002;10(6):687–95. [PubMed] [Google Scholar]
- 36.Alexopoulos GS. Depression in the elderly. Lancet. 2005;365(9475):1961–70. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 37.Nitschke JB, Sarinopoulos I, Mackiewicz KL, Schaefer HS, Davidson RJ. Functional neuroanatomy of aversion and its anticipation. Neuroimage. 2006;29(1):106–16. doi: 10.1016/j.neuroimage.2005.06.068. [DOI] [PubMed] [Google Scholar]